Abstract
The latest revision of the International Standards for the Neurological Classification of Spinal Cord Injury (ISNCSCI) was available in booklet format in June 2011, and is published in this issue of the Journal of Spinal Cord Medicine. The ISNCSCI were initially developed in 1982 to provide guidelines for the consistent classification of the neurological level and extent of the injury to achieve reliable data for clinical care and research studies. This revision was generated from the Standards Committee of the American Spinal Injury Association in collaboration with the International Spinal Cord Society's Education Committee. This article details and explains the updates and serves as a reference for these revisions and clarifications.
Keywords: Physical examination, Neurological, Motor, Sensory, Classification, Spinal cord injuries, Manual muscle testing, International standards for the neurological classification of spinal cord injury, ASIA impairment scale, Revisions, American spinal injury association, International spinal cord society
Introduction
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) was initially developed in 1982 as the American Spinal Injury Association (ASIA) Standards for the Neurological Classification of Spinal Cord Injuries in order to develop greater precision in the definitions used to classify spinal cord injury (SCI).1 The ASIA Standards defined the neurological levels and the extent of the injury (utilizing the Frankel Scale)2 to achieve greater consistency and reliable data among centers participating in the National SCI Statistical Center Database.
Subsequently, major revisions were made in 1990, 1992, 1996, and 2000 (with reprints of the 2000 guidelines in 2002, 2006, and 2008).3 In 1992, the International Spinal Cord Society (ISCoS, then known as the International Medical Society of Paraplegia) endorsed the Standards, and with the 1996 revision, the Standards were renamed the International Standards for Neurological and Functional Classification of Spinal Cord Injury.4 The term ‘functional’ was deleted from the name in 2000.5,6 A reference manual was first published in 1994, with an updated version in 2003.7
In 2010, the International Standards Training e-Learning Program (InSTeP) was developed by ASIA, with updated recommendations for the neurological examination and classification as part of a web-based training program that is now available online.8 InSTeP includes a six-module course designed to enable clinicians to perform accurate and consistent neurological examinations of individuals with SCI. These modules include Basic Anatomy; Sensory Examination; Motor Examination; Anorectal Examination; Scoring, Scaling, and the ASIA Impairment Scale (AIS) Classification; and a module on Optional Testing. Additional training courses have been developed for the performance of the International Standards examination in the pediatric population (WeeSTep) as well as the Autonomic Standards e-Program.
The purpose of the SCI classification standards remains unchanged from that stated 25 years ago: ‘Accurate communication between clinicians and researchers working with spinal cord injury patients requires that standards be used in the classification of neurological impairment. Such standards can then be useful in clinical tools in the daily care of SCI patients, and also can be used as a base for detailed research protocols.’9 Subsequent widespread and consistent use of precisely defined classifications has facilitated clinical patient care as well as research in SCI medicine. Since the 2000 revision, there have been significant changes involving adjustments in the recommended methods for the examination and clarifications of how to determine classification that have necessitated another major revision in the Standards.
As such the 2011 ISNCSCI has been published.10,11 These changes were substantial enough that it was determined that the 2003 reference manual was not up-to-date and should no longer be distributed. In order to give specialists the ability to understand the changes in the International Standards, this article provides additional detail regarding the clarifications and revisions, with explanations as to why these changes were made. Some of the clarifications to the ISNCSCI have been detailed in a 2010 published review of the Standards.12 Changes that have been made are consistent with the InSTeP training program.
ASIA has adopted a process to review and if needed, to revise the ISNCSCI every 3 years. The review and revision of the ISNCSCI was performed by ASIA's International Standards Committee with input from the Education Committees of ASIA and ISCoS and approved by ASIA's Board of Directors.
Clarifications
The clarifications of the seventh edition of the ISNCSCI booklet include the following:
1. Describing in greater detail the motor and sensory examination, including positions for motor testing to grade a muscle function as 4 or 5.
Details on execution of the examination are available as part of the InSTeP program.8 These clarifications were consensus driven with the goals of increasing reproducibility and of reinforcing specific manual muscle techniques, utilizing static positioning with the patient resisting the examiner's force.13 Table 1 lists the specific positions for testing key muscles for grades 4 and 5. Standardization in performing muscle testing will allow for consistency in grading among examiners.
Table 1.
