Abstract
Objective: The purpose of this study was to evaluate three-dimensional (3D) dehiscence of upper anterior alveolar bone during incisor retraction and intrusion in adult patients with maximum anchorage. Methods: Twenty adult patients with bimaxillary dentoalveolar protrusion had the four first premolars extracted. Miniscrews were placed to provide maximum anchorage for upper incisor retraction and intrusion. A computed tomography (CT) scan was performed after placement of the miniscrews and treatment. The 3D reconstructions of pre- and post-CT data were used to assess the dehiscence of upper anterior alveolar bone. Results: The amounts of upper incisor retraction at the edge and apex were (7.64±1.68) and (3.91±2.10) mm, respectively, and (1.34±0.74) mm of upper central incisor intrusion. Upper alveolar bone height losses at labial alveolar ridge crest (LAC) and palatal alveolar ridge crest (PAC) were 0.543 and 2.612 mm, respectively, and the percentages were (6.49±3.54)% and (27.42±9.77)%, respectively. The shape deformations of LAC-labial cortex bending point (LBP) and PAC-palatal cortex bending point (PBP) were (15.37±5.20)° and (6.43±3.27)°, respectively. Conclusions: Thus, for adult patients with bimaxillary protrusion, mechanobiological response of anterior alveolus should be taken into account during incisor retraction and intrusion. Pursuit of maximum anchorage might lead to upper anterior alveolar bone loss.
Keywords: Alveolar bone loss, Adult patients, Computed tomography, Three-dimensional registration
1. Introduction
The tooth-alveolar bone complex is a complicated mechanical unit combining both mineralized and periodontal soft tissues in orthodontic tooth movement, of which the main function is to transfer the occlusal force from the tooth to the surrounding bone. However, little is known about alveolar bone adaptation during incisor retraction and intrusion, especially in adult patients with maximum anchorage. Despite the fact that the relationship between maximum anchorage and tooth displacement has been well-recognized (Lai et al., 2008; Yao et al., 2008; Liu et al., 2011), retrospective alveolar bone loss assessment remains to be established. Meikle (1980) and Fuhrmann (1996; 2002) discovered that retraction of the upper anterior tooth might induce dehiscence, even fenestration in the cortical plate. Edwards (1976) and Hwang and Moon (2001) reported the limitation of alveolar bone modeling and remodeling during retraction and intrusion of maxillary incisors. Kim Y. et al. (2009) evaluated alveolar bone loss around incisors in surgical skeletal Class III patients, and Nelson and Artun (1997) showed the relationship between age and alveolar bone loss. Wehrbein et al. (1995) and Evangelista et al. (2010) appraised the prevalence of alveolar bone dehiscence in untreated patients and subjects who have undergone tooth retraction. However, Decker and Chen (2009) demonstrated good upper alveolar bone adaptation after 32 years of follow-up by case report. Shimpo et al. (2003) thought that lingual alveolar bone height was maintained due to bone formation during moving first molar lingually in rats. Further research is necessary for alveolar bone dehiscence involving large incisor retraction and intrusion in adult patients with maximum anchorage.
In order to assess dentoalveolar morphology in both sagittal and vertical dimensions, orthodontists often use cephalometric tracings. However, this fails to reveal dehiscence in palatal cortical bone attributed to surrounding bone superimposition (Mah et al., 2010). For this reason, three-dimensional (3D) evaluation is necessary, which could provide 3D displacements for dentoalveolar changes (Vannier, 2003; Nakasima et al., 2005; Garib et al., 2010). Cone beam computed tomography (CBCT) cannot quantify the dentoalveolar changes by pre- and post-treatment 3D registration, due to lack of stable references with 3D craniofacial model (Cevidanes et al., 2010). CT scanning might be an acceptable imaging technique supplying a quantitative assessment of upper alveolar bone by CT registration in clinics (Nelson and Michael, 1998), and might permit an accurate topographical calculation of alveolar bone displacements (Liu et al., 2010). Therefore, this study was designed to evaluate maxillary alveolar bone morphology after incisor retraction and intrusion in adult bimaxillary malocclusion by retrospective 3D registration.
