Abstract
The present study tested the proposition that an intervention to reduce alcohol use among college students will also reduce their risky sexual behavior. In a randomized, controlled trial, 154 heavy-drinking, predominantly White, heterosexual college students at behavioral risk for infection with HIV and other STDs were assigned to receive no intervention or a two-session, in-person, motivational interviewing-based intervention focused on either: (a) reducing alcohol risk behavior, (b) reducing HIV risk behavior, or (c) reducing both alcohol and HIV risk behavior. Three-month retrospective assessments of alcohol use and sexual behavior were conducted at intake and at 3-, 6-, 9-, 12-, and 15-month follow-up appointments. During follow-up, participants who received the single-focus Alcohol risk-reduction intervention drank less frequently and consumed fewer drinks per drinking day compared to no-intervention control participants, but did not differ from control participants in their frequency of intercourse without a condom or number of sexual partners. Participants who received the single-focus HIV risk-reduction intervention evidenced fewer unprotected sex events during follow-up, compared to control participants. The number of sexual partners reported during follow-up did not differ by condition. Effects of the interventions did not vary significantly over time and were not moderated by participant gender. Results suggest that intervening to reduce alcohol use may not reduce risky sexual behavior among non-minority college students, but that a brief motivational intervention targeting HIV risk behavior may have utility for reducing the frequency of unprotected sex in this population.
Keywords: alcohol use, sexual behavior, HIV risk, motivational interviewing, college students, randomized controlled trial
Sexual behavior that increases risk for infection with HIV and other sexually transmitted diseases (STDs) appears to be common among college students. In one large survey, fewer than a third of sexually active undergraduate students reported consistent condom use during intercourse (Douglas et al., 1997). A more recent survey found that only about 4 in 10 students always used a condom during vaginal sex, and fewer used one during anal sex (Buhi, Marhefka, & Hoban, 2010). Among students with any sexual experience, almost 9% reported having four or more sex partners within the last school year (Buhi et al., 2010). Other studies suggest that the average college student has two new sexual partners per year (Cooper, 2002).
Alcohol use also is common among college students. Although most are light to moderate drinkers, many students engage in heavy, problematic levels of consumption (Knight et al., 2002) thought both to decrease the likelihood of condom use (e.g., Kaly, Heesacker, & Frost, 2002) and to increase the likelihood of having multiple, casual partners (e.g., Grello, Welsh, & Harper, 2006). Findings that alcohol use and risky sexual behavior often co-occur may be explained in part by developmental or personality factors (e.g., a tendency toward sensation-seeking) that underlie both behaviors (Cooper, 2002; Igra & Irwin, 1996). However, research suggests also that alcohol consumption sometimes contributes causally to the occurrence of HIV risk behavior. Data from several event-level survey studies (e.g., Kiene, Barta, Tennen, & Armeli, 2009; Neal & Fromme, 2007; Scott-Sheldon, Carey, & Carey, 2008) and laboratory research (e.g., Gordon & Carey, 1996; MacDonald, Zanna, & Fong, 1996) are consistent with this hypothesis.
Researchers have considered a number of mechanisms that might account for a causal link between alcohol use and sexual risk taking (for reviews, see Cooper, 2002, 2006). For example, “alcohol myopia” theory states that alcohol acts by reducing the scope and efficiency of information processing (Steele & Josephs, 1990), such that highly salient cues (such as sexual arousal) continue to be processed, whereas cues that arise from more complex processing (e.g., thoughts about potential long-term consequences such as getting AIDS) either fail to enter awareness or are no longer seen as significant. Other researchers have suggested that a link between alcohol consumption and sexual behavior can be understood as a consequence of activation, during intoxication, of individually held expectations that mirror widely-held cultural beliefs about the effects of alcohol (Dermen & Cooper, 1994; Dermen, Cooper, & Agocha, 1998; Lang, 1985; Reinarman & Leigh, 1988). Conflicting findings regarding the nature of the relationship between alcohol use and sexual risk taking appear to reflect the underlying complexity of the relationship (Cooper, 2006; Graves, 1995). However, despite continued uncertainty regarding alcohol’s role, many authors have suggested that efforts to reduce risky sex among college students should include a focus on reducing heavy drinking (e.g., Downing-Matibag & Geisinger, 2009; Hoban, Ottenritter, Gascoigne, & Kerr, 2003; Kaly et al., 2002; Neal & Fromme, 2007).
Although little research has systematically examined whether reducing heavy and problematic drinking can lead to reductions in HIV risk behavior, several mechanisms might contribute to such an effect (Leigh & Stall, 1993; Cooper, 1992). To the extent that alcohol consumption directly increases the likelihood of risky sex, a general reduction in drinking may lead to a decrease in alcohol-induced risk taking. Less frequent drinking may also decrease an individual’s exposure to “risky situations,” such as bars, that may encourage sexual risk taking independent of alcohol’s effects. Finally, a reduction in drinking may become part of a general lifestyle change, in which maintaining good health has greater salience (Leigh & Stall, 1993).
In addition to encouraging an overall reduction in alcohol use, it may be valuable to suggest specific methods for reducing alcohol-related risk of engaging in risky sexual behavior. For instance, individuals who have strong sex-related alcohol expectancies or who feel strongly conflicted about whether or not to use condoms can be advised that they may be especially subject to an increased tendency toward risk taking after drinking (Dermen & Cooper, 2000; Dermen et al., 1998). To avoid reinforcing the notion that alcohol provides an excuse for risk taking (cf. Bolton, Vincke, Mak, & Dennehy, 1992; Dermen et al., 1998), information can be provided about a range of approaches that the individual can take to avoid such a consequence (e.g., practicing assertion regarding condom use).
In sum, interventions that address alcohol use and its effects have the potential to enhance the efficacy of HIV prevention efforts via a number of potential mechanisms. In the present study, we set out to test the hypothesis that efforts to reduce risky sexual behavior will be enhanced by adding a component aimed at reducing drinking. To maximize the potential utility of results from this study, we employed brief, practical intervention approaches based on the principles of motivational interviewing (Miller & Rollnick, 1991, 2002). Reviews of an extensive literature (e.g., Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Larimer & Cronce, 2007) have found individual-focused interventions based on motivational interviewing (MI) to be consistently efficacious in reducing drinking among college students. The use of MI methods has been recommended also in the area of HIV prevention (e.g., Brown & Lourie, 2001; Carey & Lewis, 1999; Pedlow & Carey, 2003; Rutledge, 2007), because many individuals whose behavior puts them at increased risk of infection with HIV and other STDs fail to see the need for change or fail to take steps toward change even if they think that doing so might be beneficial (Grimley, Prochaska, Velicer, & Prochaska, 1995).
To date, most research on the application of MI methods to risky sexual behavior has studied interventions that combine such methods with skills-building intervention components (e.g., Belcher et al., 1998; Carey, Maisto et al., 1997; Carey et al., 2000; Jaworski & Carey, 2001). However, recent studies have examined the use of MI methods as the central component of a stand-alone motivational intervention. In a study of heterosexual college men, a decisional balance exercise conducted in a non-confrontive, MI style was found to increase condom use during a one-month follow-up period (LaBrie, Pederson, Thompson, & Earleywine, 2008). In a study of young African-American men who have sex with men, a 30-minute MI intervention significantly increased the proportion who agreed to receive HIV counseling and testing and who returned later to receive their test results, compared to a traditional, education-based intervention of the same length (Outlaw et al., 2010).
