Abstract
Background
There have been few outcomes studies with follow-up after performing ulnar shortening osteotomy for ulnar impaction syndrome. We investigated the long-term clinical and radiological outcomes of ulnar shortening osteotomy for the treatment of idiopathic ulnar impaction syndrome.
Methods
We retrospectively reviewed 36 patients who had undergone ulnar shortening osteotomy for idiopathic ulnar impaction syndrome for a mean follow-up of 79.1 months (range, 62 to 132 months). The modified Gartland and Werley scores were measured pre- and postoperatively. The radiographic parameters for the assessment of the distal radioulnar joint (DRUJ) as well as the relationship between these radiographic parameters and the clinical and radiological outcomes were determined.
Results
The average modified Gartland and Werley wrist score improved from 65.5 ± 8.1 preoperatively to 93.4 ± 5.8 at the last follow-up visit. The average preoperative ulnar variance of 4.7 ± 2.0 mm was reduced to an average of -0.6 ± 1.4 mm postoperatively. Osteoarthritic changes of the DRUJ were first seen at 34.8 ± 11.1 months follow-up in 6 of 36 wrists (16.7%). Those who had osteoarthritic changes in the DRUJ had significantly wider preoperative ulnar variance, a longer distal radioulnar distance and a greater length of ulnar shortening, but the wrist scores of the patients who had osteoarthritic changes in the DRUJ were comparable to those who did not have osteoarthritic changes in the DRUJ.
Conclusions
The clinical outcomes are satisfactory for even more than 5 years after ulnar shortening osteotomy for treating idiopathic ulnar impaction syndrome despite the osteoarthritic changes of the DRUJ. The patients who need a larger degree of ulnar shortening may develop DRUJ arthritis.
Keywords: Idiopathic ulnar impaction syndrome, Ulnar shortening osteotomy, Long-term outcome, Osteoarthritis, Distal radioulnar joint
Ulnar impaction syndrome can cause medial wrist pain related to excessive weight bearing across the ulnar aspect of the wrist.1) Idiopathic ulnar impaction syndrome is frequently seen radiographically in patients with static positive ulnar variance or dynamic positive ulnar variance with wrist pronation and a forceful grip.1,2)
Although ulnar shortening osteotomy has been successfully used for treating idiopathic ulnar impaction syndrome,3-5) several long term studies showed that 28-38% of the patients had radiographic degenerative changes in the distal radioulnar joint (DRUJ) 2-6 years after this procedure.4,6,7) Koppel et al.6) suggested that such changes are due to joint remodeling and they are unlikely to lead to symptomatic osteoarthritis because these patients were symptom-free. However, Sagerman et al.8) reported that one of their patients who had undergone ulnar shortening osteotomy developed symptomatic distal radioulnar arthritis. Nishiwaki et al.9) showed that the greater the amount of ulnar shortening, the higher the peak pressure is at the DRUJ, suggesting that excessive pressure at the DRUJ can lead to osteoarthritis of this joint. Furthermore, morphological variations in the DRUJ may influence the congruity and the pressure at the DRUJ after ulnar shortening osteotomy.8,10,11)
There have been few reports with regard to the long term outcomes of ulnar shortening osteotomy. Here we hypothesize that the preoperative DRUJ types and shortening length may affect the long term outcomes of ulnar shortening osteotomy. Thus, we evaluated the clinical and radiographic outcomes of ulnar shortening osteotomy in patients who have idiopathic ulnar impaction syndrome with a minimum of 5 years follow-up.
METHODS
This study was approved by the Institutional Review Board of Seoul National University Hospital and informed consent was obtained from all the enrolled patients.
Demographic and Surgical Data
Thirty six patients with idiopathic ulnar impaction syndrome were treated with ulnar shortening osteotomy and they were followed for a minimum of five years (range, 62 to 132 months). The average duration of postoperative follow-up was 79.1 ± 15.7 months. There were 12 men and 24 women with an average age of 45.8 ± 11.5 years. None of them had a history of wrist or forearm fracture or premature growth arrest.
The diagnosis was made by the medical history and physical examination, including the use of a provocative maneuver such as the ulnocarpal stress test,1) and the plain radiographs, which showed static or dynamic positive ulnar variance12) with or without cystic change(s) of the lunate or triquetrum.
