Abstract
Background and the Purpose of the Study
Patients undergoing high-dose chemotherapy for hematological malignancies are susceptible to development of oral mucositis, and no effective modality has been reported for its prophylaxis and treatment. The aim of this study was to evaluate the effectiveness of zinc mouthwash on chemotherapy-induced oral mucositis lesions.
Methods
In this double-blind randomized trial, patients under chemotherapy for acute leukemia were divided into two test and control groups of 15 patients each. The groups were homogeneous with respect to medical history, tumor characteristics, and therapeutic details. The test group received 10ml 0.2% zinc sulfate mouthwash, and the control group received 10ml 0.2% chlorhexidine gluconate mouthwash, twice a day for a period of two weeks. Spijkervet scale was used to grade the severity of mucositis at every other week during eight weeks. The severity scores were analyzed with repeated measure ANOVA using SPSS 13.0 computer software.
Results
Mean severity scores were generally lower in the test group compared to the controls at all four time intervals evaluated; but only, the differences in weeks of 2 and 3 were statistically significant (P=0.025).
Conclusion
Zinc mouthwash used in conjunction with chemotherapy may reduce the severity of oral mucositis lesions in patients with leukaemia.
Keywords: Hematological malignancies, Oral hygiene, Palliative care
INTRODUCTION
Oral mucositis is a condition characterized by damages to the epithelium of the oral cavity, pharynx, and gastrointestinal tract from chemical irritations, radiation therapy, or chemotherapy for a hematological malignancy (1). Many protocols have been proposed to prevent or reduce the severity of oral mucositis, but no treatment modality is yet known to be a definite prophylactic agent (2).
Although chlorhexidine gluconate mouthwash is traditionally used in patients with oral mucositis, there is little evidence to recommend it as a gold standard. While some reports indicate positive effects of chlorhexidine mouth rinse on oral mucositis, recent studies have found either no effect or even negative effects (3). The bitter taste, dental pigmentation, dysgeusia, and unpleasant sensation experienced together with ineffectiveness provide sufficient reasons for recommending an alternative to the chlorhexidine mouthwash (4). Among medications with wound healing effects, zinc sulphate seems to be one of the promising agents in mucositis prevention (5). Zinc is an essential cofactor in various cellular processes such as DNA synthesis, RNA polymerase and reverse transcriptase, and has effects on wound healing, growth and immunity. The growth and reproductive effects of zinc are related to its influences on DNA synthesis, protein synthesis, and cell division (6).
Considering the effects of zinc on re-epithelialization and wound healing, the aim of this study was to evaluate the effectiveness of a zinc-containing mouthwash on chemotherapy-induced oral mucositis, in comparison with chlorhexidine gluconate mouthwash as control.
MATERIAL AND METHODS
In this double-blind randomized study, patients were selected from those with acute leukemia under chemotherapy in the oncology ward of Shahid Gazi Hospital in Tabriz, Iran. Patient data including age, gender, the history of chemotherapy, the dose of the drug, and any known allergy to mouthwashes were recorded by means of a questionnaire. Patients under chemotherapy on the basis an established treatment plan for acute myeloid leukemia (Cytarabine in the induction phase, and Novantrone in the consolidation phase) were included in this study. Exclusion criteria included age<15 years old, any systemic disease with other diagnosis of malignancies or chemotherapy-induced oral mucositis, any oral ulcers and mucosistis developed before starting chemotherapy, known allergy to zinc-containing or chlorhexidine mouthwashes. All probable risks and benefits of the study were explained to the patients/guardians. Upon inclusion in the study, subjects gave written informed consents. The study protocol was approved by the Research Ethics Committee at Tabriz University of Medical Sciences.
