Abstract
Despite the high co-occurrence of alcohol consumption and gambling, few studies have investigated alcohol use changes during gambling treatment. Using latent growth modeling, we examined weekly alcohol use trajectories of treatment-seeking pathological gamblers across 36 weeks, allowing rates of change to differ across the 12-week pre-treatment, during treatment, and post-treatment periods. For these secondary data analyses, we retained drinking gamblers (N = 163) from a combined sample of two randomized clinical trials for the treatment of pathological gambling. Results indicated a decrease in alcohol use corresponding with treatment entry and maintenance of less drinking during treatment and post-treatment. Despite these decreases in alcohol use overall, 31% (50 of 163) of participants exhibited risky drinking during the treatment or post-treatment periods. Gender, age, at-risk drinking (at any point in the 36-week interval), baseline gambling severity, treatment condition, and gambling during treatment predicted latent alcohol use growth factors. Although entry into gambling treatment was temporally associated with reductions in alcohol use in this retrospective analysis, a substantial portion of the sample exhibited at-risk drinking after treatment entry, suggesting that interventions targeting reductions in alcohol use may be useful for this population.
Keywords: Pathological gambling, treatment, alcohol use, at-risk drinking
Gambling and alcohol use disorders commonly co-occur. Nationally representative samples suggest that 45% to 73% of pathological gamblers have lifetime alcohol use disorders (Cunningham-Williams, Cottler, Compton, & Spitznagel, 1998; Petry, Stinson, & Grant, 2005). Among treatment-seeking pathological gamblers, comorbidity is also high, with 59% reporting lifetime histories of alcohol use disorders (Kausch, 2003). Despite the high comorbidity rates of these disorders, few studies have examined if drinking changes during gambling treatment.
Not only are gambling and substance use disorders frequently comorbid (Kessler et al., 2008), but the behaviors tend to co-occur. Among non-pathological gamblers, up to 80% reported consumption of 4 to10 alcohol drinks during their last gambling episode (Baron & Dickerson, 1999), and those who drank while gambling tended to gamble in more risky ways and experienced more negative consequences of gambling (Cronce & Corbin, 2010; Giacopassi, Stitt, &Vandiver, 1998). The drinking pattern reported in Baron and Dickerson’s (1999) study suggests that a large majority of non-pathological gamblers are risky drinkers (>4 drinks per day for males, >3 drinks per day for females; National Institute of Alcohol Abuse and Alcoholism [NIAAA], 2007). At-risk drinking rates are also high among individuals with gambling problems. Abbott, Williams, and Volberg (2004) reported 40% to 54% of problem and pathological gamblers identified in a community survey engaged in risky drinking, and Smith and colleagues (2010) estimated 31% of treatment-seeking gamblers were risky drinkers.
The high rates of drinking among non-pathological gamblers (Baron & Dickerson, 1999) as well as among individuals who have developed gambling-related problems (Abbott et al., 2004; Smith et al., 2010) are concerning given that quantity of alcohol use appears to be related to severity of gambling problems. In a large statewide survey, Blankenship, Starling, Woodall, and May (2007) found that gamblers reporting 3 or more alcohol drinks per occasion were more likely to endorse problem gambling behaviors than those who consumed 1 or 2 drinks per occasion. Using national epidemiological data, French, MacLean, and Ettner (2008) also found an association between severity of gambling problems and alcohol consumption, with the strength of the relationship increasing as alcohol use increased. In addition, Abbott et al. (2004) reported that hazardous alcohol use predicted continued difficulties with gambling over a 7-year period among individuals with problem and pathological gambling.
With repeated pairings of the behaviors, gambling situations may become conditioned cues for drinking. In a laboratory study, Stewart and colleagues (2002) found that participants randomized to a condition in which they could gamble were more likely to purchase and consume alcoholic drinks than participants randomized to a non-gambling control activity. Those who drank alcohol during the laboratory gambling situation reported histories of more frequent gambling, more years gambling, and more gambling-related problems compared to those who did not consume any alcohol when randomized to the laboratory gambling situation. A study by Zack and colleagues (2005) examined implicit associations between gambling and alcohol. The results suggested that positive gambling words (i.e., winning) activated alcohol-related semantic networks for gamblers who reported drinking in response to gambling wins, and that this association was stronger for those with more severe alcohol problems. If gambling becomes a conditioned cue for alcohol use as these studies suggest, then the absence of, or a reduction in, gambling during the course of gambling treatment may result in lower drinking as well.
Theoretical conceptualizations of behavior change can also be useful in explaining why two behaviors, such as alcohol use and gambling, may decrease in close temporal proximity. The decision to seek treatment for one problem behavior may spur thinking about changes in other domains. Hall and Rossi (2008) found a high degree of similarity in decision-to-change processes across 48 health behaviors. This similarity in decision processes may facilitate the spread of change to other behaviors recognized as unhealthy once primary behavior change begins. Noar and colleagues (2008) frame these changes using a hierarchical model of health behavior attitudes and behaviors. Attitudes toward change of multiple health behaviors are united under a global construct of general health orientation. In this model, change in the higher-order health behavior orientation (e.g., “I need to be more healthy”) may produce multiple individual health behavior attitude changes (e.g., “I need to change smoking, gambling, and alcohol use”) that in turn cascade down to changes in attitudes toward specific behaviors (e.g., “I should stop smoking, only gamble moderately, and stop at two drinks”). These specific attitudes may ultimately produce change in their respective behaviors. Although treatment-seeking gamblers may present to treatment for gambling, they may also be open to changes in multiple health behavior attitude domains, as driven by the higher-order health orientation construct.
A contrasting perspective is that of symptom substitution. A concern during the treatment of addictions (Kadden, Litt, Kabela-Cormier, & Petry, 2009), symptom substitution involves switching one substance for another during treatment. Given the strong associations between alcohol and gambling highlighted above, and behavioral and biological similarities across addictive disorders (Petry, 2006, 2007a; Potenza, 2006; Shaffer et al., 2004), symptom substitution (increased alcohol use while attempting to decrease gambling) is a viable hypothesis.
Two studies (Toneatto, Skinner, & Dragonetti, 2002; Stinchfield, Kushner, & Winters, 2005) examined the percent of pathological gamblers who drank before and after gambling treatment. Toneatto et al. (2002) found similar rates of self-reported past-month alcohol use (yes/no) at study intake (55.4%) and at a 1 year follow-up (50.6%). Stinchfield and colleagues (2005) categorized treatment-seeking pathological gamblers as never, less than monthly, monthly, weekly, and daily drinkers at baseline and at a 6-month follow-up. Participants evidenced lower drinking levels between baseline and post-treatment follow-up, with the greatest reduction occurring in the initially highest frequency drinkers (e.g., 54% moved from weekly or daily drinking to monthly or less drinking). These results (Toneatto et al., 2002; Stinchfield et al., 2005) do not support symptom substitution, but neither study examined alcohol use during the treatment period. The lack of during treatment assessment of alcohol use limits our ability to understand drinking behavior during gambling treatment, as alcohol use can fluctuate greatly between pre- and post-treatment periods. Additionally, although the Stinchfield et al. (2005) study noted drinking frequency reductions following gambling treatment, neither study examined quantity of alcohol use. Given that many gamblers drink at binge levels (Abbott et al., 2004; Baron & Dickerson, 1999; Smith et al., 2010) and that two large-scale studies identified associations between problem gambling and quantity of alcohol consumed (Blankenship et al., 2007; French et al., 2008), studies that examine drinking quantity may provide a more detailed picture of changes in alcohol use among individuals seeking gambling treatment.