Only a few studies have examined the use of MI methods to address substance use and risky sexual behavior simultaneously. In one such study, incarcerated adolescents were assigned to receive two sessions of either relaxation training or MI-based motivational enhancement, as a supplement to other services delivered at the facility (Rosengard et al., 2007). Motivational sessions focused on alcohol and marijuana use as well as associated risky behaviors, such as illegal activity and sexual behavior. Among adolescents who reported few depressive symptoms at baseline, participation in the motivational intervention was associated with lower frequency of sex without a condom during the three months following release from the facility. In a study with adolescent residents of a short-term detention facility, a three-to-four-hour intervention that combined MI-style discussion of alcohol use (primarily as it affects risky sexual behavior) with a traditional psychosocial HIV/STD risk-reduction intervention was compared to (a) a three-hour intervention involving the latter component delivered in isolation and (b) a two-hour information-only control condition (Bryan, Schmiege, & Broaddus, 2009). Results suggested that, with regard to frequency of condom use, outcomes of the two active interventions did not differ significantly from each other but were better than those of the control condition. However, the three conditions did not differ in their effects on frequency of alcohol use in conjunction with sexual intercourse. A study conducted with HIV-positive youths (ages 16-25) found that a MI-based intervention that focused on sexual risk, substance use, and medication adherence (participants chose two topics), compared to a wait-list control group, yielded greater reductions in unprotected intercourse but had no differential effect on alcohol use (Naar-King et al., 2006).
In a study of college women at risk of alcohol-exposed pregnancy, a single-session MI-based intervention that addressed both alcohol use and effective contraceptive use, compared to a minimal-intervention (brochure) control condition, yielded greater reductions in alcohol use and improvements in effective contraceptive use, as well as lower rates of risk for alcohol-exposed pregnancy (Ingersoll et al., 2005). Finally, in a study of two six-session hepatitis and HIV risk-reduction interventions for out-of-treatment drug users, the MI-based intervention yielded greater reductions in alcohol use than an educational intervention over the course of the one-year follow-up period (Zule, Costenbader, Coomes, & Wechsberg, 2009). Likelihood of condom use at last intercourse (at 6- and 12-month follow-up assessments) increased in both conditions.
The present study was designed to assess the independent and joint effects of a drinking risk-reduction intervention and an HIV risk-reduction intervention on subsequent drinking (frequency of drinking; drinks per drinking day) and HIV risk behavior (number of unprotected sex events; number of sexual partners). To this end, heavy-drinking heterosexual male and female college students at behavioral risk for infection with HIV and other STDs were randomly assigned to receive no intervention or an intervention that focused on either: (a) reducing alcohol risk behavior, (b) reducing HIV risk behavior, or (c) reducing both alcohol and HIV risk behavior. Thus, content of the intervention was factorially crossed: presence or absence of alcohol risk-reduction content with presence or absence of HIV risk-reduction content.
With regard to alcohol outcomes, we hypothesized that the Alcohol risk content factor would produce a main effect, such that participants who received either the Alcohol risk-reduction intervention or the Combined intervention would drink less during follow-up than participants who received no intervention or the HIV risk-reduction intervention. HIV risk-reduction content was not expected to affect drinking behavior. With regard to HIV risk behavior, we hypothesized that both the Alcohol risk content and HIV risk content factors would produce main effects, such that HIV risk behavior levels during follow-up would be lowest among participants who received the Combined intervention (due to the additive effects of alcohol and HIV risk content) and highest among Control participants (i.e., those who received no intervention). Although analyses were planned to test for the presence of interactions between conditions, no such interactions were hypothesized. Because men and women experience different concerns and relative risks regarding HIV and alcohol risk behavior (e.g., Dekin, 1996; Jadack, Hyde, & Keller, 1995; Randolph, Torres, Gore-Felton, Lloyd, & McGarvey, 2009), we also examined the impact of participant gender on response to the above interventions, although no hypotheses were developed in this regard.
Method
Participants
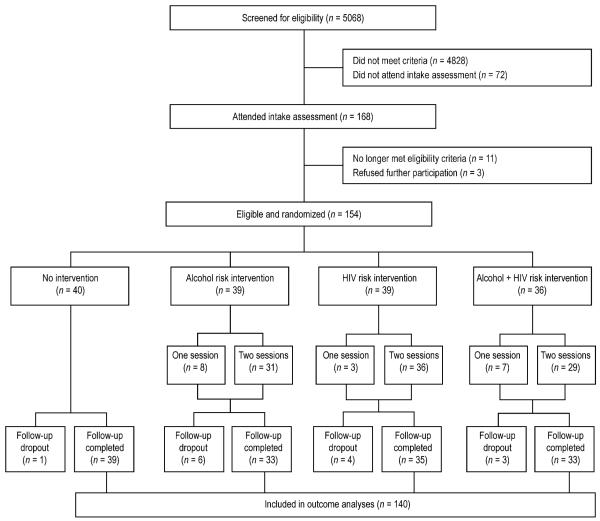
This study was approved by Institutional Review Boards at the Research Institute on Addictions and the University at Buffalo. Participants were students at colleges and universities in the Buffalo, NY, metropolitan area. Figure 1 shows participant flow through the study.
Figure 1.
Participant flow through the study.
A total of 154 eligible students (91 women, 63 men) met eligibility criteria and participated in the study. Participants ranged from 18 to 30 years of age (M = 20.7, SD = 2.0). All were unmarried and nearly all described themselves as heterosexual (two women reported being bisexual). Proportions of the sample in their first through sixth years of college were 25.3%, 21.4%, 26.6%, 14.9%, 9.1%, and 2.6%, respectively. Participant racial/ethnic group membership was 86.4% White, 5.2% Hispanic, 3.9% African-American, 3.9% Asian-American, and 0.6% American Indian. Lifetime alcohol problem scores on the Young Adult Alcohol Problems Screening Test (YAAPST; Hurlbut & Sher, 1992) ranged from 1 to 20 (out of a possible 27 points; M = 9.2, SD = 3.9). Marijuana use during the prior three months was reported by 64.9% of participants, hallucinogen use by 20.8%, cocaine use by 9.1%, and opiate use by 7.1%. Lifetime number of sex partners reported by participants ranged from 1 (6.5% of participants) to more than 20 (4.5%); over half (55.2%) reported having at least 5 lifetime partners. A history of infection with a sexually transmitted disease was reported by 8.4% of participants. Participants reported a mean of 38.3 (SD = 32.6) occurrences of vaginal or anal intercourse during the 90-day baseline, of which about a third were preceded by alcohol use (M proportion = .32, SD = .25).
Students were recruited through classroom screenings, flyers, and newspaper advertisements for a “study on drinking and college-related experiences.” During an initial pre-screening, either in class or via telephone, students were told that we were interested in the “health-related behaviors of college students” and answered a series of 13 questions. Potentially eligible students then completed a more detailed telephone screening interview. Eligibility criteria were designed to include students whose alcohol use and sexual behavior both presented some risk but whose responses did not indicate a need for more intensive intervention. Eligible students reported (a) being 18 to 30 years of age; (b) consuming at least five (men) or four (women) drinks at least once in the past two weeks; (c) having either a heterosexual or bisexual orientation; (d) seven or more occurrences of unprotected heterosexual intercourse in the past 90 days, and (e) having two or more sex partners in the past 90 days or having a partner who had other partners in the past 24 months but had not been tested for HIV during the past 12 months. Students were excluded if they had a score of 20 or higher on the Short-form Alcohol Dependence Data Questionnaire (Davidson & Raistrick, 1986; modified to assess heaviest drinking in lifetime) or reported 10 or more days of illicit drug use in the past month and had a score of 3 or greater on the 10-item Drug Abuse Screening Test (Skinner, 1982; Yudko, Lozhkina, & Fouts, 2007), or if they reported any of the following: being married; planning to move out of town in the next two months; currently abstaining from alcohol; currently facing legal charges or disciplinary action for an alcohol-related incident; having ever been treated for alcohol or drug abuse; currently receiving counseling for a drinking or drug problem; having injected an illicit drug in the prior six months; recently having difficulties controlling aggressive behavior; currently having serious thoughts of suicide; currently taking prescription medications for anxiety or depression, or any other medication for which alcohol use was contraindicated; or currently being, or attempting to become, pregnant. Students who met eligibility criteria were scheduled for an in-person meeting with an intervention counselor.