A total of 30 patients were selected, and matched with respect to medical history, tumor characteristics, and therapeutic details. Subjects were allocated to experimental and control groups of 15 patients each. The required dilution of (0.2%) zinc sulphate and chlorhexidine gluconate mouthwashes were prepared in the department of Medicinal Chemistry, Faculty of Pharmacy, Tabriz University of Medical Sciences, Tabriz, Iran. Patients were instructed to rinse with 10 ml of 0.2% zinc sulphate mouthwash two times par day for 14 days in the experimental group, and with10 ml of 0.2% chlorhexidine mouthwash in the same manner in the control group. The mouthwashes were coded with ‘A’ and ‘B’ letters on the bottles, and the investigator as well as the subjects were blinded to the type of the mouthwash which was administered to the groups by a simple random method.
All patients were examined every other week for during eight weeks. The efficacy of the treatment at each session was determined by recording the length (E) of the lesion, measured by a digital caliper, and its severity (K), based on local signs, according to the Spijkervet scale (7). Eight distinguishable irradiated areas of the mouth including buccal mucosa (left & right), soft and hard palate, dorsum and border of the tongue (left & right) and the mouth floor were evaluated (Table 1). The score of each area was defined as the product of the length and severity score. The mucositis score α in each individual was defined as the mean of the scores assigned to the evaluated areas, and ranged from 0 to 16.
Table 1.
Scores of the local signs (K) and the lengths (E) of the oral mucositis lesions used in mucositis score α (from Spijkervet et al. (7)).
| Local sign | K | Length | E |
|---|---|---|---|
| No mucositis | 0 | – | |
| White discoloration | 1 | 1≤cm | 1 |
| Erythema | 2 | 1–2 cm | 2 |
| Pseudomembranes | 3 | 2–4 | 3 |
| Ulceration | 4 | >4 cm | 4 |
Independent t-test was used to reveal any probability of differences between groups in the baseline. The mucositis score changes for the two groups during the four weeks were compared using the repeated measure ANOVA. Statistical significance level was set at p<0.05. The data were analyzed using SPSS 13.0 computer software.
RESULTS AND DISCUSSION
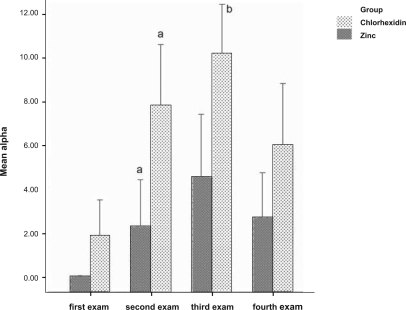
All 30 patients completed the course of study. There were no significant difference between the case and control groups in the first week (p=0.124). The trend of changes in the assessed oral mucositis index during the course of the study were similar in both groups. As shown in figure 1, the mean α index in both groups increased from first week to the third week, and then decreased in fourth week. Although mean α index was generally lower in the test group compared to the controls at all four time intervals evaluated, repeated measure ANOVA revealed that the difference was statistically significant in weeks 2 and 3 (P=0.025).
Figure 1.
Mean mucositis score (α) in the case and control groups which were examined every other week. Identical letters denote statistically significant differences (p<0.0.5).
The findings of the present study provide preliminary evidence for the effect of zinc on oral mucositis. Although zinc acts as an antioxidant which protects cell membranes against injury from free radicals and can be effective during the initiation and message generation phases of a mucositis lesion (5, 6), its effect during the healing phase is unknown. In the week 4 of the present study, zinc did not have a significant effect on the lesions in comparison with the control. The results of a similar study on the efficacy of topical phenytoin on oral mucositis also did not eventually show a significant difference (8). It could be hypothesized that, at final stages of the treatment, the prophylactic agent should be administered at a higher concentration or at closer intervals. Oral administration of the drug could also be considered, although it would entail the assessment of the serum level of the medication.
In the present study, a lower severity of oral mucositis was found in the patients receiving zinc-containing mouthwash, which is in accordance with the findings of previous studies (9, 10). Confluent mucositis was also reported to improve fast in the zinc sulfate group in comparison to the placebo group (9). Lin et al. (10) have reported that zinc supplementation in conjunction with radiotherapy postponed the development of severe mucositis in patients with oral cancers (10).
