Abstract
Aspergillus is damaged by polymorphonuclear neutrophils (PMNs) by means of nonoxidative and oxidative mechanisms, which may be affected by antifungal and antibacterial agents that patients with invasive pulmonary aspergillosis often receive. The pharmacodynamic interactions among deoxycholate amphotericin B (AMB), ciprofloxacin (CIP), and human PMNs against Aspergillus fumigatus growth are unknown. We therefore studied the interactions between 0.032 to 2.0 μg/ml of AMB, 0.1 to 50 μg/ml of CIP at a fixed AMB/CIP ratio of 1:3.125, and PMNs from six donors at an effector-to-target (E:T) ratio of 400:1 against a clinical A. fumigatus isolate using an XTT metabolic assay and the Bliss independence pharmacodynamic-interaction model. CIP exhibited no antifungal activity alone or in combination with PMNs. Synergy was found between AMB and PMNs, with interaction indices (II) of 0.06 to 0.21; the highest interaction of 21% ± 3.6% was observed at 0.22 ± 0.09 μg/ml of AMB. The AMB and CIP (AMB+CIP) combination was synergistic (II = 0.39) at low AMB concentrations and antagonistic (II = 1.39) at high AMB concentrations, with a maximal synergistic interaction of 16% ± 3.7% observed at 0.16 ± 0.08 μg/ml of AMB. The triple combination AMB+CIP+PMNs was synergistic, with interaction indices of 0.05 to 0.20, and a maximal synergistic interaction of 24% ± 4% was observed at 0.20 ± 0.07 μg/ml of AMB. The increased percentage of Bliss synergy of the triple combination AMB+CIP+PMNs (24% ± 4%) was the product of those of the constituent double combinations AMB+PMNs (21% ± 3.6%) and AMB+CIP (16% ± 3.7%). Thus, the antifungal activity of AMB, at clinically relevant concentrations, was enhanced in combination with PMNs and CIP against A. fumigatus growth in a concentration-dependent manner.
INTRODUCTION
Aspergillus spp. are common pathogens causing life-threatening, invasive fungal disease in immunocompromised patients (21, 26). Patients at risk for invasive aspergillosis are also at risk for the development of bacterial infections, for which fluoroquinolones may be used for prophylactic and therapeutic purposes concomitantly with antifungal agents, such as amphotericin B (AMB) (1, 13). Although fluoroquinolones have no intrinsic antifungal activity, high levels of topoisomerases, the targets of fluoroquinolones, have been reported in pathogenic fungi (18). Ciprofloxacin (CIP), a fluoroquinolone, was previously found to interact pharmacodynamically with antifungal agents by altering their growth-inhibitory activities against Candida albicans and Aspergillus fumigatus (22).
Polymorphonuclear neutrophils (PMNs) are important components of the innate host defense against invasive aspergillosis (4). Oxidative pathways are among the main antifungal mechanisms of PMNs that are involved in hyphal damage (17). During the oxidative burst, activation of NADP (NADPH) oxidase results in the production of a superoxide anion (O2−), a reactive oxygen intermediate that is released. Both amphotericin B and ciprofloxacin exert immunomodulating activity on human immunocompetent cells, affecting humoral and cellular immunity (5, 6, 20).
In this study, we investigated the interactions between human PMNs, ciprofloxacin, and deoxycholate AMB. Each of the agents listed has distinct mechanisms of action. The Bliss independence no-interaction theory is based on the probability law of independent events and can be used to analyze pharmacodynamic interactions among such agents that have independent actions (12). We therefore analyzed the pharmacodynamic interactions among AMB, ciprofloxacin, and PMNs against A. fumigatus with the Bliss independence no-interaction theory.
MATERIALS AND METHODS
Isolates and medium.
The A. fumigatus 4215 (ATCC MYA-3626) strain was used in this study. The strain was stored on potato dextrose agar slants at −70°C. Aspergillus conidia were collected with a wet swab from 5- to 7-day-old cultures in Sabouraud dextrose agar. Conidial suspensions were adjusted spectrophotometrically at 530 nm to 80 to 82% transmittance and diluted in order to obtain two times the final inoculum, which ranged from 0.4 × 104 to 5 × 104 CFU/ml (this range was chosen based on CLSI guidelines) in the medium, which consisted of RPMI 1640 medium buffered at pH 7 with 0.165 M MOPS (morpholinepropanesulfonic acid) (BioWhittaker, Walkersville, MD). Candida parapsilosis (ATCC 22019), Candida krusei (ATCC 6258), A. fumigatus (ATCC MYA-3626), and Escherichia coli (ATCC 259222) were used as quality controls.