The present study used longitudinal data of drinking behavior over 36 weeks to understand more fully the drinking patterns among treatment-seeking pathological gamblers. We assessed drinking behavior prior to treatment (12 weeks), during treatment (12 weeks), and following gambling treatment (12 weeks). Using weekly estimates of drinking quantity (in standard drinks per week), this study provides a more dynamic and thorough view of drinking behavior in relation to gambling treatment relative to prior studies. Given initial results from the Toneatto et al. (2002) and Stinchfield et al (2005) studies, we hypothesized that drinking behavior for the overall sample would remain the same or decrease during gambling treatment.
Method
Two randomized clinical trials of psychotherapy for pathological gambling (Petry et al., 2006; Petry, 2010) provided data for the current analyses. We combined data from the two studies in order to achieve a sufficient number of drinking gamblers and to increase power for planned analyses. The Petry et al. (2006) study evaluated the efficacy of individual, therapist-delivered cognitive-behavioral treatment (CBT) for pathological gambling in comparison to (1) a referral to Gamblers Anonymous (GA) only and (2) a referral to GA plus CBT workbook (with no therapist contact). The Petry (2010) study compared individually-delivered CBT to the same CBT plus contingency management reinforcing engagement in non-gambling social activities. Both studies (Petry et al., 2006; Petry, 2010) used the same inclusion and exclusion criteria, as well as the same materials, format, intensity, and duration. With the exception of greater education among those in the Petry (2010) study, participants in the two studies did not differ in basic demographic characteristics, lifetime gambling severity, recent gambling frequency or intensity, proportion of drinkers, or proportion of risky drinkers. For the current analyses, we used data collected with the same instruments and at the same time points in both studies.
Participants
Recruitment occurred via media announcements targeting those who experience problem gambling. Callers completed a phone screen to establish whether they met Diagnostic and Statistical Manual for Mental Disorders (DSM-IV; American Psychological Association, 1994) criteria for pathological gambling. We excluded individuals if they 1) had a less than 5th grade reading ability, 2) had current severe and uncontrolled psychiatric symptoms (psychosis or suicidality), or 3) were already receiving treatment for pathological gambling. Research assistants invited callers with pathological gambling and recent gambling activity for an in-person intake assessment. Participants provided informed consent, as approved by the university’s Institutional Review Board.
From a combined sample total of 333 participants, we excluded 40 cases missing all post-intake alcohol data, leaving 293 cases. The 40 deleted cases were younger and tended to drink more heavily when drinking (ps < .05), although drinking frequency was similar between groups. The groups were otherwise similar in terms of study, treatment condition, basic demographics, and gambling severity, frequency, and intensity (ps > .05). From these 293 participants, we retained the cases (56%, 163/293) with any alcohol consumption reported in the 36-week period under consideration. Subsequent analyses are limited to these 163 drinking gamblers who drank at least one alcoholic drink at any point during the 36-week period under consideration.
To characterize drinking patterns, we classified participants according to whether they met criteria for at-risk drinking at any time during the 36-week period. We refer to this classification as “ever risky drinkers” throughout the remainder of the paper. Ever at-risk drinking was defined using the NIAAA guidelines (2007) of >14 standard drinks per week or >4 per day for males, and >7 drinks per week or >3 per day for females. Forty-seven percent (76/163) of the drinking gamblers reported drinking at or above the NIAAA at-risk drinking guidelines on one or more occasions during the 36-week study period. For these ever risky drinkers, the number of weeks of risky drinking (by either daily or weekly criteria) ranged from 1 to 36 weeks, with a median of 4 risky drinking weeks (IQR = 1–12.75; M = 8.2, SD = 9.5).
Table 1 presents baseline descriptive data for ever risky (n = 76) and nonrisky (n = 87) drinkers in our sample of drinking pathological gamblers. Ever risky drinkers were younger, more often male, had more lifetime gambling and alcohol-related problems, and, as expected, drank more heavily (frequency and quantity) than their nonrisky drinking peers.
Table 1.
Descriptive Characteristics for Ever Risky and Nonrisky Drinking Pathological Gamblers
| Descriptive Variables | Risky Drinkers (n = 76) |
Nonrisky Drinkers (n = 87) |
Statistic | p |
|---|---|---|---|---|
| Study (%) | Χ2(1) = 3.61 | .06 | ||
| Petry et al. (2006) | 79 | 66 | ||
| Petry et al. (2010) | 21 | 34 | ||
| Treatment Condition (%) | Χ2(3) = 6.59 | .09 | ||
| GA Referral Only | 21 | 15 | ||
| GA + Workbook | 29 | 23 | ||
| GA + CBT | 42 | 40 | ||
| GA + CBT + CM | 8 | 22 | ||
| Ethnicity (%) | FET = 4.27 | .12 | ||
| Caucasian | 82 | 91 | ||
| African American | 12 | 3 | ||
| Other | 7 | 6 | ||
| Marital Status (%) | FET = 6.37 | .09 | ||
| Single | 41 | 24 | ||
| Married/remarried | 40 | 42 | ||
| Divorced, separated, widowed | 17 | 28 | ||
| Partnered (not married) | 2 | 6 | ||
| Male (%) | 71 | 56 | Χ2(1) = 3.78 | .05 |
| Age | 40.4 (11.1) | 48.9 (11.1) | t(161) = 4.88 | <.001 |
| Years Education | 12.5 (1.8) | 12.5 (1.8) | t(161) = 0.25 | .80 |
| Median Past Year Earned Income (IQR) |
$27K ($11–47) | $31K ($10–50) | z = −0.32 | .75 |
| SOGS Scores Lifetime | 13.1 (3.4) | 12.1 (3.5) | t(161) = −1.96 | .05 |
| Baseline Gambling (Past 60 Days) | ||||
| Days Gambled | 23.0 (17.4) | 20.5 (17.2) | t(161) = −0.93 | .35 |
| Median Dollars (IQR) | $2973 ($1096–7550) |
$3620 ($1504–9900) |
z = −0.94 | .35 |
| Pre-treatment Drinking Behavior | ||||
| Drinking Weeks (Out of 12) | 6.6 (4.4) | 4.6 (4.6) | t(161) = −2.74 | <.001 |
| Drinking Days (Out of 84) | 21.3 (25.9) | 8.4 (14.8) | t(116) = −3.83 | <.001 |
| Drinks per Drinking Day | 5.0 (3.9) | 1.5 (0.6) | t(71) = −7.37 | <.001 |
| Baseline ASI Scores | ||||
| Medical | 0.26 (0.29) | 0.36 (0.34) | t(161) = 1.86 | .07 |
| Employment | 0.24 (0.27) | 0.24 (0.25) | t(160) = −0.05 | .96 |
| Gambling | 0.68 (0.21) | 0.68 (0.19) | t(161) = 0.08 | .94 |
| Alcohol | 0.17 (0.17) | 0.06 (0.07) | t(97) = −5.64 | <.001 |
| Drug | 0.02 (0.07) | 0.01 (0.03) | t(103) = −1.47 | .15 |
| Legal | 0.07 (0.17) | 0.04 (0.12) | t(130) = −1.24 | .22 |
| Family/Social | 0.26 (0.21) | 0.22 (0.21) | t(161) = −1.29 | .20 |
| Psychiatric | 0.28 (0.21) | 0.27 (0.21) | t(161) = −0.28 | .78 |
Note. Values presented are means (standard deviations) unless otherwise specified. Changes in ttest degrees of freedom reflect use of corrections for unequal variance between groups with the exception of ASI Employment (1 missing case). GA = Gamblers Anonymous, CBT = Cognitive Behavioral Therapy, CM = Contingency Management, SOGS = South Oak Gambling Screen, ASI = Addiction Severity Index, FET = Fisher’s Exact Test. IQR = Inter-quartile range.
