Abstract
The objective of this study was to assess the impact of parent attention and distraction on symptom complaints by children with and without chronic functional abdominal pain. The water load symptom provocation task was used to induce visceral discomfort in pediatric patients with abdominal pain (N = 104) and well children (N = 119), ages 8–16 years. Parents were randomly assigned and trained to interact with their children according to one of three conditions: Attention, Distraction, or No Instruction. Children's symptom complaints and parents’ responses were audiotaped and coded. Children completed a self-report measure of gastrointestinal (GI) symptoms before and after interacting with their parents. Parents’ and children's perceptions of their interaction were assessed. Compared to the No Instruction condition, symptom complaints by pain patients and well children nearly doubled in the Attention condition and were reduced by half in the Distraction condition. The effect of attention on symptom complaints was greater for female pain patients than for male patients or well children. Findings for self-report GI symptoms were similar to those for audiotaped symptom complaints. Both pain patients and well children in the Distraction condition rated parents as making them feel better compared to ratings for the Attention condition. Parents of pain patients rated distraction as having greater potential negative impact on their children than attention. Parents’ responses to children's symptom complaints can significantly increase or decrease those complaints. Girls with functional abdominal pain are particularly vulnerable to the symptom-reinforcing effects of parental attention.
Keywords: Functional abdominal pain, Attention, Distraction, Social learning, Parent–child interaction
While sympathy with joy intensifies the sum of joy in the world, sympathy with pain does not really diminish the amount of pain.
– Oscar Wilde, The Soul of Man under Socialism
1. Introduction
Chronic or recurrent abdominal pain is common among children and adolescents (McGrath, 1990). Social learning theory (Bandura, 1977; Craig, 1983) and research using self-report methods suggest that significant others may influence the course of pain in these youth (Walker et al., 1993, 2002). This study pioneered observational research on pediatric abdominal pain with a laboratory procedure – the water load symptom provocation test (WL-SPT) – that creates visceral sensations similar to those of the naturally occurring pain episodes of pediatric abdominal pain patients (Walker et al., in press). We manipulated parents’ responses to their children following the WL-SPT and examined the impact on children's symptom complaints.
Drawing on literature on operant reinforcement of pain complaints (e.g., Romano et al., 1992; Manimala et al., 2000; Flor et al., 2002; Jollife and Nicholas, 2004), we expected that parental attention to children's discomfort would be associated with significantly more symptom complaints than parent behavior intended to distract. Based on the likelihood that abdominal pain patients had a long parental reinforcement history vis-à-vis abdominal symptoms, we expected the impact of parental attention on children's symptoms to be stronger for pain patients than for well children. Moreover, based on the assumption that pain patients are used to receiving reinforcing rather than distracting responses from parents in response to their symptoms, we expected that parental behavior aimed at distraction would be unexpected and would have a weaker impact on pain patients than on well children. To test these hypotheses, parents of pain patients and well children were trained to respond to their children with attention or distraction following induction of visceral discomfort.
A third condition examined spontaneous parent behavior. In this control condition, we expected parents of pain patients to exhibit higher levels of attending and lower levels of distracting responses to their children's discomfort than parents of well children. This hypothesis was based on evidence that pediatric abdominal pain patients report more solicitous attention from their parents during illness episodes than their peers (Walker et al., 1993).
We also assessed parents’ and children's reactions to parent training. Because chronic pain is associated with attention by family members (e.g., Romano et al., 1992), we expected parents of pain patients to find it more difficult to implement distraction than attention. We further expected parents of pain patients to rate attention as having greater potential benefit and less potential negative impact on their children than distraction. Because parents of pain patients may view their children as particularly vulnerable to visceral discomfort, we expected these parents to make significantly higher ratings of their children's discomfort following water ingestion compared to parents of well children. Finally, because research has found that parents are more likely to attend to illness behavior of girls and younger children (Walker and Zeman, 1992), we also examined age and gender effects and interactions.
2. Methods
All study procedures were approved by the Medical Center's Institutional Review Board.
2.1. Participants
2.1.1. Abdominal pain patients (N = 110)
The patient sample consisted of children between 8 and 16 years of age (M = 11.46; SD = 2.11) referred to a pediatric gastroenterology clinic for evaluation of abdominal pain. Eligibility criteria included (a) at least three episodes of periumbilical or lower abdominal pain during the previous three months, (b) no chronic illness or disability, (c) living with a parent, and (d) no organic disease revealed in a medical evaluation by the pediatric gastroenterology service. Sixty percent of participants were female. The sample was 93% Caucasian, 4% African-American, 2% Asian, and 1% Hispanic. Duration of abdominal pain ranged from three months to 11 years (M = 71.95 months; SD = 194.78). Participating parents included 105 mothers (95%), 4 fathers (4%), and 1 grandparent (1%).
2.1.2. Well children (N = 120)
Participants in a public school survey of children's health were eligible for the study if they (a) reported on the survey that they had experienced no more than two episodes of abdominal pain in the past two weeks, (b) obtained a score on the Children's Somatization Inventory (Walker and Greene, 1989) below the sample median for their gender,1 and (c) by parent report, had no chronic illness or disability. Participants ranged in age from 8 to 15 years (M = 11.23; SD = 1.94) and 50% were female. The sample was 95% Caucasian, 2% African-American, 1% Asian, and 2% from other ethnic backgrounds. Participating parents included 108 mothers (90%), 8 fathers (7%), and 4 grandparents (3%). T-test and chi-square analyses revealed no demographic differences between pain patients and well children.
