Abstract
OBJECTIVES/HYPOTHESIS
The primary study goal was to measure health state utility values in patients with chronic rhinosinusitis (CRS) before and after undergoing endoscopic sinus surgery (ESS). A secondary goal was to assess the meaning of these values by comparing them with other chronic disease processes and currently available medical or surgical treatments.
STUDY DESIGN
Prospective, observational cohort study
METHODS
Adults with CRS were enrolled after electing ESS and observed over a 5-year period. Baseline demographic and medical comorbidities were recorded for each patient, as well as computed tomography (CT), endoscopy, olfaction, and disease-specific quality of life scores. Utility values were derived using the Short-Form 6D (SF-6D) at baseline and again after surgery.
RESULTS
The mean SF-6D utility value for the baseline health state of all patients with CRS (n=232) was 0.65 (95% CI: 0.63–0.66). Baseline utility values correlated with disease-specific QOL as measured by the Rhinosinusitis Disability Index (RSDI) (r=−0.660; P<0.001), but not baseline CT, endoscopy, or olfactory scores. Follow-up utility values (≥6 months) after ESS improved by 0.087 (95% CI: 0.06–0.12; P<0.001) in patients with no history of sinus surgery and 0.062 (95% CI: 0.04–0.09; P<0.001) in those undergoing a revision procedure.
CONCLUSIONS
Patients with CRS who failed medical therapy and elected to undergo ESS report health state utility values which are significantly lower than the United States population norm. Utility values showed improvement after ESS which was statistically and clinically significant. These results provide the initial data necessary for formal cost-effectiveness analyses incorporating ESS.
Keywords: sinusitis, endoscopic surgical procedure, treatment utility, cost-benefit analysis
INTRODUCTION
Chronic rhinosinusitis (CRS) is a debilitating condition with significant impacts on sinonasal function and overall health. Patient-reported quality of life (QOL) has become the primary metric by which CRS disease burden is measured and outcomes are assessed after treatment.1 Patients with CRS consistently show declines in disease-specific and general QOL, including physical, emotional, and functional domains.2 Prior studies have demonstrated sustained improvements in QOL after endoscopic sinus surgery (ESS), providing justification for surgical treatment in patients who have failed medical therapy.2
Health state values, or “utilities,” are a measure of preference-based health-related quality of life (HRQOL) often used by health economists.3 Utility values are unique because they represent an individual’s valuation or preference for being in a particular health state. This differs from generic QOL instruments, such as the Medical Outcomes Study Short Form-36 Health Survey (SF-36), which quantify a health state in terms of symptoms and functioning without ascribing a value.4 Health state utilities are defined on a scale from 0.0 – 1.0, with 0.0 representing death and 1.0 representing perfect health.
Health state utilities are clinically useful because they measure outcomes in a single, common metric, allowing meaningful comparison across diseases and interventions. Utility values are also a critical component of economic evaluations of medical interventions, including cost-effectiveness research. Cost-effectiveness analysis is a specific methodology for quantifying and comparing the costs-per-health-benefit achieved by particular interventions.3 The US Public Health Service Panel on Cost Effectiveness in Health and Medicine has recommended that the quality-adjusted life year (QALY) be used as the standard measure of health benefit in cost effectiveness research.5 A QALY is the additional year(s) of life gained by a treatment or intervention weighted by the utility, or quality, of those additional year(s). At present, utility values for patients with CRS have not been described and it is unknown whether patients’ utility improves after ESS. As health care systems are increasingly forced to make choices to allocate scare funding resources, it is imperative that sufficient data are available to make evidence-based recommendations regarding CRS and available treatment strategies.
The goal of this study was to measure health state utility values in a prospective, observational cohort of patients with chronic rhinosinusitis before and after endoscopic sinus surgery. A secondary goal was to assess the meaning of these values by comparing them with other chronic disease processes and currently available medical or surgical treatments.
MATERIALS and METHODS
Patients
Adults (≥18 years) with CRS were prospectively enrolled and observed over a 5-year period at Oregon Health and Science University (OHSU) between September, 2004 –April, 2009. Patients were recruited if they had CRS according to consensus criteria of the American Academy of Otolaryngology-Head and Neck Surgery, continued to have symptoms despite prior medical therapy, and elected to pursue surgical treatment.6 Demographic information and social history were collected at the time of enrollment, including age, gender, current tobacco use (packs/day), and current alcohol consumption (grams/week). The presence or absence of polyps, acetylsalicylic acid (ASA) intolerance, septal deviation, allergies (skin prick or a modified radioallergosorbent system), asthma, and depression was documented for each enrollee. The Institutional Review Board at OHSU provided approval and oversight for all study activities and informed consent was obtained from all subjects.