Measures/Procedures
Baseline measures
The South Oaks Gambling Screen (SOGS; Lesieur & Blume, 1987; Stinchfield, 2002) assessed severity of gambling problems, with scores of 5 and higher indicating probable lifetime pathological gambling. Research assistants administered the Addiction Severity Index (ASI; McLellan et al., 1988; Lesieur & Blume, 1992; Petry, 2003) at baseline. ASI scores indicate problem severity in eight domains of functioning: medical, employment, legal, alcohol, drug, family/social, psychological, and gambling. Scores range 0–1 for each domain, with scores closer to 1 indicating greater severity. Petry (2003, 2007b) found the ASI to be reliable and valid in assessing severity of problems among pathological gamblers. We used the Gambling Timeline Followback Method (G-TLFB; Weinstock, Whelan, & Meyers, 2004) to measure self-reported gambling frequency and intensity (dollars spent) at baseline and at study follow-ups. The G-TLFB has good reliability and validity for the measurement of gambling behavior (Hodgins & Makarchuk, 2003; Petry, 2003; Weinstock et al., 2004).
Alcohol data
At intake, participants provided self-reported alcohol quantity and frequency data (in standard drinks) for the 90 days preceding treatment entry using the timeline followback (TLFB; Sobell & Sobell, 1992). For the present analyses, we focused on alcohol consumption quantity rather than frequency given evidence suggesting a stronger link with gambling behavior for the former (Blankenship et al., 2007) and the ability to detect more detailed changes in alcohol use (e.g., changes in quantity even if frequency remains stable). At about 8 and 24 weeks post-intake, we again collected alcohol consumption data using the TLFB retrospectively back to the date of the last visit. The resulting data record for each case had up to 36 continuous weeks of daily alcohol data spanning the 12 weeks preceding treatment entry through 24 weeks post-study intake.
Treatment Conditions
In all treatments, the primary focus was gambling. Generally, study therapists did not emphasize alcohol or other substance use unless the participant initiated discussion of substance use. We randomized participants to a treatment condition using a computerized urn procedure, balancing for gambling severity and demographics (e.g., age, gender). Treatment duration was eight sessions, but we allowed 12 weeks from the date of intake to complete treatment.
Referral to GA alone
In a brief, 15-minute meeting, study therapists recommended GA, provided a list of times and locations for meetings throughout the state of Connecticut, discussed potential barriers to attendance, and encouraged participants to select a meeting to attend. Participants did not meet with study therapists again for the remainder of the study.
Referral to GA plus a cognitive-behavioral based workbook
In addition to the GA referral, participants received an extensive workbook (Petry, 1998) paralleling the content and activities of the in-person CBT format (see below), with instructions to complete one chapter each week. No additional therapy contact occurred for the remainder of the study.
Referral to GA plus individual CBT sessions
In addition to a GA referral, participants completed eight, 50-minute individual sessions with a study therapist. Petry (2005) describes the therapy topics, handouts, and homework assignments. Briefly, the therapy materials concerned understanding gambling behavior (triggers, functional analysis), increasing alternate activities, coping and refusal skills, challenging irrational thinking, and relapse prevention.
Referral to GA plus individual CBT session plus contingency management
In addition to the GA referral and individual CBT therapy, participants could earn up to $187 in vouchers over the course of the study for engaging in up to three non-gambling social activities (e.g., GA meetings, volunteering, going to the movies or dinner with non-gambling family or friends, etc.) per week. Participants exchanged the earned vouchers for retail goods and services.
Data Analysis
We calculated weekly alcohol intake totals (in standard drinks) from the daily TLFB data for each participant, and we log-transformed these weekly data to improve normality of the distributions. If a participant was missing one day or more of TLFB alcohol data in a given week, we considered that week missing. Overall, follow-up rates for these 163 drinking gamblers were 90% for the 8-week evaluation and 88% for the 24-week follow-up. Of the 163 drinking gamblers, 140 (86%) had complete data (36 weeks of TLFB data). The number of missing weeks (M = 1.33, SD = 4.0) of TLFB alcohol data ranged from 0 to 21 weeks out of the 36-week span under consideration, with only 6% (9/163) of the sample missing more than 10 weeks out of 36.
We examined trajectories of weekly alcohol consumption using a series of latent growth models with full information maximum likelihood (FIML) estimation. FIML uses all available data and does not exclude cases with missing data (Kline, 2005). FIML assumes data are missing at random (MAR: Kline, 2005), an assumption that is not testable directly (Allison, 2003). With the exception of a significant association between missing data status and study, those with versus without missing data did not differ in terms of age, gender, ever at-risk drinking status, gambling severity, pre-treatment gambling frequency or dollar amount, treatment group, or gambling frequency or dollar amount during treatment (ps > .05). Based on these comparisons, we believed the MAR assumption to be reasonable for these data.