2.2. Recruitment
2.2.1. Patients
Parents of children scheduled for evaluation of abdominal pain at a pediatric gastroenterology clinic were identified by clinic staff and contacted by telephone several days prior to their initial clinic visit to inform them about the research and screen for eligibility. Families of children whose medical evaluation revealed no evidence of organic disease were subsequently contacted by telephone and invited to return to the medical center to participate in the present laboratory study. Of the 198 patients who met eligibility criteria, 110 (56%) returned to the medical center to participate in the laboratory study.
2.2.2. Well children
Families of children who completed a health survey in the public schools of a county adjacent to that of the medical center were contacted by telephone until the sample was filled (we contacted 189 families to obtain a sample of 120, for a participation rate of 63%).
2.3. Water load symptom provocation test
Development and validation of the WL-SPT is described elsewhere (Walker et al., in press). Adapted from a procedure used in studies of gastric motility (Koch et al., 1997), the WLSPT requires children to drink water until they feel “completely full”. They drink from a tube connected to a reservoir that is hidden from view so they do not have visual cues regarding the amount of water ingested but must rely on internal sensations to assess perceived fullness. The WL-SPT produces discomfort similar in nature but less intense than that experienced by pediatric abdominal pain patients during typical episodes of abdominal pain (Walker et al., in press).
2.4. Parent conditions
Parents were randomly assigned to one of three conditions: Attention, Distraction, or No Instruction. Parents were not aware of other conditions and children were not aware of parent training. In the Attention and Distraction conditions, parents were trained in how to interact with their child during the 5-min interaction scheduled to occur immediately after the child completed water ingestion. To justify the parent–child interaction, parents and children were told that after the child drank water the parent would keep the child company for 5 min while the child's physiological reactions were recorded (Jones et al., 2005).2
Parent training procedures were adapted from Chambers et al. (2002). First, parents viewed a videotape featuring a professional narrator and actors who presented seven vignettes of interactions between a boy and his mother following the WLSPT. For example, the boy was shown holding his abdomen and saying, “I'm so full”. The same video clips were presented in both conditions, but the mother's responses to the boy differed on videotapes for the Attention and Distraction conditions. Next, parents were given written examples of responses appropriate for their training condition, asked to highlight responses that were most natural for them, and encouraged to add their own examples. Thus, the training allowed parents to tailor responses to their natural style of communication. Finally, parents practiced their responses while viewing a videotape featuring five new vignettes of the child actor. This videotape segment differed from the original vignettes in that the actress playing the mother was not present. The tape was paused immediately after the child made a statement to allow parents to practice responding in a manner appropriate to their assigned condition. After each vignette, parents were given feedback by the Experimenter. Parents “passed” training if they responded appropriately to at least four of the five vignettes. If this criterion was not met, parents were given further instructions before responding to five additional practice vignettes.
2.4.1. Attention Condition
In the Attention Condition, parents were reminded that their children would experience some discomfort associated with water ingestion and were told, “Probably there have been times when your child was uncomfortable and you reassured him/her and gave him/her sympathy for how he/she was feeling”. Parents were asked to respond to their children in that manner during the 5 min after the WL-SPT. Specifically, they were asked to, “Keep your child focused on how his/her body is feeling, reassure your child about the discomfort he/she is feeling, apologize for his/her discomfort, and express sympathy for how full and uncomfortable he/she is feeling”. The written examples of statements they might make included: “I know it hurts now, but you'll be OK later”, “What does it feel like?”, and “I can imagine it must feel really uncomfortable”.
2.4.2. Distraction Condition
In the Distraction Condition, parents were reminded that their children would experience some discomfort associated with water ingestion and were told, “Probably there have been times when your child was uncomfortable and you distracted him/her and tried to keep his/her mind off how he/she was feeling”. They were asked to respond to their children in that manner during the 5 min after the WL-SPT. Specifically, they were asked to, “Keep your child's mind off how he/she is feeling, distract your child from the discomfort he/she is feeling, and involve him/her in a conversation about something he/she enjoys”. Written examples of statements they might make included: “Let's talk about something else to get your mind off of it. Tell me about ________” and “What would you like to do this evening?”
2.4.3. No Instruction Condition
To control for parent exposure to training materials and experimenter interaction in the training conditions, parents in the No Instruction Condition were shown a videotape about the University.
2.5. Measures
2.5.1. Gastrointestinal symptom index
A symptom checklist developed for use with the WL-SPT assessed symptoms experienced by patients in association with abdominal pain episodes (Walker et al., in press). Immediately after water ingestion and again after the parent–child interaction, children rated how much they felt each of four GI symptoms (stomachache, nausea/upset stomach, feel like throwing up, and sick) using a 5-point rating scale ranging from none (0) to a whole lot (4). Ratings were summed and averaged to create a GI Symptom Index with scores that could range from 0 to 4. Internal consistency was good (α = .87).
2.5.2. Post-Interaction Questions
Parents’ and children's perceptions of their 5-min interaction were assessed following the interaction. All parents were asked, “How much physical discomfort was your child feeling?” and “How different was what we asked you to say today from what you usually say to your child when he/she has a stomach ache or is not feeling good?” In addition, parents in the Attention and Distraction conditions were asked, “How difficult was it for you to say what you were asked to say?” and, regarding their training, “Do you think it would make your child feel better/worse if you said these things when he/she has a stomach ache at home?” Children were asked, “Did your mom or dad make you feel better/worse when you stomach was really full?” If children answered yes, they were asked “How much better/worse did she/he make you feel?” and, “Think about how your mom or dad usually acts when you don't feel good. Was she/he acting the same as usual or different than usual today?” Responses were on a 5-point scale ranging from not at all (0) to a whole lot (4).
