Abstract
Computer assisted surgery (CAS) was used to improve the positioning of implants during total knee arthroplasty (TKA). Most studies have reported that computer assisted navigation reduced the outliers of alignment and component malpositioning. However, additional sophisticated studies are necessary to determine if the improvement of alignment will improve long-term clinical results and increase the survival rate of the implant. Knowledge of CAS-TKA technology and understanding the advantages and limitations of navigation are crucial to the successful application of the CAS technique in TKA. In this article, we review the components of navigation, classification of the system, surgical method, potential error, clinical results, advantages, and disadvantages.
Keywords: Knee, Arthroplasty, Computer assisted navigation
Computer assisted navigation was first developed in neurosurgery to improve the accuracy and precision. This technology is particularly well suited to orthopedic surgery because bony structures and anatomic relationships remain stable between the time of image capture and surgical intervention. Computer assisted navigation was first applied in orthopedic surgery for the insertion of pedicle screws.1) The first published clinical case of computer assisted total knee arthroplasty (TKA) was performed in August 1997.2)
Currently, there are several navigation tools including OrthoPilot (Aesculap AG & Co, Tuttlingen, Germany), Vector Vision (BrainLab, Heimstetten, Germany), and Knee Track Module (Stryker Howmedica Osteonics, Allendale, NJ, USA). A recent survey showed that 33.1% of surgeons use navigation for at least 50% of their TKAs and that 25% of surgeons use navigation for 75% or more of their TKAs.3)
Limb alignment and soft tissue balancing are important for the success of TKA. Malalignment may negatively affect implant function and lead to decreased survival rate in TKA.4) The decreased survival due to malalignemnt is likely due to off-axis loading, polyethylene wear, and subsequent implant loosening.5) Therefore, components must be placed as precisely as possible and ligaments must be carefully balanced. Despite the use of manual intramedullary or extramedullary guides, significant errors in postoperative mechanical axis of greater than 3° are estimated to occur in at least 10% of TKAs, including those performed by experienced surgeons.6)
Computer assisted navigation was developed to improve the position of implants during TKA. Computer assistance achieves more accurate postoperative alignment through more precise and reproducible bony resection and ligament balancing.7,8) However, no long-term result studies or clinical trials provide evidence that navigation lowers the revision rate. Here, we review computed assisted surgery (CAS) technology, its advantages, disadvantages, applications, and the limitations of navigation.
DEFINITION
The acronym for computer assisted orthopedic surgery is CAOS. Computer assisted systems are divided into three categories: active robotic system, semi-active robotic system, and passive system.9) The earliest and most complex system was the active robotic system. Semi-active systems do not perform surgical tasks but may limit the placement of surgical tools. These systems allow the surgeon to freely operate within a predetermined safe zone and provide resistance when the surgeon's actions approach the boundaries of this zone. The most common example of a passive system is a navigation, in which information such as resection plane orientation or limb alignment is displayed on a monitor.
Registration is the process of matching the actual anatomical structures with any radiograph, fluoroscopy, or computed tomography (CT) scans that have been entered into the computer. After specifying the location of landmarks of each bone using a pointer, the computer can track the position of markers, cut surfaces, and axial alignment.
COMPONENTS OF COMPUTER ASSISTED NAVIGATION
Navigation consists of three elements: computer platform, tracking system, and rigid body marker. The tracking system visualizes the rigid body markers and tracks their motion with the help of computer processing within the three dimensional space. The marker or tracker should be attached to the patient's bones or surgical instruments to track the target objects. It corresponds to the dynamic reference base (DRB) when the target objects are the patient's bones, and it corresponds to the cutting block adaptor when the target objects are the surgical instruments or implants.
Computer Platform
The computer platform controls the coordination of inputs from the surgical field, interprets the data mathematically, and displays the resultant information on a monitor. The computer is programmed to know the shape and position of the instrument, pointer probe, and cutting block adaptor. The computer platform calculates the three-dimensional position of the trackers.
Tracking System
The tracking system consists of an optical camera, electromagnetic coil, or an ultrasonic probe to pick up infrared light, electromagnetic pulses, or ultrasonic waves, respectively, that originate from the trackers.