2. Materials and methods
2.1. Subjects and treatment procedures
This research was accepted by the Research Ethic Committee of Shandong University Dental School. Twenty bimaxillary dentoalveolar protrusion patients (mean age (22.28±3.16) years) were randomly selected. All patients received information about the procedure including the damage of CT radiation lesion and miniscrew methodologies and gave consent. Then the four first premolars were extracted and the patients were treated by using oriental preadjusted appliance KOSAKA slot brackets (OPA-K, Tomy, Fukushimaken, Japan), and miniscrews were placed as anchorage for the integral retraction and intrusion of the maxillary tooth. Force of 150 g per side of elastic chains was applied from the miniscrew to the upper crimpable hook to retract and intrude the upper anterior tooth (Fig. 1). The patients were visited at one month intervals.
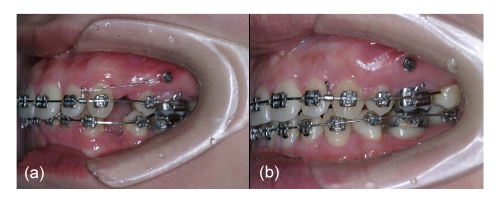
Fig. 1.
Miniscrews of pre-(a) and post-treatment (b)
Miniscrews were placed in the interradicular locations between the first molar and second premolar at the attached gingival level height
2.2. CT data acquirement
The whole skull CT scan was performed at one week after implanting the miniscrews (T1), and post-treatment (T2), respectively, which was undertaken in the same way by 16-row helical CT. The CT scan was performed perpendicular to the apical-coronal direction on each slice, using the lateral scanogram of the head position to set the gantry angle. The CT data were saved as digital imaging and communications in medicine (DICOM) format.
2.3. 3D virtual model reconstruction
All 3D models were constructed from CT images with a voxel dimension of 0.350 mm×0.625 mm×0.625 mm. The bone and tooth structures were separated by the threshold based on Hounsfield unit (HU) in Materialism’s interactive medical image control system (MIMICS). In order to include the alveolar regions and exclude tooth structure, a lower limit of 392 HU and a higher limit of 1 900 HU were defined. The tooth excluding bone structure was separated with a lower limit of 1 500 HU and a higher limit of 3 725 HU. The separated and independent masks were created for each part, which allowed for the next generation of individual geometrical files and 3D models. All 3D masks were exported as stereolithography (STL).
2.4. Registration of pre- and post-treatment models
In MIMICS, STL was moved to a certain location by point-registration, which was accomplished by laying the zygomatic arch landmarks (Nada et al., 2011) on pre- and post-treatment STLs and 3D models (Fig. 2). The software calculated the transformation matrix to fit best between the start-end points on STL, and then applied it to the one selected. After point-registration, STL-registration was performed to place STL on the CT-mask to improve the accuracy. In order to ensure the precision, corresponding landmarks were identified repeatedly (minimal point distance filter was 0.10 mm, which was satisfied as Fig. 3). All the registrations were undertaken three times in two weeks and the best one was chosen for measurements.
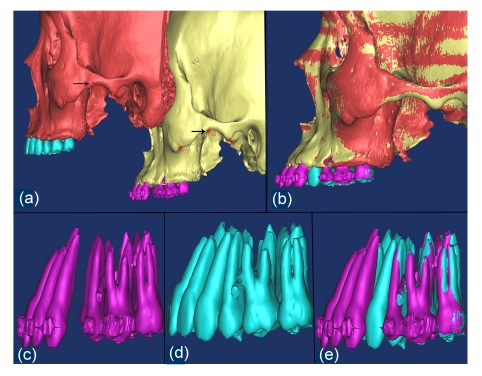
Fig. 2.
Effect of point-registration
The teeth and maxilla were registered with the surface points that did not change after orthodontic treatment. (a) Most protruding points on the inferior margin of the zygomatic arch (black arrows); (b) Registration of pre- and post-treatment models; (c) Pre-models of the teeth; (d) Post-models of the teeth; (e) Pre- and post-models of the teeth that were matched to each other after the registration of maxillary
Fig. 3.