2.6. Procedure
Two experimenters met parents and children upon arrival. The Parent Experimenter conducted informed consent procedures with the child in the parent's presence. Next, the Child Experimenter escorted the child to an adjacent room while the Parent Experimenter conducted informed consent procedures with the parent. Parents assigned to the Attention or Distraction conditions learned of the training at this time and were informed that this portion of the study was optional; no parent declined to participate. Child Experimenters were blind to parent condition and child group.
Following notification that parent training was completed, the Child Experimenter administered the WL-SPT to the child while the parent waited in the adjacent room. As soon as the child had completed the WL-SPT and GI Symptom Index, the Parent Experimenter was notified. The Parent Experimenter and parent then entered the room and the parent was asked to keep the child company for 5 min while the Experimenters attended to another task. Five minutes later, the Parent Experimenter knocked on the door and asked to see the parent. The parent returned to the original room and completed the Post-Interaction Questions. Meanwhile, the Child Experimenter administered the GI Symptom Index and Post-Interaction Questions to the child.
All verbal interactions in both rooms were audiotaped. Parents and children were aware of the use of the audio recording system and were told it was necessary to monitor the correct execution of study procedures by Experimenters.
2.7. Coding procedures and training manipulation check
2.7.1. Coding of parent–child interactions
Audiotapes of the 5-min interaction between parents and children were transcribed and coded. The coding system was a modification of the Child-Adult Medical Procedure Interaction Scoring–Revised (CAMPIS-R; Blount et al., 1997; Blount et al., 1990). For this study, codes for parents’ utterances included (1) Attending Talk, defined as any talk by the parent about the child's symptoms, (2) Distracting Talk, defined as any talk by the parent that did not focus on the child's physical sensations or WL-SPT procedure, and (3) Uncodeable Talk, which included parents’ inaudible utterances and statements about the procedures. Codes for children's utterances were (1) Symptom Complaints, which included statements about symptoms, and (2) Other Talk, which included all other utterances.
Prior to coding, transcripts were reviewed by a primary rater and divided into independent utterances that each received a single code (Yoder, 2004).3 Reliability was assessed with a secondary rater completing the same coding process for 25% of the transcripts. Due to the event-coded nature of the data, reliability calculations were computed with an intra-class correlation (Bakeman, 2000). Intra-class correlation reliability coefficients were excellent for all coding categories, ranging from .95 to .99.
2.7.2. Parent training condition manipulation check
Parents successfully completed training for the Attention and Distraction conditions if they responded appropriately to four out of five practice vignettes. Six parents who did not achieve success complied with their assigned condition during the interaction and therefore were retained in the sample.
Every parent made at least 31 utterances during the interaction. A 3 (Condition) × 2 (Group) analysis of variance (ANOVA) revealed a significant effect of condition, F(217) = 19.35, p < .001, on total number of parent utterances. Post hoc tests indicated that parents in the No Instruction condition made significantly (p < .001) fewer utterances (M = 48.82, SD = 14.37) than parents in the two training conditions, which did not different significantly from each other (Attention condition M = 59.41, SD = 15.24, p < .001; Distraction condition M = 64.22, SD = 15.63).
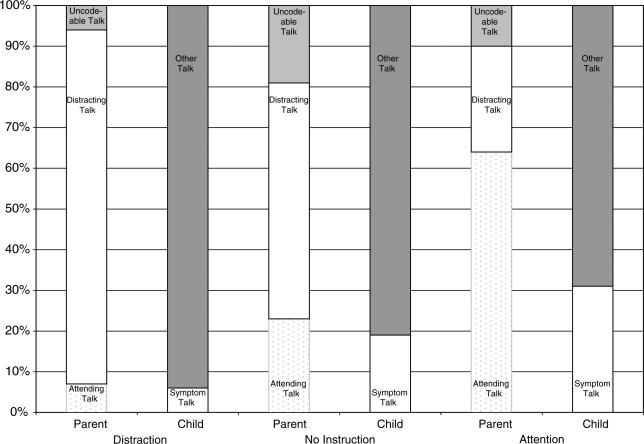
The criterion for compliance was that at least one-third of parents’ utterances during the interaction were consistent with their training condition. All parents met this criterion. Fig. 1 shows, by condition, the mean proportion of parent Attending, Distracting, and Uncodeable utterances and the mean proportion of child Symptom Complaints and Other utterances. Within each condition, there were no differences by child group or gender in the proportion of each type of parent utterance.
Fig. 1.
By condition, mean proportions of parents’ Attending, Distracting, and Uncodeable Talk, and mean proportions of children's Symptom Complaints and Other Talk.
As predicted, in the Attention and the Distraction conditions, the proportion of utterances consistent with the respective training condition was significantly greater than that in the No Instruction condition (Attention versus No Instruction condition on proportion of Attending Talk, t(147) = 19.17, p < .001; Distraction versus No Instruction condition on proportion of Distracting Talk, t(145) = 15.42, p < .001). Thus, training for the Attention and Distraction Conditions successfully manipulated parent behavior.