Disease Severity
The severity of CRS was quantified using computed tomography (CT), sinonasal endoscopy, olfactory testing, and disease-specific QOL. Standard CT scans of the nose and sinuses using 3mm cross-sections were obtained at baseline and staged according to the Lund-Mackay CT scoring system (total score of 0 to 24 is possible, with higher scores indicating more disease).7 Rigid sinonasal endoscopy was performed at baseline and after surgery. The endoscopic appearance was graded according to the system outlined by Lund and Kennedy (0–20 total score, with higher scores indicating more severe disease).8 Olfaction was tested using the Smell Identification Test (SIT). The SIT is 40-item, forced choice, odorant strip test which is graded from 0 – 40, with 40 representing perfect smell (Sensonics, Inc. Haddon Heights, NJ).9 CRS-specific QOL was assessed using the Rhinosinusitis Disability Index (RSDI).10 The RSDI is a 30-item survey developed to assess the impact of CRS on physical, emotional, and functional domains. Scores on the RSDI range from 0–120, with higher scores representing poorer health.
Health State Utility Values
Each subject completed the Short-Form 6D (SF-6D) at baseline and again after surgical treatment. The SF-6D is a subset of question from the SF-36 which evaluates 6 multi-level dimensions of health, enumerating a total of 18,000 possible health states.11 Health domains include physical functioning, role limitation, social functioning, bodily pain, mental health, and vitality. The SF-6D instrument has been used extensively for cost effectiveness research and has been shown to be valid and reliable.12 Health states denoted by SF-6D scores were transformed into health state utility values using a weighted algorithm outlined by Brazier et al. and used with permission from the Department of Health Economics and Decision Science at The University of Sheffield, Sheffield, UK .11 This algorithm estimates the value that the general population places on any particular health state that is described with the SF-6D questions. In other words, how the average person in the population would feel if they had the particular symptoms and functioning described by a patient who completes the SF-6D questionnaire with a certain set of responses. The boundaries of the SF-6D range from 0.3–1.0, with lower scores indicating poorer valuation of a particular health state and 1.0 being in perfect health. A change in utility value of 0.03 on this scale is considered to be the minimal clinically important difference (MCID).13
Surgical Treatment
Each patient underwent endoscopic sinus surgery by one of three different surgeons at OHSU. The extent and nature of each surgery was dictated by the clinical picture, as per standard of care. Study coordinators assisted with the completion of all outcome measures and ensured clinicians remained blinded to all patient-reported responses throughout the study duration, including olfaction, QOL, and SF-6D scores.
Statistical Analysis
Mean utility values for CRS patients at baseline are presented along with standard deviations (SD) and confidence intervals where appropriate. Differences in baseline utility between subgroups defined by demographics and medical comorbidities were compared using a two-sided t-test for equality of means. Correlation between baseline utility values and disease severity measures (CT, endoscopy, olfaction, QOL) was performed using Pearson’s correlation coefficient. The change in utility value after ESS is presented in those patients with at least 6 months follow-up, using the value from the last available time-point for analysis. A primary endpoint of ≥6 month follow up was selected since mean QOL outcomes in this population have been shown to be static after 6 months and up to 20 months post-surgery.14 Differences in utility change after surgery were compared in subgroups defined by medical comorbidities, using multivariate linear regression to control for age, gender, and depression. Bivariate correlations between change in utility after ESS and change in other disease severity measures was also performed using Pearson’s correlation coefficient. A P-value <0.05 was considered statistically significant.
Baseline utility values for the overall cohort with CRS were then compared to other chronic disease processes present within the literature as well as norms for the United States (US) population. Similarly, changes in utility after ESS were compared with changes reported after medical/surgical interventions for other common chronic diseases. US norms were derived from the report of Hanmer et al. detailing SF-6D scores in a nationally representative survey of healthy American adults.15 The US norms were derived using a standardized weighted average of our CRS cohort by age and gender distributions. Utility values for other chronic illnesses and associated interventions were obtained from previously published reports identified by a Pubmed database search utilizing “SF-6D”and “utility” as a keywords. Studies were reviewed if they utilized the SF-6D instrument to assess utilities at baseline and/or after an intervention. A total of 23 studies were identified which reported mean utility values for a given chronic disease. Mean utility values were displayed graphically for a range of common chronic disease processes and associated medical and surgical treatments. No attempt was made to adjust for age, gender, or associated medical comorbidities.
RESULTS
A total of 232 patients with CRS were enrolled during the study period. All patients elected and underwent endoscopic sinus surgery for CRS and completed all necessary study documentation at baseline. Baseline SF-6D utility values were available for 230 / 232 patients (99.1%), with 2 having incomplete or illegible evaluations. Follow-up utility values (≥6 months) after ESS were available for 168/232 (72.4%) of enrollees at an average of 17.5(6.3) months following surgery. Patients lost to follow-up were analyzed with respect to age, gender, and comorbidities, with no significant differences appreciated compared to those who did complete the study protocol. Patients included in follow-up analysis did have lower baseline utility scores compared to those lost to follow-up (0.62 vs 0.66; P =0.011).