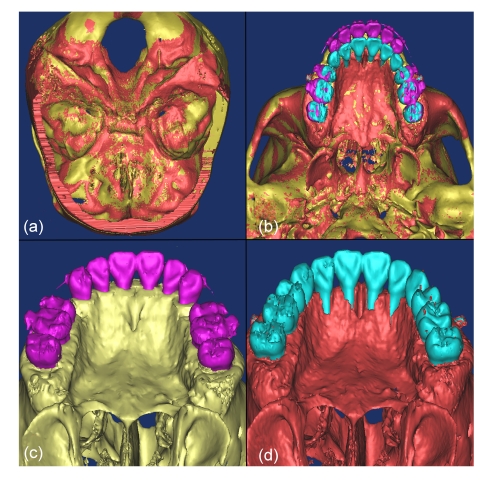
Effect of STL registration
(a) STL registration with cranial base; (b) STL model occlusal view; (c) T1 STL model occlusal view; (d) T2 STL model occlusal view
2.5. 3D measurement
After registration, the morphology changes of upper alveolar bone and upper central incisor displacement were evaluated in 3D model and sagittal slices (Fig. 4). The landmarks identified on each CT scan were: labial alveolar ridge crest (LAC), palatal alveolar ridge crest (PAC), upper incisor crown edge (UICE), upper incisor root apex (UIRA), labial cortex bending point (LBP), and palatal cortex bending point (PBP). The variables measured on each CT scan were shown in Tables 1 and 2. All the measurements were performed by the same investigator.
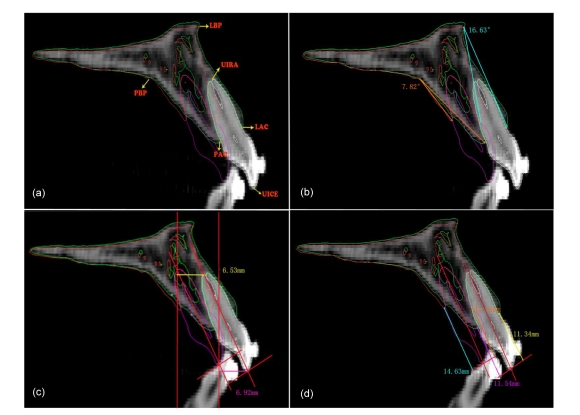
Fig. 4.
Distance between T1 and T2 models
(a) The landmarks identified on CT scan; (b) Bending angles of labial cortex and palatal cortex between T1 and T2 models; (c) Measurements of the retraction distance at the cusp tip of the crown and the apex of the root in sagittal plane between T1 and T2 models; (d) Vertical distance differences from UICE to LAC and PAC measured parallel to long axis between T1 and T2 models
Table 1.
Definitions of alveolar measurements used
| Measurement variables | Definition |
| UICE to LAC | Vertical distance difference from UICE to LAC (T1-T2) measured parallel to long axis |
| UICE to PAC | Vertical distance difference from UICE to PAC (T1-T2) measured parallel to long axis |
| Bending angle of labial cortex (BAL) | Angle formed with the points LAC (T1)-LBP-LAC (T2) |
| Bending angle of palatal cortex (BAP) | Angle formed with the points PAC (T1)-PBP-PAC (T2) |
| Bone height loss percentage at LAC | UICE to LAC (T1-T2)/distance measured perpendicular to long axis from LAC to UIRA (T1)×100% |
| Bone height loss percentage at PAC | UICE to PAC (T1-T2)/distance measured perpendicular to long axis from PAC to UIRA (T1)×100% |
Table 2.
Definitions of teeth measurements used
| Measurement variables | Definition |
| Drift distance of upper incisor crown edge | Upper central incisor retraction amount at edge in sagittal plane |
| Drift distance of upper incisor root apex | Upper central incisor retraction amount at root apex in sagittal plane |
| Upper incisor intrusion measurement | Perpendicular distance difference between incisor edge of maxillary central incisor and the palatal plane |
2.6. Statistical analysis
The statistical data of drift distance were analyzed using SAS 9.13 software. The mean and standard deviation (SD) of each variable measurement were estimated. Differences of flexure distance in upper anterior alveolar bone and tooth displacements were assessed for significance using paired t-test. Error of the method based on double measurements was performed on twenty randomly selected patients for 3D linear measurements (Dahlberg, 1940; Houston, 1983) and was calculated as:  (d is the deviation; n is the number of paired objects). The error was 0.29 mm for 2D linear measurement. The statistical difference was not significant between two measurements by paired t-test.
(d is the deviation; n is the number of paired objects). The error was 0.29 mm for 2D linear measurement. The statistical difference was not significant between two measurements by paired t-test.