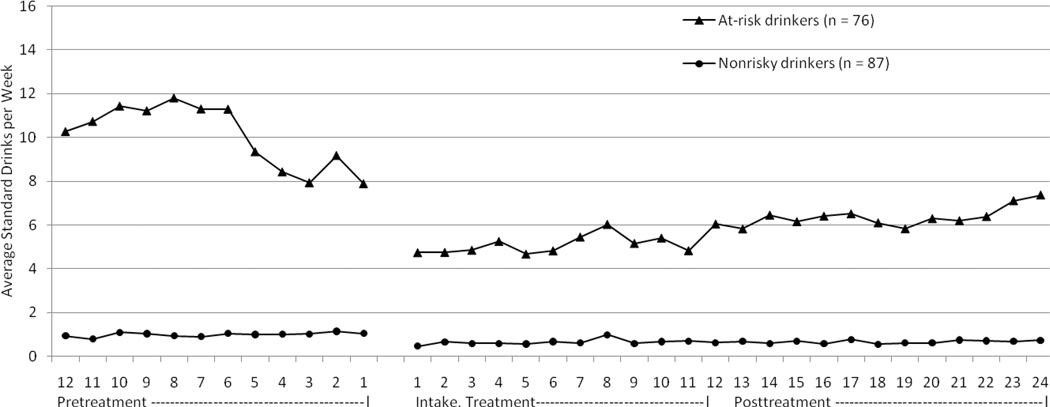
We chose a piecewise latent growth modeling approach for the ability to examine changes in drinking patterns prior to, during, and following gambling treatment using the 36 weekly estimates of alcohol use. The piecewise approach permits growth rates to change across periods without the necessity of higher order polynomial terms (Flora, 2008). These models also permit more flexibility with explanatory variables, as covariates may significantly predict the latent growth factors in some time periods but not others (Flora, 2008). With the piecewise approach, we needed to define treatment versus post-treatment phases. As noted above, the therapy included eight sessions to be completed within 12 weeks. In deciding whether the treatment phase would constitute 8 versus 12 weeks for the piecewise model, we examined the alcohol data (Figure 1); a possible inflection point near the 12th week suggested a natural breakpoint for the two slopes. For simplicity, we refer to these periods as pre-treatment (12 weeks), treatment (12 weeks), and post-treatment (12 weeks).
Figure 1.
Average drinks per week prior to, during, and following gambling treatment among drinking gamblers (N = 163) categorized by presence of at-risk drinking during the 36-week period.
For the series of models, we began with an intercept-only model and added additional parameters in each subsequent model to examine change in model fit. Once the growth model adequately represented the data, we examined the conditional models that include covariates. We determined model fit using several fit indices, including the Chi square difference test, Comparative Fit Index (CFI; Bentler, 1990), Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), root-mean-square error of approximation (RMSEA; Stieger, 1990), and standardized root mean residual (SRMR). The Chi square difference test compares nested models for improvement in fit; significant tests indicate improvement, with better fit indicated by the model with the smaller Chi square value. For both the CFI and TLI, better fit is indicated by values approaching 1.0; values >0.90 are generally considered to indicate adequate fit (Bollen & Curran, 2006). Smaller values indicate fit for the RMSEA and the SRMR, with <0.10 indicating adequate fit and <.05 indicating good fit (Brown & Cudeck, 1993). We conducted the latent growth modeling using MPLUS (version 4; Muthén & Muthén, 2006) and all other analyses with SPSS (version 15.0).
Results
Drinking Behavior
Figure 1 displays the average standard drinks per week for risky and nonrisky drinking gamblers spanning the 12 pre-treatment weeks, 12 treatment weeks, and 12 post-treatment weeks. Risky drinking status indicates the presence of risky drinking at any time in the 36-week period. A substantial decrease in average drinks per week was evident at treatment entry, particularly among the ever risky drinker group. Average number of drinking days (i.e., frequency) varied across the pre-treatment, during treatment, and post-treatment periods for both ever risky drinkers (M’s = 21.3, 10.4, and 21.6 days out of 84 possible days in each time period) and nonrisky drinkers (M’s = 8.4, 3.2, and 6.3 days out of 84 possible days), with significant within-subject (time period: pre-treatment, during treatment, post-treatment), between-subject (ever at-risk drinking status), and time by at-risk status interaction effects (ps < .05). Quadratic trends were significant for the within-subject and interaction effects (ps < .05). Significant within, between, and interaction effects were also evident for the average number of drinks per week (i.e., quantity), with significant quadratic trends for the within-subject and interaction effects (ps < .05). Risky drinkers decreased weekly alcohol intake during the treatment period but appeared to escalate drinking slightly during the post-treatment period (pre-treatment, during treatment, and post-treatment M’s = 10.3, 5.4, and 6.3 drinks/week). Nonrisky drinkers followed a similar pattern at a lower level of drinking (M’s = 1.0, 0.55, and 0.66 drinks/week).
In addition to the baseline variable comparisons in Table 1, we examined whether ever risky and nonrisky drinking patterns were associated with gambling treatment variables. Ever risky drinkers completed fewer treatment sessions or workbook chapters (M = 5.0, SD = 3.2) compared to nonrisky drinkers (M = 6.5, SD = 2.6), t(109) = 3.02, p = .003. No differences were present in the number of GA sessions attended between ever risky (M = 1.5, SD = 3.0) and nonrisky (M = 2.8, SD = 6.4) drinkers, t(118) = 1.62, p = .11. For gambling behavior during treatment, no differences were present for gambling frequency [ever risky drinkers: M = 8.4 days, SD = 13.3; nonrisky drinkers: M = 7.3 days, SD = 10.0, t(152) = −0.56, p = .58], or dollars gambled [ever risky drinkers: Mdn = $290, IQR = $0–995; nonrisky drinkers: Mdn = $330, IQR = $0–2527, U = 2738.5, p = .52].
Changes in Risk Status
We examined movement in at-risk status from the pre-treatment period to the period following treatment entry (treatment and post-treatment considered together for this analysis). Significant changes in at-risk status were present, χ2(1) = 18.98, p < .001. In the pre-treatment period, 55 (of 163 drinking gamblers, 34%) participants met criteria for at-risk drinking. Of these 55 participants, 26 participants reported no at-risk drinking following treatment entry, and 29 participants continued to exhibit risky drinking patterns following treatment entry; throughout the remaining 24 weeks, seven reported 1 week, four reported 2–3 weeks, five reported 4 to 7 weeks, and 13 reported ≥ 8 weeks of risky drinking. Of the 108 (of 163 drinking gamblers, 66%) participants who were nonrisky drinkers in the pre-treatment period, 87 continued to report nonrisk levels of drinking following treatment entry. However, 21 participants who reported no at-risk drinking pre-treatment exhibited some at-risk level drinking after treatment entry. Following treatment entry, nine of the 21 ‘new’ risky drinkers reported only 1 week (out of 24 weeks) in which drinking levels were risky. An additional six reported 2 to 3 weeks of risky drinking, and five individuals reported 4 to7 weeks of risky drinking in the 24-week period. Four individuals (2% of the drinking gamblers, n = 163; 1% of the full sample, N = 293) who reported no risky drinking in the 12 weeks before treatment exhibited a more concerning pattern of risky drinking following treatment entry (≥ 8 weeks out of 24 which met at-risk drinking criteria).