Positions for testing key muscles for grades 4 or 5
| C5 | Elbow flexed at 90°, arm at patient's side and forearm supinated |
| C6 | Wrist in full extension |
| C7 | Shoulder is in neutral rotation, adducted, and in 90° of flexion with elbow in 45° of flexion |
| C8 | Full-flexed position of the distal phalanx with the proximal finger joints stabilized in extended position |
| T1 | Full-abducted position of fifth digit (of the hand) |
| L2 | Hip flexed to 90° |
| L3 | Knee flexed to 15° |
| L4 | Full-dorsiflexed position of ankle |
| L5 | First toe fully extended |
| S1 | Hip in neutral rotation, the knee is fully extended, and the ankle in full plantar flexion |
2. Defining the motor level in a patient with no correlating key motor function to test (i.e. above C5, between T2–L1, and S2–5).
Anecdotally, this is a difficult concept to teach, which was supported by a low percentage of ‘correct’ answers during the development of InSTeP, as well as subsequent psychometric analysis of the imbedded test questions concerning motor levels with no motor function. In cases where key muscle functions are not clinically testable by a manual muscle examination, the motor level is presumed to be the same as the sensory level, if testable motor function above (rostral) that level is intact (normal) as well.
Some examples are provided to illustrate this point.
Example 1: If the sensory level is C4, and there is no C5 motor strength (or the strength is graded <3), the motor level is C4.
Example 2: If the sensory level is C4, with the C5 key muscle function strength graded as ≥3, the motor level would be C5. This is because the strength at C5 is ≥3 with the ‘muscle function’ above considered normal. Presumably, if there were a C4 key muscle function it would be graded as normal since the sensation at C4 is intact.
Example 3: If the sensory level is C3, with the C5 key muscle function strength graded as ≥3, the motor level is C3. This is because the motor level presumably at C4 is not considered normal (since the C4 dermatome is not normal), and the rule of all levels rostral needing to be intact is not met.
Example 4: If all upper-limb key muscle functions are intact, with intact sensation through T6, the sensory level as well as the motor level is recorded as T6.
Example 5: In a case similar to Example 4, but the T1 muscle function is graded 3 instead of 5, while T6 is still the sensory level, the motor level is T1, as all the muscles above the T6 level cannot be considered normal. It is important to recognize that the motor level follows the sensory level only if the rule of ‘all the key muscle functions above are graded as normal’ applies.
Similar rules apply in the lower extremity, where L2 is the first lower extremity key muscle function that is tested. L2 can only be considered the motor level if sensation at L1 and more rostral is intact.
Example 6: If the sensory level is T12, the hip flexor motor function (L2 key muscle) is graded as 3 bilaterally and muscle strength of upper extremity key muscle groups are graded 5/5, the motor level is T12. While L2 motor function is graded as a 3, the motor function above that level (L1) is not normal (because the sensory level is not normal) and thereby the sensory and motor level is T12.
Example 7: If the sensory level is L2 and the hip flexor muscle function is graded as 2 with all upper extremity key motor function graded as 5: the sensory level is L2, and the motor level is L1. While the rule of the motor level deferring to sensory level is utilized when there is no functional motor level to test (i.e. above the L2 level), once there is a key motor functional level to test (in this case at L2), the motor level no longer defers to the sensory level.
3. Documenting the zone of partial preservation (ZPP) in a situation where there is no sparing of motor or sensory function below the motor and sensory levels. The relevant (right and left) motor and sensory levels are documented in the designated area on the worksheet.
Previously, it was not clear as to what should be documented in the box on the worksheet when the motor and/or sensory level was the same as the neurologic level of injury (NLI) without any sparing. For example, a patient with a T6 NLI with a neurological complete injury (AIS A) and no sparing of motor or sensory function below T6, has been categorized by some clinicians by placing a ‘dash mark’ in the box for ZPP on the worksheet, while others may place ‘NA’ (not applicable). The clarification is that for this type of example, if there is no sparing below the NLI, then the motor and sensory levels should be documented (in this case T6) in the box for ZPP.
One should note that motor function does NOT follow sensory function in recording ZPP. Rather, the caudal extent of the motor ZPP must be based on the presence of voluntary muscle contraction below the motor level. While the motor level defers to the sensory level in the regions where there is no key motor function to test (C1–C4, T2–L1, etc.), motor ZPP does not defer to the sensory ZPP. Specifically, if the NLI is T6 in a case with a neurologically complete injury (AIS A), with impaired sparing of light touch sensation at T7 bilaterally and all other sensations absent, one should document T7 for sensation in the ZPP boxes on the worksheet bilaterally and the motor level of T6 should be placed in the ZPP box bilaterally. Lastly, non-key muscles are not included in the ZPP.