Optic tracking systems require two or three charged coupled device cameras to pick up infrared light from the trackers, which are recognized by three to five active emitters or passive reflective balls. Optical cameras function well when they are placed 1.8 to 2.5 m from the trackers and the line of sight is unobstructed. Validation studies of optical tracking systems have demonstrated high reliability and accuracy, with a translational error of 0.25 mm and an angular error of 1°.10) Measurement error increases with increasing distance from the camera. The disadvantages of optical tracking systems include the volume of the infrared camera, wear of reflecting balls, and the adaptation of the surgical technique to maintain the line of sight.
Electromagnetic (EM) tracking systems require a transmitter and trackers (dynamic reference frames, a pointer probe, and a paddle probe). EM tracking systems do not require reference arrays, cameras, or line of sight. The disadvantage of EM tracking systems is the distortion of the field created by metals and some non-metals. In addition, trackers are linked to the computer by wires which can be troublesome during the surgical procedure. Validation studies have shown that occasional outliers may be off by several degrees which makes this method less reliable.11)
Marker or Tracker (DRB, Pointer Probe, Cutting Block Adaptor)
Active markers emit light from a bulb and have a battery or wire as a power source. Passive markers reflect infrared light. The tracking system and its associated computer perform a triangulation process to determine the position of each marker. The computer does not detect bone. Any movement of a DRB represents movement of the bone itself. In addition to DRBs, a variety of equipment has associated markers to track the instruments. The software particular to the navigation system has been programmed with the geometry of the instrument. For example, the system can determine the location of the pointer tip and the longitudinal axis of the pointer probe.
REFERENCING
Referencing of the target objects defines points in virtual space with a pointer probe that can be triangulated by the tracking system.12) The tracking system triangulates to obtain the x, y, z coordinates of each marker, and is linked to a computer. Accuracy of imageless referencing depends on the expertise of the surgeon in choosing the correct reference points.
There are two methods of referencing: kinematic and bone morphing. Kinematic referencing is simple and useful in determining the center of the hip and ankle. Because the hip center is not directly visible, this method is accomplished by tracking the femur as it is rotated in a circular motion. The bone morphing method selects dozens of surface match points by painting the bone with a pointer probe. The created virtual image allows enhanced capabilities such as prosthetic sizing, bone resection level, and kinematic assessment.
SYSTEM CLASSIFICATIONS
Computer assisted navigation may be "closed" or "open". Closed, or proprietary, systems provide support limited to a specific prosthesis or surgical technique. Open systems are general and support implantation of various prostheses from different manufacturers.
Computer navigation systems can be grouped into three different types according to the referencing methods: CT-based, fluoroscopy based, and imageless systems.
In CT-based systems, CT scans of the femoral head, knee, and the distal tibia are performed before TKA and images are used to make a three-dimensional model. The main advantages of the CT-based system are that it is specific to the patient's anatomy and it can be used in cases of extreme deformities. The main disadvantage is that it is mandatory to obtain a CT scan which may be seen an additional expense, waste of time, or an unreasonable source of radiation for the patient.
The fluoro-based system uses an instrumented image intensifier and permits the collection of a limited number of fluoro images. While taking the fluoro images, specific markers are captured in the images allowing the computer to relate the image position to the marker position. After imaging is complete, the instrument is identified by the tracking system.
The imageless or non-image system functions without CT or fluoroscopy. The manufacturer of the navigation system obtains CT scans from a large number of patients and stores them in a database. During TKA, multiple landmarks are obtained from surface points, such as femoral epicondyles and tibial plateaus, or from kinematic algorithms to determine joint centers. The database morphs a model of the femur and tibia that best fits the registered surface points. The main advantages of the imageless system are the avoidance of a CT scan and its irradiation. However, information concerning the rotational positioning of the implants is questionable and this method relies on the surgeon's ability to indicate bony landmarks using a pointer. This system is the simplest and most widely used computer assisted tools for TKA.