2.7.3. Parent- and child-rated “typical” behavior
To assess the ecological validity of the parent manipulation, parents and children rated the extent to which parents’ behavior during the interaction differed from parents’ typical behavior toward their children during times of illness. There were no significant differences by group, condition, child gender, or child age. Parents and children viewed parents’ behavior in the laboratory as no more than a little different from their typical behavior when their children were ill.
3. Results
3.1. Preliminary analyses
Seven participants were omitted due to incomplete data or deviation from the protocol, leaving a total sample of N = 223 (104 pain patients; 119 well children). Results of ANOVA and chi-square analyses revealed no significant child age or gender differences by parent training condition.
3.2. Impact of Attention and Distraction on children's symptom complaints
3.2.1. Analytic strategy for hypothesis testing
Multiple regression analyses with planned contrasts tested study hypotheses regarding linear and quadratic effects. Linear effects assessed differences between the two training conditions (Attention versus Distraction); quadratic effects compared all three conditions (Attention, Distraction, and No Instruction). The main set of contrasts examined effects of all three conditions by group (Pain, Well). Least Significant Difference (LSD) multiple comparisons were used to follow up significant effects of planned comparisons. Unplanned effects of gender and age group (less than 12 years of age; 12 years and older) were followed up with post hoc tests using the Bonferroni correction to control for multiple exploratory comparisons. The total number of children's utterances or their pre-interaction GI symptom index score was included as a covariate in analyses of children's symptom complaints and GI symptom scores, respectively.4
3.2.2. Children's vocal symptom complaints
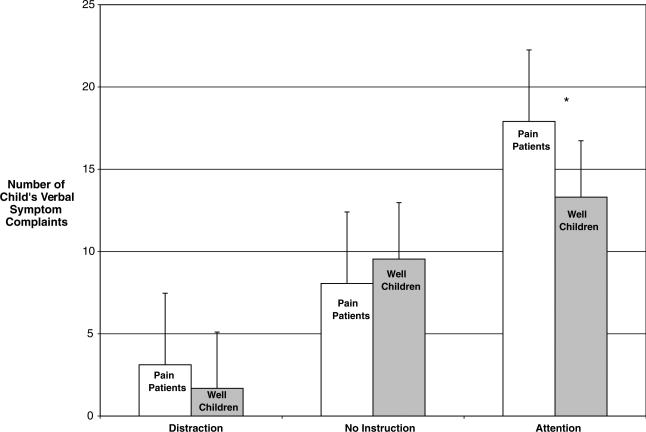
The total number of child utterances was a significant covariate, β(210) = .31, p < .001, of children's vocal symptom complaints. A significant linear effect of condition, β(210) = .69, p < .001, reflected that children in the Attention condition expressed significantly more symptom complaints (M = 15.48, SE = .59) than children in the Distraction condition (M = 2.35, SE = .61). Qualifying this main effect was the predicted quadratic interaction effect of group by condition, β(210) = –.12, p < .01 (Fig. 2). In the Attention Condition, pain patients made significantly more symptom complaints (M = 17.90, SD = .83) than well children (M = 13.31, SD = .78, p < .001). Symptom complaints by pain patients and well children did not differ in the Distraction and No Instruction conditions.
Fig. 2.
Means and standard errors for children's symptom complaints by condition and group controlling for total number of child utterances. *Significant at p < .01.
Overall, females made more symptom complaints than males, β(210) = .09, p < .05 (M = 9.64, SE = .67 for females; M = 8.12, SE = .74 for males). This gender effect was qualified by a three-way quadratic interaction of condition by group by gender, β(210) = –.12, p < .01. In the Attention condition, female pain patients made significantly more symptom complaints (p < .05) than well females and well males but did not differ significantly from male pain patients (M = 19.53, SE = .98 for female pain patients; M = 12.07, SE = 1.08 for well females; M = 14.54, SE = 1.08 for well males; M = 14.65, SE = 1.39 for male pain patients). Thus, in the Attention condition, female pain patients accounted for the observation of more symptom complaints by pain patients compared to well children. No differences in symptom complaints by group or gender were observed in the Distraction or No Instruction conditions.
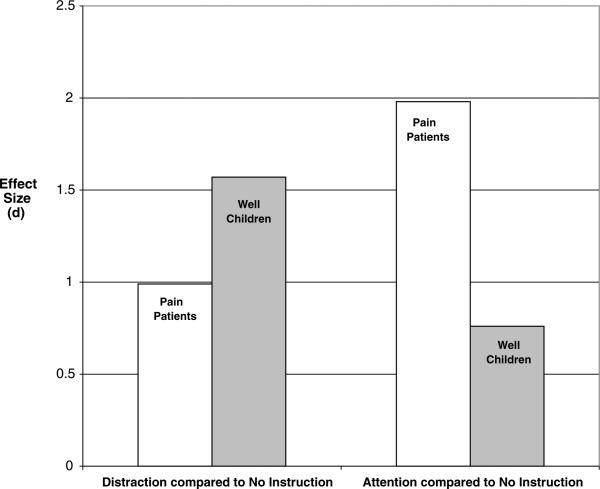
Effect sizes of parent condition on children's symptom complaints were calculated using weighted pooled standard deviation estimates across groups (Fig. 3).
Fig. 3.
Effect sizes of parent training conditions compared to the No Instruction condition on symptom complaints by pain patients and well children.