In cases of an incomplete injury, the ZPP is not applicable and therefore ‘NA’ is recorded in the box on the worksheet.
4. Distinguishing between a sensory incomplete versus a motor incomplete (AIS B from C) injury, as well as between motor incomplete injuries (AIS C from D). Specifically, one should use the motor level on each side to differentiate AIS B from C injuries, and the single neurological level for AIS C from D injuries when applying the classification definitions.
This concept was previously documented, but was still found to cause some confusion. The following cases will help illustrate this aspect of the classification (Tables 2 and 3).
Table 2.
Case example to differentiate AIS B versus AIS C
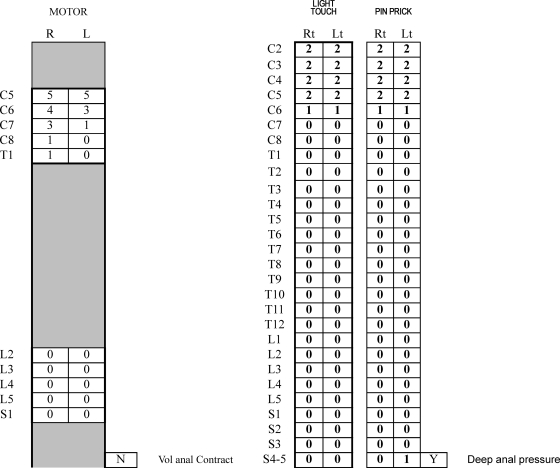 |
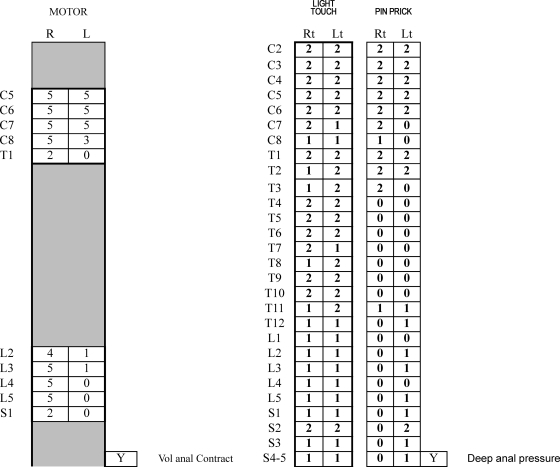
Table 3.
Case example to differentiate AIS C versus AIS D
 |
The example listed in Table 2 reveals a sensory level bilaterally of C5, with a motor level of C6 bilaterally. The single NLI is C5 and the patient has sensory sacral sparing, allowing classification as an ‘incomplete injury’. The case can meet the criteria for a ‘motor incomplete’ injury, despite no voluntary anal contraction (VAC), if there is motor sparing more than three levels below the motor level on either side of the body. As the motor level bilaterally is C6, there would need to be motor sparing below T1 (more than three levels below the motor level). The case does not show this, and as such represents an AIS B classification. If, however, one incorrectly used the NLI (C5 in this case) as the starting point, as there is sparing more than three levels below this NLI, the classification would be AIS C. This is not the proper classification. If this were an acute injury, and the person were to recover (improvement of) normal sensory function at the C6 level, then this patient would ultimately be reclassified as an AIS B; showing worsening classification status despite actually having a small degree of neurological improvement.
Table 3 lists another example to illustrate this concept. The sensory level on the right – C7; left – C6; and motor level is right – C8; and left C8. The single NLI is C6 and this represents a motor incomplete injury because of the presence of VAC. By using the single NLI of C6, there are 16 key muscle functions testable for AIS C versus D determination, and 8 are graded as ≥3; therefore this case is classified as AIS D. If one were to mistakenly use the motor level in this case of C8 (rather than the single NLI), then only 4 of 12 muscle functions would grade ≥3, and would therefore be incorrectly classified as an AIS C.
5. Utilizing non-key muscle functions in the AIS classification.
This concept was included in the 2003 reference manual,7 and has been controversial.12 The committee decided that while these muscle functions are not used in determining motor levels or scores (i.e. motor index scoring), non-key muscles (if tested) may be used to determine sensory versus motor incomplete status (AIS B versus C) (see Table 4 for illustration). The reason for this is that the presence of motor function cannot be ignored and may be a sign of further potential recovery in a person with a sensory incomplete injury. This would be extremely important in inclusion/exclusion criteria for research studies or as an outcome measure in a trial designed to restore strength in persons with motor complete injuries.