3. Results
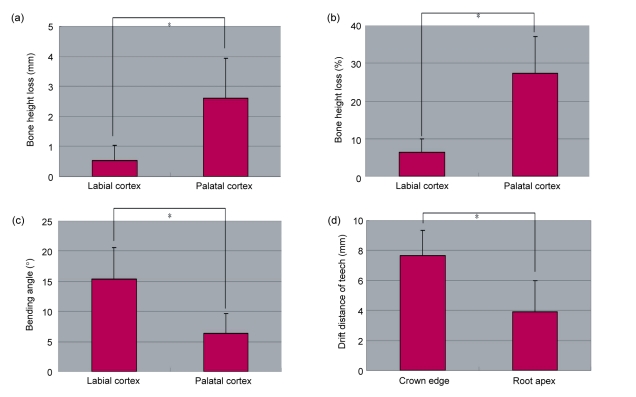
After active post-treatment, upper alveolar bone height losses of bone height at LAC and PAC were 0.543 and 2.612 mm, respectively (Fig. 5a) and the percentages were (6.49±3.54)% and (27.42±9.77)% (Fig. 5b), respectively. The bending angle of labial cortex (BAL) was (15.37±5.20)°, and the bending angle of palatal cortex (BAP) was (6.43±3.27)° (Fig. 5c). Statistically significant differences were observed between BAL and BAP by paired t-test (P<0.05).
Fig. 5.
Data measured at landmark points
(a) Bone height losses at labial and palatal sides; (b) Bone height loss percentages at labial and palatal sides; (c) Bending angles of labial and palatal cortex; (d) Amounts of upper incisor retraction at edge and apex. * P<0.05 (n=20)
The drift distance of the upper central incisor crown edge and root apex were (7.64±1.68) and (3.91±2.10) mm, respectively (Fig. 5d), which demonstrated that there was a statistically significant difference between them. The upper central incisor intrusion measurement was (1.34±0.74) mm. Palatal bone dehiscence was observed in every virtual model after upper incisor retraction and intrusion in adult patients with maximum anchorage (Fig. 3d).
4. Discussion
The results showed that palatal bone dehiscence was obvious in every virtual post-treatment model, and the loss percentage of alveolar bone height on the lingual side was more obvious than that of the labial side. Meanwhile, there was alveolar bone flexure on both sides, but the extent of the palatal side was more limited. Therefore, risk of alveolar bone loss should be considered during incisor retraction and intrusion in maximum anchorage patients.
Upper anterior alveolar bone dehiscence cannot be explained by concepts that bone traces with tooth movement (Reitan, 1964; Reitan and Kvam, 1971). The mechanism of alveolar bone dehiscence around the tooth remains unclear. In order to explain the bone dehiscence to incisor retraction and intrusion, two aspects should be taken into consideration. Firstly, it is thought to be caused by modeling of the bone surrounding the tooth, which is based on the bone reaction to retraction and intrusion. Frost (1964) showed mathematically the relationship between the distinctive given stimuli and reactions of the bone. Frost, (1994) thought that bone strains can reach lower values than 1500–2000 µE physiologically, and healthy bone can endure and adapt to mild overloads (1500–3000 µE) but cannot resist pathological overloads (>3000 µE). This study confirmed that the phenomena of alveolar bone resorption were dominant during a large number of retractions and intrusions. Therefore, it is improper for large retraction in limited bone structure. Secondly, upper alveolar bone loss is attributed to an intrinsic configuration. For upper anterior alveolar bone configuration, the alveolar process consists of palatal and buccal cortical plates and the cancellous trabeculae (Geramy, 2000). In the apical-coronal-sagittal direction the margin of bone is thinned to a knife edge, and alveolar bone quantity is limited and possesses higher density (Sarikaya et al., 2002; Park et al., 2008). In this study, upper anterior alveolar bone was subjected to force generated by elastic traction, and the force was applied to the crimpable hook on the distal lateral incisors with an elastic power chain extending from miniscrews. Force direction was upwards and retracted, and stress and deformation might concentrate on LAC and PAC (Cobo et al., 1996), where local alveolar bone loss occurred to modify its structure to decrease alveolar strains. The mechanics were similar with the root resorption during incisor retraction and intrusion in maximum anchorage patients (Liou and Chang, 2010).
