Abstract
We report here on a new arthroscopic direct repair technique for a radial tear of the posterior root of the medial meniscus (PRMM) using a posterior trans-septal portal. Radial tears of the PRMM are commonly observed in the elderly population of Korea and Japan, and the life style of these people requires squatting and kneeling down in daily life. A radial tear of the PRMM results in the loss of hoop tension and this accelerates degenerative changes in the knee joint and causes early osteoarthritis. Several reports in the medical literature have focused on various repair techniques for these tears by using pull out sutures. These techniques result in nonanatomic fixation of the meniscus, which may lead to disturbed meniscal excursion and failure to restore hoop tension. Arthroscopic direct repair may contribute to restoring hoop tension and preventing accelerated degenerative changes in the knee joint of these patients.
Keywords: Radial tear, Medial meniscus posterior root, Direct repair, Arthroscopy
Radial tear of the meniscus is a tear that is oriented perpendicular to the long circumferential axis of the meniscus. A radial tear of the posterior root medial meniscus (PRMM) is defined as a tear that occurs within 10 mm of the posterior tibial attachment of the medial meniscus.1) A full thickness (complete) radial tear severely compromises the meniscal function by disrupting the critical circumferential collagen bundles, such that the meniscus can no longer develop the hoop stresses necessary to disperse an axial load. As a result, extrusion of the medial meniscus occurs, leading to decreased contact area and increased contact pressures in the medial compartment of the knee. This can lead to the early occurrence or acceleration of existing osteoathrosis of the knee joint. Ahn et al.2) have reported on the pullout suture techniques for repair of these tears for restoring the hoop tension of the meniscus. These repair techniques may disturb the normal meniscal movement during flexion in a loaded condition. To overcome these problems, we have developed a new arthroscopic technique of direct repair for the radial tear of the PRMM with using a posterior trans-septal portal.3)
TECHNIQUE
Complete radial tears of the PRMM are often associated with degenerative changes in knee joint. The meniscus has a good blood supply at its posterior tibial attachment site (which contains the perimeniscal capillary plexus and small vessels that penetrate the meniscus); hence, the meniscus has good repair potential.4) However it is essential to rule out the presence of degenerative changes at the tear site as a degenerated meniscus has poor healing potential. We used stringent selection criteria for making repairs using our technique. Those patients who were younger than sixty years, those with no or early osteoarthritis (Kellgren and Lawrence grade 0 and 1) and no varus or valgus deformities (more than 10 degree) were selected for repair. The duration of symptoms before surgery was less than 1 month. The most important indication was that the remnant tissue of the PRMM should be sufficient to repair. If we can see the short remnant tissue of the PRMM, then it is impossible to repair. At the beginning, comprehensive arthroscopic examination of the knee joint was performed through the standard anterolateral and anteromedial portals. Through the anterolateral portal, blood tinged meniscal tissue and the size of the remnant tissue were checked. A complete radial tear of the PRMM was confirmed by arthroscopic examination through the posteromedial portal. Evaluation of the knee joint for degenerative changes was done. If during this arthroscopic examination we found an associated horizontal tear of the medial meniscus, then it was treated by removing the free torn edge of the meniscus. Then we proceeded with making an additional posteromedial portal and a posterior trans-septal portal, which were made by passing the scope through the posterolateral portal. First, the arthroscope was advanced through the trans-septal portal to reach the posteromedial compartment. Using this approach, a complete radial tear of the PRMM was clearly visible (Fig. 1). With the arthroscope in the trans-septal portal, a suture hook (Linvatec, Largo, FL, USA) loaded with No.1 polydioxanone suture (PDS) was introduced through the lower posteromedial portal.5) The suture hook was manipulated by hand so that the sharp tip penetrated the remnants of the medial meniscus (the inner side of the posterior root site) from inside to outside (Fig. 1). The free end of the suture in the posteromedial space was grasped and brought up to the upper posteromedial portal close to the tip of a 5 mm cannulated tube. Next, the suture hook was passed through the body (the outer portion) of the medial meniscus from inside to outside using shuttle relay. The shuttle relay was then connected with the No. 1 PDS (Fig. 2) and then it was passed through the meniscus body portion and the remnant of the posterior root portion (Fig. 3A). We tied these edges of the torn meniscus using a SMC sliding knot (Fig. 3B). This step was repeated until 2 sutures were placed. Care was taken during this technique to avoid tangling the sutures.
