Abstract
Takayasu's arteritis is an inflammatory disease of unknown origin involving aorta, its primary branches and pulmonary artery. This article briefly reviews the pathology, clinical features and treatment of Takayasu's arteritis, focusing mainly on the disease in children.
MeSH: Takayasu's arteritis, Aortoarteritis, Vasculitis, Heart failure, Angioplasty
Introduction
Takayasu's arteritis is a chronic inflammatory disease that involves the aorta, its branches and the pulmonary arteries1–5. The inflammation results in varying degree of stenosis, occlusion or dilatation of the involved vessels. The aetiology and the precise pathogenesis of Takayasu's arteritis are still unknown but much has been learnt about the disease since its initial description by M.Takayasu, a Japanese ophthalmologist in 1908.6 This article reviews the salient features of Takayasu's arteritis, especially as seen in children.
Epidemiology
Takayasu's arteritis is recognised world-wide, although it is commoner in south-east Asia, Africa and south America.7 This disease is the commonest cause of renovascular hypertension in Asian children,8 but exact prevalence data is not available. A systematic survey in Japan during 1982-84 revealed 2,600 patients of Takayasu's arteritis,9 and the incidence was estimated at 2.6 per million persons/year in USA10 and 1.2 per million persons/year in Sweden in hospital based studies.11
Takayasu's arteritis is predominantly a disease of young adults in the second and third decades of life. The onset of illness may be earlier, including in childhood12,13 but rarely in infancy.14 The female:male ratio has varied from 9: 1 in reports from Japan9 to 1.3: 1 in India.15 The female preponderance is less obvious in children.15–17 Interestingly, the pattern of vessel involvement in Takayasu's arteritis also varies in different parts of the world.18 The involvement of the aortic arch and its branches is common in Japan, whereas the thoracoabdominal aorta is mainly involved in patients from Korea and India. It is not known whether this variation reflects differing causes of Takayasu's arteritis. Racial variation also occurs as the disease is uncommon in Caucasians. Moreover, in Israel, Takayasu's arteritis is seen in Sepharadic jews but not in Ashkanazi Jews.9
Genetic susceptibility to Takayasu's arteritis has been extensively studied. There are heterogeneous population data regarding HLA associations in TA. HLA B-52 and DR-2 are associated with Takayasu's arteritis in Japan,19 HLAB-52 and B-5 association is also reported from Korea and India,18 whereas HLA B-39 is frequently found in Mexican Takayasu's arteritis patients.20 Further characterisation of HLA association in Takayasu's arteritis is being studied in order to identify alleles or epitopes responsible for the susceptibility to this disease.20,21
Histopathology
TA involves mainly the elastic arteries.1,22,23 The disease may be patchy with normal skip areas in between, or diffuse along the length of the entire vessel. In the initial acute stage of the disease, exudative and granulomatous inflammation is seen, whereas fibrosis predominates later, but the two stages may co-exist.23 The initial site of inflammation is around vasa vasorum in the media and the adventitia. Mononuclear cell infiltration predominates and granulomas with giant cells (epitheloid or foreign body type) are seen. Fragmentation of elastic fibres (elasticophagia) is prominent.23 Destruction of the smooth muscle cells in the media leads to weakening of the vessel wall and dilatation. Deposition of ground substance rich in acid mucopolysachharide and reactive fibrosis occurs in the intima at the site of medial inflammation.22 Later in the disease process, nodular fibrosis in all layers of the artery is seen and the intima may become several times thicker than media (Figure 1) obliterating the lumen. Rapid or more severe inflammation leads to vessel dilatation and aneurysm formation, but stenosis and occlusions are more common. Thromboses in stenosed arteries are sometimes seen. The corresponding organ shows ischaemic changes, and this ischaemia largely determines the clinical features of the disease.
Figure 1.

Pathology in the chronic phase of Takayasu's arteritis showing fibrosis in all the layers of the vessel wall and markedly thickened intima (arrow)
Pathogenesis
The exact pathogenesis of Takayasu's arteritis is unknown. It's relationship to tuberculosis has long been debated.24 Takayasu's arteritis is more common in the parts of the world with high incidence of tuberculosis, but exceptions like Japan are intriguing.25 Case reports of occurrence of Takayasu's arteritis with rheumatoid arthritis,3 ulcerative colitis,26 systemic lupus,27 Crohn's disease,28 sarcoidosis12,29 amyloidosis30 etc, although sporadic, may indicate immune mechanisms in the pathogenesis. Relatively little information about the disease in the acute stage is available. Aetiopathogensis may not be obvious by studying the chronic phase of the disease, as in rheumatic heart disease. Evidence from the study of lesions in the active phase suggests that inflammation results from cell mediated immune responses.31. A number of lymphocytes (αβ-Tcells, γδ T cells and natural killer cells) infiltrate and incite the damage by liberating perforin on to arterial tissue. Further characterisation of T-cells receptors suggests that these cells are reactive to particular antigen/s.31 The exact antigens involved remain unknown. However, evidence is mounting that heat shock protein(HSP)-65 may be one of the important antigens. HSP-65 is a major antigen of mycobacterium tuberculosis, BCG and many other bacterial species as well as synthesised by tissues in response to stress.32 Cross reactivity and sequence homology between HSP-65 and HLA class II molecules has been described.32 Moreover, expression of HSP-65, HLA class I and II antigens is also markedly increased in affected aortic tissue.31 Thus, genetically linked immune responses to unidentified antigen may incite autoimmune damage by cell mediated pathways, and may result in the disease and relapses. A detailed discussion on immunopathogenesis of Takayasu's arteritis has recently been published.32
Diagnosis
The criteria for the diagnosis of Takayasu's arteritis as suggested by Ishikawa33 are shown in Table 1. The criteria adopted by the American College of Rheumatology are shown in Table 2.34 None of the diagnostic criteria are entirely satisfactory, but the clinical diagnosis in the proper context is seldom difficult. Essentially, the diagnosis depends on the typical angiographic morphology, history or presence of constitutional symptoms suggestive of a systemic illness, and the differential diagnosis of other, similar conditions such as other causes of inflammatory aortitis (e.g. syphilis, tuberculosis, giant cell arteritis, Buerger's, Behcet's, Cogan and Kawasaki diseases, spondyloarthropathies), developmental abnormalities (e.g. Ehlers-Danlos syndrome, Marfan's syndrome) Other aortic abnormalities such as neurofibromatosis, ergotism and radiation fibrosis need to be excluded.12 Atherosclerosis of aorta is distinguished on clinical and morphological grounds, but secondary atherosclerotic changes may occur in older patients with Takayasu's arteritis.