SURGICAL METHODS
Image-free navigation is the most common navigation technique. Therefore, we will focus on issues of the registration step in this article. The DRB is rigidly fixed to the femur and tibia because any movement creates an error. Two pins of 3 mm diameter is preferred to single 5 mm pins with bicortical fixation to avoid incidental fracture.13) Femoral pins in the medial femoral condyle or in a percutaneous transepicondylar position are carefully placed to avoid neurovascular injury. The hip center is determined using kinematic referencing.9) Registration of the anatomical landmarks around the knees is the most critical step for the surgeon as well as the most likely source of error. The distal femoral center is defined by the computer by the point under the roof of the intercondylar notch and lies on the transepicondylar and anteroposterior (AP) axis of Whiteside. The surgical depression is the reference for the medial epicondyle. The lateral prominent point is the reference for the lateral epicondyle. For the tibial reference, the transverse tibial axis is a line that connects the AP mid points of the medial and lateral condylar surfaces. The transverse tibial axis should approximate the transepicondylar axis in regards to coupled rotation. The proximal tibial center is the bisection of the transverse axis and AP axis of the proximal tibia. Identifying landmarks on the distal femur and proximal tibia are highly variable.14) In sight of this variance, some systems use the kinematic referencing of the knee to establish the average axis of knee rotation.6,9) Anatomical and kinematic methods have been developed to locate the ankle center. Anatomic methods require the surgeon to digitize the surface points of medial and lateral malleoli. Computer soft ware picks a point on the transmalleolar axis which is 40% from the most medial point.
The check points can be validated throughout the procedure to avoid the development of tracker error. Computer assisted navigation may then be used to assess each step, including bony resections and ligament balancing.
Computerized navigation is not a failsafe method. Surgeons must be aware of the assumptions and default settings built into the computer systems. The bony landmarks should be located accurately on the imageless system. If the landmarks are not accurately localized, no computer can compensate for this. Navigation will be less accurate in revision TKA or primary TKA with distorted bony anatomy than in primary TKA of simple cases.15) This limitation could be understood from the fact that navigation cannot find things which surgeon cannot define and point out.
POTENTIAL ERRORS
Aside from technical errors inherent in the registration process, some errors exist in the abilities of the computer and tracking system to place markers. This error generally ranges from 0.1-1 mm for each of the three x, y, and z coordinates. Additional errors may occur when bony landmarks are pointed. The pointer can miss the bone due to the overlying soft tissue and cartilage. In addition, the navigation system could malfunction when there are dirty reflectors or camera. If the patient has severe osteopenia, the pins placed in the bones to hold the trackers may move, making all further measurement inaccurate. Because only the cutting guides are navigated, the surgeons may make an error during the bone resection by bending the saw blade, especially when attempting to cut through the sclerotic area of bone. Also, differences in cement thickness during implantation may lead to malalignment even though the bone resection is accurate.
CLINICAL RESULTS
CAS-TKA has demonstrated that the mechanical axis and the position of components are significantly better than those determined by the conventional technique (Figs. 1-3).5,7,10,16,17) It aslo reduces outliers and decreases the standard deviation.5,16) Mason et al.5) performed a meta-analysis to compare the alignment outcomes for CAS-TKA versus conventional TKA. They reported that mechanical axis malalignment of greater than 3° occurred in 9.0% of CAS-TKA versus 31.8% of conventional TKA. Navigation systems can also increase accuracy, precision, and repeatability of TKA.18,19)
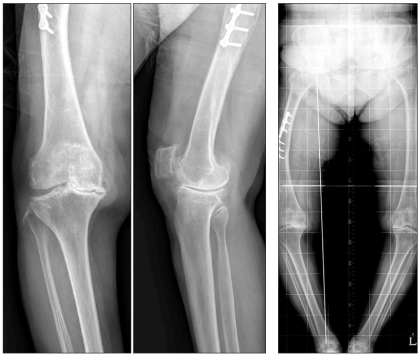
Fig. 1.
Application of a computer assisted navigation in total knee arthroplasty for a patient with extra-articular deformity. A 74-year-old man had malunion after fracture of the femoral shaft. In the preoperative roentgenogram, the mechanical axis was varus 29.3°.