Demographics, medical comorbidities, and social history for the study cohort are detailed in Table 1. The average age was 47.8(14.1) with just over half male gender. Nasal polyposis was present in 44.4% and 59.1% had undergone a prior sinus surgical procedure. Preoperative disease severity measures are shown in Table 2. Baseline scores on CT, endoscopy, olfaction, and QOL are similar to those published in other surgical cohorts with CRS.
Table 1.
Baseline demographics, comorbid conditions, and clinical characteristics (n=232)
| Variables: | Mean (SD) | Range: [min, max] | n(%) |
|---|---|---|---|
| Age (years) | 47.8 (14.1) | [18, 79] | |
| Gender: | |||
| Male | 121 (52.2) | ||
| Female | 111 (47.8) | ||
| Follow-up (mo.) | 17.5 (6.3) | [5, 39] | |
| Clinical characteristics: | |||
| Asthma | 86 (37.1) | ||
| Nasal polyposis | 103 (44.4) | ||
| Allergy | 58 (25.0) | ||
| Aspirin intolerance | 25 (10.8) | ||
| Depression | 38 (16.4) | ||
| Septal deviation | 70 (30.2) | ||
| History of prior sinus surgery | 137 (59.1) | ||
| Social history: | |||
| Tobacco use (packs/day) | 0.6 (0.4) | [0.1, 1.0] | 12 (5.2) |
| Alcohol consumption (gr./wk.) | 58.8 (62.8) | [0.2, 300.0] | 106 (45.7) |
SD= standard deviation of mean; min= minimum value in continuous range; max= maximum value in continuous range; mo.= months of follow-up; mRAST= confirmed via modified radioallergosorbent testing; gr. /wk.= grams per week.
Table 2.
Baseline measure of CRS disease severity (n=232)
| Variables: | Mean (SD) | Range: [min, max] |
|---|---|---|
| RSDI physical | 19.8 (7.4) | [2, 38] |
| RSDI functional | 15.8 (6.7) | [1, 34] |
| RSDI emotional | 13.8 (7.4) | [0, 39] |
| RSDI total | 49.3 (8.7) | [3, 105] |
| Diagnostic testing: | ||
| Lund-Kennedy endoscopy score | 7.3 (4.4) | [0, 20] |
| Lund-Mackay CT score | 12.7 (6.5) | [0, 24] |
| Olfactory (SIT) score | 26.8 (10.4) | [4, 39] |
CRS= chronic rhinosinusitis; SD= standard deviation of mean; min= minimum value in continuous range; max= maximum value in continuous range; RSDI= Rhinosinusitis Disability Index; CT= computed tomography; SIT= Smell Identification Test (Sensonics Inc., Haddon Heights, NJ).
The mean utility value for the baseline health state of all patients with CRS was 0.65 (95% CI: 0.63–0.66), with a range 0.37–0.96. On bivariate analysis, baseline utility values were found to be different between men and women (0.66 vs. 0.63; P =0.037; Table 3) and those with depression compared to those without depression (0.61 vs. 0.66; P=0.012). A trend for worse scores was seen in younger patients compared to older subjects, although this did not reach significance (P=0.104). Those patients with polyps did report slightly better baseline utility values than those without polyps (P=0.029). Differences in baseline utility were examined among subgroups defined by medical comorbidities after adjusting for age, gender, and depression in multivariate modeling. Utility values did not differ significantly based on prior surgery or the presence of allergies, asthma, ASA intolerance, or septal deviation.
Table 3.