Table 1.
Ishikawa's criteria for the clinical diagnosis of Takayasu's disease
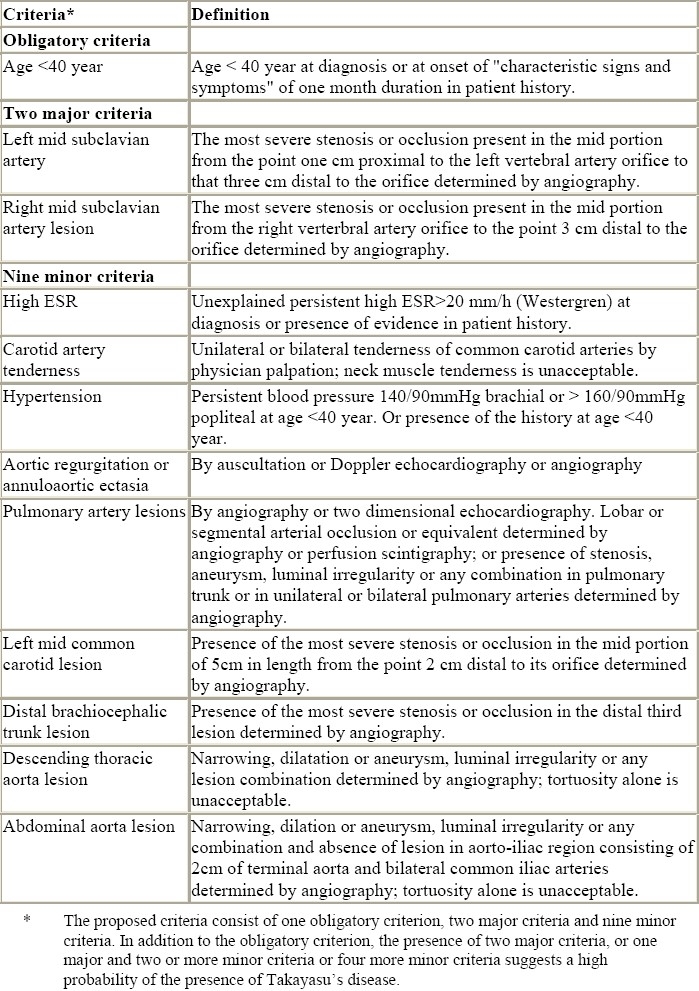
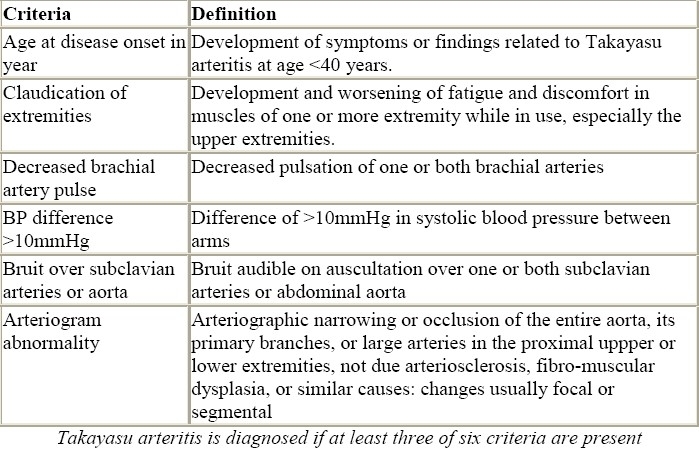
Table 2.
1990 criteria of American College of Rheumatology for the classification of Takayasu arteritis
Angiographic morphology
Conventional or digital subtraction angiography has been considered the gold standard for the diagnosis of Takayasu's arteritis. Angiography shows luminal irregularity, vessel stenosis, occlusion, dilatation or aneurysms in the aorta or its primary branches.
Neurofibromatosis of the abdominal aorta and some other causes of mid-aortic syndrome may produce an identical angiographic picture in children.35 Based on angiographic morphology, Takayasu's arteritis is divided into type I (involving aortic arch and its branches), type II (thoracoabdominal aorta and its branches) and type III (involving lesions of both type I & II) (Figures 2 and 3). Involvement of pulmonary arteries in addition to any of the above types is grouped as type IV.4,12
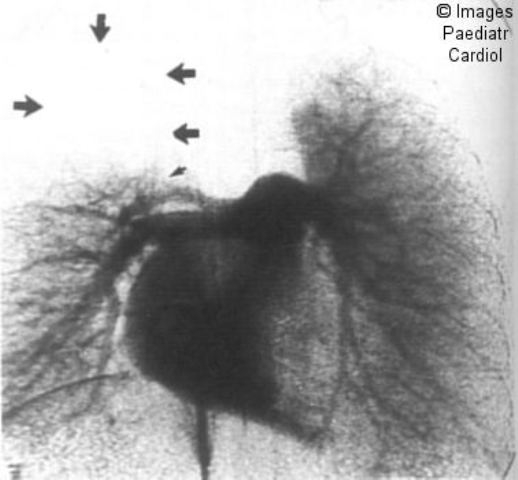
Figure 2.