Antimicrobial compounds and combination microtitration plates.
Ciprofloxacin (Bayer AG, Leverkusen, Germany) and AMB (Ben Venue Laboratories, Inc., Bedford, OH) stock solutions were prepared according to the manufacturers' guidelines and diluted in the assay medium in order to obtain working solutions of 200 μg/ml and 8 μg/ml, respectively. Amphotericin B and ciprofloxacin were serially diluted 2-fold in the medium in order to obtain four times the final concentrations, which ranged from 0.032 to 2.0 μg/ml and from 0.1 to 50 μg/ml, respectively. The combination of AMB with ciprofloxacin at a fixed ratio of 1:3.125 was prepared by 2-fold serial dilutions of a combination of 2 μg/ml AMB and 6.25 μg/ml CIP. This fixed ratio is usually observed in vivo because the maximum concentration in serum (Cmax) of ciprofloxacin after a dosage of 400 mg every 12 h (q12h) intravenously (i.v.) is approximately three times higher than the Cmax of AMB after a dosage of 1 mg/kg of body weight (2, 25). All experiments were performed in 96-well flat-bottom microtitration plates (Corning Inc., Corning, NY). The plates were stored at −70°C and thawed on the day of experiment.
Preparation of PMNs.
Elutriated human PMNs from six healthy adult volunteers were obtained from the Department of Transfusion Medicine, National Institutes of Health, Bethesda, MD. They were further processed with 5% dextran solution (Pharmacis Fine Chemicals, Piscataway, NJ) for sedimentation of excess erythrocytes. Contaminating erythrocytes were lysed by suspension of the neutrophilic pellet in distilled water for 15 to 20 s, followed by the addition of hypertonic saline to correct the tonicity of the solution. PMNs were finally suspended in Hanks' balanced salt solution without Ca2+ and Mg2+. The viability of the PMNs was tested by the trypan blue exclusion method. PMNs were added into the wells at an effector-to-target (E:T) ratio of 400:1 before the inoculation. Different E:T ratios were tested, ranging from 1:1 to 800:1, in order to choose the E:T ratio that resulted in approximately 50% of fungal growth, which would allow us to detect both synergy and antagonism. E:T ratios resulting in very small and very large percentages of growth would not be able to detect antagonistic and synergistic interactions, respectively.
XTT colorimetric assay.
After incubation of microtitration plates containing the agents alone and in double and triple combinations for each donor at 37°C for 24 h, the growth in each well was determined with the XTT assay by measuring the fungal-biomass-associated metabolic activity (10). One hundred microliters of XTT-menadione solution was added to each well in order to obtain final concentrations of 100 μg/ml XTT-25 μM menadione. XTT conversion by viable hyphae was measured at 450 nm. The percentage of fungal growth was calculated for each concentration with the equation (A450 of a well − background A450)/(A450 of the drug-free well − background A450 of the drug-free well) × 100%, where the background A450 was measured from a plate inoculated with a conidium-free inoculum.
Pharmacodynamic interaction analysis.
The interactions within the double and triple combinations of AMB (0.03 to 2 μg/ml), ciprofloxacin (at a 1:3.125 fixed ratio with AMB), and PMNs (at an E:T ratio of 400:1) were analyzed with the Bliss independence zero-interaction theory. Based on this pharmacodynamic theory, if three agents, A, B, and C, do not interact, they act independently and the effects of their joint actions should follow the probability law of independent events (15). This effect derives from the equation IIND = ΣI − ΠI, where IIND is the growth inhibition of a Bliss independence combination and ΣI and ΠI are the summation and the product, respectively, of growth inhibitions (Is) of each constituent agent alone and in combination [i.e., IIND = (IA + IB + IC) − (IA × IB) − (IA × IC) − (IB × IC) − (IA × IB × IC)]. The latter equation can be simplified by replacing I with 1 − E, where E is the percentage of fungal growth. Thus, the Bliss independence effect can be calculated by the equation EIND = EAMB × ECIP × EPMN, where EAMB, ECIP, and EPMN are the percentages of growth with AMB, ciprofloxacin, and PMNs alone, respectively, and EIND is the theoretical percentage of growth if the constituting agents of the combinations acted independently.