This research observed alveolar bone bending phenomena both in labial and palatal sides, which supported the theory that alveolar bone modeling was the result of bending stimuli (Akhter et al., 2002). When retraction force was applied to the tooth, the new alveolar bone formation was observed on both sides (Milne et al., 2009). According to the theory of bending beam (Meikle, 2006), bone bending of the labial cortical is more obvious than that of the palatal cortical. Moreover, bone loss happened in both vertical and horizontal directions. When the palatal bending was less, the relapse of palatal plates during retention period was observed on subsequent visits (Naraghi, 2010). Therefore, the anatomical limitation of palatal bone should be greatly emphasized on the tooth movement.
In order to obtain appropriate alveolar bone response during incisor retraction and intrusion in adult patients, we must pay attention to the fundamental knowledge to improve treatment strategy. For example, minor tooth movement and bone quantity limitation should be considered, force magnitude direction should be controlled, detriment of periodontal injury should be evaluated by regular radiographic examination, and ridge expansion osteotomy should be emphasized as an alternative way of decreasing the anatomical limitation of palatal portion (Kim S.J. et al., 2009; AlGhamdi, 2010). With these effective procedures, we might be able to lower the incidence of alveolar bone dehiscence, accomplishing our goal of maintaining the health, function, and aesthetics of the periodontium in the orthodontic treatment.
In the present investigation, the upper anterior teeth of bimaxillary patients were mainly retracted with bodily movement, interpreted as en masse retraction provided by miniscrews (Aljhani and Zawawi, 2010). The controlled tipping movement is a favorable pattern but might induce more obvious dehiscence during retraction of the protruded maxillary incisors (Årtun and Urbye, 1988), which needs to be further verified. Incidentally, all the data evaluated by CT came from the original alveolar bone, while the palatal newly born plate may be invisible because of the low density. It is necessary to access the long-term alveolar effect of orthodontic treatment.
5. Conclusions
For adult patients with bimaxillary protrusion, mechanobiological response of anterior alveolus should be taken into account during incisor retraction and intrusion. Pursuit of maximum anchorage might lead to upper anterior alveolar bone loss.
Acknowledgments
We wish to thank Prof. Guang-chun WANG (Research Center of Mould, Shandong University, China) for his assistance.
Footnotes
Project supported by the Shandong Science and Technology Planning Project Contract Research (Nos. 2008GG30002019 and 2008GG 30001001) of China and the Shandong University Dental School Project Research (Nos. P2009009, P2009010, and P2010010), China
References
- 1.Akhter MP, Cullen DM, Recker RR. Bone adaptation response to sham and bending stimuli in mice. J Clin Densitom. 2002;5(2):207–216. doi: 10.1385/JCD:5:2:207. [DOI] [PubMed] [Google Scholar]
- 2.AlGhamdi AST. Corticotomy facilitated orthodontics: review of a technique. Saudi Dent J. 2010;22(1):1–5. doi: 10.1016/j.sdentj.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aljhani A, Zawawi KH. The use of mini-implants in en masse retraction for the treatment of bimaxillary dentoalveolar protrusion. Saudi Dent J. 2010;22(1):35–39. doi: 10.1016/j.sdentj.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Årtun J, Urbye KS. The effect of orthodontic treatment on periodontalbone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop. 1988;93(2):143–148. doi: 10.1016/0889-5406(88)90292-2. [DOI] [PubMed] [Google Scholar]
- 5.Cevidanes LHC, Motta A, Proffit WR, Ackerman JL, Styner M. Cranial base superimposition for 3-dimensional evaluation of soft-tissue changes. Am J Orthod Dentofacial Orthop. 2010;137(4):S120–S129. doi: 10.1016/j.ajodo.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cobo J, Argüelles J, Puente M, Vijande MD. Dentoalveolar stress from bodily tooth movement at different levels of bone loss. Am J Orthod Dentofacial Orthop. 1996;110(3):256–262. doi: 10.1016/S0889-5406(96)80008-4. [DOI] [PubMed] [Google Scholar]