Severe type I arteritis with complete occlusion of left carotid and subclavian artery. The right subclavian artery is also occluded
Figure 3.

Extensive Thoracoabdominal aortic involvement
Involvement of the left and right subclavian arteries is very common in Takayasu's arteritis. Thoracoabdominal aortic involvement is commoner (type II/III) in children.15–17 The infrarenal aorta or the iliac vessels are not usually involved in Takayasu's arteritis. Similarly, the inferior mesentric artery is rarely involved. Unlike coarctation of the aorta, intercostal collaterals rarely occur as the diffuse intimal disease in the aorta also involves the ostia of these intercostal vessels (Figure 4). Aortic intimal calcification may be seen.
Figure 4.

The disease in a 4-year old child. Note the diffuse involvement of descending aorta and paucity of collaterals
Saccular or fusiform aneurysms of the aorta occur in 2-26% of cases, and usually coexist with stenotic lesions.36,37 Aneurysms without stenosis occur in 1-2% of cases.36 Pseudoaneurysm or dissection of the aorta are extremely rare.23
The angiographic features reflect only the luminal aspects of inflammation and occur relatively late in the course of the disease. More recently, cross-sectional imaging with helical computerised tomography,38 ultrasound39 or contrast enhanced magnetic resonance imaging40 provide information on mural changes of the vessels. computerised tomography scan may reveal aortic wall thickness (Figure 5) and aortic calcification, helical computerised tomography angiography may show enhancement of thickened aortic wall with inflammation. Similarly, T1-weighted contrast enhanced magnetic resonance imaging also depicts wall thickness and its enhancement with activity of the disease. These noninvasive modalities may replace angiography for the diagnosis, and for monitoring therapy and progression of the disease.
Figure 5.
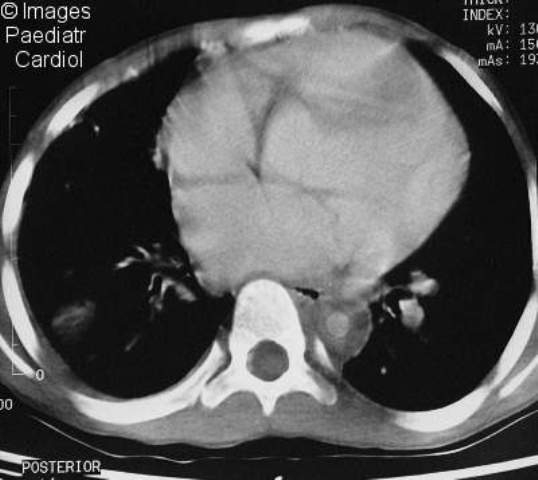
Contrast enhanced CT scan showing concentric, thickened aortic walls of the descending thoracic aorta
Clinical features
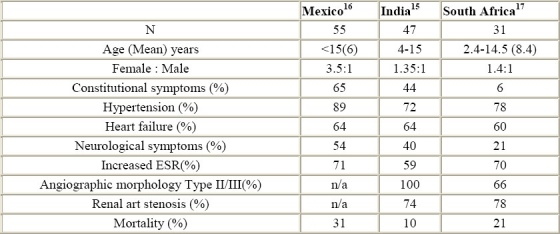
Takayasu's arteritis has an early active inflammatory phase and a late chronic, but many patients do not give a history suggestive of previous inflammatory illness. The active phase of the illness lasts for weeks to months, and may have a remitting and relapsing course. Constitutional symptoms like fever, anorexia, loss of weight, night sweats, arthralgia, skin rash etc. may occur during the active phase but the correct diagnosis of Takayasu's arteritis is seldom made in the early phase. Evidence of vessel inflammation such as tenderness along arteries, bruits and aneurysm may point to the diagnosis of Takayasu's arteritis. The clinical features in three large series from different parts of the world are shown in table 3. Systemic symptoms are seen in a high proportion of children with Takayasu's arteritis. The usual presenting symptoms are due to hypertension, heart failure or a neurological event. Claudication, bruit or a missing pulse in an asymptomatic child are other uncommon presentations. Children with Takayasu's arteritis have higher morbidity and mortality than adults.15,16
Table 3.
Takayasu's arteritis in children
Hypertension in Takayasu's arteritis results from renal artery stenosis or aortic narrowing and aortic fibrosis. It is often severe and may cause hypertensive encephalopathy or heart failure. Takayasu's arteritis is the commonest cause of renovascular hypertension in Asian children. The diagnosis of Takayasu's arteritis may be suggested by a missing pulse or a renal or aortic bruit. However, these are not universal. The diagnosis of hypertension may be entirely missed if all the peripheral pulses are not carefully examined. Renal arterial stenosis may be bilateral and usually coexists with aortic involvement41,42 (Figure 6). The ostia of the renal arteries are commonly involved, but the intrarenal vasculature and small vessels are generally normal. Therefore the use of ACE inhibitors in Takayasu's arteritis needs to be carefully considered and such drugs preferably started only after obtaining an aortogram.43
Figure 6.

Digital subtraction angiogram of a 9-year old boy showing bilateral renal arterial stenosis and severe perirenal aortic narrowing
Heart failure from Takayasu's arteritis is common in children (Table 3) and is an important cause of mortality. Hypertension is the most common reason for heart failure, but may occur in the absence of severe hypertension.15 Myocarditis, coronary arterial involvement, organic valvar involvement, or pulmonary artery involvement may cause or contribute to the heart failure. Frequently, children with heart failure and Takayasu's arteritis are misdiagnosed as having dilated cardiomyopathy as the echocardiogram shows systolic ventricular dysfunction and hypertension may be missed. Mild hypertension in the presence of severe heart failure, left ventricular hypertrophy on echocardiogram, or a dilated aorta may point to the correction diagnosis.