The inclusion criteria for the diagnosis were 1) the absence of trauma to the forearm and wrist; 2) symptoms of ulnar wrist pain that are aggravated by pronation and ulnar deviation of the wrist with activities such as opening a jar, squeezing a wet towel, typing or shift ing gears; 3) a positive provocation test (the ulnocarpal stress test); 4) positive ulnar variance with or without cystic change(s) of the carpus seen on plain X-rays; and 5) a follow-up period of more than 5 years.
The exclusion criteria were 1) radiologic evidence of old fracture of the forearm or wrist; 2) radiologic evidence of congenital anomalies such as a Madelung deformity;3) and 3) less than 5 years follow-up.
A shortening transverse osteotomy was performed to obtain a final ulnar variance between 0 and -1 mm. This was fixed with a six or seven-hole 3.5 mm standard compression plate (25 cases) or a one-third tubular plate (Stryker Trauma, Selzach, Switzerland) when the ulna was too small for a standard compression plate (11 cases). A postoperative long arm splint was applied for the first two weeks, and this was followed by a removable long arm splint for 4 to 8 weeks.13)
Clinical Evaluations
All 36 wrists of 36 patients were evaluated preoperatively using the Gartland and Werley evaluation scoring system, as modified by Chun and Palmer.5) In this grading system, equal emphasis was placed on the subjective and objective findings and with giving 50 points to these two sets of findings for a maximum score of 100 points. The subjective variables were pain, function and motion and the objective measurements were the range of motion, the grip and pinch strength, healing of the osteotomy and the preoperative and postoperative ulnar variance. The result was excellent when the wrist score was 91 to 100, good when it was 81 to 90, fair when it was 66 to 80 and poor when it was 0 to 65. The patients were evaluated postoperatively every two to four weeks until radiologic union was confirmed, and the wrist scores were obtained at six months and once yearly thereafter.
Radiographic Evaluations
All the radiographic images were digitally acquired using a picture archiving and communication system (PACS, M-view, Infinitt, Korea) and measurements were done using PACS soft ware. The radiographs of the wrist were evaluated by two authors. Intra-observer reliability was evaluated by asking one examiner to repeat all the radiographical assessments after a period of 3 weeks. Inter-observer reliability was evaluated by asking another author to verify all the radiographical assessments.
The anteroposterior images of the wrist were taken with the shoulder in 90 degrees abduction, the elbow in 90 degrees flexion and the forearm in neutral rotation. The lateral images were taken with 0° shoulder abduction, and with the elbow and forearm maintaining the same amount of flexion and rotation.
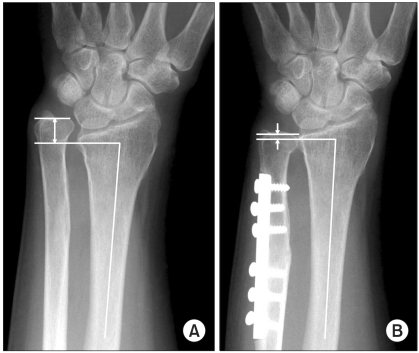
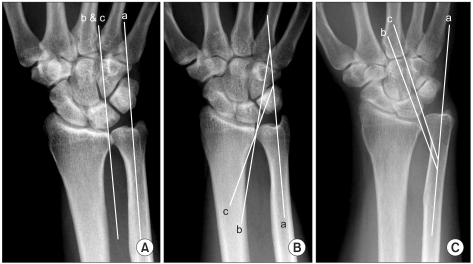
Ulnar variances were measured by the method of perpendiculars, whereby a line is drawn perpendicular to the longitudinal axis of the radius at its distal ulnar aspect, and the distance between this point and the line at the end of the ulna is measured (Fig. 1).14) Dorsal subluxation of the DRUJ was quantified preoperatively by measuring the radioulnar distance15) on a true lateral radiograph of the wrist, in which the pisoscaphoid distance was less than 3 mm (Fig. 2).
Fig. 1.