Mean baseline SF-6D utility values across demographic, comorbid, and clinical characteristics (n=230)
| Variables: | Utility Score Mean (SD) |
P-value |
|---|---|---|
| Age: | ||
| 18–49* | 0.637 (0.098) | |
| 50–79 | 0.662 (0.124) | 0.104 |
| Gender: | ||
| Male | 0.664 (0.121) | |
| Female | 0.633 (0.100) | 0.037 |
| Study follow-up: | ||
| ≥ 6 months | 0.619 (0.108) | |
| None | 0.661 (0.112) | 0.011 |
| Asthma: | ||
| Present | 0.657 (0.128) | |
| Absent | 0.645 (0.101) | 0.426 |
| Nasal polyposis: | ||
| Present | 0.668 (0.123) | |
| Absent | 0.635 (0.099) | 0.029 |
| Allergy: | ||
| Present | 0.641 (0.118) | |
| Absent | 0.652 (0.110) | 0.503 |
| Aspirin intolerance: | ||
| Present | 0.679 (0.129) | |
| Absent | 0.646 (0.110) | 0.165 |
| Depression: | ||
| Present | 0.608 (0.098) | |
| Absent | 0.658 (0.113) | 0.012 |
| Septal deviation | ||
| Present | 0.665 (0.110) | |
| Absent | 0.643 (0.112) | 0.176 |
| History of prior sinus surgery | ||
| Yes | 0.643 (0.113) | |
| No | 0.659 (0.110) | 0.301 |
| Tobacco use | ||
| Yes | 0.634 (0.109) | |
| No | 0.650 (0.112) | 0.623 |
| Alcohol consumption | ||
| Yes | 0.661 (0.104) | |
| No | 0.640 (0.118) | 0.162 |
age was dichotomized at the median age value for this cohort
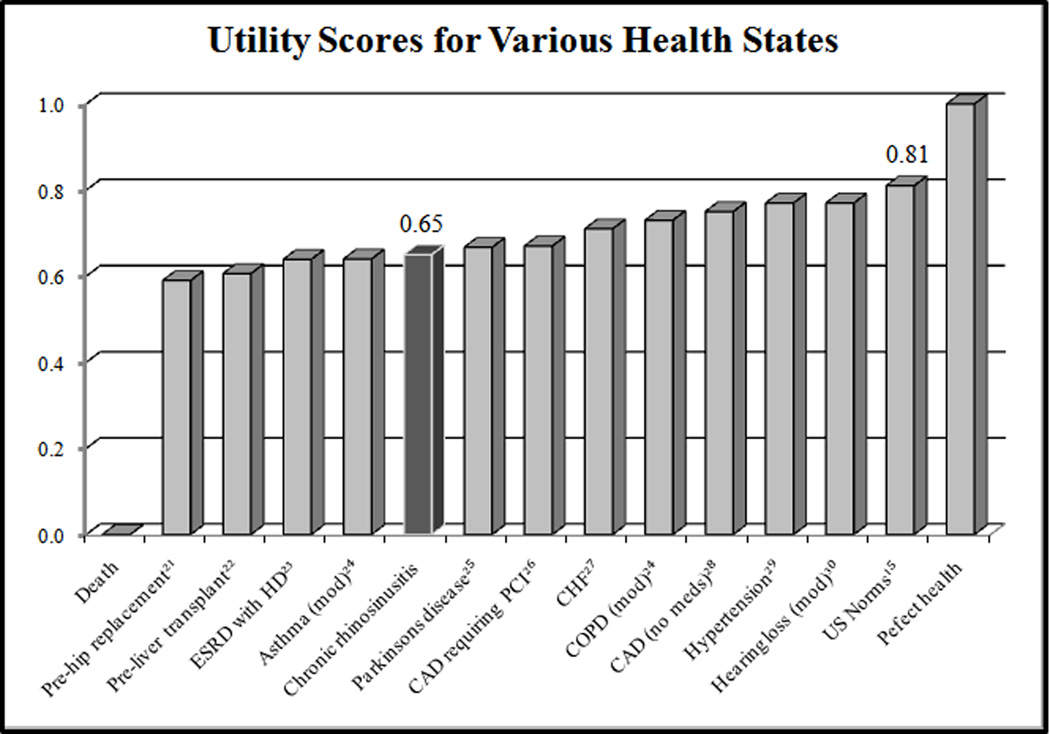
Correlation between utility and baseline disease severity was assessed. The strongest correlation was seen between utility value and disease-specific QOL as measured by the RSDI total score (r= −.660; P<0.001; Figure 1). Robust correlations were not seen between utility values and baseline CT, endoscopy, or olfactory scores.
FIGURE 1.
Correlation between utility value and CRS disease severity measures. SF-6D = Short Form 6D; RSDI=Rhinosinusitis Disability Index; CT=computed tomography; SIT=Smell Identification Test.
After endoscopic sinus surgery, a significant improvement in utility values was seen in the overall study cohort (P<0.001). Utility values improved by 0.087 (95% CI: 0.06–0.12; P<0.001) in patients with no history of sinus surgery and 0.062 (95% CI: 0.04–0.09; P<0.001) in those undergoing a revision procedure (Table 4). Significant improvement was found across all subgroups with the exception of patients with self-reported depression, for which the results did not quite reach significance (P=0.100). The degree of reported improvement was similar between all patient subgroups, with the exception that patients who presented without nasal polyposis reported significantly more mean improvement in utility following ESS than those with polyps (Table 4).
Table 4.