- 7.Dahlberg G. Statistical methods for medical and biological students. Public Health. 1940;54:92–93. doi: 10.1016/S0033-3506(40)80086-3. [DOI] [Google Scholar]
- 8.Decker JD, Chen C. Adaptive response of the human dentoalveolar process: correction of a Class I protrusive and mutilated dentition, with 32-year follow-up. Am J Orthod Dentofacial Orthop. 2009;135(4):113–122. doi: 10.1016/j.ajodo.2007.04.048. [DOI] [PubMed] [Google Scholar]
- 9.Edwards JG. A study of the anterior portion of the palate as it relates to orthodontic therapy. Am J Orthod. 1976;69(3):249–273. doi: 10.1016/0002-9416(76)90075-0. [DOI] [PubMed] [Google Scholar]
- 10.Evangelista K, Vasconcelos KF, Bumann A, Hirsch E, Nitka M, Silva MA. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138(2):133.e1–133e7. doi: 10.1016/j.ajodo.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 11.Frost HM. Mathematical Elements of Lamellar Bone Remodeling. Springfield, Illinois: Charles C Thomas; 1964. pp. 22–25. [Google Scholar]
- 12.Frost HM. Wolff’s law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64(3):175–188. doi: 10.1043/0003-3219(1994)064<0175:WLABSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Fuhrmann R. Three-dimensional interpretation of periodontal lesions and remodeling during orthodontic treatment. J Orofac Orthop. 1996;57(4):224–237. doi: 10.1007/BF02190235. [DOI] [PubMed] [Google Scholar]
- 14.Fuhrmann R. Three-dimensional evaluation of periodontal remodeling during orthodontic treatment. Semin Orthod. 2002;8(1):23–28. doi: 10.1053/sodo.2002.28168. [DOI] [Google Scholar]
- 15.Garib DG, Yatabe MS, Ozawa TO, da Silva Filho OG. Alveolar bone morphology under the perspective of the computed tomography: defining the biological limits of tooth movement. Dental Press J Orthod. 2010;15(5):192–205. doi: 10.1590/S2176-94512010000500023. [DOI] [Google Scholar]
- 16.Geramy A. Alveolar bone resorption and the center of resistance modification (3-D analysis by means of the finite element method) Am J Orthod Dentofacial Orthop. 2000;117(4):399–405. doi: 10.1016/S0889-5406(00)70159-4. [DOI] [PubMed] [Google Scholar]
- 17.Houston WJB. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83(5):382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 18.Hwang CJ, Moon JL. The limitation of alveolar bone remodeling during retraction of the upper anterior teeth. Korean J Orthod. 2001;31(1):97–105. [Google Scholar]
- 19.Kim SJ, Park YG, Kang SG. Effects of Corticision on paradental remodeling in orthodontic tooth movement. Angle Orthod. 2009;79(2):284–291. doi: 10.2319/020308-60.1. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y, Park JU, Kook YA. Alveolar bone loss around incisors in surgical skeletal Class III patients: a retrospective 3-D CBCT study. Angle Orthod. 2009;79(4):676–682. doi: 10.2319/070308-341.1. [DOI] [PubMed] [Google Scholar]
- 21.Lai EH, Yao CC, Chang JZ, Chen I, Chen YJ. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008;134(5):636–645. doi: 10.1016/j.ajodo.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 22.Liou EJ, Chang PM. Apical root resorption in orthodontic patients with en-masse maxillary anterior retraction and intrusion with miniscrews. Am J Orthod Dentofacial Orthop. 2010;137(2):207–212. doi: 10.1016/j.ajodo.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 23.Liu H, Liu DX, Wang GC, Wang CL, Zhao Z. Accuracy of surgical positioning of orthodontic miniscrews with a computer-aided design and manufacturing template. Am J Orthod Dentofacial Orthop. 2010;137(6):728.e1–728e10. doi: 10.1016/j.ajodo.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 24.Liu H, Lv T, Zhao F, Wang KT, Liu DX. Drift characteristics of miniscrews and molars for anchorage under orthodontic force: 3-dimensional computed tomography registration evaluation. Am J Orthod Dentofacial Orthop. 2011;139(1):e83–e89. doi: 10.1016/j.ajodo.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Mah JK, Huang JC, Choo H. Practical applications of cone-beam computed tomography in orthodontics. J Am Dent Assoc. 2010;141(3):7–13. doi: 10.14219/jada.archive.2010.0361. [DOI] [PubMed] [Google Scholar]