(A) Measurement of ulnar variance (arrow) on the preoperative anteroposterior wrist radiograph. (B) Measurement of ulnar variance (arrows) on the postoperative anteroposterior wrist radiograph.
Fig. 2.
(A) The preoperative lateral radiograph showed the measurement of the radioulnar distance (RU). The pisoscaphoid distance (PS) was used to define a true lateral radiograph of the wrist. (B) The postoperative lateral radiograph showed a decrease in the RU.
The types of the DRUJ have been classified by Tolat et al.16) as follows (Fig. 3).
Fig. 3.
Types of the distal radioulnar joint (DRUJ). (A) Type I: The apposing joint surfaces (b & c) are parallel to the long axis of the ulna (a). (B) Type II: The apposing joint surfaces (b & c) are oblique to the long axis of the ulna (a). The sigmoid notch and the ulnar seat angles are positive. (C) Type III: The apposing joint surfaces (b & c) are reversely oblique to the long axis of the ulna (a). The sigmoid notch and the ulnar seat angles are negative.
Type I: The apposing joint surfaces are parallel to the longitudinal axis of the ulna.
Type II: The apposing joint surfaces are oblique (the sigmoid notch angle being positive).
Type III: The apposing joint surfaces are in a rever se oblique (the sigmoid notch angle being negative).
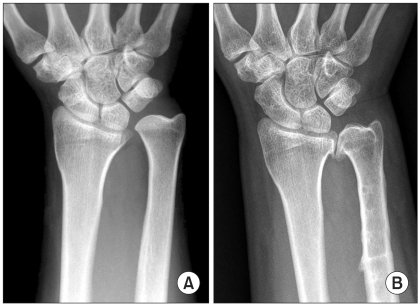
We defined osteoarthritic changes of the DRUJ as any osteophyte formation seen around the DRUJ on the plain radiography (Fig. 4).
Fig. 4.
(A) Positive ulnar variance was seen on the preoperative anteroposterior wrist radiograph. No osteoarthritic changes of the distal radioulnar joint (DRUJ) were seen. (B) Osteoarthritic changes of the DRUJ after a follow-up period of 44 months.
Statistical Analysis
The wrist scores and ulnar variances were analyzed using paired Student's t-tests. Correlation analyses were performed to assess for any associations between the ulnar variance and the radioulnar distance. The Mann-Whitney U-test was also used for comparisons between the group with DRUJ arthritis and those who did not have DRUJ arthritis. Cronbach's α test was used to measure the intraand interobserver reliability. A p-value of < 0.05 was considered statistically significant.
RESULTS
Clinical Evaluations
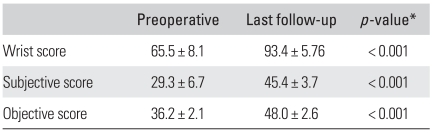
The average scores had improved from 65.5 ± 8.1 preoperatively to 93.4 ± 5.8 at the last follow-up visit (p < 0.001, paired Student's t-tests). Each component of the wrist score demonstrated statistically significant improvement (Table 1).
Table 1.
The Outcomes According to the Chun and Palmer Wrist Grading System
Values are presented as mean ± SD.
*p using paired Student t-tests.
There were no nonunions or infections. Two patients developed postoperative reflex sympathetic dystrophy, which improved at 9 months and 11 months, respectively, after the operation. Both the patients' wrist scores were favorable at the last follow-up. One patient was diagnosed with post-motor vehicle accident myofascial pain syndrome after surgery, and the final wrist score was fair.
Radiographic Findings
The inter-observer reliabilities of the radiographic measurements (the type of DRUJ, the perioperative ulnar variance and the radioulnar distance) were 0.95, 0.84, and 0.86, respectively (Cronbach α coefficient value). The intra-observer reliablities of the radiographic measurements were 0.97, 0.90 and 0.88, respectively. These results indicated that the measurements were reliable, as taken by a single observer (one of the authors) and they were used in the analyses.
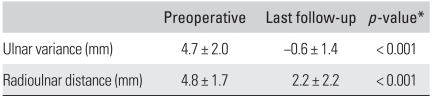
The preoperative ulnar variance was 4.7 ± 2.0 mm, and the postoperative ulnar variance was -0.6 ± 1.4 mm (p < 0.001, the paired Student's t-test). The shortened length was on average 5.3 ± 2.2 mm.