Familiarity with the disease may suggest the correct diagnosis, even when no obvious pointers are present. Half of the children with heart failure have mitral regurgitation and rheumatic heart disease may be falsely diagnosed.15 Aortic regurgitation from a dilated aorta is rarely seen in children. Treatment of hypertension or aortic obstruction ameliorates the heart failure in the majority of children. However, heart failure in the absence of hypertension suggests myocarditis as a cause for ventricular dysfunction. Myocarditis in Takayasu's arteritis is rare and may respond to immunosuppresive treatment.44
Coronary arterial involvement in Takayasu's arteritis is usually ostial and proximal (Figure 7), but diffuse lesions or arteritis and aneurysm rarely occur.45,46 About 10% of adult patients with Takayasu's arteritis have coronary arterial involvement but the incidence in children has not been studied. Coronary arterial involvement may cause myocardial infarction,47 angina or heart failure and may necessitate angioplasty, or surgical treatment even in children.48,49
Figure 7.

Left main coronary arterial narrowing in a 16 year old girl with Takayasu's arteritis (Reproduced with permission from Ref. 46)
Pulmonary arterial involvement has been found in nearly 70% of the patients on angiographic studies50,51, but is usually mild. Pulmonary artery involvement correlates with extensive aortic involvement50 but pulmonary arterial involvement as the only lesion or as presenting manifestation of disease is also described.52 The disease involves segmental and subsegmental branches, more in the upper lobes but larger branches may be involved (Figure 8). The angiographic picture may closely mimic thromboembolism. A history of haemoptysis, chest pain, disproportionate pulmonary arterial hypertension, or abnormal ventilation-perfusion scan53 may suggest pulmonary involvement. Response of pulmonary arterial lesions to therapy has not been well studied.
Figure 8.
Pulmonary arterial involvement in a young child (Reproduced with permission from Ref. 51)
Neurological symptoms such as headache, visual disturbances and amaurosis fugax are common in Takayasu's arteritis. Syncope and transient ischaemic attacks may occur due to severe carotid or vertebral artery stenosis. In children, cerebrovascular accidents are often secondary to severe hypertension and its complications. Hypertensive retinopathy is commoner than ischemic retinopathy in Takayasu's arteritis.54 Type I Takayasu's arteritis involving the aortic arch and its branches is uncommon in children (Table 3).
Assessment of disease activity
The presence of systemic symptoms, raised ESR and worsening of vessel stenosis are considered evidence of active disease (Table 4).12 However, histological evidence of disease have been observed in clinically inactive disease,55 and angiographic progression of disease has occurred in the absence of clinically active disease.12 Recent advances in noninvasive imaging may assist in identifying active inflammation.38,40
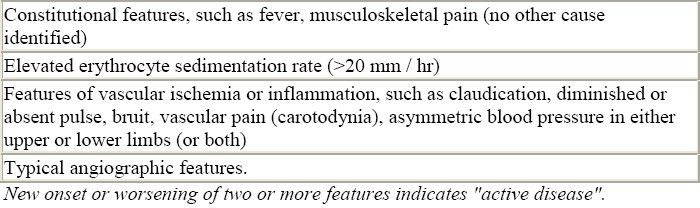
Table 4.
Criteria for Active Disease in Patients with Takayasu Arteritis12
Interestingly, raised interleukin-6 and RANTES have been reported to correlate with the disease activity, and may prove useful in the monitoring of therapy.56
Treatment
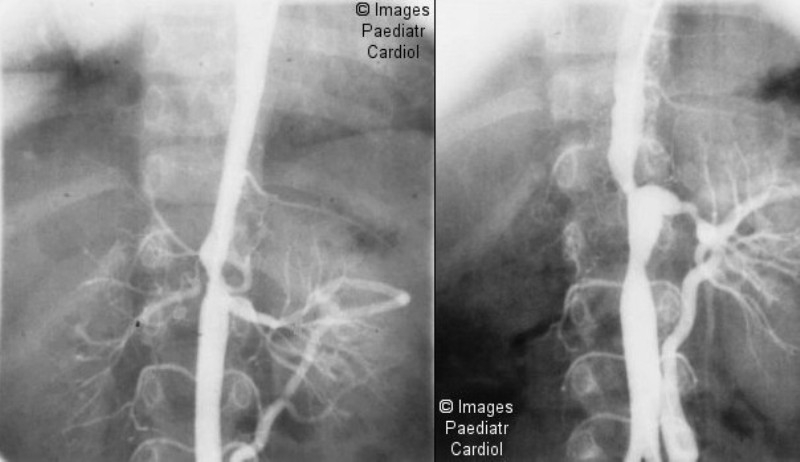
In the acute phase of TA, treatment with corticosteroids (1mg/kg/d) leads to clinical remission in 60% of cases.12 Immunosuppression with cyclosphosphamide (1-2mg/kg/d), azathioprin (1-2mg/kg/d) or methotrexate (0.15-0.35 mg/kg/week) may be tried in resistant cases, or in order to reduce steroid dosages.12 The duration of treatment varies empirically on clinical assessment of activity. Median duration to remission was 11 months in children in one series,12 but there are, to date, no large studies involving children. Rare instances of reappearance of pulses or a reduction in renal artery stenosis with steroid treatment have been reported.57,58 The major morbidity and mortality of Takayasu's arteritis results from stenosis and occlusion of the aorta, renal and carotid arteries. Balloon dilatation of stenosed segments has revolutionised the treatment of Takayasu's arteritis. Percutaneous transluminal renal arterial dilatation (PTRA) is successful in up to 90% of cases41,42 and blood pressure control is achieved in 60% (Figure 9).