Intake Assessment Procedure and Measures
Intake assessments to provide baseline data and a final confirmation of eligibility were conducted by an intervention counselor of the same gender as the participant. Alcohol use and sexual behavior during the prior 90 days were assessed retrospectively using a modified Timeline Follow-back (TLFB) interview (based on Carey et al., 1998; see also Carey, Carey, Maisto, Gordon, & Weinhardt, 2001; Weinhardt et al., 1998). For each day, participants reported the number of standard drinks consumed, type of any other drugs used, whether vaginal or anal intercourse occurred, and (for each occurrence) the initials and gender of the partner, the type of contraception used (if any), and whether alcohol or drugs were used prior to sex. Supplementary questions assessed whether each partner was non-monogamous, had ever used injection drugs, or (for male partners of female participants) had ever had sex with another man. Outcome variables computed from TLFB data were frequency of alcohol use (number of drinking days), intensity of alcohol use (drinks per drinking day), frequency of unprotected intercourse (without a latex or polyurethane condom), and number of sexual partners. A structured interview and self-administered questionnaire packet included other measures pertaining to behaviors, attitudes, and beliefs. Participants received either two psychology subject pool credits or $20 as compensation for participating in the assessment.
Collateral assessments of drinking
To encourage accurate participant reports, collateral reports of participants’ alcohol use were obtained when possible by means of a telephone-administered TLFB interview at baseline and at each follow-up assessment. Although college student self-reports of drinking generally are accurate (Hagman, Clifford, Noel, Davis, & Cramond, 2007; LaForge, Borsari, & Baer, 2005), we compared participant and collateral reports (when available) to establish the degree of concordance between them. Collateral reports for the six assessment windows (intake, 3-, 6-, 9-, 12-, and 15-month) were available for 89.6%, 83.1%, 83.1%, 75.3%, 73.4%, and 66.9% of participants, respectively. At intake, collateral reports of their relationship to the participant were as follows: 51% friend, 24% “significant other,” 18% roommate, 4% sibling, and 3% cousin.
Intervention Procedure
Counselors were blind to condition assignment until after completion of the intake interview. At that time, counselors opened the next in a series of random assignment envelopes (prepared in advance by the project director using a random number table) to determine which (if any) feedback report to prepare. For participants assigned to an intervention condition, data from some questionnaire measures (placed early in the packet) were used in the preparation of feedback while the participant completed the remaining questionnaires. Personalized feedback information, calculated manually by the counselor using a detailed feedback preparation manual, was written onto a printed, condition-specific feedback form. Immediately after participants completed their questionnaires, counselors informed participants of their random assignment to one of four conditions: Alcohol risk-reduction, HIV risk-reduction, Combined, or Control. Individuals assigned to the Control condition scheduled their 3-month follow-up assessment and had no further contact with staff until follow-up. Students assigned to an intervention condition immediately participated in the first of two individual motivational counseling sessions, conducted by the counselor who conducted the intake interview.
In all three intervention conditions, the counselor’s goals were to create an awareness of the need for change, to increase participants’ motivation to make a change, and to discuss plans for change. Intervention procedures were closely modeled on a “drinker’s check-up” approach (Miller, Sovereign, & Krege, 1988) similar to that employed in motivational enhancement therapy (Miller, Zweben, DiClemente, & Rychtarik, 1994). The counselor began by eliciting and reflecting the participant’s thoughts and concerns regarding the target topic. The counselor then elicited participant reactions to personalized feedback on the participant’s behavioral risk status. Finally, the counselor elicited participant thoughts and feelings regarding costs and benefits of making a change and of not changing and asked open-ended key questions with an eye toward eliciting a decision to change. If appropriate, the counselor also elicited information about steps the participant might take in making a change. The participant then scheduled a second session to be held approximately five weeks later and left with his or her Personal Feedback Report, an explanatory booklet, a Decisional Balance Sheet (if completed), a Change Plan Worksheet (if completed), and a booklet describing strategies and sources of support for reducing risk behavior (materials developed or adapted for this study and available from the first author). This first session lasted approximately 45 minutes for Alcohol risk-reduction and HIV risk-reduction intervention participants and 60 minutes for Combined intervention participants. After each session, the counselor mailed a handwritten note affirming the participant, summarizing his or her statements, and expressing optimism about change.
During the second session, participant thoughts about and efforts to change were reviewed, and motivational interviewing methods were employed with the goal of encouraging either initiation or continued use of risk-reduction strategies and resources. This session lasted approximately 30 minutes for Alcohol risk-reduction and HIV risk-reduction intervention participants and 45 minutes for Combined intervention participants. At the end, participants scheduled their 3-month follow-up assessment.
Alcohol risk-reduction intervention
In this condition, the initial focus was on eliciting what the participant likes and does not like about drinking. When appropriate, the counselor inquired about drinking patterns, drinking games, perceptions of peer norms, and values and goals relevant to alcohol use. For lighter drinkers, emphasis was placed on eliciting reasons for not drinking heavily. Feedback included the following, derived from screening and intake assessments: (a) number of standard drinks per week and percentile ranking compared to same-sex American college students; (b) estimated blood alcohol concentration (BAC) peaks in a typical week and on a heavier day of drinking (computed using BACCuS 2.01 software; Markham, Miller, & Arciniega, 1993); (c) levels of risk associated with tolerance (as indexed by BAC peaks), other drug use, and family history; (d) levels of lifetime and recent consequences of alcohol use (obtained from the YAAPST; Hurlbut & Sher, 1992); (e) and thoughts about cutting down (derived from the Readiness to Change Questionnaire; Rollnick, Heather, Gold, & Hall, 1992). A nine-page handout provided to participants in this condition offered suggestions for setting goals, self-monitoring, use of drinking moderation strategies, and finding alternatives to drinking and included a list of relevant counseling services, websites, and other material.
HIV risk-reduction intervention
In this condition, the initial focus was on eliciting participant thoughts and concerns regarding current or recent sexual relationships, risks for pregnancy and STDs, the use or non-use of condoms within sexual relationships, perceived peer norms regarding STD concerns and condom use, and values and goals relevant to protective behavior. Other topics addressed, when appropriate, included reasons for sometimes choosing to use condoms (for those whose use was inconsistent) and the perceived importance of mutual caring behavior in relationships. Feedback included the following: (a) history of risk-related sexual behavior, including (i) the number of occurrences of unprotected sex (no condom) in the prior 90 days, (ii) the proportion of sex that was unprotected, (iii) the proportion of UB students who used condoms more often than the participant (based on screening data collected during a pilot phase of the study), (iv) the number of sex partners reported in the prior 90 days, (v) whether any of the participant’s partners had a history of HIV risk behavior, and (vi) whether the participant reported ever having a STD; (b) percent of items correct on the HIV Knowledge Questionnaire (Carey, Morrison-Beedy, & Johnson, 1997); and (c) plans regarding consistent condom use with a main partner and with other partners. A seven-page booklet provided to participants in this condition provided suggestions for setting safer-sex goals, seeking additional information on HIV prevention, practicing safer sex, and being assertive with a partner regarding condom use, and provided specific information regarding condoms and their proper use as well a list of relevant counseling resources, websites, and other material. Overall, the focus of this intervention was on HIV risk and its reduction, although risk for other STDs also was discussed.
Combined risk-reduction intervention
Procedures in this condition incorporated those of the two single-focus conditions and addressed more directly the potential contribution of alcohol use to risky sexual behavior. The counselor initially guided discussion toward topics to which the participant was receptive and sought to integrate discussion of alcohol and sexual behavior when possible. Although discussing alcohol-related sexual behavior as a specific topic was a goal, less time was spent on this topic than on alcohol use and HIV risk as separate topics, which generally were given equal time. If a student reported never drinking in conjunction with sex or reported never using condoms regardless of whether or not alcohol was consumed, the topic of alcohol-related sexual behavior was dealt with only briefly. Feedback covered both domains of behavior (as previously described) and also included information regarding the number of sex occurrences that occurred after drinking during the prior 90 days, the proportion of sex that occurred after drinking, and the extent to which the participant expected alcohol to increase sexual enjoyment, disinhibition, and risk taking (as measured by the Sex-Related Alcohol Expectancy Scale; Dermen & Cooper, 1994). The informational booklet provided to participants in this condition was simply a combination of the two single-focus booklets.