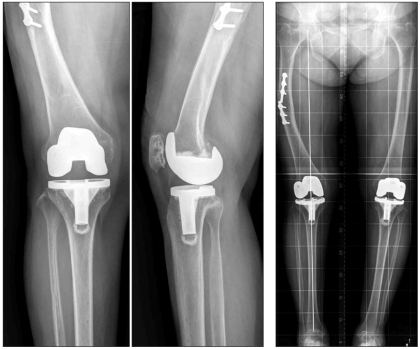
Fig. 3.
Accuracy of postoperative limb alignment in total knee arthroplasty (TKA) using a computer assisted navigation. In the postoperative 2 year roentgenogram of the same patient shown in Figs. 1 and 2, the mechanical axis was valgus 0.5° after TKA using the computer assisted navigation.
Although the coronal and sagittal alignment of the individual components can also be improved with navigation, a debate still exists as to whether a navigation does20,21) or does not22,23) improve the rotational alignment of the femoral and tibial component. The assessment of the transepicondylar axis or the AP axis seems to be inconsistent compared to mechanical axis alignment. Because the positioning of the medial epicondylar sulcus may be incorrect and the discrimination between the surgical and anatomical transepicondylar axis may be difficult, errors in judgement for femoral rotation can occur.24)
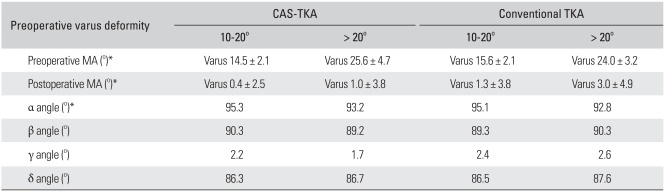
Some authors criticized the advantage of CAS-TKA. Bauwens et al.25) reported that CAS provided few advantages compared with the conventional technique by meta-analysis. They found that CAS increased the length of operative time by 23% and did not significantly improve the accuracy of the mechanical axes alignments. Chauhan et al.21) believed that standing radiographs may be prone to measurement error, making them less accurate than computer-generated findings. We performed a comparative analysis of CAS-TKA and conventional TKA in varus deformity of more than 10°.26) Patients with a preoperative varus deformity of more than 20° tended to have more postoperative varus mechanical alignment than those with a preoperative varus deformity between 10° and 20° in both CAS-TKA and conventional TKA (Table 1). This study showed that careful registration of the femoral mechanical axis is required in CAS-TKA for patients with severe varus deformity. The possibility of insufficient femoral valgus resection and inadequate positioning of intramedullary rod should be recognized in conventional TKA.
Table 1.
Differences in Measured Angle between CAS-TKA and Conventional TKA According to Severity of Preopertive Varus Deformity
CAS: computer assisted surgery, TKA: total knee arthroplasty, MA: angle between the femoral and tibial mechanical axes.
*p < 0.05 between groups divided according to the preoperative varus deformity.
Although many reports refer to the benefits of computer assisted TKA in reducing radiographic outliers, there are few reports about the clinical benefits in the mid- and long-term periods.27) Although two recent case-control studies with mid-term follow-up periods28,29) concluded that there was no significant difference in functional outcomes despite the better alignment in the navigated group, this does not discount the possibility that CAS could be more cost-effectiveness over a longer period of time.28,29) However, Ishida et al.30) investigated the clinical results of CAS-TKA and conventional TKA after a minimum of 5 years and reported that ROM and knee score were significantly better in the navigation group than in the conventional group.
Additional sophisticated studies are necessary to determine if the improvement of alignment will improve long-term clinical results and increase the survival rate of implants.