Figure 9.
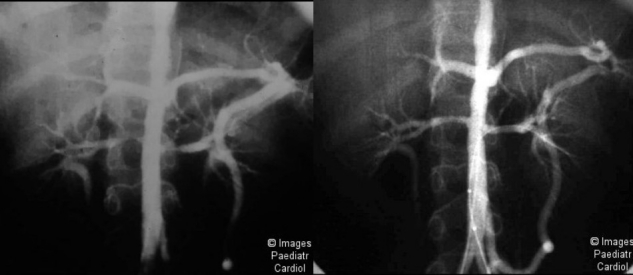
Percutaneous transluminal renal arterial dilatation of bilateral renal artery stenosis in a child (a) before and (b) after dilatation
Restenosis may occur in 20-25% cases. Renal artery stents are not usually required. Balloon dilatation is preferably done in the chronic phase of disease, but successful dilatation may be done during acute phase of Takayasu's arteritis, if required (unpublished observation). Similarly, balloon dilatation of aortic narrowing is highly effective even in diffuse, long segment stenoses (Figure 10).
Figure 10.

Balloon dilatation of severe, long segment aortic narrowing (a) before and (b) after the dilatation
Close to 90% success rates have been reported for aortic angioplasty in children.59,60 Restenosis may occur in 14-20% at follow-up. Suboptimal results may be observed in long segment stenosis but clinical benefits usually occurs even with these. Remarkable recovery from heart failure follows successful dilatation59,60 (Figure 11). The use of stents in children with Takayasu's arteritis is discouraged and small dissecting flaps may heal well. However, stents have also been successfully used to treat occlusive dissecting flaps, or aortic obstruction.61 Interventional treatment of carotid stenosis, although uncommonly involved in children, is also feasible.62 Because of the diffuse, inflammatory and possibly progressive nature of the disease, surgical treatment is not preferred for Takayasu's arteritis except for undilatable symptomatic stenotic lesions and for large aneurysms.63
Figure 11.
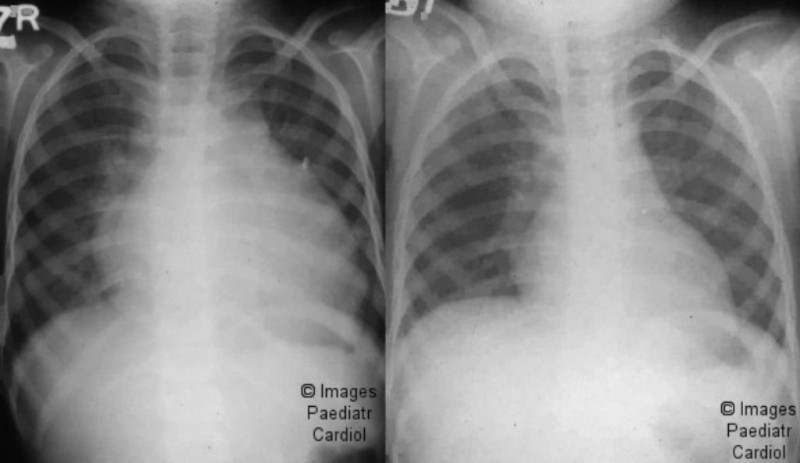
The chest x-rays of the same patient as in figure 10. (a) before, and (b) 3 months after the dilatation
Prognosis
Takayasu's arteritis in children is a serious illness and a mortality of 10-30% has been reported on followup.15–17 More recently, the prognosis has significantly improved due to interventional procedures for the treatment of renal and aortic stenosis. Long term follow up data on children is not available. In a study of 88 adults with Takayasu's arteritis, 5 and 10 year survival after the onset of disease was 91% and 84% respectively.64 The presence of severe Takayasu's arteritis (defined as the presence of severe grades of hypertension, aortic regurgitation, retinopathy, or aneurysms), poor functional class or cardiac involvement, predicted a poorer outcome. A relatively stable course is anticipated in the absence of severe complications. Successful pregnancies have been reported in patients with Takayasu's arteritis.65 Chronic, burnt out lesions of Takayasu's arteritis remain stable for years. In an angiogrphic study, after a seven year followup, the lesions remained stable in 80% of patients.66 However, the progression of lesions even in the absence of obvious clinical activity has also been described (Figure 12).12
Figure 12.
The progression of the disease over 1 year in a young boy. Note the development of renal artery aneurysm and disease involving the infrarenal aorta (below)
Clearly, much remains to be learnt about Takayasu's arteritis. This enigmatic disease still remains a challenge.