Intervention Monitoring and Supervision
Six masters-level counselors were trained and supervised jointly by the first and second authors (principal investigator and project director). Both authors are clinical psychologists; the first is also an experienced motivational interviewing trainer and supervisor and a member of the Motivational Interviewing Network of Trainers. Each counselor was trained in all three intervention conditions and conducted approximately equal numbers of sessions across conditions. All intervention sessions were audiotaped. The second author reviewed these tapes for protocol adherence and conducted individual clinical supervision on a weekly basis. Group supervision, involving all counselors and both supervisors, was conducted at least bi-weekly.
Counselor compliance with the protocol was formally evaluated through blind rating of tapes, using scales employed in past research (Connors, Walitzer, & Dermen, 2002) and adapted for this study. Each tape was rated by two trained research assistants on the extent to which counselors engaged in MI-consistent behaviors, both content-specific (five alcohol risk content items [e.g., eliciting concerns about drinking] and five parallel HIV risk content items) and general (two items: reflective listening, supporting self-efficacy). An additional item assessed the extent to which counselors engaged in the MI-inconsistent behavior of confrontation. Ratings of counselor engagement in each behavior were made on a 4-point scale ranging from 1 (not at all) to 4 (extensively), and average ratings across raters were computed for use in analyses.
Follow-up Assessment Procedure
In-person follow-up interviews were planned to occur 3, 6, 9, 12, and 15 months following the intake assessment. Follow-up assessments were conducted by same-gender interviewers blind to experimental condition. Participants received $30 compensation for each follow-up assessment (maximum of $150). Follow-up measures were essentially the same as those at intake, modified as needed to fit follow-up time frames. For participants who had moved out of the area, assessments were completed by telephone and by mail (19% of follow-up interviews). After completion of each interview, participants scheduled the following interview.
Analytic Strategy
Participants who were missing outcome data from any follow-up point were dropped from outcome analyses (see Figure 1). To correct departures from normality, square-root transformations were applied to drinking frequency data and log transformations were applied to data for the remaining three outcomes. For ease of presentation and interpretation, all means and standard deviations presented are from untransformed variables. Comparisons of participant and collateral reports of participant drinking were conducted through the use of Pearson correlations and paired t-tests. Tests of pre-intervention equivalence on each outcome measure were conducted as 2 × 2 × 2 (Alcohol risk content x HIV risk content x Gender) analyses of variance (ANOVAs) on baseline values. Outcome analyses were conducted as 2 × 2 × 2 × 5 (Alcohol risk content x HIV risk content x Gender x Time) repeated measures analyses of covariance on follow-up values of each dependent measure, using baseline value as a covariate.
Results
Preliminary Analyses
All of the 114 participants assigned to receive an intervention completed Session 1; 96 (84.2%) completed Session 2. Neither baseline characteristics nor condition assignment predicted likelihood of completing Session 2. Follow-up completion rates for the 3-, 6-, 9-, 12-, and 15-month windows were 95%, 94%, 92%, 91%, and 91%, respectively, and did not differ significantly by condition. However, among those participants assigned to receive an intervention, complete follow-up data were available from 93 of the 96 who attended both intervention sessions and from 8 of the 18 who attended a single intervention session. This difference was significant (p < .001 by Fisher’s exact test).
An a priori sensitivity analysis was conducted to obtain a conservative estimate of the power of our study to detect hypothesized effects. This analysis was based on the study’s design and obtained sample size, without reference to the observed data. Given alpha = .05, power = .80, and a post-attrition N of 140, calculations indicated that we could expect to detect an intervention content main effect greater than or equal to η2 = .031 (in the small-to-medium range as described by Cohen, 1988) and a two-way intervention content interaction effect greater than or equal to η2 = .059 (in the medium range).
Demographic and other descriptive characteristics did not differ significantly by intervention condition, nor did baseline frequency of unprotected sex. However, baseline levels of the remaining three outcome variables were found to be significantly unbalanced across conditions in this sample. Baseline and follow-up means and standard deviations of the outcome variables are presented in Table 1. An analysis of baseline drinking frequency data (number of drinking days in the 90-day window) found an Alcohol risk content X HIV risk content interaction, F (1, 146) = 4.00, p = .047, η2 = .023. However, simple main effects tests probing the interaction were not significant. A significant gender main effect on this variable, F (1, 146) = 17.59, p < .001, η2 = .103, indicated that men drank more frequently than women during baseline (M days = 39.3, 26.6, SDs = 20.0, 14.1, respectively). An analysis of baseline drinking intensity data revealed a main effect of HIV risk content, F (1, 146) = 5.03, p = .026, η2 = .030, such that participants assigned to receive HIV risk content (HIV or Combined conditions) reported more drinks per drinking day than those assigned not to receive HIV risk content (Control or Alcohol conditions). Also, a significant gender main effect, F (1, 146) = 9.58, p = .002, η2 = .057, indicated that men drank more per drinking day than women at baseline (M drinks = 6.9, 5.4, SDs = 3.7, 2.4, respectively). Finally, an analysis of baseline data on number of partners found an HIV risk content main effect, F (1, 146) = 7.23, p = .008, η2 = .044, such that participants assigned to receive HIV risk content had more partners than did participants assigned not to receive such content. Also, a significant gender effect, F (1, 146) = 6.92, p = .009, η2 = .042, indicated that men reported more sexual partners at baseline than did women (M = 2.1, 1.6, SDs = 1.5, 1.1, respectively). No other effects on baseline data were detected.
Table 1. Baseline and Follow-up Means (SDs) of Study Outcome Variables for the Four Conditions.
| Follow-up Assessment | |||||||
|---|---|---|---|---|---|---|---|
| Intake | 3-month | 6-month | 9-month | 12-month | 15-month | ||
| Variable | Condition | ||||||
| Drinking Days | Control | 29.5 (17.9) | 29.2 (18.9) | 30.4 (19.5) | 27.1 (19.0) | 27.6 (19.4) | 24.9 (15.7) |
| ALC | 35.3 (15.6) | 27.5 (12.9) | 26.0 (17.0) | 24.8 (14.7) | 24.6 (13.5) | 21.7 (13.5) | |
| HIV | 35.4 (20.4) | 28.7 (19.7) | 28.1 (22.2) | 25.6 (18.9) | 27.0 (16.8) | 28.5 (19.8) | |
| ALC + HIV | 26.2 (14.2) | 28.5 (21.5) | 24.3 (17.3) | 27.4 (20.0) | 25.3 (20.6) | 26.5 (18.8) | |
| Drinks per | Control | 5.1 (2.4) | 5.0 (2.4) | 5.0 (2.1) | 5.3 (2.4) | 5.0 (2.7) | 5.1 (2.9) |
| Drinking Day | ALC | 5.9 (3.2) | 5.2 (2.9) | 4.2 (2.0) | 4.3 (2.0) | 4.4 (2.1) | 4.0 (2.1) |
| HIV | 7.1 (3.1) | 6.3 (3.9) | 6.2 (3.8) | 6.7 (5.3) | 6.8 (5.2) | 6.1 (4.3) | |
| ALC + HIV | 6.3 (3.8) | 5.3 (2.8) | 5.3 (2.8) | 5.1 (2.4) | 5.0 (2.6) | 5.2 (2.6) | |
| Occurrences of | Control | 37.8 (45.4) | 30.4 (32.7) | 23.2 (23.8) | 22.1 (24.3) | 19.2 (22.3) | 17.6 (20.6) |
| Unprotected Sex | ALC | 29.7 (31.2) | 26.7 (25.4) | 17.3 (16.7) | 18.8 (17.2) | 18.2 (16.1) | 16.7 (17.8) |
| H IV | 34.7 (33.9) | 19.1 (25.4) | 16.6 (19.0) | 13.1 (19.5) | 15.5 (21.4) | 15.4 (18.8) | |
| ALC + HIV | 27.9 (17.9) | 22.1 (19.3) | 19.5 (20.3) | 20.3 (17.9) | 18.9 (18.7) | 11.7 (13.0) | |
| Number of | Control | 1.6 (0.9) | 1.4 (0.8) | 1.4 (1.1) | 1.3 (1.0) | 1.5 (1.2) | 1.3 (1.0) |
| Partners | ALC | 1.5 (1.0) | 1.2 (0.7) | 1.2 (0.6) | 1.2 (1.1) | 1.1 (0.6) | 1.1 (0.5) |
| HIV | 2.1 (1.4) | 1.2 (0.7) | 1.3 (0.8) | 1.3 (1.1) | 1.4 (1.1) | 1.6 (1.4) | |
| ALC + HIV | 2.1 (1.8) | 1.4 (0.9) | 1.6 (1.1) | 1.4 (1.1) | 1.3 (0.9) | 1.3 (1.1) | |
Notes: Control = No intervention; ALC = Alcohol risk-reduction intervention; HIV = HIV risk-reduction intervention; ALC + HIV = Combined alcohol and HIV risk-reduction intervention. All means represent data assessed in a 90-day window.