Mean changes in SF-6D utility values across demographic, comorbid, and clinical characteristics (n=168)
| Utility Change after Endoscopic Sinus Surgery |
Difference; Unadjusted |
|
|---|---|---|
| Variables: | Mean (SD); P-value* | P-value |
| Age: | ||
| 18–49 | 0.084 (0.125); p<0.001 | |
| 50–79 | 0.060 (0.113); p<0.001 | 0.205 |
| Gender: | ||
| Male | 0.062 (0.109); p<0.001 | |
| Female | 0.081 (0.128); p<0.001 | 0.307 |
| Asthma: | ||
| Present | 0.065 (0.116); p<0.001 | |
| Absent | 0.077 (0.122); p<0.001 | 0.522 |
| Nasal polyposis: | ||
| Present | 0.051 (0.099); p<0.001 | |
| Absent | 0.092 (0.132); p<0.001 | 0.026 |
| Allergy: | ||
| Present | 0.096 (0.136); p<0.001 | |
| Absent | 0.064 (0.112); p<0.001 | 0.122 |
| Aspirin intolerance: | ||
| Present | 0.058 (0.102); p<0.001 | |
| Absent | 0.074 (0.121); p=0.023 | 0.591 |
| Depression: | ||
| Present | 0.048 (0.140); p=0.100 | |
| Absent | 0.076 (0.115); p<0.001 | 0.274 |
| Septal deviation | ||
| Present | 0.064 (0.125); p=0.001 | |
| Absent | 0.075 (0.118); p<0.001 | 0.619 |
| History of prior sinus surgery | ||
| Yes | 0.062 (0.115); p<0.001 | |
| No | 0.087 (0.124); p<0.001 | 0.194 |
age was dichotomized at the median age value for this cohort
Change in utility after surgery was also compared in subgroups defined by demographics and medical comorbidities using multivariate regression modeling. None of the measured covariates significantly influenced improvement in utility after surgery, including age, gender, asthma, aspirin intolerance, and depression. Similar to baseline findings, change in utility after surgery correlated strongly to change in RSDI total score (r = −0.604; P<0.001) but not changes in other disease severity metrics.
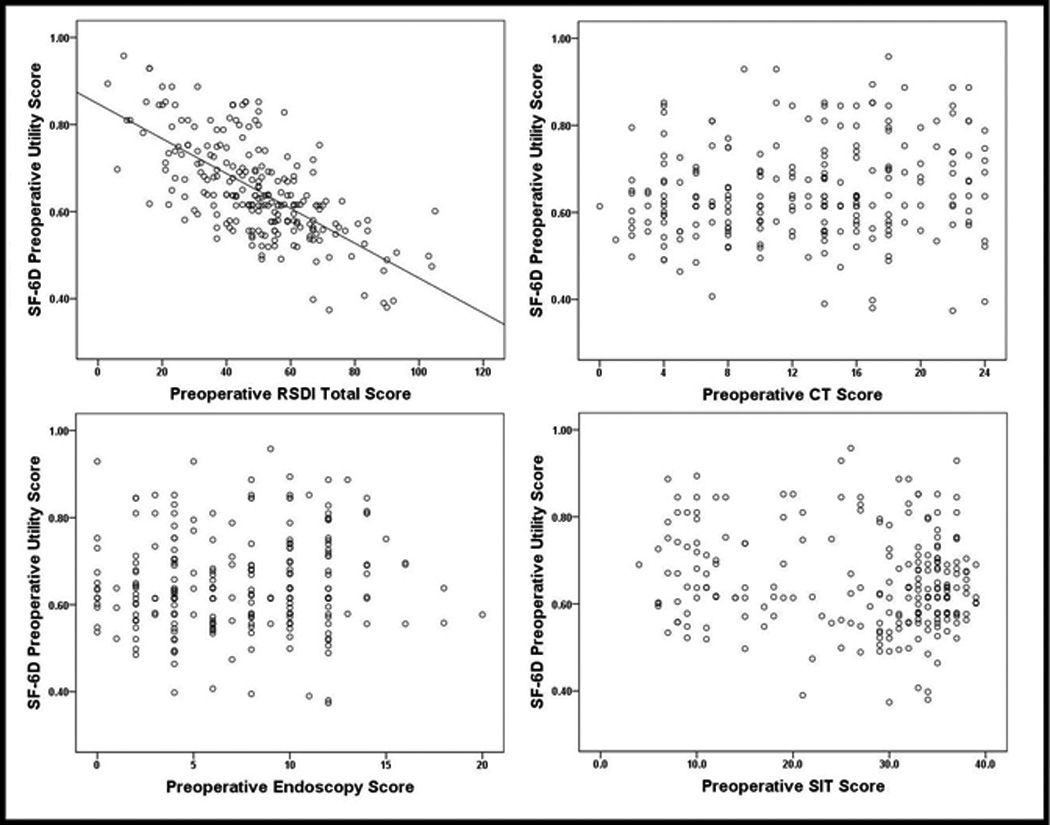
The baseline health state utility value of CRS patients was found to be well below the weighted average norm of the US population (0.81) and similar to that seen in many other chronic diseases (Figure 2). Similarly, the overall change in utility after sinus surgery appears comparable to those seen after medical or surgical treatments utilized in other chronic conditions (Figure 3). The change in utility value after ESS exceeded the minimal clinically important difference for both primary and revision surgical procedures.
FIGURE 2.