Compared to the No Instruction Condition, the Attention Condition had a large effect on symptom complaints by pain patients (d = 1.98), roughly two and a half times greater than the effect of the Attention Condition on well children (d = .76). The effect of attention on pain patients was substantially greater for female pain patients (d = 2.38) than for male pain patients (d = 1.36). Compared to the No Instruction Condition, the Distraction condition had a large effect for well children (d = 1.57) and a smaller yet sizeable effect on sympton reduction for pain patients (d = .99).
3.2.3. GI symptom index
A significant group effect, β(210) = .10, p < .05, indicated that, controlling for baseline scores, pain patients had higher GI symptom index scores (M = .63, SE = .05) following the parent–child interaction than well children (M = .47, SE = .04). This effect was qualified by the linear interaction of group by condition by gender, β(210) = –.15, p < .01, with the pattern of results similar to that for vocal symptom complaints in that the effect of parental attention on children's symptoms was strongest for female pain patients.
3.3. Spontaneous Attention and Distraction by parents in the No Instruction Condition
In the No Instruction Condition, no significant effects were found for group, gender, or child age for any category of parent utterance. However, a marginally significant gender effect, β(68) = .22, p = .052, indicated that parents made more attending statements to daughters (M = 12.59, SE = 1.01) than to sons (M = 9.70, SE = 1.03). Conversely, another marginally significant gender effect, β(68) = –.13, p = .077, indicated that parents made more distracting statements to sons (M = 29.67, SE = 1.25) than to daughters (M = 26.80, SE = 1.24).
3.4. Parent and child perceptions of Attention versus Distraction
ANOVAs examined the effects of group (Pain, Well) and training condition (Attention versus Distraction) on post-interaction assessments. Hypothesized interactions of group and gender were followed up with LSD comparisons. Unplanned effects of child age and sex were explored with Bonferroni-corrected multiple comparisons.
3.4.1. Difficulty of condition adherence
Overall, parents rated the difficulty of adhering to their training conditions as quite low (less than 1 on a 0–4 rating scale). However, as predicted, a significant interaction of group by condition, F(142) = 5.16, p < .05, indicated that among parents of well children, those in the Attention condition reported significantly more difficulty (p < .01) adhering to their condition (M = .40, SD = .55) than did those in the Distraction condition (M = .07, SD = .24). Among parents of pain patients, the reported difficulty of adherence did not differ between the Attention (M = .21, SD = .45) and Distraction conditions (M = .28, SD = .73). Within the Distraction condition, there was a trend (p = .081) for parents of pain patients to report more difficulty compared to parents of well children. No significant group differences in adherence difficulty were observed in the Attention condition.
3.4.2. Parent-rated child discomfort
As predicted, a significant group effect, F(211) = 6.35, p < .05, indicated that parents of pain patients rated their children's physical discomfort higher (M = 1.30, SD = .91) than did parents of well children (M = .96, SD = .92). In addition, a significant effect of condition, F(211) = 3.49, p < .05, reflected that parents in the Attention condition rated their children as experiencing more discomfort (M = 1.36, SD = .96) than did parents in the Distraction condition (M = .96, SD = .86, p < .05).
3.4.3. Perceived impact of Attention versus Distraction
Analysis of parents’ ratings of the potential positive impact on the child of parental behavior yielded a significant group by condition interaction, F(138) = 4.21, p < .05. Unexpectedly, post hoc analyses (p < .05) revealed that parents of well children in the Attention condition rated the potential positive impact of attention as greater (M = 2.53, SD = .93) than parents of well children in the Distraction condition rated the potential positive impact of distraction (M = 1.92, SD = 1.26, p < .05). In contrast, parents of pain patients in the Attention condition rated the positive impact of attention at a level that did not differ from ratings of the positive impact of distraction by parents of pain patients in the Distraction condition (M = 2.06, SD = 1.07, and M = 2.24, SD = 1.25), respectively.
Regarding the potential negative impact of parent behavior, a significant effect of condition, F(110) = 4.24, p < .05, indicated that parents in the Distraction condition rated distraction as having greater potential for negative impact on children (M = .52, SD = 1.00) compared to ratings of negative impact of attention made by parents in the Attention condition (M = .23, SD = .66, p < .05). As predicted, a significant interaction of group by condition, F(110) = 6.22, p < .05, qualified this main effect. Parents of pain patients in the Distraction condition rated distraction as having greater potential negative effects (p < .01) in comparison to ratings of the negative impact of attention made by parents of pain patients in the Attention condition (M = .68, SD = 1.19 for Distraction; M = .00, SD = .00 for Attention). Indeed, every parent of a pain patient rated attention as having no potential for negative impact on their children. In contrast, parents of well children did not differ in their ratings of the potential negative impact of Attention (M = .43, SD = .86) versus Distraction (M = .34, SD = .71). Within the Attention condition, there was a trend (p = .055) for parents of well children to rate attention as having greater potential negative impact compared to ratings by parents of pain patients. Ratings of negative impact did not differ between parents of pain patients versus well children in the Distraction condition.
A significant effect of group by condition by age, F(110) = 5.36, p < .05, indicated that ratings of the negative impact of distraction were significantly higher (p < .05) for parents of young pain patients in the Distraction condition (M = 1.07, SD = 1.28), compared to ratings of the potential negative impact of attention by parents of young (M = .00, SD = .00) and adolescent (M = .00, SD = .00) pain patients in the Attention condition. Thus, the pattern of findings indicated that parents of pain patients, particularly young pain patients, perceived that the potential negative effect of Distraction on their children was greater than that for Attention.