Table 4.
Utilizing non-key muscles for AIS scoring
 |
There is a need for more input, data, and discussion before this concept can be taught in a standardized manner. In addition, specific levels will need to be determined for each muscle so that there will be consistency among examiners in documenting that the motor function spared is more than three levels below the motor level.
Revisions
The revisions of the standards include the following:
1. Replacing the term deep anal sensation with the term deep anal pressure (DAP).
Prior to the development of InSTeP, there were no instructions provided on the technique to be used for this part of the examination. Consensus determined that the term ‘pressure’ would reinforce the technique of applying gentle pressure to the anorectal wall (innervated by the somatosensory components of the pudendal nerve – S4/S5) or with the examiner's distal thumb and index finger,14 as opposed to other more vigorous techniques that may potentially relay information by other neurological pathways (i.e. autonomic).
2. Determining that if sensation is abnormal at C2, the level that should be designated is C1.
Previous versions of the International Standards did not include directions on the classification if C2 is abnormal. While further study is required, it was felt that this would allow for consistency amongst clinicians and researchers.
3. Clarifying that in patients who have light touch or pin prick sensation at S4–S5, examination for DAP is not required.
While testing for DAP is still recommended to complete the worksheet, its performance in this scenario would not change the classification as the patient already has a designation for a sensory incomplete injury. In this situation a digital rectal examination is still required, however, to test for motor sparing (i.e. voluntary anal sphincter contraction).
4. Defining that the ZPP in patients with a neurologically complete injury (AIS A) has been revised to be consistent with InSTeP.
Specifically, the method used to determine the levels of the ZPP has been changed to include the ‘dermatomes and myotomes caudal to the sensory and motor levels on each side of the body that remain partially innervated’ in a neurologically complete injury. In the previous edition of the ISNCSCI,3 the ZPP was determined from the NLI. This distinction is important when discussing the levels of sparing for the ZPP. For instance, in a patient who has a C5 sensory level, with a C6 motor level with slight motor sparing at C7, the NLI is C5 with a ZPP for motor of C7. If one uses the motor level as the ZPP definition, this person would have one motor level of sparing. If using the NLI as the definition, then C7 represents two levels of sparing. It was felt that the updated classification more accurately describes the sparing for a person with a complete injury.