DEBATING ISSUES
Blood Loss
The breaching of the medullary canal using an intramedullary guide system is postulated to cause significant blood loss during conventional TKA. Although some authors have shown that blood loss and transfusion rates are significantly reduced when navigation is used,21,31) others have denied this finding and have shown that there is no significant difference in blood loss following computer assisted versus conventional TKA.6,9)
Embolic Events
Conventional TKA using an intramedullary guide can potentially cause fat embolism due to the elevated intramedullary pressures generated by the alignment rods. Fat embolism associated with the use of the intramedullary alignment rods might be reduced with navigation.9) One study comparing CAS-TKA with the conventional technique observed a higher rate of acute postoperative confusional state with the conventional technique.21) This was attributed to transient hypoxia caused by fat embolism although none of the patients suffered any long term sequelae. However, most studies comparing these two methods have not shown any significant differences in postoperative thromboembolic events.25,32)
Fractures
Potential complication are the fracture of the femur or tibia due to the fixation of the reference arrays and technical failures such as drill and pin breakages. However, these complications do not occur at significant levels.21,25)
ADVANTAGES
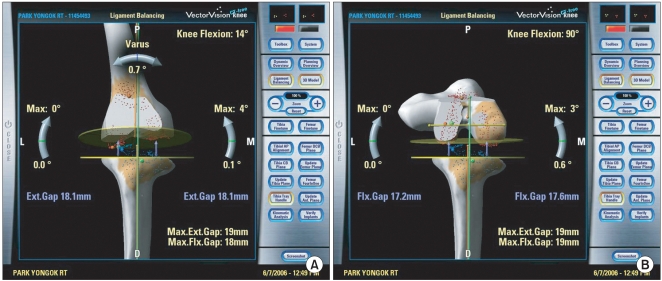
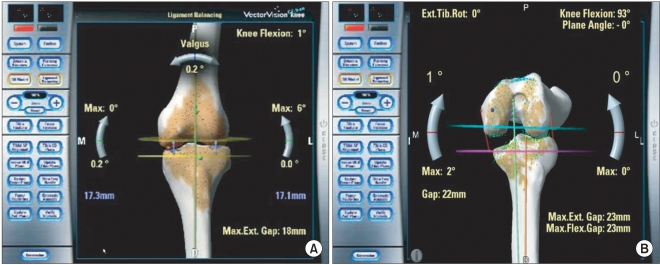
The advantages of computer assisted navigation are increasing the accuracy of bony resection and decreasing the chance of malposition of the implants. The surgeon can estimate the level of femoral and tibial joint line intraoperatively (Fig. 2). This also helps soft tissue balancing and can quantify the size of the gap and the stability (Fig. 3).
Fig. 2.
Soft tissue balancing under navigation guide in total knee arthroplasty. Navigation helps to check the balance of extension gap (A) and flexion gap (B).
Most surgeons are impressed by the navigation since they can see that the component position initially determined by the conventional technique is frequently inaccurate. The errors usually are small, but the combination of the both femoral and tibial components in a similar direction could lead to a considerable inaccuracy. In addition, navigation can be used in teaching laboratories and operating rooms as training tools for less experienced surgeons and can serve as a valuable research tool.9,33)
DISADVANTAGES
Computer assisted navigation requires new instrumentation and increases the operative time by up to 20 minutes.9,15,34) Another possible complication of CAS is an increased incidence of deep infection due to the longer exposure time.
The procedures appear cumbersome in comparison to those of the conventional technique. It may require a number of cases before the surgeon feels comfortable with the navigation system.6) The present cost of most navigation systems may limit its use for low-volume institutions.
Computer assisted TKA using the medial parapatellar approach is associated with a delayed recovery of the quadriceps during early postoperative rehabilitation because of the additional quadriceps dissection required to place the femoral referencing array.