Children rated the extent to which their parents made them feel better during the interaction. A significant group effect, F(211) = 4.48, p < .05, indicated that well children gave their parents higher ratings (M = 1.79, SD = 1.26) than did pain patients (M = 1.37, SD = 1.13). A significant effect of Condition, F(211) = 4.45, p < .05, demonstrated significantly greater positive impact ratings (p < .05) by children in the Distraction condition (M = 1.93, SD = 1.21) than by children in the Attention (M = 1.45, SD = 1.18) and No Instruction conditions (M = 1.40, SD = 1.20), which did not differ significantly from each other. Finally, a significant effect of age group, F(211) = 8.12, p < .01, revealed that younger children rated the positive impact of their parents’ behavior as greater (M = 1.79, SD = 1.31) than did adolescents (M = 1.32, SD = 1.01).
Analyses for children's ratings of the extent to which their parents made them feel worse could not be conducted because only one of 223 participants, a 10-year-old pain patient whose parent was in the Distraction Condition, rated his parent as making him feel worse.
4. Discussion
Following experimental induction of visceral discomfort in abdominal pain patients and well children, manipulation of parental attention and distraction substantially influenced spontaneous symptom complaints by both groups of children during a 5-min interaction with their parents. Compared to a control condition that did not manipulate parent behavior, children's symptom complaints nearly doubled under conditions of parent attention and were reduced by half under conditions of parent distraction. Thus, we demonstrated that parent behavior has a powerful impact on children's experience of visceral discomfort. To the extent that these effects are found to generalize beyond the laboratory setting, they can inform parents’ efforts to help their children cope with one of the most common somatic symptoms of childhood.
Several potential mechanisms may explain how parent attention increased children's symptom complaints. First, parent attention may have focused children's attention on somatic sensations and rewarded expression of symptom complaints. Parent attention also may have influenced children's cognitive and emotional reactions to their discomfort, indirectly increasing the salience of the affective component of physical discomfort associated with suffering. For example, the fact that their parents expressed interest and concern may have caused children to evaluate their discomfort as more threatening. Finally, we cannot rule out the possibility that parent attention encouraged children's verbal symptom complaints but did not increase their discomfort.
Parent attention increased symptom complaints by female pain patients to a much greater extent than for male pain patients or well children. Because girls place high value on interpersonal relationships (Leadbeater et al., 1999; Little and Garber, 2004), the reinforcement value of attention to symptoms may be stronger for girls than for boys. For example, sympathy associated with attention communicates a shared representation of experience and feelings of concern for the other person (Decety and Chaminade, 2003). Thus, parent attention may be especially powerful in reinforcing girls’ symptoms if they value the caring from others associated with being in the sick role. The fact that parental attention had a stronger impact on female pain patients than on well girls may reflect the patients’ longer history of symptom reinforcement and readier acceptance of sick role status. Regardless of patient status, in contrast, boys may find parent attention to their symptoms aversive if it carries the implication that they are weak or dependent.
The control condition revealed parents’ spontaneous behavior toward children following symptom induction. Contrary to expectations, parents of pain patients and well children in this control condition did not differ in their level of attending or distracting utterances. However, our ability to detect group differences was limited by the low rate of utterances in the No Instruction condition; in the absence of instructions to interact with their children, some parents read a book or made phone calls during the 5-min period with their child. Despite the limited interaction between parents and children in the control condition, we observed a trend for parents in this condition to make more attending statements to daughters than to sons, and, conversely, more distracting statements to sons than to daughters.
We also examined parents’ perceptions of attention and distraction. The good news for clinicians is that parents of pain patients found it no more difficult to learn and to implement distraction than attention, suggesting that they could be trained to use distraction to reduce their children's symptom complaints. Parents also were asked to evaluate whether responses consistent with their training condition might have a positive or negative impact on their children if employed at home during children's illness episodes. Parents of pain patients rated attention and distraction as equally beneficial in relieving their children's discomfort, but they rated distraction as having greater potential for negative impact than attention. Moreover, unlike parents of well children, no parent of a pain patient rated attention as having any potential for negative impact on their child. This is consistent with a previous finding that parents of children with unexplained abdominal pain rarely viewed attention from family members as a factor contributing to their child's pain (Claar and Walker, 1999). Interestingly, parents of well children rated attention as more useful than distraction in making their children feel better, perhaps reflecting a culture bias that parents should attend to their children's symptoms. Thus, professionals who observe that parental attention reinforces a child's symptom complaints may have difficulty convincing parents to reduce attention to symptoms.
Children's perceptions of the effects of parental attention and distraction were consistent with empirical studies suggesting that distraction is a useful strategy to help children cope with pain (e.g., Blount et al., 1992). Both pain patients and well children rated parents in the Distraction condition as making them feel better compared to ratings by children whose parents were in the Attention condition. To our knowledge, this is the first study to evaluate children's perceptions of various types of parent responses to their discomfort. Greater parental awareness that children find distraction helpful might encourage more frequent use of distraction.