References
- 1.Nasu T. Pathology of pulseless disease: A systematic study and critical review of twenty-one autopsy cases reported in Japan. Angiology. 1963;14:225–242. doi: 10.1177/000331976301400502. [DOI] [PubMed] [Google Scholar]
- 2.Sen PK, Kinare SG, Kelkar MD, Parulkar GB. nonspecific Aortoarteritis-A Monographi Based on a Study of 101 cases. Bombay: Tata McGraw-Hill publishing Co; 1972. [Google Scholar]
- 3.Nakao K, Ikeda M, Kimata S, Niitani H, Miyahara M, Ishimi Z, Hashiba K, Takeda Y, Ozawa T, Matsushita S, Kuramochi M. Takayasu's arteritis. Clinical report of eighty four cases and immunological studies of seven cases. Circulation. 1967;35:1147–1155. doi: 10.1161/01.cir.35.6.1141. [DOI] [PubMed] [Google Scholar]
- 4.Lupi-Herrera E, Sanchez-Torres G, Marcushamer J, Mispireta J, Horwitz S, Vela JE. Takayasu's arteritis. Clinical study of 107 cases. Am Heart J. 1977;93:94–103. doi: 10.1016/s0002-8703(77)80178-6. [DOI] [PubMed] [Google Scholar]
- 5.Ishikawa K. Natural history and classification of occlusive thromboartopathy (Takayasu's disease) Circulation. 1978;57:27–35. doi: 10.1161/01.cir.57.1.27. [DOI] [PubMed] [Google Scholar]
- 6.Takayasu M. Case with unusual changes of the central vessels in the retina (in Japanese) Acta Soc Ophthal Jap. 1908;12:554–555. [Google Scholar]
- 7.Lande A, Bard R, Rossi P, Passariello R, Castrucci A. Takayasu's arteritis. A world-wide entity. NY State J Med. 1976;32:379–392. [PMC free article] [PubMed] [Google Scholar]
- 8.Chugh KS, Sakhuja V. Takayasu's arteritis as a cause of renovascular hypertension in Asian countries. Am J nephrol. 1992;306:464–465. doi: 10.1159/000168409. [DOI] [PubMed] [Google Scholar]
- 9.Sekiguchi M, Sazuki J. An overview of Takayasu Arteritis. Heart Vessels. 1992;(Suppl 7):6–10. doi: 10.1007/BF01744537. [DOI] [PubMed] [Google Scholar]
- 10.Hall S, Barr W, Lie JT. Takayasu arteritis. A study of 32 North American patients. Medicine (Baltimore) 1985;64:89–99. [PubMed] [Google Scholar]
- 11.Waern AU, Andersson P, Hemmingson A. Takayasu's arteritis: A hospital region based study on occurrence, treatment and prognosis. Angiology. 1983;34:311–320. doi: 10.1177/000331978303400504. [DOI] [PubMed] [Google Scholar]
- 12.Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS. Takayasu arteritis. Ann Intern Med. 1994;120:919–929. doi: 10.7326/0003-4819-120-11-199406010-00004. [DOI] [PubMed] [Google Scholar]
- 13.Ladhani S, Tulloh R, Anderson D. Takayasu disease masquarading as interruption of the aortic arch in a 2 year old child. Cardiol Young. 2001;11:244–246. doi: 10.1017/s104795110100021x. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell CS, Parisi MT. Magnetic resonance imaging of Takayasu's aortitis in an infant. J Am Osteopath Assoc. 1997;97:607–609. doi: 10.7556/jaoa.1997.97.10.607. [DOI] [PubMed] [Google Scholar]
- 15.Shrivastava S, Srivastava RN, Tandon R. Idiopathic obstructive aortoarteritis in children. Indian Paediatr. 1986;23:403–410. [PubMed] [Google Scholar]
- 16.Hahn D, Thomson PD, Kala U, Beale PG, Levin SE. A review of Takayasu's arteritis in children in Guateng, South Africa. Pediatr nephrol. 1998;12:668–675. doi: 10.1007/s004670050526. [DOI] [PubMed] [Google Scholar]
- 17.Dabague J, Reyes PA. Takayasu's arteritis in mexico: a 38 year clinical perspective through literature review. Int J Cardiol. 1996;54(Suppl):S87–S93. doi: 10.1016/s0167-5273(96)88779-1. [DOI] [PubMed] [Google Scholar]
- 18.Yajima M, Numano F, Park YB, Sagar S. Comparative studies of patients with Takayasu arteritis in Japan, Korea and India. Comparison of clinical manifestations, angiography, and HLA-B antigen. Jpn Circ J. 1994;58:9–14. doi: 10.1253/jcj.58.9. [DOI] [PubMed] [Google Scholar]
- 19.Kimura A, Ota M, Katsuyama Y, Ohbuchi N, Takahashi M, Kobayashi Y, et al. Mapping of the HLA-linked genes controlling the susceptibility to Takayasu's arteritis. Int J Cardiol. 2000;75:S105–A110. doi: 10.1016/s0167-5273(00)00178-9. [DOI] [PubMed] [Google Scholar]
- 20.Vargas-Alarcon G, Zuniga J, Gamboa R, Harnandez-pacheco G, Hesiquio R, Cruz D, et al. DNA sequencing of HLA-B allels in Mexican patients with Takayasu arteritis. Int J Cardiol. 2000;75:S117–S122. doi: 10.1016/s0167-5273(00)00188-1. [DOI] [PubMed] [Google Scholar]
- 21.Yoshido M, Kimura T, Katsuragi K, Numano F, Sasazuki T. DNA typing of HLA-B gene in Takayasu arteritis. Tissue antigens. 1993;42:87–90. doi: 10.1111/j.1399-0039.1993.tb02242.x. [DOI] [PubMed] [Google Scholar]
- 22.Kinare SG, Gandhi MS, Deshpande JR. Mumbai: 1998. Non-specific aortoarteritis (pathology and radiology) monograph published by Quest publications. [Google Scholar]
- 23.Hotchi M. Pathological Studies on Takayasu arteritis. Heart vessels. 1992;(Suppl 7):11–17. doi: 10.1007/BF01744538. [DOI] [PubMed] [Google Scholar]