Chlorhexidine, as an oral rinse, has been also evaluated in several randomized clinical trials for preventing oral mucositis (4). A meta-analysis, however, has shown no effect for chlorhexidine in the prevention of mucositis in patients under chemotherapy and radiotherapy (2). The results of the present study also showed relatively higher scores of oral mucositis in patients receiving chlorhexidine mouthwash, compared to those using the zinc-containing mouthwash. This indicates that chlorhexidine may not be a suitable agent in the prevention of oral mucositis in predisposed individuals.
In conclusion, zinc sulfate was found to be beneficial in reducing the severity of chemotherapy-induced oral mucositis and might be indicated as a therapeutic option in cancerous patients under chemotherapy and/or radiotherapy. These results should be confirmed by additional randomized studies with larger numbers of patients.
ACKNOWLEDGEMENT
The study was supported by the vice chancellor for research, Tabriz University of Medical Sciences.
REFERENCES
- 1.Volpato LE, Silva TC, Oliveira TM, Sakai VT, Machado MA. Radiation therapy and chemotherapy-induced oral mucositis. Braz J Otorhinolaryngol. 2007;73:562–568. doi: 10.1016/S1808-8694(15)30110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stokman MA, Spijkervet FK, Boezen HM, Schouten JP, Roodenburg JL, de Vries EG. Preventive intervention possibilities in radiotherapy- and chemotherapy-induced oral mucositis: Results of meta-analyses. J Dent Res. 2006;85:690–700. doi: 10.1177/154405910608500802. [DOI] [PubMed] [Google Scholar]
- 3.Imfeld T. Chlorhexidine-containing chewing gum. J Schwiz Monatsschr Zahnmed. 2006;116:467–483. [PubMed] [Google Scholar]
- 4.Potting CM, Uitterhoeve R, Op Reimer WS, Van Achterberg T. The effectiveness of commonly used mouthwashes for the prevention of chemotherapy-induced oral mucositis: a systematic review. Eur J Cancer Care. 2006;15:431–439. doi: 10.1111/j.1365-2354.2006.00684.x. [DOI] [PubMed] [Google Scholar]
- 5.Yanagisawa H. Zinc deficiency and clinical practicevalidity of zinc preparations. Yakugaku Zasshi. 2008;128:333–339. doi: 10.1248/yakushi.128.333. [DOI] [PubMed] [Google Scholar]
- 6.Oberleas D, Harland BF. Treatment of zinc deficiency without zinc fortification. J Zhejiang Univ Sci B. 2008;9:192–196. doi: 10.1631/jzus.B0710632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spijkervet FK, van Saene HK, Panders AK, Vermey A, Mehta DM. Scoring irradiation mucositis in head and neck cancer patients. J Oral Pathol Med. 1989;18:167–171. doi: 10.1111/j.1600-0714.1989.tb00756.x. [DOI] [PubMed] [Google Scholar]
- 8.Baharvand M., Sarrafi M., Alavi K., Jalali Moghaddam E. Efficacy of topical phenytoin on chemotherapy-induced oral mucositis; a pilot study. DARU. 2010;18:46–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Ertekin MV, Tekin SB, Erdogan F, Karslioglu I, Gepdiremen A, Sezen O, Balci E, Gündogdu C. The effect of zinc sulphate in the prevention of radiation-induced dermatitis. J Radiat Res. 2004;45:543–548. doi: 10.1269/jrr.45.543. [DOI] [PubMed] [Google Scholar]
- 10.Lin LC, Que J, Lin LK, Lin FC. Zinc supplementation to improve mucositis and dermatitis in patients after radiotherapy for head-and-neck cancers: a double-blind, randomized study. Int J Radiat Oncol Biol Phys. 2006;65:745–750. doi: 10.1016/j.ijrobp.2006.01.015. [DOI] [PubMed] [Google Scholar]