This study has a number of strengths. Manipulation of parent behavior and standard induction of child discomfort allowed us to control parent and child behavior in a way that is not possible with nonexperimental designs. Other studies of chronic pain have examined the impact of parents’ observed or reported solicitousness on patient behavior (e.g., Dunn-Geier et al., 1986; Whitehead et al., 1994; Levy et al., 2004) but none has manipulated parents’ behavior toward their children under controlled conditions. Our symptom induction procedure had high external validity, as it produces symptoms similar to those associated with naturally occurring pain episodes in children with functional abdominal pain (Walker et al., in press). The training procedures also appeared to yield ecologically valid parent behavior. Regardless of whether parents were trained in the Attention or Distraction condition, they rated their responses to their children as typical, suggesting that parents had prior experience with both types of responses and executed the experimental task in a natural way. Moreover, children rated parent behavior as normal and did not discover the parent training. Finally, we can be particularly confident in our results because findings based on audiotapes of children's spontaneous symptom complaints converged with those based on a self-report symptom questionnaire.
Several study limitations should be noted. First, the WL-SPT induced discomfort at a level below pain threshold. The relation of parental attention and distraction to children's symptom complaints might differ with a more noxious stimulus. However, Blount et al. (1989) demonstrated the impact of similar parental behaviors on children's distress in the context of bone marrow aspiration, a highly noxious medical procedure. Second, the majority of participating parents were mothers. Fathers may have a different impact on their children's symptom complaints or the impact of parent behavior may depend on whether parent and child gender match. Gender has begun to emerge as an important factor in other studies of the impact of significant others’ behavior on pain patients (e.g., Chambers et al., 2002; Filligim et al., 2003). Finally, sequential analysis of spontaneous interactions would allow stronger causal inferences and examination of reciprocal influences.
Findings from this study suggest important directions for research on the role of parent–child interaction in pediatric chronic pain. First, the finding that parental attention had a stronger impact on the symptoms of girls than boys with functional abdominal pain deserves further examination and may provide leads to why females tend to report more frequent abdominal pain than males (Adelman et al., 1995). Second, parent attention and distraction had direct, immediate effects on children's symptom complaints. Additional research is needed to assess the long-term effect of parental attention and distraction on the course of functional abdominal pain. The fact that parent behavior could be manipulated to significantly increase or decrease children's symptom complaints during a 5-min interaction suggests that repeated interactions over time could have considerable influence on children's illness behavior. The fact that distraction significantly decreased children's symptom complaints suggests that parent training in distraction may be a useful component of interventions for pediatric chronic pain. However, our findings regarding parents’ perceptions of the value of attention and distraction in alleviating children's discomfort underscore that these interventions also must address parent beliefs and treatment acceptability.
Acknowledgements
This research was supported by a grant to the investigators from the National Institute on Child Health and Development (HD23264), by a core grant (HD15052) to the John F. Kennedy Center, Vanderbilt University, by the Vanderbilt Digestive Disease Research Center (DK058404), and by Grant M01 RR-00095 to Vanderbilt University Medical Center from the National Center for Research Resources, National Institutes of Health. The authors thank the staff of the Pediatric Gastroenterology, Hepatology and Nutrition Clinic at Vanderbilt University for assistance with patient recruitment and medical evaluations. We also thank Renee Cox, Kari Freeman, Angela Profeta, Kristen Reeslund, and Kelly Voss for their contributions to data collection. Special thanks to Ronald Blount and Christine Chambers for consultation on study methods.
Footnotes
This eligibility criterion for the well sample was included to exclude children with the high levels of nonspecific somatic symptoms that are common in children with functional abdominal pain and to reduce the likelihood that the well sample would include children with types of pain (headache, chest pain, limb, and joint pain) other than abdominal pain.
Children's heart rate and galvanic skin response were assessed throughout the procedure. Preliminary results have been reported elsewhere (Jones et al., 2005).
If parent utterances fit more than one code (less than 2% of total utterances), Attending Talk was given top priority, followed by Distracting Talk and Uncodeable Talk. For child codes, Symptom Complaint was given priority over Other Talk.
Prior research had shown that amount of water consumed, time until satiation, and body mass index did not influence children's symptom levels following the WL-SPT (Walker et al., in press); therefore, these variables were not included as covariates in data analysis.
References
- Adelman AM, Revicki DA, Magaziner J, Hebel R. Abdominal pain in an HMO. Fam Med. 1995;27:321–5. [PubMed] [Google Scholar]
- Bakeman R. Behavioral observation and coding. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. Cambridge University Press; New York: 2000. [Google Scholar]
- Bandura A. Social learning theory. Prentice-Hall; Englewood Cliffs, NJ: 1977. [Google Scholar]