The mean radioulnar distance was 4.8 ± 1.7 mm preoperatively and 2.2 ± 2.2 mm at the final follow-up (p < 0.001, the paired Student's t-test) (Table 2).
Table 2.
Radiologic Findings
Values are presented as mean ± SD.
*p using paired Student t-tests.
The preoperative ulnar variance demonstrated weak positive correlation with the preoperative radioulnar distance (R = 0.395, p = 0.014, Pearson's correlation), indicating the more positive the ulnar variance, the larger the radioulnar distance with the ulnar translating dorsally.
The types of DRUJ were as follows.
Type I: 1 patient (2.8%).
Type II: 9 patients (25.0%).
Type III: 26 patients (72.2%).
Osteoarthritis of the DRUJ
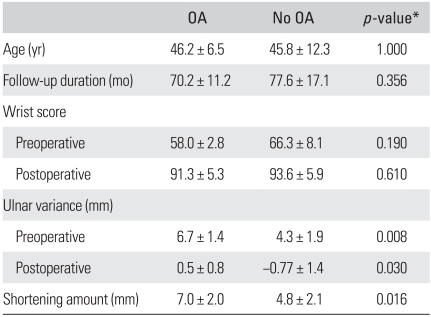
Radiographic changes consistent with osteoarthritis of the DRUJ were noted in 6 of 36 wrists (16.7%). These changes were first noted at a mean follow-up period of 34.8 months (range, 22 to 46 months) after surgery. This occurred in one of the type II (1/9) cases and in 5 of the type III (5/26) cases. We analyzed the cases with and without DRUJ osteoarthritis. We compared these two groups using the Mann-Whitney U-test (Table 3).
Table 3.
Comparison of Two Groups with/without Distal Radioulnar Osteoarthritis (OA)
Values are presented as mean ± SD.
*p-value using Mann-Whitney U-test.
There was no difference in the clinical outcomes between the two groups. The patients with osteoarthritic change of the DRUJ did not complain of pain or limitation of motion on the last follow-up visit, but one patient showed crepitus on forearm rotation while compressing the DRUJ.
There was no statistically significant difference in the wrist scores between the two groups preoperatively and at the last follow-up. There was also no difference regardless of age and the follow-up duration.
However, there was a statistically significance difference with regard to ulnar variance. The preoperative ulnar variance in those with osteoarthritis (OA) was 6.7 ± 1.4 mm and that in those patients without OA was 4.3 ± 1.9 mm (p = 0.008).
There was a significant difference in the shortening length between the two groups (those with OA, 7.0 ± 2.0 mm; those without OA, 4.8 ± 2.1 mm; p = 0.016).
In terms of the radioulnar distance, there was a significant difference between the two groups preoperatively (6.8 ± 2.0 mm in those with OA; 4.5 ± 1.4 mm in those without OA; p = 0.006) but there was no significant difference postoperatively in those with OA (1.9 ± 3.9 mm) and those without OA (2.2 ± 1.8 mm, p = 0.279).
DISCUSSION
This study demonstrates that the clinical outcomes of ulnar shortening osteotomy are satisfactory for more than 5 years postoperatively, despite the fact that 16% of the patients had radiographic arthritic changes of the DRUJ that appeared at a mean follow-up of 3 years after surgery.
We also found changes in the postoperative radiographs when compared to those done preoperatively. The radioulnar distance had significantly decreased postoperatively.
The factors associated with the observed osteoarthritic changes of the DRUJ were analyzed. Based on the statistical date, we concluded that factors such as the ulnar variance, the degree of shortening and the radioulnar distance were related to the postoperative osteoarthritic changes.