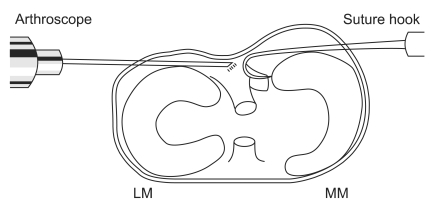
Fig. 1.
The suture hook penetrated the remnants of the medial meniscus (inner side of the posterior root site) from inside to outside. LM: lateral meniscus, MM: medial meniscus.
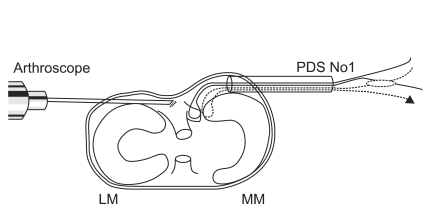
Fig. 2.
Sutures are passed through both ends of the tear with the arthroscope in the trans-septal portal. PDS: polydioxanone suture, LM: lateral meniscus, MM: medial meniscus.
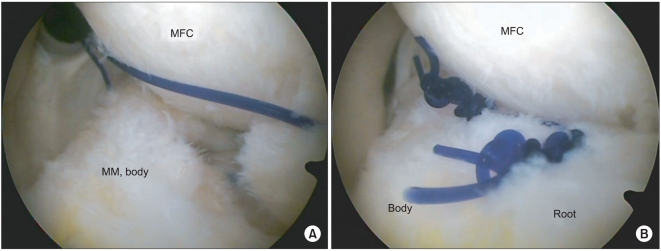
Fig. 3.
(A) Arthroscopic view of the suture connecting the root and body portion of the torn meniscus. (B) The torn edges of the meniscus are secured with two SMC knots. MFC: medial femoral condyle, MM: medial meniscus.
Postoperative Rehabilitation
The patients were started on toe touch crutch walking and range of motion exercises by the third postoperative day and they continued this for the next 6 weeks. After six weeks the patients were allowed to walk with partial weight bearing over the next 4 weeks. The patients were encouraged to return to their routine activity by 12 weeks. We have experience with 4 cases treated by this method to date. There have been no complications due to muscle atrophy or bony change during follow-up. At one year follow-up, all the patients had excellent results and on the second-look arthroscopy we could see complete healing with good continuity, as observed through the posteromedial portal.
DISCUSSION
Menisci protect the articular cartilage from high contact pressures. This action is dependent on the longitudinal orientation of the intrameniscal fibers and this results in the generation of circumferential tension in the meniscus as a vertical load is applied (hoop stress). Radial tears of the meniscus can result from trauma or degenerative changes and they can occur anywhere in either meniscus. Radial tears of the lateral meniscus have been reported as a result of sports injuries in young patients. However, radial tears of the medial meniscus have been reported to be common in elderly patients who have complaints of severe knee pain.1) In vitro biomechanical studies, Allair et al.6) have proved that a radial tear of the PRMM is biomechanically equivalent to total meniscectomy, which leads to accelerated degenerative changes. The loss of attachment at the ends allows the normal centrifugal pull of the meniscocapsular attachments to displace the meniscus peripherally. The inability of the meniscus to distribute force and the peripheral subluxation of the meniscus that occurs in radial tears of the PRMM compromise the ability of the meniscus to protect the articular surfaces of the knee. This leads to abnormal stresses that cause accelerated degenerative changes in the affected compartment.7)
Ahn et al.2) have recently reported on the pull out suture techniques for restoring the hoop tension of the medial meniscus with a radial tear. These arthroscopic pullout suture techniques fix the torn site of the meniscus with the cartilage at around 60 degrees of knee flexion. Vedi et al.8) reported on the meniscal movement in normal knees under a load during motion. The posterior horn of the medial meniscus moves a mean 3.9 mm in the anteroposterior direction. Seo et al.1) reported that after repair of a radial tear of the PRMM by the pullout suture techniques the pivot of the meniscus movement moves to the pullout suture site instead of the original attachment site, and this restricts the normal meniscal movement. The pullout suture techniques may not restore hoop stress and it may put the suture site under high stress and especially during extension and it may lead to failure of sutures. Tuckman et al.7) reported that the only way to restore the ability to resist the hoop stresses would be to reattach the meniscus with bridging the circumferentially oriented collagen fibers across the tear site. Therefore, we have developed this new arthroscopic direct repair technique for restoring the hoop tension.