ESRD=end stage renal disease; HD=hemodialysis; mod=moderate; meds=medications; CAD=coronary artery disease; PCI=percutaneous coronary intervention; CHF=congestive heart failure; COPD=chronic obstructive pulmonary disease; US=United States.
FIGURE 3.
PD=Parkinson’s disease; CPAP=continuous positive airway pressure; TNF=tumor necrosis factor alpha.
DISCUSSION
In this cohort of patients with CRS, a significant decline in utility value was reported across all demographic and disease groupings compared to age and gender-matched US norms. Declines in utility correlated with the RSDI, a commonly used CRS-specific QOL instrument, but not CT scan, endoscopy, or olfaction. Patients undergoing surgery reported higher utilities for their health following the procedure, in excess of the minimally important clinical difference, suggesting that ESS improves the subjective health state experienced by patients with CRS.
Many studies have demonstrated significant improvement in sinonasal symptoms and QOL after ESS in patients with refractory CRS.2 Although results from these studies appear robust, it can be difficult to appreciate the importance or value of these findings within the broader healthcare context. An individual with a chronic disease process inherently makes judgments on the value of their current state of health, as compared with their baseline health or an anticipated state of health after a proposed intervention. Although rarely articulated in a formal fashion, these value judgments serve as the basis for treatment decisions, especially in the setting of non-life-threatening illnesses like CRS.16 Health state utilities, such as those presented in this study, quantify these value judgments in an explicit fashion. A single measure of value can then be used to compare across different conditions and treatment options. The findings from this study thus provide important, initial data which can be used to inform decision making on a broader level.
Although patients in this study reported health states which were valued much lower than population norms, these results may not be generalizable to all patients with CRS. The cohort followed in this study was recruited at a tertiary medical center and represents patients who had already failed maximal medical therapy and had elected sinus surgery. This may represent a subset of patients with more severe CRS than those who might otherwise respond to medical therapy. Those patients included in follow-up analysis also had lower baseline utilities compared to those lost to follow-up. However, CRS disease severity (CT score, endoscopy, and QOL) did mirror that seen in most reported surgical series.2 Although the cohort did include a large number of revision surgical cases (59.1%), baseline utility values were similar in patients undergoing primary or revision procedures. Taken together, these findings suggest that our data may be extrapolated to the over 250,000 CRS patients who undergo surgery each year in the US.17 That being said, controlled, multi-institutional studies which include both surgically and non-surgically treated patients will be necessary to fully appreciate long-term utility outcomes in patients with CRS.
The approach we used to measure the utility value assigned to different health outcomes is based on what are termed “societal” values for health states. These values represent what the general population feels about any particular health state, including both people with the particular condition and those without. This valuation approach is recommended by the U.S. Public Health Service's Panel on Cost-Effectiveness in Health and Medicine for use in analyses that address population-level resource allocation decisions.18 This approach stands in contrast to an individual perspective, wherein someone who actually has a particular medical condition values how they personally feel about living in that state of health. Although from a clinical decision-making standpoint the individual perspective may be more relevant, the societal perspective is used almost exclusively for policy-making on a broader, public health level because it reflects the priorities of the society as a whole.16
At present it remains unknown how patients with CRS would value their health status from an individual perspective. Clinicians should be cautious inferring that patients with CRS would value their health status equivalent to that reported in this study. There are numerous instances wherein the general population gives a lower value to a particular health state than those who actually have the condition, such as in post-laryngectomy patients.19,20 In these instances, the health state is considered better by those who have experienced it and worse by those who imagine it. Alternatively, patients with CRS might value their health state worse than that described by the general population in this study. Further research will be necessary to understand the individual perspective in order to better inform clinical decision making regarding ESS.
The utility decline for presurgical CRS patients was comparable to many other chronic disease states reported in the literature. This illustrates the significant impairment in health state experienced by patients with CRS, something which is perhaps not readily appreciated. Additionally, the level of improvement after surgery was clinically significant and similar to that seen after a range of medical and surgical treatments utilized in other chronic illnesses. These data suggest that the value gained by ESS compares favorably to other well-established treatments. These comparisons were intended to provide an overall context to understand the utility values in patients with CRS, rather than as a direct statistical appraisal. Just as utility values in the current study might not be fully generalizable to all patients with CRS, utility values published from other disease states may not fully represent that condition.
CONCLUSION
Patients with CRS who failed medical therapy and elected to undergo ESS report health state utility values which are significantly lower than the population norm. Utility values showed improvement after ESS which was statistically and clinically significant. These results provide the initial data necessary for formal cost-effectiveness analyses incorporating ESS. Collection of health state utilities should be considered in future studies which assess outcomes after treatment of CRS.