APPLICATION TO REVISION TKA
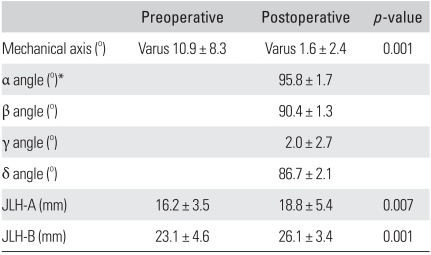
Previous surgery and bone loss make it difficult to detect anatomical landmarks and to find an accurate position for the prosthesis in revision TKA. The navigation system not only finds a more accurate position from the coronal and sagittal planes, but it also reduces the probability of technical error by allowing the surgeon to check the joint line height and the mechanical axis at every step of the procedure (Figs. 4-6). Recently, we performed a prospective study of 21 patients with a mean follow-up period of 4.8 years after revision TKA using CAS.35) Average knee and function scores improved from 40.2 and 34.8 to 89.5 and 76.9, respectively. Average mechanical axis improved from varus 10.9° to varus 1.6°. Eighteen of 21 patients (85.7%) had a mechanical axis within ± 3° from neutral alignment. The joint line height has significant correlation between preoperative and last follow-up measurement (Table 2).
Fig. 4.
Application of computer assisted surgery technique in revision total knee arthroplasty. Preoperative weight-bearing roentgenogram shows a varus deformity due to severe polyethylene wear.
Fig. 6.
Accuracy of postoperative limb alignment in revision total knee arthroplasty (TKA) using computer assisted surgery (CAS) technique. At 5.2 years after CAS-revision TKA of the same patient shown in Figs. 4 and 5, neutral limb alignment and stable implant position were maintained.
Table 2.
Mechanical Axis, Position of Implant, and Joint Line Height after CAS-revision TKA
CAS: computer assisted surgery, TKA: total knee arthroplasty, JLH-A: a distance of joint line height from the tip of the fibular styloid to the lower margin of the femoral component, JLH-B: a distance of joint line height from the medial epicondyle to the lower margin of the femoral component.
However, some difficulties exist with the use of CT-based systems. Three dimensional reconstruction is more demanding due to artifacts and the interpretation of such modified images may be erroneous. For imageless systems, registration may be difficult because implants may be unstable and bone loss may be severe enough to cause inaccuracies in defining surgical landmarks. Therefore, careful registration with either kinematic analysis or with anatomic landmarks is required under such conditions. Furthermore, the market for revision arthroplasty is smaller and companies are probably less committed to invest money. In the future, it is probable that some specific instruments and soft ware will be designed for CAS-revision TKA.
THE FUTURE
Questions remain about whether the cost saving realized from reducing the outliers of alignment and revision rate will outweigh the initial cost of the navigation systems. It also could be argued that navigation may not be worthy of the investment of time and money by the high volume expert. Future studies should have high methodological standards including randomization, follow-up periods, and control of preoperative, intraoperative, and postoperative protocols.
To further investigate the advantages and disadvantages of CAS, it is necessary to ascertain kinematic patterns of patients before and after surgery. The main criticism of using navigation systems to characterize knee kinematics is that data are acquired under passive manipulation. Future research should define the relationship between the passive kinematics measured in the operating room and the active kinematics in daily living activity.
Development of navigation systems would address major challenges in TKA, enabling less invasive surgery. Less invasive TKA could potentially enhance patient recovery and function following TKA. Navigation systems may aid in this procedure by guiding the surgeon's actions when the visual field is limited through a smaller incision.
The navigation soft ware will evolve to be more convenient and accurate. The navigation equipment will likely become less expensive, simpler, and easier.
CONCLUSION
A major benefit of computer assisted navigation is the reduction of mechanical axis and component positioning outliers. In addition, navigation allows for a more accurate and reproducible evaluation of component sizing, kinematics, and ligament balancing. However, additional study will be necessary to determine whether the improvement in implant alignment influences long-term results and survival rate to off set the increased surgical time and potential complications of CAS.
An orthopedic surgeon's experience, adaptability, and knowledge of CAS-TKA are crucial to the success of CAS-TKA. Only orthopedic surgeons who clearly understand the technology, goals, surgical method, potential error, and limitations of navigation can decide whether the use of navigation systems are appropriate for a specific case.
Fig. 5.