Primary Outcome Analyses
No significant interactions between time or gender and the other predictor variables were found in any analysis.
Alcohol outcomes
Baseline-adjusted drinking frequency data evidenced an Alcohol risk content X HIV risk content interaction, F (1, 131) = 6.77, p = .010, η2 = .046. Simple Alcohol risk content main effects tests revealed that drinking was less frequent during follow-up among participants in the Alcohol condition, compared to the Control condition, F (1, 131) = 5.39, p = .022, η2 = .040, but that drinking frequency outcomes did not differ significantly between those in the Combined and HIV conditions, F (1, 131) = 1.99, p = .160, η2 = .015. Simple HIV risk content main effects tests revealed that drinking frequency outcomes did not differ significantly between those in the HIV and Control conditions, F (1, 131) = 2.55, p = .113, η2 = .019, but that drinking was more frequent during follow-up among participants in the Combined condition, compared to the Alcohol condition, F (1, 131) = 4.42, p = .038, η2 = .033. A significant main effect of gender, F (1, 131) = 6.60, p = .011, η2 = .045, indicated that baseline-adjusted drinking frequency during follow-up was higher among men than among women (data not shown). A significant main effect of time also was detected, F (3.46, 452.78) = 2.84, p = .030, η2 = .020, reflecting a significant overall linear decrease in drinking frequency over the course of follow-up, F (1, 131) = 6.62, p = .011.
Baseline-adjusted drinking intensity data evidenced an Alcohol risk content main effect, F (1, 131) = 4.58, p = .034, η2 = .028, such that individuals in the Alcohol content conditions (Alcohol, Combined) drank less per drinking day during follow-up than those in the Control and HIV conditions. Although the Alcohol risk content x HIV risk content interaction was not significant, F (1, 131) = 2.24, p = .137, η2 = .014, inspection of means and results of simple main effects tests suggested that the Alcohol risk content main effect was carried by the difference between Alcohol and Control condition outcomes. Alcohol condition participants drank significantly fewer drinks per drinking day than did Control condition participants, F (1, 131) = 6.82, p = .010, η2 = .050, whereas outcomes of Combined and HIV condition participants did not differ, F (1, 131) = 0.19, p = .662, η2 = .001. No HIV risk content main effect was detected, F (1, 131) = 0.32, p = .572, η2 = .002. A significant main effect of gender, F (1, 131) = 19.57, p < .001, η2 = .122, indicated that baseline-adjusted drinking intensity during follow-up was higher among men than among women (data not shown). A significant main effect of time also was detected, F (3.12, 408.65) = 5.77, p = .001, η2 = .038, reflecting a significant overall linear decrease in drinking intensity over the course of follow-up, F (1, 131) = 11.04, p = .001.
Sexual behavior outcomes
A test of the main effect of HIV risk content on baseline-adjusted frequency of unprotected sex was not significant, F (1, 131) = 2.54, p = .114, η2 = .018, nor were tests of the main effect of Alcohol risk content, F (1, 131) = 1.81, p = .181, η2 = .013, or the interaction between HIV risk content and Alcohol risk content, F (1, 131) = 1.49, p = .225, η2 = .011. However, inspection of means and tests of simple main effects of HIV risk content indicated that participants in the HIV condition engaged in unprotected sex less frequently during follow-up than did participants in the Control condition, F (1, 131) = 4.23, p = .042, η2 = .031, whereas outcomes of those in the Combined and Alcohol conditions did not differ, F (1, 131) = 0.06, p = .801, η2 = .000. Simple main effects tests of Alcohol risk content detected no significant effects. A significant main effect of time, F (3.01, 394.27) = 3.56, p = .014, η2 = .024, reflected a significant overall linear decrease in frequency of unprotected sex over the course of follow-up, F (1, 131) = 6.65, p = .011.
Baseline-adjusted data on number of partners revealed a trend-level HIV risk content X Alcohol risk content interaction, F (1, 131) = 3.47, p = .065, η2 = .025. However, probing revealed no significant simple main effects. No other effects on this outcome were detected.
Supplemental Analyses of Alcohol Use and Sexual Behavior during Follow-up
We did not hypothesize a specific mechanism by which exposure to alcohol risk material was expected to reduce risky sexual behavior in this study. However, to explore whether any of the interventions reduced the use of alcohol in sexual contexts, we conducted supplemental analyses employing the same analytic approach as for our primary outcomes. Analyses of baseline-adjusted follow-up data (not shown) on frequency of drinking prior to sex and proportion of sex events preceded by drinking both failed to detect any significant effects of condition, as did an analysis of the total number of intercourse events during follow-up.
Intervention Integrity
Intervention session audiotapes were available for 198 of the 210 intervention sessions conducted (108 tapes from session one, 90 from session two; some tapes were missing due to equipment failure or counselor error). Agreement between the two raters of each session (defined as being within one point of each other on the four-point scale) exceeded 93% for all 13 items. Univariate ANOVAs with post hoc testing confirmed that (a) alcohol-specific intervention behaviors were equivalently present in the Alcohol and Combined conditions but absent in the HIV condition, (b) HIV risk-specific intervention behaviors were equivalently present in the HIV and Combined conditions but absent in the Alcohol condition, (c) use of general MI-consistent behaviors was high and equivalent across the three intervention conditions, and (d) use of confrontation was low and equivalent across the three conditions (details available from the first author).
Comparison of Participant Drinking Self-Reports with Collateral Reports
Within-window correlations between participant and collateral reports of participant drinking ranged from .57 to .74 for both frequency and intensity, ps < .001. Participant and collateral reports did not differ significantly except that participant drinking frequency reported by participants was slightly higher than that reported by collaterals during baseline, t(137) = 3.43, p = .001, (M days = 31.0, 26.9, SDs = 17.0, 17.3, respectively) and the 3-month follow-up window, t(127) = 2.55, p = .012, (M days = 28.2, 24.8, SDs = 17.8, 17.0, respectively).
Discussion
A two-session, alcohol-focused, motivational intervention was found to yield reduced drinking frequency and drinking intensity (relative to a no-intervention control) but had no impact on frequency of unprotected sex or number of sexual partners. In contrast, an intervention that focused solely on sexual risk for HIV infection was found to yield a reduced frequency of unprotected sex, although it too had no effect on number of partners. Although drinking frequency and intensity and unprotected sex frequency declined in the sample as a whole over the course of the 15-month follow-up period, intervention effects on these variables remained stable during follow-up, despite the brief nature of the interventions. In contrast, most studies of individual-level drinking interventions delivered to college students show diminishing differences between intervention and control groups after about six months of follow-up, particularly on measures of drinking quantity (Carey et al., 2007). Effect sizes of the detected intervention effects were in the small-to-moderate range, consistent with findings from past research on drinking reduction in college students (Carey et al., 2007) and comparing favorably to effects obtained in research on sexual risk reduction in adolescents (Johnson et al., 2003) and college students (e.g., Kiene & Barta, 2006). In concrete terms, comparing Alcohol to Control condition participants, effects on the alcohol variables during follow-up (estimated by back-transformation of baseline-adjusted means) corresponded to average between-group differences of between six and seven drinking days (per 90-day window) and one drink per drinking day. The average effect on unprotected sex frequency corresponded to roughly four fewer unprotected sex events (per 90-day window) in HIV condition participants, relative to those in the Control condition.