Growth Models
Table 2 displays the fit indices for the piecewise models using the full sample of 163 drinking gamblers. The intercept-only model (Model 1) provided a poor fit of the data. Model 2, using a piecewise growth structure with one latent intercept and three linear latent slopes (one slope for each 12-week phase) provided an improvement over the intercept-only model (M2 vs. M1, p < .001), but overall fit was still poor. Based on visual inspection of the observed means of alcohol use over the 36 weeks, poor fit of this model, and misfit of the first 5 weeks of during treatment alcohol use to the intercept, we chose to specify a modified piecewise model using two intercepts. For the two-intercept model (Model 3), the 12 weekly estimates of pre-treatment alcohol use loaded on the first intercept and all post-intake (during treatment and post-treatment; 24 weekly estimates) alcohol use loaded on the second intercept. The observed means indicated a substantive drop in alcohol use at the start of treatment and this two-intercept structure provided a better fit (relative to the one intercept model, M3 vs. M1, p < .001). This approach also permitted the prediction of alcohol use starting levels separately for pre-treatment and at the start of treatment in the conditional model.
Table 2.
Model Fit Indices
| Models | χ2 (df) | Δ χ2(df) | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|
| 1. Intercept-only | 4176.93 (664) | --- | .56 | .59 | .18 | .14 |
| 2. Linear Piecewise Growth [I1, LS1, LS2, LS3] |
2129.87 (652) | M2 vs. M1: 2047.06 (12) |
.82 | .82 | .12 | .08 |
| Modified-Piecewise: | ||||||
| 3. Intercepts-only Pre-treatment: I1 Post-intake: I2 |
2694.29 (661) | M3 vs. M1: 1482.64 (3) |
.75 | .76 | .14 | .09 |
| 4. Linear growth Pre-treatment: I1, LS1 Post-intake: I2, LS2, LS3 |
1712.95 (646) | M4 vs. M3: 981.34 (15) |
.87 | .87 | .10 | .06 |
| 5. Model 6 with correlated errors | 1263.60 (600) | M5 vs. M4: 449.35 (46) |
.92 | .91 | .08 | .06 |
Note. CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root Mean Square Error of Approximation; SRMR = Standardized Root Mean Residual; I1= Pre-treatment intercept; LS1= Pre-treatment linear slope; LS2= During treatment slope; LS3= Post-treatment slope; I2= Intercept at Treatment entry.
Next, we added three linear slopes, corresponding to pre-treatment, during treatment, and post-treatment phases with the 12 weekly observed drinking estimates within each phase loading on their respective slope (Model 4). The resulting model includes 1) a traditional latent growth model (intercept and slope) for the pre-treatment phase, and 2) a piecewise spline fitted for growth in the remaining weeks with growth permitted to differ in rate of change between the during treatment and post-treatment phases. The latter piece includes the post-intake intercept, the during treatment slope, and the post-treatment slope. All five latent factors (i.e., intercepts and slopes) were permitted to correlate. Model 4 was a significantly better fitting model compared to the two-intercepts-only model (M4 vs. M3, p < .001); despite the improvement, the overall model fit was not adequate per fit indices (see Table 2). In Model 5, we added correlated errors to Model 4. After examining posthoc modification indices, we permitted error variances within two units of time to correlate (e.g., week 4 may correlate with weeks 5 or 6). Given the retrospective self-reported nature of the drinking data, we anticipated some amount of correlation in the adjacent or near adjacent error variances. With the addition of correlated errors (Model 5), the fit of the model was adequate (CFI/TLI > 0.90; RMSEAR/SRMR < .10).
Average starting level of (log-transformed) drinks/week in pre-treatment was 0.82 (SE = 0.09), which was significantly different from 0 (p < .001). Average starting level of drinks/week at the beginning of treatment was 0.57 (SE = .07), again significantly greater than 0 (p < .001). The significant improvement in fit between Models 1 and 3 indicates that the introduction of a second intercept better accommodated this decrease in alcohol use between pre-treatment and treatment phases. Significant individual variability around the mean intercept was present for both intercepts [M (SE), Pre-treatment: 1.33 (0.16), Post-intake: 0.77 (.09)].
None of the three slope means differed significantly from 0, indicating that within each phase, growth was stable on average [M (SE), Pre-treatment: 0.08 (0.06), During treatment: 0.09 (0.05), and Post-treatment: 0.02 (0.05), all ps > .05]. Although the mean growth was near 0, significant individual variability around the mean slope was present for each slope [M (SE), Pre-treatment: 0.27 (0.08), During treatment: 0.22 (0.04), and Post-treatment: 0.20 (0.04), all ps < .001].
Table 3 displays the standardized covariances among the latent growth parameters and the three statistically significant associations. The two intercepts were significantly and positively associated, indicating that more alcohol use at the start of the pre-treatment phase was associated with more alcohol use at the start of the treatment phase. The pre-treatment intercept and slope were significantly and negatively associated, suggesting that individuals with higher starting levels of alcohol use evidenced less growth in alcohol use during the pre-treatment period, possibly due to a ceiling effect. A similar inverse relationship was present for the post-intake intercept and the during treatment slope.
Table 3.
Standardized Covariances among Latent Growth Factors
| Latent Factors | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Pre-treatment Intercept | --- | |||
| 2. Pre-treatment Slope | −0.62* | --- | ||
| 3. Post-intake Intercept | 0.53* | 0.03 | --- | |
| 4. During treatment Slope | −0.09 | 0.07 | −0.36* | --- |
| 5. Post-treatment Slope | −0.07 | −0.15 | −0.16 | 0.26 |
p< .05
Predictors of Drinking Levels and Change in Drinking
For the conditional model, we included demographic characteristics related to drinking (age, gender, and ever at-risk drinking status), gambling severity (baseline SOGS score), treatment condition (using three dummy codes), and gambling during treatment (product of days gambled and dollars gambled during the treatment period). We used the product of gambling frequency and intensity in order to take into account both aspects of gambling behavior while limiting the number of included covariates. All growth factors were regressed on the baseline characteristics (age, gender, ever at-risk drinking status, and gambling severity). Only the post-intake growth factors were regressed on the treatment-related variables (treatment condition and gambling activity during treatment), as we would not expect these variables to be associated with pre-treatment behavior.
Table 4 lists the standardized regression coefficients for the covariates. The conditional model fit the data adequately, model χ2 (856) = 1554.87, CFI/TLI = .91/.91, RMSEA/SRMR = .07/.06. Of the four covariates predicting the pre-treatment intercept, only gender and ever at-risk drinking status significantly predicted mean alcohol use at the start of the pre-treatment phase while controlling for other covariates in the model. As would be expected, males and ever at-risk drinkers were more likely to have higher alcohol use levels at the start of the pre-treatment phase compared to females and nonrisky drinkers, respectively. None of the four baseline characteristics significantly predicted pre-treatment change in alcohol use.
Table 4.