Soft tissue balancing under navigation guide in revision total knee arthroplasty (TKA). Navigation helps to check the balance of extension gap (A) and flexion gap (B) in revision TKA.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Merloz P, Tonetti J, Cinquin P, Lavallee S, Troccaz J, Pittet L. Computer-assisted surgery: automated screw placement in the vertebral pedicle. Chirurgie. 1998;123(5):482–490. doi: 10.1016/s0001-4001(99)80077-4. [DOI] [PubMed] [Google Scholar]
- 2.Krackow KA, Bayers-Thering M, Phillips MJ, Bayers-Thering M, Mihalko WM. A new technique for determining proper mechanical axis alignment during total knee arthroplasty: progress toward computer-assisted TKA. Orthopedics. 1999;22(7):698–702. [PubMed] [Google Scholar]
- 3.Friederich N, Verdonk R. The use of computer-assisted orthopedic surgery for total knee replacement in daily practice: a survey among ESSKA/SGO-SSO members. Knee Surg Sports Traumatol Arthrosc. 2008;16(6):536–543. doi: 10.1007/s00167-008-0518-x. [DOI] [PubMed] [Google Scholar]
- 4.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994;(299):153–156. [PubMed] [Google Scholar]
- 5.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Stulberg SD, Loan P, Sarin V. Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am. 2002;84(Suppl 2):90–98. [PubMed] [Google Scholar]
- 7.Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: comparison with conventional methods. J Arthroplasty. 2005;20(7 Suppl 3):132–138. doi: 10.1016/j.arth.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 8.Catani F, Biasca N, Ensini A, et al. Alignment deviation between bone resection and final implant positioning in computer-navigated total knee arthroplasty. J Bone Joint Surg Am. 2008;90(4):765–771. doi: 10.2106/JBJS.G.00293. [DOI] [PubMed] [Google Scholar]
- 9.Siston RA, Giori NJ, Goodman SB, Delp SL. Surgical navigation for total knee arthroplasty: a perspective. J Biomech. 2007;40(4):728–735. doi: 10.1016/j.jbiomech.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 10.Pitto RP, Graydon AJ, Bradley L, Malak SF, Walker CG, Anderson IA. Accuracy of a computer-assisted navigation system for total knee replacement. J Bone Joint Surg Br. 2006;88(5):601–605. doi: 10.1302/0301-620X.88B5.17431. [DOI] [PubMed] [Google Scholar]
- 11.Graydon AJ, Malak S, Anderson IA, Pitto RP. Evaluation of accuracy of an electromagnetic computer-assisted navigation system in total knee arthroplasty. Int Orthop. 2009;33(4):975–979. doi: 10.1007/s00264-008-0586-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khadem R, Yeh CC, Sadeghi-Tehrani M, et al. Comparative tracking error analysis of five different optical tracking systems. Comput Aided Surg. 2000;5(2):98–107. doi: 10.1002/1097-0150(2000)5:2<98::AID-IGS4>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 13.Mihalko WM, Duquin T, Axelrod JR, Bayers-Thering M, Krackow KA. Effect of one- and two-pin reference anchoring systems on marker stability during total knee arthroplasty computer navigation. Comput Aided Surg. 2006;11(2):93–98. doi: 10.3109/10929080600668122. [DOI] [PubMed] [Google Scholar]
- 14.Jenny JY, Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand. 2004;75(1):74–77. doi: 10.1080/00016470410001708150. [DOI] [PubMed] [Google Scholar]
- 15.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;(433):152–159. doi: 10.1097/01.blo.0000150564.31880.c4. [DOI] [PubMed] [Google Scholar]
- 16.Bathis H, Perlick L, Tingart M, Luring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty: a comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86(5):682–687. doi: 10.1302/0301-620x.86b5.14927. [DOI] [PubMed] [Google Scholar]
- 17.Decking R, Markmann Y, Fuchs J, Puhl W, Scharf HP. Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20(3):282–288. doi: 10.1016/j.arth.2004.09.047. [DOI] [PubMed] [Google Scholar]