The clinical outcomes were excellent. The average wrist score had improved from 65.5 to 93.4. Most of the patients were able to use their wrists without pain or discomfort even after 5 years. Our long term data demonstrated satisfactory results, which was consistent with previous follow-up reports of a shorter duration.3-5,17)
In our study, type III was the most common type of DRUJ followed by type II and then type I. Tolat et al.16) reported that in patients with a normal DRUJ, type II was the most common (50%) followed by type I (38%) and type III (12%). With regard to the declination angles, Moremans et al.17) reported that 8 had less than 85 degrees (similar to type III), 5 had more than 95 degrees (similar to type II), and 15 had between 85 and 95 degrees (similar to type I), which was different from our results. We revealed that type III comprised the majority of cases of DRUJ in the patients with idiopathic ulnar impaction syndrome among our study cohort. Studies focusing on the different types of DRUJ in an asymptomatic cohort would be helpful.
There was some correlation among the ulnar variance and the distal radioulnar distance. There was a positive correlation between ulnar variance and the distal radioulnar distance, which is consistent with our previous data.3)
We found radiographic changes consistent with osteoarthritis of the DRUJ in 6 of 38 wrists after ulnar shortening osteotomy. Regardless, there were no differences in clinical outcome whether or not OA was present. There were no significant differences with regard to the wrist scores either. Some authors maintain that problems may occur in the DRUJ aft er ulnar shortening at the last follow-up. Deshmukh et al.10) reported that the the DRUJ was incongruent after ulnar shortening in a cadaveric study. Miura et al.18) reported that the peak DRUJ pressure had increased in normal cadavers when the ulna was shortened, and especially in the type I and type III joints. Tolat et al.16) suggested that the type III joint is difficult to shorten beyond 2 to 3 mm without disturbing the configuration of the DRUJ. Minami and Kato4) reported that the postoperative occurrence of degenerative changes of the DRUJ was seen in 28% of wrists aft er ulnar shortening osteotomy. Koppel et al.6) also reported radiological changes of the DRUJ were seen in 38% of wrists aft er ulnar shortening osteotomy. Nakamura et al.7) reported that postoperative osteoarthrosis of the DRUJ was seen in 12 wrists (38%), but only 2 cases were symptomatic.
We conclude that the preoperative ulnar variance, the radioulnar distance and the degree of shortening could be attributed to the osteoarthritic changes of the DRUJ.
An increased distal radioulnar distance is seen with greater degrees of dorsal subluxation. In our study, the radioulnar distance was decreased on the postoperative radiographs, implying a decrease in dorsal subluxation aft er ulnar shortening. This should result in increased pressure at the DRUJ.
Thus, both the ulnar variance and the radioulnar distance should decrease aft er ulnar shortening osteotomy, and the resulting increase in pressure at the DRUJ may contribute to the arthritic changes of the DRUJ found in this study.
There are several limitations to be noted in this study. First, there were no CTs or MRIs performed in our study. Therefore, we could not analyze the transverse section of the DRUJ or accurately measure the ulnar and sigmoid notch angles or evaluate the ligament status around the ulnar wrist such as the triangular fibrocartilage complex. Second, functional evaluation such as DASH (disabilities of the arm, shoulder and hand) was not performed. The general medical condition of the upper extremities was not assessed. Third, the number of cases with arthritic changes of the DRUJ was small and the number of type III DRUJs (which already harbor factors that increase the risk for subsequent problems at the DRUJ)8,16) comprised the majority of all the cases, as well as those with OA.
In conclusion, the clinical outcomes are satisfactory for even more than 5 years after ulnar shortening osteotomy for treating idiopathic ulnar impaction syndrome despite of the osteoarthritic changes of the DRUJ. However, we must assess the osteoarthritic changes of the DRUJ with longer term follow-up.