Standardized Regression Coefficients for Predictors
| Covariates | Pretreatment Intercept |
Pretreatment Slope |
Post-intake Intercept |
During treatment Slope |
Post- treatment Slope |
|---|---|---|---|---|---|
| Age | 0.05 | −0.18 | −0.12 | 0.33* | 0.12 |
| Male | 0.41* | 0.05 | 0.34* | 0.45* | 0.00 |
| Ever At-risk Drinkers | 0.73* | 0.01 | 0.59* | 0.14 | 0.16 |
| Lifetime SOGS | −0.00 | −0.18 | −0.20* | 0.14 | 0.04 |
| Treatment Condition | --- | --- | |||
| GA + Workbook | −0.02 | −0.37 | 0.57 | ||
| GA + CBT | −0.13 | −0.51 | 0.18 | ||
| GA + CBT + CM | −0.07 | −0.79* | − 0.14 | ||
| Gambling during Treatment | --- | --- | −0.18* | 0.16 | 0.12 |
Note. Referent for the treatment condition dummy codes is the GA-only condition. Standardized coefficients provide an indication of the strength of a relationship, with values ranging −1.0 to +1.0. GA = Gamblers Anonymous. SOGS = South Oaks Gambling Screen. CBT = Cognitive-behavioral treatment. CM = Contingency management.
p < .05
Four variables (gender, ever at-risk drinking status, baseline gambling severity, and gambling activity during treatment) significantly predicted mean level of alcohol use at the start of treatment. Males and ever at-risk drinkers had higher starting levels of alcohol use for the treatment period. Both lifetime gambling severity and gambling during treatment were negatively associated with alcohol use levels at the start of treatment.
Age, gender, and treatment condition significantly predicted alcohol use trajectories during treatment while controlling for other covariates. The during treatment slope (rate of upward growth in alcohol use) was positively associated with age. Males evidenced more escalation in alcohol use than females during the treatment period. For treatment condition, only the dummy code for CBT+CM was significantly associated with growth in alcohol use; participants in the CBT+CM condition had slower rates of growth in alcohol use during the treatment period compared to the GA-only condition. None of the six covariates significantly predicted the post-treatment slope.
Discussion
A substantial portion of the full sample (26%, 76 of 293 treatment-seeking gamblers) and drinkers (47%, 76 of 163 treatment-seeking gamblers who drank) met criteria for at-risk drinking at any point during the 36-week study period. Ever risky drinkers were younger, reported more alcohol-related problems, drank more frequently and intensely, and were less likely to adhere to gambling treatment. In the growth models, drinking appeared to decrease substantially at treatment entry, but was stable within each of the three time periods (i.e., nonsignificant slopes). However, we highlight a caution about these findings. Although these models indicate an overall reduction of alcohol use with treatment entry, 50 of the 76 ever risky drinkers exhibited drinking at or above NIAAA risky drinking guidelines during the treatment and/or post-treatment periods. The overall decreased alcohol use is encouraging, but continued at-risk drinking among the sample suggests that further reductions in drinking would be beneficial.
Understanding Alcohol Use Changes During Gambling Treatment
Reduced alcohol use during treatment did not appear to be a product of treatment itself, because reductions occurred before treatment exposure or within one treatment session. Therefore, other factors likely prompted the decreases in alcohol use. These factors may include 1) fewer conditioned cues for alcohol, 2) gambling-related financial constraints that limited funds for alcohol, or 3) the decision to change gambling behavior ‘spreading’ to other health behavior domains (i.e., alcohol). Consistent with this latter concept and in our experience treating pathological gamblers, gambling clients commonly present with a desire to change multiple other health behaviors such as eating, exercise, or alcohol and/or drug use. Data from this study appear consistent with Noar et al.’s (2008) conceptualization of health behavior change; changes in higher-order health orientation (e.g., “I want to be a healthier person”) may produce motivation to change multiple behaviors.
Future research might examine whether gambling treatment provides an opportunity to capitalize on these attitude changes and foster change in multiple domains (e.g., at-risk drinking and gambling). Multiple health behavior targets have been studied in other areas such as weight gain prevention during smoking cessation (Spring et al., 2009) and smoking cessation during substance abuse treatment (Baca & Yahne, 2009; Prochaska, Delucchi, & Hall, 2004). In general, reviews (Baca & Yahne, 2009; Prochaska et al., 2004; Spring et al., 2009) indicate that multiple behavior targets do not undermine treatment and may improve outcomes overall. Interventions targeting alcohol use may be helpful in preventing or delaying returns to risky drinking among individuals who seek treatment for gambling.
Predictors of the latent growth factors included at-risk drinking status, gender, age, lifetime gambling severity, treatment condition, and gambling during treatment. Individuals who drank in a risky manner at any time during the 36-week study period had higher levels of drinking at the start of the pre-treatment and treatment phases compared to nonrisky drinkers. Males had higher starting levels of alcohol use for both the pre-treatment and treatment phases compared to females, but males also had more during treatment escalation in alcohol use. Age was positively related to increases in alcohol use during this same period. Lifetime gambling severity and gambling during treatment were inversely related to alcohol use at treatment entry, such that less severe gamblers and those who gambled less during treatment drank more than those with greater gambling severity and activity. These associations may capture the ambiguity toward gambling changes experienced by some participants entering treatment. Individuals who entered gambling treatment less motivated toward gambling changes, perhaps because their gambling was less severe, may be less motivated to make changes in alcohol use as well. In Noar and colleagues’ (2008) conceptualization, the lack of change in both alcohol and gambling may represent less change in higher-order global health behavior attitudes. Future studies may model gambling and alcohol simultaneously to examine these relationships in more detail. Such models may examine whether individuals who fail to change their gambling behavior during treatment also fail to change alcohol use patterns. Participants randomized to the CBT+CM treatment condition, which reinforced nongambling social activities, had less escalation in alcohol use during the treatment period than patients randomized to GA only. Thus, CBT+CM participants did not appear to replace gambling with social activities involving alcohol use in general.
Despite the high comorbidity of alcohol and gambling, few studies have examined changes in alcohol use during gambling treatment. This study, along with the Toneatto et al. (2002) and Stinchfield et al. (2005) studies, indicates entry into gambling treatment may be associated reductions in alcohol use. Although our results suggest that alcohol consumption is unlikely to increase during gambling treatment for the majority of gamblers within the time period studied, we also noted some changes in risk status toward heavier drinking. For most of these individuals, we view this change as consistent with Kadden et al.’s (2009) regression toward the mean conceptualization (e.g., increased from 0 weeks of risky drinking in the 12 weeks before treatment to 1 week of risky drinking in the 24 subsequent weeks). However, a few patients exhibited onset of regular risky drinking, and future efforts may investigate patient-specific factors that lead to increases in risky drinking patterns.
Limitations/Strengths
A limitation of our study is that results cannot be generalized to other substances. Because illicit substance use was rare in this sample, we did not attempt to model it in these analyses. We also did not collect data on smoking in both studies. Given the high prevalence rate of smoking in pathological gamblers (Petry & Onken, 2002), future studies may examine whether gambling treatment is associated with changes in smoking. Further, we examined changes in alcohol use over a relatively narrow window of time. Although drinking did not increase during the study period relative to the 12-week pre-treatment period in the majority of this sample, these results do not address later changes in alcohol or other drug use.