For each double and triple combination, the theoretical Bliss independence concentration-effect data were calculated using the above-mentioned equation and analyzed with nonlinear-regression analysis based on the sigmoid curve with variable slope described by the equation E = B + (Emax − B)/[1 + 10(logEC50 − logC) × m], where E is the percentage of growth (dependent variable) at the drug concentration C (independent variable), Emax is the maximum percentage of growth observed in the drug-free control (i.e., 100%), B is the minimum percentage of growth at an infinite drug concentration (i.e., 0%), EC50 is the effective drug concentration producing 50% of the Emax, and m is the slope of the concentration-effect curves (Hill coefficient) (Prism 5.0; GraphPad Inc.).
Pharmacodynamic interactions were determined at three different effective levels, the EC10, EC50, and EC90, which are drug concentrations corresponding to 10, 50, and 90% of growth, respectively. These three ECs describe interactions at high, medium, and low drug concentrations, relative to the MIC (the EC10 is close to the MIC, and the EC90 is much lower than the MIC). The EC50 was derived directly from the sigmoid equation, whereas the EC10 and EC90 were estimated based on the EC50 solving the sigmoid equation for log C and by using 10% and 90%, respectively, as E. The experimentally observed effective concentrations (ECOBS) were compared with the theoretical Bliss independence effective concentrations (ECIND) for each combination. The interaction indices of EC10,OBS/EC10,IND, EC50,OBS/EC50,IND, and EC90,OBS/EC90,IND were then calculated, and synergy or antagonism was concluded when these indices were significantly lower or higher than 1, respectively, based on their 95% confidence interval; if this interval included 1, Bliss independence was concluded.
Finally, the magnitudes and AMB concentrations of Bliss interactions within the double and triple combinations were compared. The percentage of Bliss interactions at each AMB concentration was calculated by subtracting the experimental percentage of growth from the theoretical percentage of growth and analyzed with nonlinear-regression analysis using the bell-shaped curve described by the equation E = Emax × e{−0.5×[(logC−logCmax)/SD]2}, where E is the percentage of the Bliss interaction, Emax is the maximal percentage of the Bliss interaction, C is the concentration of AMB, Cmax is the AMB concentration of Emax, and the standard deviation (SD) is a measure of the widths of Bliss interactions (Prism 5.0; GraphPad Inc.). The Emaxs, Cmaxs, and SDs of the double and the triple combinations were then compared using a one-way analysis of variance (ANOVA).
RESULTS
Effects of single compounds.
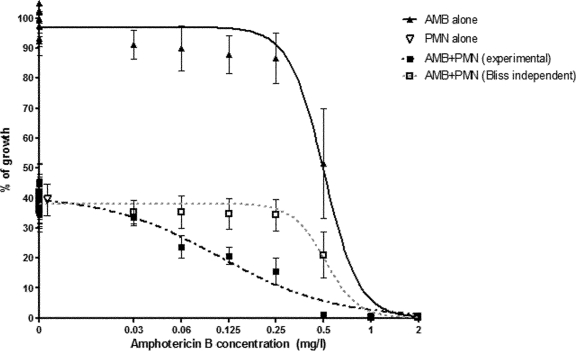
The MIC of AMB was 0.5 μg/ml against A. fumigatus, with its antifungal activity following a sigmoidal concentration-effect curve (EC50 = 0.51 μg/ml, m = −4.2, R2 = 0.85), as shown in Fig. 1. PMNs alone resulted in fungal growth of 39% ± 6% at the E:T ratio of 400:1, whereas CIP alone resulted in fungal growth of 97% ± 5% for the entire range of CIP concentrations.
Fig. 1.
Double combination of amphotericin B (AMB) and polymorphonuclear cells (PMNs). Concentration-effect data and regression curves for AMB alone, PMNs alone, the double combination AMB+PMNs at an E:T ratio of 400:1, and the Bliss independence theoretical combination AMB+PMNs if AMB and PMNs act independently. Error bars represent standard errors among 2 replicates and 6 donors. Bliss synergy was found between AMB and PMNs, as the experimental curve (dashed black line) is shifted to the left of the theoretical (dashed gray line) concentration-effect curve of AMB+PMNs (i.e., a lower percentage of growth was obtained when AMB was combined with PMNs than was obtained by the theoretical combinations). The open triangle next to the y axis corresponds to 0 μg/ml of AMB, but it was shifted to the right for visualization purposes.