Acknowledgments
Rodney J. Schlosser, MD is a consultant for BrainLAB (Westchester, IL), Medtronic Inc.(Minneapolis, MN), and Gyrus ACMI (Bartlett, T.) and receives funding support from Medtronic Inc., NeilMed Pharmaceuticals Inc. (Santa Rosa, CA), and Arthocare Corporation (Austin, TX); Zachary M. Soler, MD is a consultant for Ora (Andover, MA); Timothy L. Smith is a consultant for Intersect ENT Inc. (Palo Alto, CA) which provided any financial support for this investigation. Timothy L. Smith, MD, MPH and Jess C. Mace, MPH also received grant funding from the National Institute on Deafness and Other Communication Disorders, one of the National Institutes of Health (R01DC005805-05; PI: Smith).
Footnotes
Financial Disclosure Information: There is no conflict of interest or financial disclosure for Eve Wittenberg, MPP, PhD;
REFERENCES
- 1.Meltzer EO, Hamilos DL, Hadley JA, et al. Rhinosinusitis: Establishing definitions for clinical research and patient care. Otolaryngol Head Neck Surg. 2004;131:S1–S62. doi: 10.1016/j.otohns.2004.09.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soler ZM, Smith TL. Quality of Life Outcomes After Functional Endoscopic Sinus Surgery. Otolaryngol Clin North Am. 2010;43:605–612. doi: 10.1016/j.otc.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torrance GW. Measurement of health state utilities for economic appraisal: A review. J Health Econom. 1986;5:1–30. doi: 10.1016/0167-6296(86)90020-2. [DOI] [PubMed] [Google Scholar]
- 4.Ware JE, Kosinski M, Gandek BG, et al. The factor structure of the SF-36® health survey in 10 countries: Results from the International Quality of Life Assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):1159–1165. doi: 10.1016/s0895-4356(98)00107-3. [DOI] [PubMed] [Google Scholar]
- 5.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172–1177. [PubMed] [Google Scholar]
- 6.Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline. Otolaryngol Head Neck Surg. 2007;137 Suppl:S1–S31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 7.Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology. 1993;31:183–184. [PubMed] [Google Scholar]
- 8.Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997;117:S35–S40. doi: 10.1016/S0194-59989770005-6. [DOI] [PubMed] [Google Scholar]
- 9.Doty RL. The Smell Identification TestTM Administration Manual. 3rd ed. Haddon Heights, New Jersey: Sensonics; 1995. pp. 1–17. [Google Scholar]
- 10.Benninger MS, Senior BA. The development of the rhinosinusitis disability index. Arch Otolaryngol Head Neck Surg. 1997;123:1175–1179. doi: 10.1001/archotol.1997.01900110025004. [DOI] [PubMed] [Google Scholar]
- 11.Brazier J, Roberts J, Deverill M. The estimation of preference-based measures of health from the SF-36. J Health Econ. 2002;21:271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 12.Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across 7 patient groups. Health Econ. 2004;13:873–884. doi: 10.1002/hec.866. [DOI] [PubMed] [Google Scholar]
- 13.Walters SJ, Brazier J. What is the relationsip between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes. 2003;1:4. doi: 10.1186/1477-7525-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soler ZM, Smith TL. Quality-of-life outcomes after endoscopic sinus surgery: How long is long enough? Otolaryngol Head Neck Surg. 2010;143:621–625. doi: 10.1016/j.otohns.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hanmer J, Lawrence WF, Anderson JP, Kaplan RM, Fryback DG. Report of nationally representative values for the noninstitutionalized US adult population for 7 health-related quality-of-life scores. Med Decis Making. 2006;26:391–400. doi: 10.1177/0272989X06290497. [DOI] [PubMed] [Google Scholar]
- 16.Hunink M, Glaziou P, Siegel J, et al. Decision making in health and medicine: Integrating Evidence and Values. New York City, NY: Cambridge University Press; 2001. [Google Scholar]
- 17.Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngscope. 2010;120:635–638. doi: 10.1002/lary.20777. [DOI] [PubMed] [Google Scholar]
- 18.Saha S, Hoerger TJ, Pignone MP, Teutsch SM, Helfand M, Mandelblatt JS. The art and science of incorporating cost-effectiveness into evidence-based recommendations for clinical preventative services. Am J Prev Med. 2001;20:36–43. doi: 10.1016/s0749-3797(01)00260-4. [DOI] [PubMed] [Google Scholar]
- 19.Otto RA, Dobie RA, Lawrence V, Sakai C. Impact of laryngectomy on quality of life: Perspective of the patient versus that of the health care provider. Ann Otol Rhinol Laryngol. 1997;106:693–699. doi: 10.1177/000348949710600815. [DOI] [PubMed] [Google Scholar]