- Blount RL, Bachanas PJ, Powers SW, Cotter MC, Franklin A, Chaplin W, et al. Training children to cope and parents to coach them during routine immunizations: effects on child, parent, and staff behaviors. Behav Ther. 1992;23:689–705. [Google Scholar]
- Blount RL, Cohen LL, Frank NC, Bachanas PJ, Smith AJ, Manimala MR, et al. The Child-Adult Medical Procedure Interaction Scale – Revised: an assessment of validity. J Pediatr Psychol. 1997;22:73–88. doi: 10.1093/jpepsy/22.1.73. [DOI] [PubMed] [Google Scholar]
- Blount RL, Corbin SM, Sturges JW, Wolfe VV, Prater JM, James LD. The relationship between adults’ behavior and child coping and distress during BMA/LP procedures: a sequential analysis. Behav Ther. 1989;20:585–601. [Google Scholar]
- Blount RL, Sturges JW, Powers SW. Analysis of child and adult behavioral variations by phase of medical procedure. Behav Ther. 1990;21:33–48. [Google Scholar]
- Chambers CT, Craig KD, Bennett SM. The impact of maternal behavior on children's pain experiences: an experimental analysis. J Pediatr Psychol. 2002;27:293–301. doi: 10.1093/jpepsy/27.3.293. [DOI] [PubMed] [Google Scholar]
- Claar RL, Walker LS. Maternal attributions for the causes and remedies of their children's abdominal pain. J Pediatr Psychol. 1999;24:345–54. doi: 10.1093/jpepsy/24.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig KD. Modeling and social learning factors in chronic pain. In: Bonica JJ, editor. Advances in pain research and therapy. Vol. 5. Raven Press; New York: 1983. [Google Scholar]
- Decety J, Chaminade T. Neural correlates of feeling sympathy. Neuropsychologia. 2003;41:127–38. doi: 10.1016/s0028-3932(02)00143-4. [DOI] [PubMed] [Google Scholar]
- Dunn-Geier BJ, McGrath PJ, Rourke BB, Latter J, D'Astous J. Adolescent chronic pain: the ability to cope. Pain. 1986;26:23–32. doi: 10.1016/0304-3959(86)90170-3. [DOI] [PubMed] [Google Scholar]
- Filligim RB, Doleys DM, Edwards RR, Lowery D. Spousal responses are differentially associated with clinical variables in women and men with chronic pain. Clin J Pain. 2003;19:217–24. doi: 10.1097/00002508-200307000-00004. [DOI] [PubMed] [Google Scholar]
- Flor H, Knost B, Birbaumer N. The role of operant conditioning in chronic pain: an experimental investigation. Pain. 2002;95:111–8. doi: 10.1016/s0304-3959(01)00385-2. [DOI] [PubMed] [Google Scholar]
- Jollife CD, Nicholas MK. Verbally reinforcing pain reports: an experimental test of the operant model of chronic pain. Pain. 2004;107:167–75. doi: 10.1016/j.pain.2003.10.015. [DOI] [PubMed] [Google Scholar]
- Jones DS, Dufton LM, Williams SE, Walker LS. Impact of a modified water load test on gastrointestinal symptom perception and autonomic activity in children with functional abdominal pain. Gastroenterology. 2005;128(4, Suppl. 2):A-167. [Google Scholar]
- Koch KL, Bingaman S, Muth E, Ouyang A. Effects of physiological gastric distention on nausea, stomach fullness, satiety and gastric myoelectrical activity in patients with irritable bowel syndrome. Gastroenterology. 1997;112:A76. [Google Scholar]
- Leadbeater BJ, Kuperminc GP, Blatt SJ, Hertzog C. A multivariate model of gender differences in adolescents’ internalizing and externalizing problems. Dev Psychol. 1999;35:1268–82. doi: 10.1037//0012-1649.35.5.1268. [DOI] [PubMed] [Google Scholar]
- Levy RL, Whitehead WE, Walker LS, Von Korff M, Feld AD, Garner M, et al. Increased somatic complaints and health care utilization in children: effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterol. 2004;99:1–10. doi: 10.1111/j.1572-0241.2004.40478.x. [DOI] [PubMed] [Google Scholar]
- Little SA, Garber J. Interpersonal and achievement orientations and specific stressors predict depressive and aggressive symptoms. J Adolesc Res. 2004;19:63–84. [Google Scholar]
- Manimala MR, Blount RL, Cohen LL. The effects of parental reassurance versus distraction on child distress and coping during immunizations. Child Health Care. 2000;29(3):161–77. [Google Scholar]
- McGrath PA. Pain in children: nature, assessment, and treatment. Guilford; New York: 1990. [Google Scholar]
- Romano JM, Turner JA, Friedman LS, Bulcroft RA, Jensen MP, Hops H, et al. Sequential analysis of chronic pain behaviors and spouse responses. J Consult Clin Psychol. 1992;60:777–82. doi: 10.1037//0022-006x.60.5.777. [DOI] [PubMed] [Google Scholar]
- Walker LS, Claar RL, Garber J. Social consequences of children's pain: when do they encourage symptom maintenance? J Pediatr Psychol. 2002;27:689–98. doi: 10.1093/jpepsy/27.8.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LS, Garber J, Greene JW. Psychological correlates of recurrent abdominal pain: a comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. J Abnormal Psychol. 1993;102:248–58. doi: 10.1037//0021-843x.102.2.248. [DOI] [PubMed] [Google Scholar]
- Walker LS, Greene JW. Children with recurrent abdominal pain and their parents: more somatic complaints, anxiety, and depression than other patient families? J Pediatr Psychol. 1989;14:231–43. doi: 10.1093/jpepsy/14.2.231. [DOI] [PubMed] [Google Scholar]
- Walker LS, Williams SE, Smith CA, Garber J, Van Slyke DA, Lipani TA, et al. Validation of a symptom provocation test for laboratory studies of abdominal pain and discomfort in children and adolescents. J Pediatr Psychol. doi: 10.1093/jpepsy/jsj062. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LS, Zeman JL. Parental response to child illness behavior. J Pediatr Psychol. 1992;17:49–71. doi: 10.1093/jpepsy/17.1.49. [DOI] [PubMed] [Google Scholar]
- Whitehead WE, Crowell MD, Heller BR, Robinson JC, Schuster MM, Horn S. Modeling and reinforcement of the sick role during childhood predicts adult illness behavior. Psychosom Med. 1994;56:541–50. doi: 10.1097/00006842-199411000-00010. [DOI] [PubMed] [Google Scholar]
- Yoder P. Communication coding manual. Unpublished manuscript. Vanderbilt University. 2004 [Google Scholar]