- 24.Sen PK, Kinare SG, Kelkar MD, Nanivadkar SA. Nonspecific stenosing arteritis of the aorta and its branches: A study of possible aetiology. Mt Sinai J Med. 1972;39:221–242. [PubMed] [Google Scholar]
- 25.Kothari SS. Aetiopathogenesis of Takayasn's arteritis and BCG vaccination: The missing link? Medical Hypotheses. 1995;45:227–230. doi: 10.1016/0306-9877(95)90109-4. [DOI] [PubMed] [Google Scholar]
- 26.Achar KN, AI-Nakib B. Takayasu's arteritis and ulcerative colitis. Am J Gastroenterol. 1986;81:1215–1217. [PubMed] [Google Scholar]
- 27.Saxe PA, Altman RP. Takayasu's arteritis syndrome associated with systemic lupus erythematosis. Semin Arthritis Rheum. 1992;21:295–305. doi: 10.1016/0049-0172(92)90023-7. [DOI] [PubMed] [Google Scholar]
- 28.Lenhoff SJ, Mee AS. Crohn's disease of the colon with Takayasu's arteritis. Postgraduate Med J. 1982;58:386–389. doi: 10.1136/pgmj.58.680.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maeda S, Murao S, Sugiyama T, Utaka I, Okamoto R. Generalized sarcoidosis with sarcoid aortitis. Acta Pathol Jpn. 1983;33:183–188. [PubMed] [Google Scholar]
- 30.Dash SC, Malhotra KK, Sharma RK, Bhuyan UN. Renal amyloidosis and non-specific aortoarteritis- a hitherto unrecognized association. Postgraduate Med J. 1984;60:626–628. doi: 10.1136/pgmj.60.707.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seko Y, Minota S, Kawasaki A. Perforin secreting killer cell infiltration and expression of -KD heat shock protein in aortic tissue of patients with Takayasu's arteritis. J Clin Invest. 1994;93:750–758. doi: 10.1172/JCI117029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seko Y. Takayasu arteritis. Insights into immunopathology. Jpn Heart J. 2000;41:15–26. doi: 10.1536/jhj.41.15. [DOI] [PubMed] [Google Scholar]
- 33.Ishikawa K. Diagnostic approach and proposed criteria for the clinical diagnosis of Takayasu's arteriopathy. J Am Coll Cardiol. 1988;12:964–972. doi: 10.1016/0735-1097(88)90462-7. [DOI] [PubMed] [Google Scholar]
- 34.Arend WP, Michel BA, Bloch DA, Hunder GG, Calobrese lH, Edworthy SM, et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheumatism. 1990;33:1129–1132. doi: 10.1002/art.1780330811. [DOI] [PubMed] [Google Scholar]
- 35.Panayiotopoulos YP, Tyrell MR, Koffman G, Reidy JF, Haycock GB, Taylor PR. Mid-aortic syndrome presenting in childhood. Br J Surg. 1996;83:235–240. [PubMed] [Google Scholar]
- 36.Sharma S, Rajani M, Talwar KK. Angiographic morphology in nonspecific aortoarteritis (Takayasu's arteritis): a study of 126 patients from north India. Cardiovasc Intervent Radiol. 1992;15:160–165. doi: 10.1007/BF02735580. [DOI] [PubMed] [Google Scholar]
- 37.Kumar S, Subramanyan R, Mandalam KR. Aneurysmal form of aortoarteritis (Takayasu's disease); Analysis of thirty cases. Clinical Radiology. 1990;42:342–347. doi: 10.1016/s0009-9260(05)82150-6. [DOI] [PubMed] [Google Scholar]
- 38.Park JH, Chung JW, Im J-G, Kim SK, Park YB, Han MC. Takayasu arteritis: evaluation of mural changes in the aorta and pulmonary artery with CT angiography. Radiology. 1995;196:89–93. doi: 10.1148/radiology.196.1.7784596. [DOI] [PubMed] [Google Scholar]
- 39.Park SH, Chung JW, Lee JW, Han MH, Park JH. Carotid artery involvement in Takayasu's arteritis: evaluation of activity by ultrasonography. J Ultrasound Med. 2001;20:371–378. doi: 10.7863/jum.2001.20.4.371. [DOI] [PubMed] [Google Scholar]
- 40.Choe YH, Han BK, Koh EM, Kim DK, Do YS, Lee WR. Takayasu's arteritis; assessment of disease activity with contrast enhanced MR imaging. Am J Roent AJR. 2000;175:505–511. doi: 10.2214/ajr.175.2.1750505. [DOI] [PubMed] [Google Scholar]
- 41.Tyagi S, Kaul UA, Satsangi DK, Arora R. Percutaneous transluminal angioplasty for renovascular hypertension in children : Initial and long term results. Pediatrics. 1997;99:44–49. doi: 10.1542/peds.99.1.44. [DOI] [PubMed] [Google Scholar]
- 42.Sharma S, Saxena A, Talwar KK, Kaul U, Mehta SN, Rajani M. Renal artery stenosis caused by nonspecific arteritis (Takayasu disease): Results of treatment with percutaneous transluminal angioplasty. AJR AM J Roentgenol. 1992;158:417–422. doi: 10.2214/ajr.158.2.1346073. [DOI] [PubMed] [Google Scholar]
- 43.Kothari SS, Sharma M, Sharma S. Enalapril induced renal arterial thrombosis in unilateral renal arterial stenosis. Ind Heart J. 1997;49:192–194. [PubMed] [Google Scholar]
- 44.Talwar KK, Chopra P, Narula JS, Shrivastava S, Singh SK, Sharma S, Saxena A, Rajani M, Bhatia ML. Myocardial involvement and its response to immunosuppressive therapy in non specific aortoarteritis (Takayasu's disease) – A study by endomyocardial biopsy. Int J Cardiol. 1988;23:323–334. doi: 10.1016/0167-5273(88)90109-x. [DOI] [PubMed] [Google Scholar]
- 45.Matsubara O, Kuwata T, Nemoto T, Kasuga T, Numano F. Coronary artery lesions in Takayasu arteritis: Pathological considerations. Heart Vessels. 1992;(Suppl 7):26–31. doi: 10.1007/BF01744540. [DOI] [PubMed] [Google Scholar]