- 20.Ubel PA, Loewenstein G, Schwarz N, Smith D. Misimagining the unimaginable: The disability paradox and health care decision making. Health Psychol. 2005;24:S57–S62. doi: 10.1037/0278-6133.24.4.S57. [DOI] [PubMed] [Google Scholar]
- 21.Feeny D, Lieling Wu, Ken Eng. Comparing Short Form 6D, standard gamble, and Health Utilities Index Mark 2 and Mark 3 utility scores: Results from total hip arthroplasty patients. Qual Life Res. 2004;13:1659–1670. doi: 10.1007/s11136-004-6189-2. [DOI] [PubMed] [Google Scholar]
- 22.Longworth L, Bryan S. An empirical comparison of EQ-5D and SF-6D in liver transplant patients. Health Econ. 2003;12:1061–1067. doi: 10.1002/hec.787. [DOI] [PubMed] [Google Scholar]
- 23.Kontodimopoulos N, Niakas D. An estimate of lifelong costs and QALYs in renal replacement therapy based on patients’ life expectancy. Health Policy. 2008;86:85–96. doi: 10.1016/j.healthpol.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 24.Szende A, Leidy NK, Stahl E, Svensson K. Estimating health utilities in patients with asthma and COPD: evidence on the performance of EQ-5D and SF-6D. Qual Life Res. 2009;18:267–272. doi: 10.1007/s11136-008-9429-z. [DOI] [PubMed] [Google Scholar]
- 25.Vossius C, Nilsen OB, Larsen JP. Health state values during the first year of drug treatment in early-stage Parkinson’s disease: a prospective, population-based, cohort study. Drugs Aging. 2009;26:973–980. doi: 10.2165/11318750-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 26.Hatoum HT, Brazier JE, Akhras KS. Comparison of the HUI3 with the SF-36 preference based SF-6D in a clinical trial setting. Value Health. 2004;7:602–609. doi: 10.1111/j.1524-4733.2004.75011.x. [DOI] [PubMed] [Google Scholar]
- 27.Kontodimopoulos N, Argiriou M, Theakos N, Niakas D. The impact of disease severity on EQ-5D and SF-6D utility discrepancies in chronic heart failure. Eur J Health Econ. 2010 May 15; doi: 10.1007/s10198-010-0252-4. Online First. [DOI] [PubMed] [Google Scholar]
- 28.Garster NC, Palta M, Sweitzer NK, Kaplan RM, Fryback DG. Measuring health-related quality of life in population-based studies of coronary heart disease: comparing six generic indexes and a disease-specific proxy score. Qual Life Res. 2009;18:1239–1247. doi: 10.1007/s11136-009-9533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joore M, Brunenberg D, Nelemans P, et al. The impact of differences in EQ-5D and SF-6D utility scores on the acceptability of cost-utility rations: results across five trial-based cost-utility studies. Value Health. 2010;13:222–229. doi: 10.1111/j.1524-4733.2009.00669.x. [DOI] [PubMed] [Google Scholar]
- 30.Barton GR, Bankart J, Davis AC. A comparison of the quality of life of hearing-impaired people as estimated by three different utility measures. Int J Audiol. 2005;44:157–163. doi: 10.1080/14992020500057566. [DOI] [PubMed] [Google Scholar]
- 31.Barton GR, Bankart J, Davis AC, Summerfield QA. Comparing utility scores before and after hearing-aid provision: results according to the EQ-5D, HUI3 and SF-6D. Appl Health Econ Health Policy. 2004;3:103–105. doi: 10.2165/00148365-200403020-00006. [DOI] [PubMed] [Google Scholar]
- 32.Schmidlin M, Fritsch K, Mathews F, Thurnheer R, Senn O, Bloch KE. Utility indices in patients with the obstructive sleep apnea syndrome. Respiration. 2010;79:200–8. doi: 10.1159/000222094. [DOI] [PubMed] [Google Scholar]
- 33.Saad AA, Ashcroft DM, Watson KD, Symmons DP, Noyce PR, Hyrich KL. Improvements in quality of life and functional status in patients with psoriatic arthritis receiving anti-tumor necrosis factor therapies. Arthrit Care Res. 2010;62:345–353. doi: 10.1002/acr.20104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slobegean GP, Younger A, Apostle KL, et al. Preference-based quality of life of end-stage ankle arthritis treated with arthroplasty or arthrodesis. Foot Ankle Int. 2010;31:563–566. doi: 10.3113/FAI.2010.0563. [DOI] [PubMed] [Google Scholar]
- 35.Osnes-Ringen H, Kvamme MK, Kristiansen IS, et al. Cost-effectiveness analyses of elective orthopaedic surgical procedures in patients with inflammatory arthropathies. Scan J Rheumatol. 2011:1–8. doi: 10.3109/03009742.2010.503661. iFirst article. [DOI] [PubMed] [Google Scholar]
- 36.Sauerland S, Weiner S, Dolezolova K, et al. Mapping utility scores from a disease-specific quality of life measure in bariatric surgery patients. Value Health. 2009;12:364–370. doi: 10.1111/j.1524-4733.2008.00442.x. [DOI] [PubMed] [Google Scholar]