Our study did not include a no treatment control condition, and it was a retrospective analysis of data collected from participants in studies evaluating the efficacy of gambling treatments. The results of this study may be limited in generalizability as gambling treatment was delivered in the context of a randomized clinical trial. GA may encourage abstinence from gambling as well as other addictive substances (e.g., alcohol), and results may differ if other forms of treatment were studied. Nevertheless, GA is the most commonly accessed treatment for gambling (National Research Council, 1999). The retrospective nature of this study also prevents definitive conclusions being drawn about the nature of interventions addressing both gambling and alcohol use, which await further investigation.
These analyses used a binary classification of at-risk drinking status as a predictor of individual drinking trajectories. We did not diagnose alcohol use disorders in this sample, and future studies may examine the predictive value of diagnostic categories on drinking trajectories. An additional consideration about this study is that the percent of drinkers and the percent of at-risk drinkers may be low relative to other estimates. In our sample of treatment-seeking gamblers, 56% (163 of 293) drank alcohol at some point in the 36-week period, whereas Maccallum and Blaszczynski (2002) found that 73% (55 of 75) of treatment-seeking gamblers reported past year alcohol use. Our proportion of at-risk drinkers (26%; 76 of 293) is below the 31% to 54% range of risky or hazardous drinking reported in problem and pathological gamblers in other studies (Abbott et al., 2004; Smith et al., 2010), but our rates of at-risk drinking are higher than estimates noted in non-gambling populations (11%; Mazas et al., 2006; Curry et al., 2000).
Strengths of this study include use of a continuous data record spanning 36 weeks of alcohol use and a focus on drinking quantity changes. Using a relatively large sample of drinking gamblers, we modeled weekly alcohol consumption prior to, during, and following gambling treatment providing a global picture of alcohol use over time. The results and conclusions are limited by the use of retrospective, self-reported alcohol use. However, studies (Babor, Steinberg, Anton, & Del Boca, 2000; Carney, Tennen, Affleck, Del Boca, & Kranzler, 1998; Del Boca & Darkes, 2003, 2007; Leigh, 2000; Neal et al., 2006) suggest that the TLFB is a reliable and valid measure of alcohol use with high concordance to estimates derived from prospective reports. Although a focus on frequency of alcohol use is valuable in some contexts, the present study’s analysis of quantity represents a strength because frequency can remain stable while quantity increases or decreases, potentially masking clinically relevant changes. Given the amount of at-risk drinking in this sample and others (e.g., Abbott et al., 2004; Baron & Dickerson, 1999; Smith et al., 2010), attention to drinking quantity seems particularly relevant.
Conclusion
In summary, the results of this study suggest that about one quarter of pathological gamblers entering gambling treatment drink alcohol in a risky manner and that decreases in alcohol use are temporally associated with entry to gambling treatment. We note that these temporal associations do not imply causality. We speculate that decreases in alcohol use are most likely not due to gambling treatment itself, but instead to a decision to change and improve overall health. Although alcohol consumption decreased with treatment entry and was maintained throughout the treatment and post-treatment phases, a substantial number of pathological gamblers continued to drink at risky levels, indicating that additional interventions targeting alcohol use may be needed. These results suggest areas for further research regarding the potential positive impact of integrating alcohol treatment alongside gambling treatment. Such interventions may encourage further reductions in risky drinking.
Acknowledgments
This research was supported by National Institutes of Health grants: R01-MH060417, T32-AA07290, P30-DA023918, R01-DA021567, R01-DA027615, R01-DA022739, R01-DA1344, R01-DA018883, R01-DA016855, R01-DA14618, P50-DA09241, P60-AA03510, and R01-DA024667.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb.
References
- Abbott MW, Williams MM, Volberg RA. A prospective study of problem and regular nonproblem gamblers living in the community. Substance Use & Misuse. 2004;39(6):855–884. doi: 10.1081/ja-120030891. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. Journal of Substance Abuse Treatment. 2009;36:205–219. doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Baron E, Dickerson M. Alcohol consumption and self-control of gambling behavior. Journal of Gambling Studies. 1999;15(1):3–15. doi: 10.1023/a:1023057027992. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indices in structural models. Psychometrika. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blankenship J, Starling R, Woodall WG, May PA. Gambling and alcohol use: Trends in the state of New Mexico from 1996–1998. Journal of Gambling Studies. 2007;23:157–174. doi: 10.1007/s10899-006-9051-3. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- Brown MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Carney MA, Tennen H, Affleck G, Del Boca FK, Kranzler HR. Levels and patterns of alcohol consumption using Timeline Follow-back, daily diaries, and real-time “electronic interviews”. Journal of Studies on Alcohol. 1998;59:447–454. doi: 10.15288/jsa.1998.59.447. [DOI] [PubMed] [Google Scholar]
- Cronce JM, Corbin WR. Effects of alcohol and initial gambling outcomes on within-session gambling behavior. Experimental and Clinical Psychopharmacology. 2010;18:145–157. doi: 10.1037/a0019114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham-Williams RM, Cottler LB, Compton WM, Spitznagel EL. Taking chances: Problem gamblers and mental health disorders: Results from the St. Louis Catchment Area Study. American Journal of Public Health. 1998;88(7):1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry SJ, Ludman E, Grothaus L, Donovan D, Kim E, Fishman P. At-risk drinking among patients making routine primary care visits. Preventive Medicine. 2000;31:595–602. doi: 10.1006/pmed.2000.0754. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: State of the evidence of the science and challenges for research. Addiction. 2003;98(S2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J. Enhancing the validity and utility of randomized clinical trials in addictions treatment research: II. Participant samples and assessment. Addiction. 2007;102:1194–1203. doi: 10.1111/j.1360-0443.2007.01863.x. [DOI] [PubMed] [Google Scholar]
- Flora DB. Specifying piecewise latent trajectory models for longitudinal data. Structural Equation Modeling. 2008;15:513–533. [Google Scholar]
- French MT, Maclean JC, Ettner SL. Drinkers and bettors: Investigating the complementarity of alcohol consumption and problem gambling. Drug and Alcohol Dependence. 2008;96:155–164. doi: 10.1016/j.drugalcdep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacopassi D, Stitt BG, Vandiver M. An analysis of the relationship of alcohol to casino gambling among college students. Journal of Gambling Studies. 1998;14:135–149. doi: 10.1023/a:1023094725055. [DOI] [PubMed] [Google Scholar]
- Hall KL, Rossi JS. Meta-analytic examination of the strong and weak principles across 48 health behaviors. Preventive Medicine. 2008;46:266–274. doi: 10.1016/j.ypmed.2007.11.006. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Makarchuk K. Trusting problem gamblers: Reliability and validity of self-reported gambling behavior. Psychology of Addictive Behaviors. 2003;17:244–248. doi: 10.1037/0893-164X.17.3.244. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Kabela-Cormier E, Petry NM. Increased drinking in a trial of treatments for marijuana dependence: Substance substitution. Drug and Alcohol Dependence. 2009;105:168–171. doi: 10.1016/j.drugalcdep.2009.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kausch O. Patterns of substance abuse among treatment-seeking pathological gamblers. Journal of Substance Abuse Treatment. 2003;25:263–270. doi: 10.1016/s0740-5472(03)00117-x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Hwang I, LaBrie R, Petukhova M, Sampson NA, Winters KC, Shaffer HJ. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine. 2008;38:1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford; 2005. [Google Scholar]
- Leigh BC. Using daily reports to measure drinking and drinking patterns. Journal of Substance Abuse. 2000;12:51–65. doi: 10.1016/s0899-3289(00)00040-7. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. The South Oaks Gambling Screen (the SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. Modifying the Addiction Severity Index for use with pathological gamblers. American Journal on Addictions. 1992;1:240–247. [Google Scholar]
- MacCallum F, Blaszcynski A. Pathological gambling and comorbid substance use. Australia New Zealand Journal of Psychiatry. 2002;36(3):411–415. doi: 10.1046/j.1440-1614.2001.01005.x. [DOI] [PubMed] [Google Scholar]
- Mazas CA, Cofta-Woerpel L, Daza P, Fouladi RT, Vidrine JI, Cinciripini PM, Gritz ER, Wetter DW. At-risk drinking in employed men and women. Annuals of Behavioral Medicine. 2006;31(3):279–287. doi: 10.1207/s15324796abm3103_10. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffiths J, McGahn P, O’Brien CP. Guide to the Addiction Severity Index: Background, administration, and field testing results. Washington, DC: US Government Printing Office; 1988. (DHHS Publication No. ADM88–1419) [Google Scholar]
- Muthén LK, Muthén B. MPlus Users Manual. Los Angeles, CA: Muthén & Muthén; 2006. [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician’s guide. 2007 NIH Publication No. 07-37690 Retrieved from http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf.