Effect of the combination AMB+PMNs.
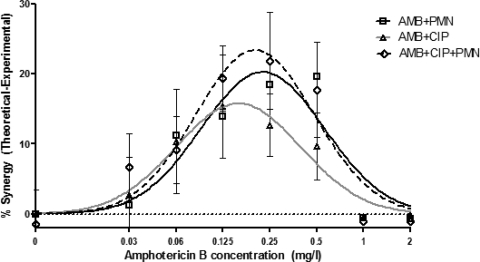
The double combination of AMB and PMNs (AMB+PMNs) for all donors followed a sigmoidal concentration-effect relationship (EC50 = 0.38 μg/ml, m = −1.9, R2 = 0.80) that, however, shifted to the left, signifying Bliss synergy, and was shallower than the concentration-effect relationship of AMB alone. The combination AMB+PMNs was Bliss synergistic, with interaction indices of 0.06 at the EC90 and 0.21 at the EC50 (Table 1) . At the EC10 (the drug concentration close to the MIC), the interaction index was lower than 1 but not by a statistically significant amount. The Bliss synergistic interactions followed a bell-shaped curve (SD = 0.40) spanning from log Cmax minus the SD to log Cmax plus the SD (i.e., 0.09 to 0.56 μg/ml of AMB, with the maximal synergistic interaction of an Emax of 21% ± 3.6% being observed at an AMB Cmax of 0.22 ± 0.09 μg/ml) (Fig. 2).
Table 1.
Bliss independence interaction analysis of double and triple combinations of AMB, CIP, and PMNsa
| Combination | Endpoint | Exptl ECOBS (μg/ml) (95% CI) | Theoretical ECIND (μg/ml) (95% CI) | Interaction index | Interpretation |
|---|---|---|---|---|---|
| AMB+CIP | EC90 | 0.11 (0.09–0.14) | 0.29 (0.25–0.32) | 0.39b | Synergy |
| EC50 | 0.37 (0.3–0.44) | 0.5 (0.45–0.57) | 0.74 | Synergy | |
| EC10 | 1.23 (1.01–1.51) | 0.88 (0.78–1.01) | 1.39b | Antagonism | |
| AMB+PMN | EC90 | 0.02 (0.01–0.03) | 0.31 (0.24–0.39) | 0.06b | Synergy |
| EC50 | 0.11 (0.06–0.19) | 0.51 (0.41–0.65) | 0.21b | Synergy | |
| EC10 | 0.68 (0.38–1.2) | 0.87 (0.69–1.09) | 0.78 | Independence | |
| AMB+CIP+PMN | EC90 | 0.01 (0.01–0.03) | 0.29 (0.22–0.36) | 0.05b | Synergy |
| EC50 | 0.1 (0.06–0.18) | 0.5 (0.39–0.64) | 0.20b | Synergy | |
| EC10 | 0.71 (0.41–1.22) | 0.89 (0.7–1.14) | 0.80 | Independence |
The double combinations AMB+CIP and AMB+PMN and the triple combination AMB+CIP+PMN were analyzed by Bliss independence interaction analysis. The double combination of CIP+PMN was not analyzed because no effect was observed at any concentration of CIP. CI, confidence interval.
Significantly smaller than 1 (P < 0.05).
Fig. 2.
Bliss synergistic interactions between amphotericin B (AMB), ciprofloxacin (CIP), and PMNs followed a bell-shaped curve, with the maximal synergistic interactions of 21% ± 3.6%, 16% ± 3.7%, and 24% ± 3.9% being observed at 0.22 ± 0.09, 0.16 ± 0.08, and 0.20 ± 0.07 μg/ml of AMB for the combinations AMB+PMNs, AMB+CIP, and AMB+CIP+PMNs, respectively. Bliss interaction curves were obtained by subtracting the theoretical data from the experimental data for the six donors.
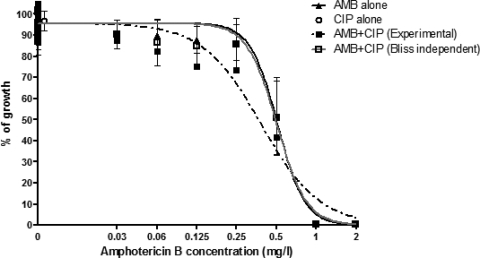
Effect of the AMB+CIP combination.