ACKNOWLEDGEMENTS
This study was supported by the Korean Human Technology Research Foundation (KOHTERF-2009-04).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Friedman SL, Palmer AK, Short WH, Levinsohn EM, Halperin LS. The change in ulnar variance with grip. J Hand Surg Am. 1993;18(4):713–716. doi: 10.1016/0363-5023(93)90325-w. [DOI] [PubMed] [Google Scholar]
- 2.Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg Am. 1982;7(4):376–379. doi: 10.1016/s0363-5023(82)80147-0. [DOI] [PubMed] [Google Scholar]
- 3.Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome. J Bone Joint Surg Am. 2005;87(12):2649–2654. doi: 10.2106/JBJS.D.02983. [DOI] [PubMed] [Google Scholar]
- 4.Minami A, Kato H. Ulnar shortening for triangular fibrocartilage complex tears associated with ulnar positive variance. J Hand Surg Am. 1998;23(5):904–908. doi: 10.1016/S0363-5023(98)80171-8. [DOI] [PubMed] [Google Scholar]
- 5.Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg Am. 1993;18(1):46–53. doi: 10.1016/0363-5023(93)90243-V. [DOI] [PubMed] [Google Scholar]
- 6.Koppel M, Hargreaves IC, Herbert TJ. Ulnar shortening osteotomy for ulnar carpal instability and ulnar carpal impaction. J Hand Surg Br. 1997;22(4):451–456. [Google Scholar]
- 7.Nakamura T, Takayama S, Kikuchi Y, Osada N, Ono H. Long-term results of the ulnar shortening procedure for triangular fibrocartilage complex tear. J Jpn Soc Surg Hand. 2002;19(3):219–224. [Google Scholar]
- 8.Sagerman SD, Zogby RG, Palmer AK, Werner FW, Fortino MD. Relative articular inclination of the distal radioulnar joint: a radiographic study. J Hand Surg Am. 1995;20(4):597–601. doi: 10.1016/S0363-5023(05)80275-8. [DOI] [PubMed] [Google Scholar]
- 9.Nishiwaki M, Nakamura T, Nakao Y, Nagura T, Toyama Y. Ulnar shortening effect on distal radioulnar joint stability: a biomechanical study. J Hand Surg Am. 2005;30(4):719–726. doi: 10.1016/j.jhsa.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 10.Deshmukh SC, Shanahan D, Coulthard D. Distal radioulnar joint incongruity aft er shortening of the ulna. J Hand Surg Br. 2000;25(5):434–438. doi: 10.1054/jhsb.2000.0456. [DOI] [PubMed] [Google Scholar]
- 11.Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg Br. 1996;21(5):587–594. doi: 10.1016/s0266-7681(96)80136-7. [DOI] [PubMed] [Google Scholar]
- 12.Jung JM, Baek GH, Kim JH, Lee YH, Chung MS. Changes in ulnar variance in relation to forearm rotation and grip. J Bone Joint Surg Br. 2001;83(7):1029–1033. doi: 10.1302/0301-620x.83b7.11062. [DOI] [PubMed] [Google Scholar]
- 13.Baek GH, Chung MS, Lee YH, Gong HS, Lee S, Kim HH. Ulnar shortening osteotomy in idiopathic ulnar impaction syndrome: surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 2):212–220. doi: 10.2106/JBJS.F.00320. [DOI] [PubMed] [Google Scholar]
- 14.Coleman DA, Blair WF, Shurr D. Resection of the radial head for fracture of the radial head: long-term follow-up of seventeen cases. J Bone Joint Surg Am. 1987;69(3):385–392. [PubMed] [Google Scholar]
- 15.Nakamura R, Horii E, Imaeda T, Tsunoda K, Nakao E. Distal radioulnar joint subluxation and dislocation diagnosed by standard roentgenography. Skeletal Radiol. 1995;24(2):91–94. doi: 10.1007/BF00198067. [DOI] [PubMed] [Google Scholar]
- 16.Tolat AR, Sanderson PL, De Smet L, Stanley JK. The gymnast's wrist: acquired positive ulnar variance following chronic epiphyseal injury. J Hand Surg Br. 1992;17(6):678–681. doi: 10.1016/0266-7681(92)90200-l. [DOI] [PubMed] [Google Scholar]
- 17.Moermans A, Degreef I, De Smet L. Ulnar shortening osteotomy for ulnar ideopathic impaction syndrome. Scand J Plast Reconstr Surg Hand Surg. 2007;41(6):310–314. doi: 10.1080/02844310701463373. [DOI] [PubMed] [Google Scholar]
- 18.Miura T, Firoozbakhsh K, Cheema T, Moneim MS, Edmunds M, Meltzer S. Dynamic effects of joint-leveling procedure on pressure at the distal radioulnar joint. J Hand Surg Am. 2005;30(4):711–718. doi: 10.1016/j.jhsa.2005.03.007. [DOI] [PubMed] [Google Scholar]