- National Research Council. Pathological gambling: A critical review. Washington, DC: National Academies Press; 1999. [PubMed] [Google Scholar]
- Neal DJ, Fromme K, Del Boca FK, Parks KA, King LP, Pardi AM, et al. Capturing the moment: Innovative approaches to daily alcohol assessment. Alcohol Clinical and Experimental Research. 2006;30(2):282–291. doi: 10.1111/j.1530-0277.2006.00025.x. [DOI] [PubMed] [Google Scholar]
- Noar SE, Chabot M, Zimmerman RS. Applying health behavior theory to multiple behavior change: Considerations and approaches. Preventive Medicine. 2008;46:275–280. doi: 10.1016/j.ypmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- Petry NM. Stopping problem gambling: A self-help manual. 1998 Unpublished manuscript. [Google Scholar]
- Petry NM. Validity of a gambling scale for the Addiction Severity Index. Journal of Nervous and Mental Disease. 2003;191(6):399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- Petry NM. Pathological gambling: Etiology, comorbidity, and treatments. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- Petry NM. Should the scope of addictive behaviors be broadened to include pathological gambling? Addiction. 2006;101(S1):152–160. doi: 10.1111/j.1360-0443.2006.01593.x. [DOI] [PubMed] [Google Scholar]
- Petry NM. Gambling and substance use disorders: Current status and future directions. American Journal on Addictions. 2007a;16:1–9. doi: 10.1080/10550490601077668. [DOI] [PubMed] [Google Scholar]
- Petry NM. Concurrent and predictive validity of the Addiction Severity Index in pathological gamblers. American Journal on Addictions. 2007b;16(4):272–282. doi: 10.1080/10550490701389849. [DOI] [PubMed] [Google Scholar]
- Petry NM, Ammerman Y, Bohl J, Doersch A, Gay H, Kadden R, et al. Cognitive-behavioral therapy for pathological gamblers. Journal of Consulting and Clinical Psychology. 2006;74(3):555–567. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- Petry NM. Cognitive behavioral and contingency management treatment for pathological gambling. 2010 Unpublished raw data. [Google Scholar]
- Petry NM, Oncken C. Cigarette smoking is associated with increased severity of gambling problems in treatment-seeking gamblers. Addiction. 2002;97:745–753. doi: 10.1046/j.1360-0443.2002.00163.x. [DOI] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66(5):564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Potenza MN. Should addictive disorders include non-substance-related conditions? Addiction. 2006;101(S1):142–151. doi: 10.1111/j.1360-0443.2006.01591.x. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. Journal of Consulting and Clinical Psychology. 2004;72:1144–1156. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, LaPlante DA, LaBrie RA, Kidman RC, Donato AN, Stanton MV. Toward a syndrome model of addiction: Multiple expressions, common etiology. Harvard Review Psychiatry. 2004;12:367–374. doi: 10.1080/10673220490905705. [DOI] [PubMed] [Google Scholar]
- Smith D, Harvey P, Battersby M, Pols R, Oakes J, Baigent M. Treatment outcomes and predictors of drop out for problem gamblers in South Australia: A cohort study. Australian & New Zealand Journal of Psychiatry. 2010;44:911–920. doi: 10.3109/00048674.2010.493502. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Followback User’s Guide: A Calendar Method for Assessing Alcohol and Drug Use. Toronto, Ontario, Canada: Addiction Research Foundation; 1992. Timeline. [Google Scholar]
- Spring B, Howe D, Berendsen M, McFadden HG, Hitchcock K, Rademaker AW, Hitsman B. Behavioral intervention to promote smoking cessation and prevent weight gain: A systematic review and meta-analysis. Addiction. 2009;104:1472–1486. doi: 10.1111/j.1360-0443.2009.02610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, McWiliams LA, Blackburn JR, Klein RM. A laboratory-based investigation of relations among video lottery terminal (VLT) play, negative mood, and alcohol consumption in regular VLT players. Addictive Behaviors. 2002;27:819–835. doi: 10.1016/s0306-4603(01)00213-1. [DOI] [PubMed] [Google Scholar]
- Stieger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks Gambling Screen (SOGS) Addictive Behaviors. 2002;27:1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- Stinchfield R, Kushner MG, Winters KC. Alcohol use and prior substance abuse treatment in relation to gambling problem severity and gambling treatment outcome. Journal of Gambling Studies. 2005;21:273–297. doi: 10.1007/s10899-005-3100-1. [DOI] [PubMed] [Google Scholar]
- Toneatto T, Skinner W, Dragonetti R. Patterns of substance use in treatment-seeking problem gamblers: Impact on treatment outcomes. Journal of Clinical Psychology. 2002;58(7):853–859. doi: 10.1002/jclp.2011. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;23:19–23. [Google Scholar]
- Weinstock J, Whelan JP, Meyers AW. Behavioral assessment of gambling: An application of the Timeline Followback Method. Psychological Assessment. 2004;16:72–80. doi: 10.1037/1040-3590.16.1.72. [DOI] [PubMed] [Google Scholar]
- Zack M, Stewart SH, Klein RM, Loba P, Fragopoulos F. Contingent gambling-drinking patterns and problem drinking severity moderate implicit gambling-alcohol associations in problem gamblers. Journal of Gambling Studies. 2005;21(3):325–354. doi: 10.1007/s10899-005-3102-z. [DOI] [PubMed] [Google Scholar]