The concentration-effect relationship of the double combination AMB+CIP is shown in Fig. 3. CIP did not have significant antifungal activity, since its concentration-effect curve was a line parallel to the x axis, as shown in Fig. 4. The concentration-effect relationship of the AMB+CIP combination was shifted to the left at low AMB concentrations, indicating Bliss synergy (interaction index of 0.39), and to the right of the concentration-effect relationship of AMB alone at higher AMB concentrations, indicating Bliss antagonism (interaction index of 1.39) (Table 1); however, this effect was significantly different from Bliss independence. The Bliss synergistic interactions also followed a bell-shaped relationship spanning from 0.06 to 0.39 μg/ml of AMB (SD = 0.4), with a maximal synergistic interaction at an Emax of 16% ± 3.7% observed at a Cmax of 0.16 ± 0.08 μg/ml of AMB (Fig. 2).
Fig. 3.
Double combination of amphotericin B (AMB) and ciprofloxacin (CIP). Concentration-effect data and regression curves for AMB alone, CIP alone, the double combination AMB+CIP at a fixed ratio of 1:3.125, and the AMB+CIP Bliss independence theoretical combination if AMB and CIP act independently. Error bars represent standard errors among 6 replicates. Bliss synergy was found at low concentrations of AMB, as the experimental curve (dashed black line) is to the left of the theoretical concentration-effect curve (gray line) of AMB+CIP (i.e., a lower percentage of growth was obtained when AMB was combined with CIP than was obtained by the theoretical combinations). At higher AMB concentrations, the experimental curve is to the right of the theoretical concentration-effect curve of the AMB+CIP combination, resulting in Bliss antagonism. The open circle next to the y axis corresponds to 0 μg/ml of AMB, but it was shifted to the right for visualization purposes.
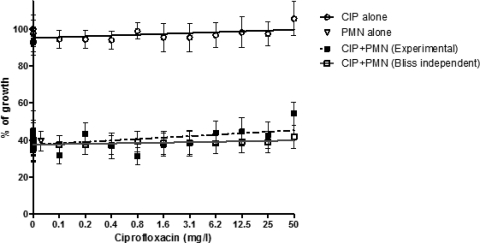
Fig. 4.
Double combination of ciprofloxacin (CIP) and polymorphonuclear cells (PMNs). Concentration-effect data and regression lines of CIP alone, PMNs alone, the double combination CIP+PMNs, and the Bliss independence theoretical combination CIP+PMNs if CIP and PMNs act independently. Ciprofloxacin did not exhibit a direct effect on Aspergillus growth and did not significantly alter the antifungal activity of PMNs. The open triangle next to the y axis corresponds to 0 μg/ml of ciprofloxacin, but it was shifted to the right for visualization purposes.
Effect of the combination CIP+PMNs.
The concentration-effect relationship of the double combination CIP+PMNs is shown in Fig. 4. Ciprofloxacin did not have any direct antifungal activity and did not alter the antifungal activity of PMNs.
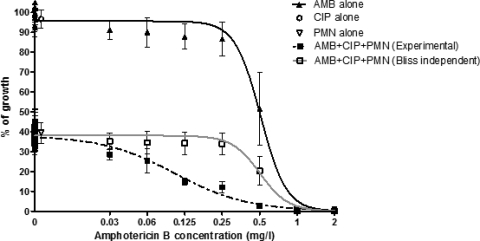
Effect of the triple combination AMB+CIP+PMNs.
The antifungal activity of the triple combination AMB+CIP+PMNs was described by a sigmoidal concentration-effect relationship (EC50 = 0.10 μg/ml, m = −1.5, R2 = 0.64) that was shifted to the left, signifying Bliss synergy, and was shallower than the theoretical Bliss independence concentration-effect curve (Fig. 5). Bliss synergy was observed with interaction indices of 0.05 at the EC90 and 0.20 at the EC50 (Table 1), whereas Bliss independence was found at higher AMB concentrations corresponding to the EC10. Bliss synergistic interactions followed a bell-shaped relationship (Fig. 2) spanning from 0.08 to 0.48 μg/ml of AMB (SD = 0.38), with the maximal synergistic interaction of 24% ± 4% observed at 0.20 ± 0.07 μg/ml of AMB. There are no significant differences among the maximal percentages of the Bliss synergistic interactions of the triple combination AMB+CIP+PMNs (24%) and the double combinations AMB+PMNs (21%) and AMB+CIP (16%) (ANOVA P value of >0.05).