Our direct repair technique using a trans-septal portal provided the advantages of easy handling of the suture hook and a relatively wide visual field for viewing the posteromedial compartment, as compared to the traditional arthroscopic techniques that could lead to iatrogenic cartilage damage of the tibial and femoral condyle and additional meniscal injury. However, we have noticed that it is a difficult technique and it demands great expertise because of the very short length of the remnant of the meniscus available for repair. We delay weight bearing up to six weeks postoperatively for the fear of retear. We believe that our technique may contribute to restore the hoop tension and prevent osteoarthritis of knee as it aims at being an anatomical repair and it allows healing of the circumferentially oriented fibers across the tear site. Our technique also preserves the normal anatomy of the posterior tibial attachment site of the medial meniscus, which is essential to generate normal hoop strains for effective load distribution across the knee joint.
Regarding the healing potential of root tear of the meniscus, von Trommel et al.9) reported on five cases of complete radial tear of the lateral meniscus that extended to the popliteus tendon, and this was repaired with a fibrin clot; the second-look arthroscopy showed healing of the periphery in all of the cases. Ahn et al.10) have reported favorable results using an all-inside repair technique for lateral meniscus root tear. In this study, of the 9 patients who agreed to second-look arthroscopy, 8 patients had arthroscopic findings that indicated complete healing of the posterior lateral meniscus root tear. However, there are not many reports in the medical literature on the results of repairing the PRMM.
Although we need to add more cases and a longer follow-up period, the early results seem promising with regard to repairing a radial tear of the PRMM.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Seo JH, Li G, Shetty GM, et al. Effect of repair of radial tears at the root of the posterior horn of the medial meniscus with the pullout suture technique: a biomechanical study using porcine knees. Arthroscopy. 2009;25(11):1281–1287. doi: 10.1016/j.arthro.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 2.Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1510–1513. doi: 10.1007/s00167-007-0310-3. [DOI] [PubMed] [Google Scholar]
- 3.Ahn JH, Chung YS, Oh I. Arthroscopic posterior cruciate ligament reconstruction using the posterior trans-septal portal. Arthroscopy. 2003;19(1):101–107. doi: 10.1053/jars.2003.50017. [DOI] [PubMed] [Google Scholar]
- 4.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10(2):90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 5.Ahn JH, Kim SH, Yoo JC, Wang JH. All-inside suture technique using two posteromedial portals in a medial meniscus posterior horn tear. Arthroscopy. 2004;20(1):101–108. doi: 10.1016/j.arthro.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 7.Tuckman GA, Miller WJ, Remo JW, Fritts HM, Rozansky MI. Radial tears of the menisci: MR findings. AJR Am J Roentgenol. 1994;163(2):395–400. doi: 10.2214/ajr.163.2.8037039. [DOI] [PubMed] [Google Scholar]
- 8.Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM. Meniscal movement: an in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81(1):37–41. doi: 10.1302/0301-620x.81b1.8928. [DOI] [PubMed] [Google Scholar]
- 9.van Trommel MF, Simonian PT, Potter HG, Wickiewicz TL. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthroscopy. 1998;14(4):360–365. doi: 10.1016/s0749-8063(98)70002-7. [DOI] [PubMed] [Google Scholar]
- 10.Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(1):67–75. doi: 10.1016/j.arthro.2009.07.007. [DOI] [PubMed] [Google Scholar]