The finding that an alcohol-focused intervention had no effect on sexual risk behavior suggests that alcohol use among college students may be largely irrelevant to their decisions regarding whether or not to use condoms or to have sex with multiple partners. In one study of college students’ reasons for not using condoms, being drunk was rated as the least important of 10 potential reasons (Civic, 2000), and it has been noted that “the strongest predictor of condom use when intoxicated is condom use when sober” (Abbey, Parkhill, Buck, & Saenz, 2007, p. 82; see Cooper, 2010, for a contrasting perspective). Consistent with this assertion, Leigh and colleagues (2008) found in a sample of college students that drinking prior to sex did not lead to a reduced likelihood of condom use. Rather, individuals were largely consistent across events with regard to their condom use (or lack thereof), even if alcohol use varied. Similar findings have been obtained in other event-level studies (Weinhardt & Carey, 2000). On the whole, evidence suggests that alcohol use among college students is more consistently related to having multiple or casual sex partners than to a reduced likelihood of condom use (Cooper, 2002), although the present study found no evidence that intervening to address alcohol use affects the number of partners with whom students choose to have sex. Another possibility is that alcohol use has an acute effect on sexual risk behavior among relatively light drinkers but not among heavier drinkers such as those recruited for this study (see Neal & Fromme, 2007).
Some researchers argue that interventions to reduce alcohol use have limited utility as a means of reducing risky sex (Lewis, Malow, & Norman, 2008). Rather, they advocate for a more nuanced approach to addressing the role of alcohol use in risky sexual behavior. For instance, Bryan, Ray, and Cooper (2007) recommend preparing young people specifically for the potential effect of alcohol in sexual situations, and Davis and colleagues (2009) suggest that prevention programs should address effects that perceived intoxication and sexual arousal may have on sexual decision-making processes. However, few studies have examined interventions that explicitly address the potential contribution of alcohol to risky sex. Those that have taken this approach have obtained some promising findings in the form of significant effects on sexual risk behavior, but have failed to demonstrate that the combined focus yielded a greater impact than could be obtained by simply addressing risky sex as a general topic (see Bryan et al., 2009; Ingersoll et al., 2005; Naar-King et al., 2006; Rosengard et al., 2007). The impact of alcohol use on sexual behavior was discussed during the Combined intervention of the present study, although such discussion was usually minimal relative to coverage of other topics. Other recommendations have been to keep the primary focus of sexual risk-reduction interventions on factors other than alcohol use, such as promoting habitual use of condoms (Štulhofer, Ba□ak, Ajdukovi□, & Graham, 2010) even in the face of potential obstacles (Dermen et al., 1998), and especially in the context of steady relationships (Scott-Sheldon et al., 2010). To the extent that alcohol use is raised as a topic in such interventions, the most effective approach might be to consider it as just one of many possible situational barriers to risk reduction.
Present findings suggesting that a brief HIV-focused motivational intervention can reduce college students’ frequency of unprotected sex are somewhat at odds with results from other studies. For instance, in a study in which a single-session STD-prevention intervention employing both MI and skills-building components was compared to information-only and wait-list control groups (Jaworski & Carey, 2001), female college students in the MI/Skills condition had fewer partners during two months of follow-up than did wait-list control participants, but frequency of unprotected sex did not vary by condition. In another study, a brief, self-administered intervention incorporating normative feedback regarding protective behaviors also was found to reduce female college students’ number of partners (during a 30-day follow-up; Chernoff & Davison, 2005). In that study, men did increase their condom use but did not change their number of partners. In a study conducted with patients receiving short-term alcohol detoxification, a brief motivational intervention and an educational intervention, both focused on HIV/STD risk reduction, had no differential effects on either condom use or number of partners during a three-month follow-up (Brems, Dewane, Johnson, & Eldridge, 2009). With regard to current findings, an interesting question for future research is whether a stronger focus on STDs other than HIV might yield larger reductions in sexual risk behavior, given the relatively low prevalence of HIV and greater prevalence of other STDs in college students.
Given that significant intervention effects on drinking frequency, drinking intensity, and unprotected sex frequency all were evident in comparisons between a single-focus condition and a no-intervention condition (e.g., for drinking frequency, between the Alcohol and Control conditions), but generally not in comparisons between two active conditions (e.g., between the Combined and HIV conditions), it is worth considering whether positive findings may have been due to attention or other nonspecific effects of intervention, rather than being due to intervention content. However, findings that the single-focus HIV condition had no effect on alcohol use and that the single-focus Alcohol condition had no effect on unprotected sex (relative to the no-intervention Control condition) argue against this interpretation of the results. Rather, it seems likely that the amount of attention paid to either topic in the Combined intervention was insufficient, given that the total length of counselor contact in the Combined condition (105 minutes) was less than what would be obtained by adding together the two single-focus conditions (150 minutes). Also possible is that combining material on both topics in a single session overloaded participants’ ability to process and remember the material discussed. Thus, it may be that successfully addressing both alcohol use and sexual behavior in a single intervention will require multiple sessions, each of which focuses on a single topic.
Also worth examining is the possibility that failure to detect the hypothesized Alcohol content effect on unprotected sex frequency was a result of inadequate power. Again, the available evidence do not support this alternative interpretation. Inspection of baseline-adjusted means (not shown) indicates that, in this sample, participants who received Alcohol risk content (Alcohol and Combined conditions) reported more, rather than less, unprotected sex during follow-up, relative to participants in the non-Alcohol risk content conditions (although, as previously noted, this effect was not statistically significant).
In summary, the present study adds to the large body of evidence supporting the use of brief alcohol-focused motivational interventions to reduce alcohol use. Further, it provides encouraging evidence that a brief HIV-focused motivational intervention may have utility for reducing the frequency of unprotected sex among college students. Strengths of the study include use of a randomized clinical trial design, manual-guided, carefully monitored interventions, objective verification of intervention adherence and discriminability, collateral verification of participant drinking, high follow-up rates, and a 15-month follow-up window. Limitations include a relatively small sample size, absence of an active control condition that addressed a topic other than alcohol use or sexual behavior, and limited emphasis on the specific topic of alcohol-related sexual behavior in the Combined intervention. Another limitation is the higher level of attrition from follow-up among the small subset of participants who completed only one of the two intervention sessions, which suggests that present findings can be applied most confidently to students exposed to the complete intervention. Also, use of an established instrument such as the Motivational Interviewing Treatment Integrity coding system (Moyers, Martin, Manuel, & Miller, 2003) would have provided further evidence that the MI-based interventions were being delivered competently. Finally, although examination of the patterns of significant between-group baseline differences that were present for three of the four outcome variables suggests that such differences did not influence our findings, it is impossible to rule out this possibility without conducting a replication in which groups are more closely balanced on these variables (e.g., by urn randomization).
With regard to future research, further consideration of the roles of both gender and ethnicity are warranted (see Randolph et al., 2009). Men were somewhat underrepresented in the sample, and most participants were non-minority White. Among college students, there is evidence that rates of HIV and STD infection are higher among minority (e.g., Black) students than among non-minority students (e.g., James, Simpson, & Chamberlain, 2008; Wu, Ringwalt, Patkar, Hubbard, & Blazer, 2009). Thus, results of the present study cannot be assumed to apply to minority college students. Also, as suggested by the large proportion of students who did not meet eligibility criteria for this study, present results do not address how the interventions studied might affect college students who do not report recent risk behavior in both alcohol use and sexual domains. More broadly, heterosexual college students in the U.S., despite having low rates of condom use, are undoubtedly at substantially lower risk for infection with HIV than clearly documented high-risk groups such as men who sex with men, injection drug users, and residents of Sub-Saharan Africa (UNAIDS, 2009). Research on the effectiveness of alcohol-focused interventions for reducing the spread of HIV infection among the highest risk U. S. and world populations is still urgently needed (Shuper et al., 2010).
Acknowledgments
This research was supported by National Institute on Alcohol Abuse and Alcoholism grant R01 AA011714.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb.