Fig. 5.
Triple combination AMB+CIP+PMNs. Concentration-effect data and regression curves for AMB alone and the effects of CIP and PMNs alone, the triple combination AMB+CIP+PMNs, and the theoretical Bliss independence combination AMB+CIP+PMNs if all constituent agents act independently from each other. Error bars represent standard errors among 2 replicates and 6 donors.
DISCUSSION
In this study, we demonstrated that conventional AMB synergistically interacts with PMNs and CIP against A. fumigatus growth in a concentration-dependent manner, with maximal synergies of 21% and 16%, respectively, observed at sub-MIC AMB concentrations. Ciprofloxacin did not have any effect alone or in combination with PMNs against A. fumigatus growth. The triple combination AMB+CIP+PMNs was also synergistic, with a maximal synergistic interaction of 24%, which is higher than those of the single constituent agents.
Bliss independence theory has been previously used to adequately describe in vitro pharmacodynamic interactions between antifungal agents, the results of which correlated with in vivo results from experimental invasive pulmonary aspergillosis (11, 14). Because Bliss independence theory is based on independent events like the distinct modes of action of the three agents investigated in the present study (12), we report its first application, to our knowledge, to describe the interaction between a systemic antifungal agent, a fluoroquinolone with no direct antifungal activity, and a nonchemotherapeutic agent like phagocytic cells. Other advantages of Bliss independence theory are the facts that it does not require full descriptions of concentration-effect relationships and that it can be applied even when the maximal and minimal responses are not the same among the combined agents (12), e.g., the maximal-minimal effects were 40 to 0%, 100 to 0%, and 100 to 0% of growth with PMNs, AMB, and CIP, respectively.
Previous studies have reported that conventional AMB enhances PMN antifungal function at a concentration of 1 or 5 μg/ml conventional AMB (6). In the present study, we investigated more comprehensively than in those studies the interactions between conventional AMB and PMNs against A. fumigatus growth by using a broader range of AMB concentrations achievable in plasma and a pharmacodynamic theory for the detection of synergy. Unlike in previous studies (6, 7), the present experiments were conducted with the addition of agent to the conidia prior to the formation of germlings, which increased the exposure time and, consequently, the effect.
There are several potential mechanisms for the enhanced antifungal activities of AMB in combination with PMNs. AMB may damage maturing Aspergillus conidia and hyphae and render them vulnerable targets for PMNs. Furthermore, it has been previously shown that signaling through Toll-like receptor 2 (TLR2) promotes the fungicidal activity of PMNs through nonoxidative pathways involving the extracellular release of gelatinases and proinflammatory cytokines, while TLR4 favors the oxidative pathways through the participation of azurophil, myeloperoxidase-positive granules, and interleukin 10 (IL-10) (3). AMB (16, 19) and ciprofloxacin (5) are well-recognized immunomodulators affecting the production of O2−, tumor necrosis factor alpha (TNF-α), and proinflammatory and anti-inflammatory cytokines from innate host defense cells. Thus, AMB may enhance the fungicidal activity of PMNs through several mechanisms.
AMB was found to interact synergistically at low concentrations of CIP and antagonistically at high concentrations of CIP. This is in agreement with previous studies where the double combination AMB+CIP was synergistic at CIP concentrations of <10.6 μg/ml and antagonistic at CIP concentrations approaching 50 μg/ml against Candida albicans and A. fumigatus using isobolographic analysis (23). This similarity of findings suggests that the findings of the Bliss model in the current study are not due to methodological bias but that they are probably related to certain biological factors that are unclear at present. Ciprofloxacin molecules are zwitterionic and are present as monomers at low concentrations, whereas at higher concentrations, they are self-associated in a head-to-tail arrangement (9). Given that ciprofloxacin molecules interact with cholesterol-containing liposomes (9), ciprofloxacin at low concentrations may participate in pore formation on fungal cell membranes imposed by amphotericin B and may thereby enhance its antifungal action. However, the self-association of ciprofloxacin molecules at high concentrations may interfere with amphotericin B pore formation, thereby decreasing its antifungal activity and thus producing an antagonistic effect, as found in the present study. This antagonistic effect is unlikely to have clinical application, as serum ciprofloxacin concentrations of 50 μg/ml are not safely achieved with standard dosing regimens. The study of variable concentration-dependent interactions of drug combinations allows us to draw possible conclusions regarding their pharmacodynamic effects in clinical practice. These results may be clinically significant, because the drug concentrations after the initial doses at the start of therapy and the concentrations between sequential doses thereafter alter gradually over time.