- 46.Talwar KK, Kumar K, Chopra P, Sharma S, Shrivastava S, Wasir HS, et al. Cardiac involvement in non-specific aortoarteritis (Takayasu's arteritis) Am Heart J. 1991;122:166–1670. doi: 10.1016/0002-8703(91)90285-p. [DOI] [PubMed] [Google Scholar]
- 47.Wolf RL, Gould NS, Green CA. Unusual arteritis causing myocardial infarction in a child. Arch Pathol Lab Med. 1987;111:968–971. [PubMed] [Google Scholar]
- 48.Lee HY, Rao PS. Percutaneous transluminal angioplasty in Takayasu's arteritis. Am Heart J. 1996;132:1084–1086. doi: 10.1016/s0002-8703(96)90036-8. [DOI] [PubMed] [Google Scholar]
- 49.Lall KS, Dombrowicz E, Pillay TM, Pollock JC. Coronary ostial patch angioplasty in children. Ann Thorac Surg. 1999;67:1478–1480. doi: 10.1016/s0003-4975(99)00221-0. [DOI] [PubMed] [Google Scholar]
- 50.Yamada I, Shibuya H, Matsubara O, Umehard I, Makino T, Numano F, Suzuki S. Pulmonary artery disease in Takayasu's arteritis: angiographic findings. AJR Am J Roent. 1992;159:263–269. doi: 10.2214/ajr.159.2.1352939. [DOI] [PubMed] [Google Scholar]
- 51.Sharma S, Kamalakar T, Rajani M, Talwar KK, Shrivastava S. The incidence and patterns of pulmonary artery involvement in Takayasu's arteritis. Clin Radiol. 1990;42:182–187. doi: 10.1016/s0009-9260(05)81929-4. [DOI] [PubMed] [Google Scholar]
- 52.Lie JT. Isolated pulmonary Takayasu arteritis. Clinicopathological characteristics. Modern Pathology. 1996;9:469–474. [PubMed] [Google Scholar]
- 53.Castellani MM, Vanoli MM, Cali GM, Bacchiani GM, Origgi CM, Reschini EM, Scorza RM, et al. Ventilation – perfusion lung scan for detecting pulmonary involvement in Takayasu's arteritis. Eur J Med. 2001;28:1801–1805. doi: 10.1007/s002590100648. [DOI] [PubMed] [Google Scholar]
- 54.Chun YS, Park SS, Park IK, Chung H, Lee J. The clinical and ocular manifestations of Takayasu's arteritis. Retino. 2001;21:132–140. doi: 10.1097/00006982-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 55.Lagneau P, Michel JB, Wuong PN. Surgical treatment for Takayasu's disease. Ann Surg. 1987;205:157–166. doi: 10.1097/00000658-198702000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Noris M, Daina E, Gamba S, Bonazzola S, Remuzzi G. Interleukin –6 and RANTES in Takayasu arteritis. A guide for therapeutic decisions? Circulation. 1999;100:55–60. doi: 10.1161/01.cir.100.1.55. [DOI] [PubMed] [Google Scholar]
- 57.Ishikawa K, Yonekawa Y. Regression of carotid stenoses after corticosteriod therapy in occlusive thromboaortopathy (Takayasu's disease) Stroke. 1987;18:677–679. doi: 10.1161/01.str.18.3.677. [DOI] [PubMed] [Google Scholar]
- 58.Kulkarni TP, D’ Cruz IA, Gandhi MJ, Dadich DS. Reversal of renovascular hypertension caused by nonspecific aortitis after corticosteroid therapy. Br Heart J. 1974;36:114–116. doi: 10.1136/hrt.36.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saxena A, Kothari SS, Sharma S, Juneja R, Shrivastava S. percutaneous transluminal angioplasty in children with nonspecific aortoarteritis. Acute and follow up results with special emphasis on left ventricular function. Cath Cardiovasc Interv. 2000;49:419–424. doi: 10.1002/(sici)1522-726x(200004)49:4<419::aid-ccd15>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 60.Tyagi S, Khan M, Kaul UA, Arora R. Percutaneous transluminal angioplasty for stenosis of aorta due to aortoarteritis in children. Paed Cardiol. 1999;29:404–410. doi: 10.1007/s002469900501. [DOI] [PubMed] [Google Scholar]
- 61.Bali HK, Jain S, Jain A, Sharma BK. Precutaneous angioplasty and stent placement in Takayasu arteritis. Int J Cardiol. 1998;66(Suppl I):S213–217. doi: 10.1016/s0167-5273(98)00171-5. [DOI] [PubMed] [Google Scholar]
- 62.Joseph G, Krishnaswami S, Baruah DK, Kuruttkulam SV, Abraham OC. Transseptal approach to aortography and carotid artery stenting in pulseless disease. Cathet Cardiovasc Diagn. 1997;40:416–420. doi: 10.1002/(sici)1097-0304(199704)40:4<416::aid-ccd23>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 63.Takagi A, Tada Y, Sato O, Miyata T. Surgical treatment of Takayasu's arteritis: A long term follow up study. J Cardiovasc Surg. 1989;30:553–558. [PubMed] [Google Scholar]
- 64.Subramanyan R, Joy J, Balakrishnan KG. Natural history of aortoarteritis (Takayasu's disease) Circulation. 1989;80:429–437. doi: 10.1161/01.cir.80.3.429. [DOI] [PubMed] [Google Scholar]
- 65.Matsumura A, Moriwaki R, Numano F. Pregnancy in Takayasu arteritis from the view of internal medicine. Heart vessels. 1992;(Suppl 7):120–124. doi: 10.1007/BF01744557. [DOI] [PubMed] [Google Scholar]
- 66.Mandalam KR, Subramanyan R, Joseph S, Rao VRK, Gupta AK, Unni NM, et al. Natural history of aortoarteritis: an angiographic study in 26 survivors. Clinical Radiology. 1994;49:38–44. doi: 10.1016/s0009-9260(05)82912-5. [DOI] [PubMed] [Google Scholar]