References
- Abbey A, Parkhill MR, Buck PO, Saenz C. Condom use with a casual partner: What distinguishes college students’ use when intoxicated? Psychology of Addictive Behaviors. 2007;21:76–83. doi: 10.1037/0893-164X.21.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belcher L, Kalichman S, Topping M, Smith S, Emshoff J, Norris F, Nurss J. A randomized trial of a brief HIV risk reduction counseling intervention for women. Journal of Consulting and Clinical Psychology. 1998;66:856–861. doi: 10.1037//0022-006x.66.5.856. [DOI] [PubMed] [Google Scholar]
- Bolton R, Vincke J, Mak R, Dennehy E. Alcohol and risky sex: In search of an elusive connection. Medical Anthropology. 1992;14:323–363. doi: 10.1080/01459740.1992.9966077. [DOI] [PubMed] [Google Scholar]
- Brems C, Dewane SL, Johnson ME, Eldridge GD. Brief motivational interventions for HIV/STI risk reduction among individuals receiving alcohol detoxification. AIDS Education and Prevention. 2009;21:397–414. doi: 10.1521/aeap.2009.21.5.397. [DOI] [PubMed] [Google Scholar]
- Brown LK, Lourie KJ. Motivational interviewing and prevention of HIV among adolescents. In: Monti PM, Colby SM, O’Leary TA, editors. Adolescents, Alcohol, and Substance Abuse: Reaching Teens Through Brief Interventions. Guilford; New York: 2001. pp. 244–274. [Google Scholar]
- Bryan A, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2007;68:327–335. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Broaddus MR. HIV risk reduction among detained adolescents: A randomized, controlled trial. Pediatrics. 2009;124:e1180–e1188. doi: 10.1542/peds.2009-0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhi ER, Marhefka SL, Hoban MT. The state of the union: Sexual health disparities in a national sample of US college students. Journal of American College Health. 2010;58:337–346. doi: 10.1080/07448480903501780. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Braaten LS, Maisto SA, Gleason JR, Forsyth AD, Durant LE, Jaworski BC. Using information, motivational enhancement, and skills training to reduce the risk of HIV infection for low-income urban women: A second randomized clinical trial. Health Psychology. 2000;19:3–11. doi: 10.1037//0278-6133.19.1.3. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: Continued development and psychometric evaluation with psychiatric outpatients. International Journal of STD and AIDS. 2001;12:365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Lewis BP. Motivational strategies can enhance HIV risk reduction programs. AIDS and Behavior. 1999;3:269–276. doi: 10.1023/a:1025429216459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Maisto SA, Kalichman SC, Forsyth AD, Wright EM, Johnson BT. Enhancing motivation to reduce the risk of HIV infection for economically disadvantaged urban women. Journal of Consulting and Clinical Psychology. 1997;65:531–541. doi: 10.1037//0022-006x.65.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS and Behavior. 1997;1:61–74. [Google Scholar]
- Carey MP, Weinhardt LS, Carey KB, Maisto SA, Gordon CM, Gleason JR. Measuring sexual and substance use behavior: The timeline method; Invited paper presented at the NIMH Exploratory Conference on the Interactions of Comorbid Mental Health Factors with High Risk Sexual Behaviors: Implications for HIV/STD Transmission; Bethesda, MD. 1998, April. [Google Scholar]
- Chernoff RA, Davison GC. An evaluation of a brief HIV/AIDS prevention intervention for college students using normative feedback and goal setting. AIDS Education and Prevention. 2005;17:91–104. doi: 10.1521/aeap.17.3.91.62902. [DOI] [PubMed] [Google Scholar]
- Civic D. College students’ reasons for nonuse of condoms within dating relationships. Journal of Sex and Marital Therapy. 2000;26:95–105. doi: 10.1080/009262300278678. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Second Edition Lawrence Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Connors GJ, Walitzer KS, Dermen KH. Preparing clients for alcoholism treatment: Effects on treatment participation and outcomes. Journal of Consulting and Clinical Psychology. 2002;70:1161–1169. doi: 10.1037//0022-006x.70.5.1161. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Alcohol and increased behavioral risk for AIDS. Alcohol Health and Research World. 1992;16:64–72. [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. Journal of Studies on Alcohol. 2002;(Supplement No. 14):101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Current Directions in Psychological Science. 2006;15:19–23. [Google Scholar]
- Cooper ML. Toward a person x situation model of sexual risk-taking behaviors: illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology. 2010;98:319–341. doi: 10.1037/a0017785. [DOI] [PubMed] [Google Scholar]
- Davidson R, Raistrick D. The validity of the short alcohol dependence data (SADD) questionnaire: A short self-report questionnaire for the assessment of alcohol dependence. British Journal of Addiction. 1986;81:217–222. doi: 10.1111/j.1360-0443.1986.tb00319.x. [DOI] [PubMed] [Google Scholar]
- Davis KC, George WH, Norris J, Schacht RL, Stoner SA, Hendershot CS, Kajumulo KF. Effects of alcohol and blood alcohol concentration limb on sexual risk-taking intentions. Journal of Studies on Alcohol and Drugs. 2009;70:499–507. doi: 10.15288/jsad.2009.70.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekin B. Gender differences in HIV-related self-reported knowledge, attitudes, and behaviors among college students. American Journal of Preventive Medicine. 1996;12:61–66. [PubMed] [Google Scholar]
- Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: I. Scale development. Psychology of Addictive Behaviors. 1994;8:152–160. [Google Scholar]
- Dermen KH, Cooper ML. Inhibition conflict and alcohol expectancy as moderators of alcohol’s relationship to condom use. Experimental and Clinical Psychopharmacology. 2000;8:198–206. doi: 10.1037//1064-1297.8.2.198. [DOI] [PubMed] [Google Scholar]
- Dermen KH, Cooper ML, Agocha VB. Sex-related alcohol expectancies as moderators of the relationship between alcohol use and risky sex in adolescents. Journal of Studies on Alcohol. 1998;59:71–77. doi: 10.15288/jsa.1998.59.71. [DOI] [PubMed] [Google Scholar]
- Douglas KA, Collins JL, Warren C, Kann L, Gold R, Clayton S, Ross J, Kolbe LJ. Results from the 1995 National College Health Risk Behavior Survey. College Health. 1997;46:55–66. doi: 10.1080/07448489709595589. [DOI] [PubMed] [Google Scholar]
- Downing-Matibag TM, Geisinger B. Hooking up and sexual risk taking among college students: A health belief model perspective. Qualitative Health Research. 2009;19:1196–1209. doi: 10.1177/1049732309344206. [DOI] [PubMed] [Google Scholar]
- Gordon CM, Carey MP. Alcohol’s effects on requisites for sexual risk reduction in men: An initial experimental investigation. Health Psychology. 1996;15:56–60. doi: 10.1037//0278-6133.15.1.56. [DOI] [PubMed] [Google Scholar]
- Graves KL. Risky sexual behavior and alcohol use among young adults: Results from a national survey. American Journal of Health Promotion. 1995;10:27–36. doi: 10.4278/0890-1171-10.1.27. [DOI] [PubMed] [Google Scholar]
- Grello CM, Welsh DP, Harper MS. No strings attached: The nature of casual sex in college students. The Journal of Sex Research. 2006;43:255–267. doi: 10.1080/00224490609552324. [DOI] [PubMed] [Google Scholar]
- Grimley DM, Prochaska JO, Velicer WF, Prochaska GE. Contraceptive and condom use adoption and maintenance: A stage paradigm approach. Health Education Quarterly. 1995;22:20–35. doi: 10.1177/109019819502200104. [DOI] [PubMed] [Google Scholar]
- Hagman BT, Clifford PR, Noel NE, Davis CM, Cramond AJ. The utility of collateral informants in substance use research involving college students. Addictive Behaviors. 2007;32:2317–2323. doi: 10.1016/j.addbeh.2007.01.023. [DOI] [PubMed] [Google Scholar]
- Hoban MT, Ottenritter NW, Gascoigne JL, Kerr DL. Campus HIV prevention strategies: Planning for success. Community College Press; Washington, DC: 2003. [Google Scholar]
- Hurlbut SC, Sher KJ. Assessing alcohol problems in college students. Journal of American College Health. 1992;41:49–58. doi: 10.1080/07448481.1992.10392818. [DOI] [PubMed] [Google Scholar]
- Igra V, Irwin CE., Jr. Theories of adolescent risk-taking behavior. In: DiClemente RJ, Hansen WB, Ponton LE, editors. Handbook of adolescent health risk behavior. Plenum Press; New York: 1996. pp. 35–51. [Google Scholar]