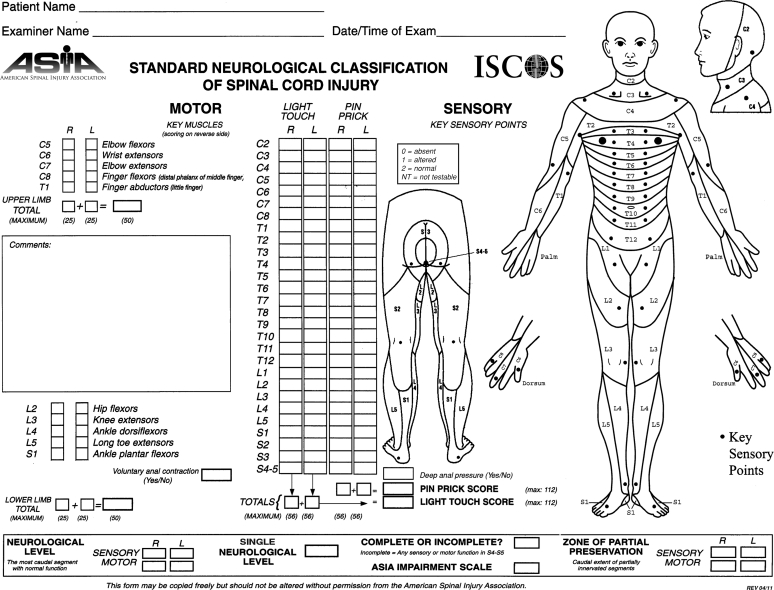
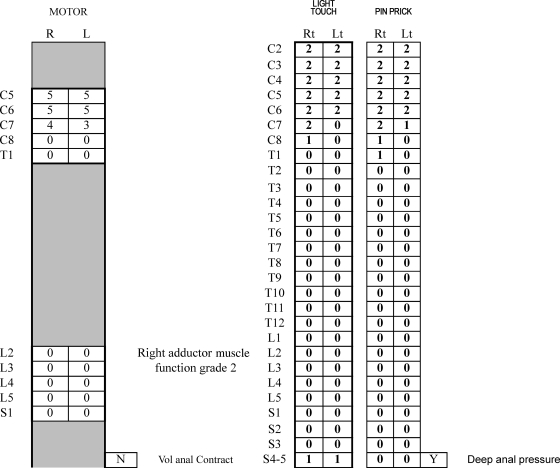
5. Updating some of the figures and adjusting the worksheet or ease of use.
The graph for the muscle innervations (Fig. 1) and the worksheet (Fig. 2) were updated. Updates on the worksheet include changing ‘Deep Anal Sensation’ to ‘Deep Anal Pressure’, the addition of a box to enter the ‘Single Neurological Level’ and a description for the ZPP.
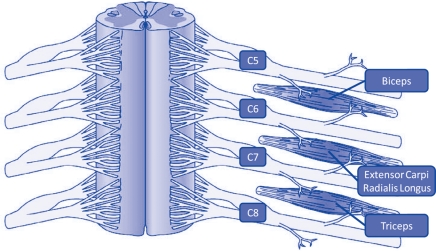
Figure 1.
Schematic depiction of innervation of each of three key muscles by two nerve segments.
Figure 2.
The ISNCSCI worksheet remains available on the ASIA website (http://www.asia-spinalinjury.org/publications/59544_sc_Exam_Sheet_r4.pdf) and can be used/downloaded without permission or cost.
Conclusion
This article serves as a readily available reference for clinicians and researchers to accompany the 2011 ISNCSCI.10,11 The electronic modules of InSTeP are intended to provide details on the execution of the examination and classification techniques.8 The Committee recognizes that there will always be some cases of SCI that do not seem to ‘fit’ the ISNCSCI. However, the International Standards classify the vast majority of cases adequately. The International Standards Committee welcomes correspondence that raises questions, offers constructive criticism, or provides new empirical data that are relevant for further refinements and improvements in the reliability and validity of the International Standards.
References
- 1.American Spinal Injury Association Standards for neurological classification of spinal injured patients. Chicago, IL: ASIA; 1982 [Google Scholar]
- 2.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries in the spine with paraplegia and tetraplegia. Paraplegia 1969;7:179–92 [DOI] [PubMed] [Google Scholar]
- 3.American Spinal Injury Association International standards for neurological classification of spinal cord injury. Atlanta, GA; revised 2000; Reprinted 2008 [Google Scholar]
- 4.American Spinal Injury Association/International Medical Society of Paraplegia (ASIA/IMSOP) International Standards for Neurological and Functional Classification of Spinal Cord Injury patients (Revised). Chicago, IL: American Spinal Injury Association; 1996 [Google Scholar]
- 5.American Spinal Injury Association/International Medical Society of Paraplegia International Standards for Neurological and Functional Classification of Spinal Cord Injury patients. American Spinal Injury Association. Chicago, IL; 2000 [Google Scholar]
- 6.Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003;26suppl. 1:S50–6 [DOI] [PubMed] [Google Scholar]
- 7.American Spinal Injury Association Reference manual for the International Standards for Neurological Classification of Spinal Cord Injury. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 8.American Spinal Injury Association ASIA Learning Center. [accessed 2011 Oct 5]. Available from www.asialearningcenter.com
- 9.American Spinal Injury Association International Standards for Neurological and Functional Classification of Spinal Cord Injury patients. American Spinal Injury Association. Chicago, IL; 1987 [Google Scholar]
- 10.International Standards for Neurological Classification of Spinal Cord Injury 2011 Revision J Spinal Cord Med 2011;34(6):535–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.International Standards for the Neurological Classification of Spinal Cord Injury Revised 2011. (Booklet) Atlanta, GA: American Spinal Injury Association [Google Scholar]
- 12.Waring WP, III, Biering-Sorensen F, Burns S, Donovan W, Graves D, Jha A, et al. 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med 2010;33(4):346–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daniels L, Worthingham C. Muscle testing: techniques of manual examination. 3rd ed Philadelphia, PA, Saunders; 1972 [Google Scholar]
- 14.Vogel LC, Samdani A, Chafetz R, Gaughan J, Betz R, Mulcahey MJ. Intra-rater agreement of the anorectal exam and classification of injury severity in children with spinal cord injury. Spinal Cord 2009;47(9):687–91 [DOI] [PubMed] [Google Scholar]