- 18.Bae DK, Yoon KH, Song SJ, Kim SG, Park KJ. Intraoperative versus postoperative measurement in total knee arthroplasty using computer-assisted orthopaedic surgery (CAOS): accuracy of CAOS. J Korean Orthop Assoc. 2005;40(2):168–173. [Google Scholar]
- 19.Bae DK, Yoon KH, Song SJ, Kim SG, Im YJ, Kim MH. Comparative analysis of radiologic measurement according to TKR using computer assisted surgery and conventional TKR. J Korean Orthop Assoc. 2005;40(4):398–402. [Google Scholar]
- 20.Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;(426):180–186. doi: 10.1097/01.blo.0000136835.40566.d9. [DOI] [PubMed] [Google Scholar]
- 21.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computerassisted knee arthroplasty versus a conventional jig-based technique: a randomised, prospective trial. J Bone Joint Surg Br. 2004;86(3):372–377. doi: 10.1302/0301-620x.86b3.14643. [DOI] [PubMed] [Google Scholar]
- 22.Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005;87(10):2276–2280. doi: 10.2106/JBJS.D.02945. [DOI] [PubMed] [Google Scholar]
- 23.Siston RA, Goodman SB, Patel JJ, Delp SL, Giori NJ. The high variability of tibial rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:65–69. doi: 10.1097/01.blo.0000229335.36900.a0. [DOI] [PubMed] [Google Scholar]
- 24.Yau WP, Leung A, Chiu KY, Tang WM, Ng TP. Intraobserver errors in obtaining visually selected anatomic landmarks during registration process in nonimage-based navigation-assisted total knee arthroplasty: a cadaveric experiment. J Arthroplasty. 2005;20(5):591–601. doi: 10.1016/j.arth.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Bauwens K, Matthes G, Wich M, et al. Navigated total knee replacement: a meta-analysis. J Bone Joint Surg Am. 2007;89(2):261–269. doi: 10.2106/JBJS.F.00601. [DOI] [PubMed] [Google Scholar]
- 26.Bae DK, Yoon KH, Kim SG, Park JW, Shin MC, Roh JH. Comparison of radiologic measurements of total knee replacement using computer-assisted navigation system and conventional system in varus deformity of the knee. J Korean Orthop Assoc. 2007;42(2):227–235. [Google Scholar]
- 27.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. 2009;24(4):570–578. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Molfetta L, Caldo D. Computer navigation versus conventional implantation for varus knee total arthroplasty: a case-control study at 5 years follow-up. Knee. 2008;15(2):75–79. doi: 10.1016/j.knee.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Spencer JM, Chauhan SK, Sloan K, Taylor A, Beaver RJ. Computer navigation versus conventional total knee replacement: no difference in functional results at two years. J Bone Joint Surg Br. 2007;89(4):477–480. doi: 10.1302/0301-620X.89B4.18094. [DOI] [PubMed] [Google Scholar]
- 30.Ishida K, Matsumoto T, Tsumura N, et al. Mid-term outcomes of computer-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1107–1112. doi: 10.1007/s00167-010-1361-4. [DOI] [PubMed] [Google Scholar]
- 31.Kalairajah Y, Simpson D, Cossey AJ, Verrall GM, Spriggins AJ. Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br. 2005;87(11):1480–1482. doi: 10.1302/0301-620X.87B11.16474. [DOI] [PubMed] [Google Scholar]
- 32.Kim YH, Kim JS, Hong KS, Kim YJ, Kim JH. Prevalence of fat embolism after total knee arthroplasty performed with or without computer navigation. J Bone Joint Surg Am. 2008;90(1):123–128. doi: 10.2106/JBJS.G.00176. [DOI] [PubMed] [Google Scholar]
- 33.Stulberg SD. Computer navigation as a teaching instrument in knee reconstruction surgery. J Knee Surg. 2007;20(2):165–172. doi: 10.1055/s-0030-1248038. [DOI] [PubMed] [Google Scholar]
- 34.Hart R, Janecek M, Chaker A, Bucek P. Total knee arthroplasty implanted with and without kinematic navigation. Int Orthop. 2003;27(6):366–369. doi: 10.1007/s00264-003-0501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bae DK, Yoon KH, Kim SG, Park KJ. Efficacy of computer assisted surgery in revision total knee arthroplasty. J Korean Orthop Assoc. 2006;41(6):974–980. [Google Scholar]