- 26.Meikle MC. The dentomaxillary complex and overjet correction in Class II, division 1 malocclusion: objectives of skeletal and alveolar remodeling. Am J Orthod. 1980;77(2):184–197. doi: 10.1016/0002-9416(80)90006-8. [DOI] [PubMed] [Google Scholar]
- 27.Meikle MC. The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur J Orthod. 2006;28(3):221–240. doi: 10.1093/ejo/cjl001. [DOI] [PubMed] [Google Scholar]
- 28.Milne TJ, Ichim I, Patel B, McNaughton A, Meikle MC. Induction of osteopenia during experimental tooth movement in the rat: alveolar bone remodelling and the mechanostat theory. Eur J Orthod. 2009;31(3):221–231. doi: 10.1093/ejo/cjp032. [DOI] [PubMed] [Google Scholar]
- 29.Nada RM, Maal TJ, Breuning KH, Berge SJ, Mostafa YA, Kuijpers-Jagtman AM. Accuracy and reproducibility of voxel based superimposition of cone beam computed tomography models on the anterior cranial base and the zygomatic arches. PLoS One. 2011;6(2):e16520. doi: 10.1371/journal.pone.0016520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakasima A, Terajima M, Mori N, Hoshino Y, Tokumori K, Aoki Y, Hashimoto S. Three-dimensional computer-generated head model reconstructed from cephalograms, facial photographs, and dental cast models. Am J Orthod Dentofacial Orthop. 2005;127(3):282–292. doi: 10.1016/j.ajodo.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 31.Naraghi S. Pattern and Amount of Change of Upper Front Teeth after Retention with a Bonded Retainer. Follow-up One to Seven Years Post Retention. Göteborg: Department of Orthodontics Institute of Odontology at the Sahlgrenska Academy University of Gothenburg, Intellecta Infolog AB; 2010. pp. 31–33. [Google Scholar]
- 32.Nelson LA, Michael SD. The application of volume deformation to three-dimensional facial reconstruction: a comparison with previous techniques. Forensic Sci Int. 1998;94(3):167–181. doi: 10.1016/S0379-0738(98)00066-8. [DOI] [PubMed] [Google Scholar]
- 33.Nelson PA, Artun J. Alveolar bone loss of maxillary anterior teeth in adult orthodontic patients. Am J Orthod Dentofacial Orthop. 1997;111(3):328–340. doi: 10.1016/S0889-5406(97)70192-6. [DOI] [PubMed] [Google Scholar]
- 34.Park HS, Lee YJ, Jeong SH, Kwon TG. Density of the alveolar and basal bones of the maxilla and the mandible. Am J Orthod Dentofacial Orthop. 2008;133(1):30–37. doi: 10.1016/j.ajodo.2006.01.044. [DOI] [PubMed] [Google Scholar]
- 35.Reitan K. Effects of force magnitude and direction of tooth movement on different alveolar bone types. Angle Orthod. 1964;34(4):244–255. [Google Scholar]
- 36.Reitan K, Kvam E. Comparative behavior of human and animal tissue during experimental tooth movement. Angle Orthod. 1971;41(1):1–14. doi: 10.1043/0003-3219(1971)041<0001:CBOHAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 37.Sarikaya S, Haydar B, Ciğer S, Ariyürek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122(1):15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 38.Shimpo S, Horiguchi Y, Nakamura Y, Lee M, Oikawa T, Noda K, Kuwahara Y, Kawasaki K. Compensatory bone formation in young and old rats during tooth movement. Eur J Orthod. 2003;25(1):1–7. doi: 10.1093/ejo/25.1.1. [DOI] [PubMed] [Google Scholar]
- 39.Vannier MW. Craniofacial computed tomography scanning: technology, applications and future trends. Orthod Craniofac Res. 2003;6(s1):23–30. doi: 10.1034/j.1600-0544.2003.232.x. [DOI] [PubMed] [Google Scholar]
- 40.Wehrbein H, Fuhrmann RAW, Diedrich PR. Human histologic tissue response after longer term orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 1995;107(4):360–371. doi: 10.1016/S0889-5406(95)70088-9. [DOI] [PubMed] [Google Scholar]
- 41.Yao CC, Lai EH, Chang JZ, Chen I, Chen YJ. Comparison of treatment outcomes between skeletal anchorage and extraoral anchorage in adults with maxillary dentoalveolar protrusion. Am J Orthod Dentofacial Orthop. 2008;134(5):615–624. doi: 10.1016/j.ajodo.2006.12.022. [DOI] [PubMed] [Google Scholar]