- Ingersoll KS, Ceperich SD, Nettleman MD, Karanda K, Brocksen S, Johnson BA. Reducing alcohol-exposed pregnancy risk in college women: Initial outcomes of a clinical trial of a motivational intervention. Journal of Substance Abuse Treatment. 2005;29:173–180. doi: 10.1016/j.jsat.2005.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadack RA, Hyde JS, Keller ML. Gender and knowledge about HIV, risky sexual behavior, and safer sex practices. Research in Nursing and Health. 1995;18:313–324. doi: 10.1002/nur.4770180405. [DOI] [PubMed] [Google Scholar]
- James AB, Simpson TY, Chamberlain WA. Chlamydia prevalence among college students: Reproductive and public health implications. Sexually Transmitted Diseases. 2008;35:529–532. doi: 10.1097/OLQ.0b013e3181676697. [DOI] [PubMed] [Google Scholar]
- Jaworski BC, Carey MP. Effects of a brief, theory-based STD-prevention program for female college students. Journal of Adolescent Health. 2001;29:417–425. doi: 10.1016/s1054-139x(01)00271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaly PW, Heesacker M, Frost HM. Collegiate alcohol use and high-risk sexual behavior: A literature review. Journal of College Student Development. 2002;43:838–850. [Google Scholar]
- Kiene SM, Barta WD, Tennen H, Armeli S. Alcohol, helping young adults to have unprotected sex with casual partners: Findings from a daily diary study of alcohol use and sexual behavior. Journal of Adolescent Health. 2009;44:73–80. doi: 10.1016/j.jadohealth.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight JR, Wechsler H, Kuo M, Seibring M, Weitzman ER, Schuckit MA. Alcohol abuse and dependence among U.S. college students. Journal of Studies on Alcohol. 2002;63:263–270. doi: 10.15288/jsa.2002.63.263. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Pedersen ER, Thompson AD, Earleywine M. A brief decisional balance intervention increases motivation and behavior regarding condom use in high-risk heterosexual college men. Archives of Sexual Behavior. 2008;37:330–339. doi: 10.1007/s10508-007-9195-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaForge RG, Borsari B, Baer JS. The utility of collateral informant assessment in college alcohol research: Results from a longitudinal prevention trial. Journal of Studies on Alcohol. 2005;66:479–487. doi: 10.15288/jsa.2005.66.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AR. The social psychology of drinking and human sexuality. Journal of Drug Issues. 1985;15:273–289. [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999-2006. Addictive Behaviors. 2007;32:2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. American Psychologist. 1993;48:1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh BC, Vanslyke JG, Hoppe MJ, Rainey DT, Morrison DM, Gillmore MR. Drinking and condom use: Results from an event-based daily diary. AIDS and Behavior. 2008;12:104–112. doi: 10.1007/s10461-007-9216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis JE, Malow RM, Norman L. Does alcohol use among sexually active college students moderate HIV risk behavior? Journal of HIV/AIDS Prevention in Children & Youth. 2008;9:138–157. [Google Scholar]
- MacDonald TK, Zanna MP, Fong GT. Why common sense goes out the window: Effects of alcohol on intentions to use condoms. Personality and Social Psychology Bulletin. 1996;22:763–775. [Google Scholar]
- Markham MR, Miller WR, Arciniega L. BACCuS 2.0: Computer software for quantifying alcohol consumption. Behavior Research Methods, Instruments, and Computers. 1993;25:420–421. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. Guilford; New York, NY: 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. Guilford; New York, NY: 2002. [Google Scholar]
- Miller WR, Sovereign RG, Krege B. Motivational interviewing with problem drinkers: II. The drinker’s check-up as a preventive intervention. Behavioural Psychotherapy. 1988;16:251–268. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1994. Project MATCH Monograph Series, Volume 2. [Google Scholar]
- Moyers TB, Martin TM, Manuel JK, Miller WR. The motivational interviewing treatment integrity (MITI) code. 2nd edition. University of New Mexico; 2003. Unpublished manual. Retrieved January 12, 2011, from http://casaa.unm.edu/download/miti.pdf. [Google Scholar]
- Naar-King S, Wright K, Parsons JT, Frey M, Templin T, Lam P, Murphy D. Healthy choices: Motivational enhancement therapy for health risk behaviors in HIV-positive youth. AIDS Education and Prevention. 2006;18:1–11. doi: 10.1521/aeap.2006.18.1.1. [DOI] [PubMed] [Google Scholar]
- Neal DJ, Fromme K. Event-level covariation of alcohol intoxication and behavioral risks during the first year of college. Journal of Consulting and Clinical Psychology. 2007;75:294–306. doi: 10.1037/0022-006X.75.2.294. [DOI] [PubMed] [Google Scholar]
- Outlaw AY, Naar-King S, Parsons JT, Green-Jones M, Janisse H, Secord E. Using motivational interviewing in HIV field outreach with young African American men who have sex with men: A randomized clinical trial. American Journal of Public Health. 2010;100:S146–S151. doi: 10.2105/AJPH.2009.166991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedlow CT, Carey MP. HIV sexual risk-reduction interventions for youth: A review and methodological critique of randomized controlled trials. Behavior Modification. 2003;27:135–190. doi: 10.1177/0145445503251562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph ME, Torres H, Gore-Felton C, Lloyd B, McGarvey EL. Alcohol use and sexual risk behavior among college students: Understanding gender and ethnic differences. The American Journal of Drug and Alcohol Abuse. 2009;35:80–84. doi: 10.1080/00952990802585422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinarman C, Leigh BC. Culture, cognition, and disinhibition: notes on sexuality and alcohol in the age of AIDS. Contemporary Drug Problems. 1988;14:435–460. [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short “Readiness to Change” questionnaire for use in brief opportunistic interventions. British Journal of Addictions. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Rosengard C, Stein LAR, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R, Miranda R. Randomized clinical trial of motivational enhancement of substance use treatment among incarcerated adolescents: Post-release condom non-use. Journal of HIV/AIDS Prevention in Children & Youth. 2007;8:45–64. doi: 10.1300/J499v08n02_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge SE. Single-session motivational enhancement counseling to support change toward reduction of HIV transmission by HIV positive persons. Archives of Sexual Behavior. 2007;36:313–319. doi: 10.1007/s10508-006-9077-8. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS and Behavior. 2010;14:845–853. doi: 10.1007/s10461-008-9426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS -- A systematic review. Alcohol & Alcoholism. 2010;45:159–166. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. American Psychologist. 1990;45:921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- Štulhofer A, Ba□ak V, Ajdukovi□ D, Graham C. Understanding the association between condom use at first and most recent sexual intercourse: An assessment of normative, calculative, and habitual explanations. Social Science and Medicine. 2010;70:2080–2084. doi: 10.1016/j.socscimed.2010.02.030. [DOI] [PubMed] [Google Scholar]
- UNAIDS . 09 AIDS epidemic update. Joint United Nations Programme on HIV/AIDS (UNAIDS) and World Health Organization (WHO); Geneva, Switzerland: 2009. Rep. No. UNAIDS/09.36E / JC1700E. [Google Scholar]
- Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP, Maisto SA, Carey KB, Cohen MM, Wickramasinghe SM. Reliability of the timeline follow-back sexual behavior interview. Annals of Behavioral Medicine. 1998;20:25–30. doi: 10.1007/BF02893805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L-T, Ringwalt CL, Patkar AA, Hubbard RL, Blazer DG. Association of MDMA/ecstasy and other substance use with self-reported sexually transmitted diseases among college-aged adults: A national study. Public Health. 2009;123:557–564. doi: 10.1016/j.puhe.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of Substance Abuse Treatment. 2007;32:189–198. doi: 10.1016/j.jsat.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Zule WA, Costenbader EC, Coomes CM, Wechsberg WM. Effects of a Hepatitis C virus educational intervention or a motivational intervention on alcohol use, injection drug use, and sexual risk behaviors among injection drug users. American Journal of Public Health. 2009;99:1–8. doi: 10.2105/AJPH.2007.126854. [DOI] [PMC free article] [PubMed] [Google Scholar]