A potential mechanism of the triple synergistic interaction is the increased AMB+CIP antifungal activity, which may facilitate phagocytosis by PMNs. In addition, AMB has been found to increase the uptake of CIP by PMNs (8), which may enhance the antifungal activity of the triple combination inside PMNs. In vivo combination studies have shown that the combination of ciprofloxacin (4 mg/kg/day) with AMB (0.1 mg/kg) provides significantly more protection to nonneutropenic mice infected by C. albicans than AMB or ciprofloxacin alone (24). Of note, ciprofloxacin (4 mg/kg/day) alone resulted in prolonged survival compared to the control, suggesting some immunomodulatory effect of this agent against candidiasis. Although it is difficult to conclude if this was the result of pharmacodynamic, pharmacokinetic, and/or immunological interactions, it seems that CIP and AMB can interact synergistically in the presence of neutrophils.
Of note, the combination of AMB and PMNs exhibited its synergistic effect against A. fumigatus growth at sub- and near-MIC concentrations (0.06 to 0.5 μg/ml) that are readily achieved in vivo. This suggests that PMNs may enhance the antifungal activity of AMB at the areas of infection. Furthermore, the fact that AMB interacted synergistically with CIP even in the absence of PMNs indicates that this combination would still have good efficacy in neutropenic patients. In vivo studies in experimental invasive aspergillosis are warranted to investigate these interactions in vivo.
This study found that the Bliss independence model proved to be a useful tool for assessing complex pharmacodynamic and immunomodulatory interactions, such as those between antifungal agents, nonantifungal compounds, and human phagocytes. We cannot draw direct clinical conclusions from just in vitro results, since conditions in the human body are much more complicated than those in in vitro experiments. By understanding what the situation is in vitro, however, we can conduct in vivo studies and test our initial hypothesis. Further animal studies are needed for better understanding of these in vitro interactions.
ACKNOWLEDGMENTS
These studies were supported in part by the Intramural Program of the National Cancer Institute and Aristotle University.
Footnotes
Published ahead of print on 12 September 2011.
REFERENCES
- 1. Afessa B., Peters S. G. 2006. Major complications following hematopoietic stem cell transplantation. Semin. Respir. Crit. Care Med. 27: 297–309 [DOI] [PubMed] [Google Scholar]
- 2. Bekersky I., et al. 2002. Pharmacokinetics, excretion, and mass balance of liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate in humans. Antimicrob. Agents Chemother. 46: 828–833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bellocchio S., et al. 2004. The contribution of the Toll-like/IL-1 receptor superfamily to innate and adaptive immunity to fungal pathogens in vivo. J. Immunol. 172: 3059–3069 [DOI] [PubMed] [Google Scholar]
- 4. Brakhage A. A., Bruns S., Thywissen A., Zipfel P. F., Behnsen J. 2010. Interaction of phagocytes with filamentous fungi. Curr. Opin. Microbiol. 13: 409–415 [DOI] [PubMed] [Google Scholar]
- 5. Dalhoff A., Shalit I. 2003. Immunomodulatory effects of quinolones. Lancet Infect. Dis. 3: 359–371 [DOI] [PubMed] [Google Scholar]
- 6. Dotis J., et al. 2008. Amphotericin B formulations variably enhance antifungal activity of human neutrophils and monocytes against Fusarium solani: comparison with Aspergillus fumigatus. J. Antimicrob. Chemother. 61: 810–817 [DOI] [PubMed] [Google Scholar]
- 7. Dotis J., et al. 2006. Effects of lipid formulations of amphotericin B on activity of human monocytes against Aspergillus fumigatus. Antimicrob. Agents Chemother. 50: 868–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Garcia I., Pascual A., Perea E. J. 1992. Effect of several antimicrobial agents on ciprofloxacin uptake by human neutrophils. Eur. J. Clin. Microbiol. Infect. Dis. 11: 260–262 [DOI] [PubMed] [Google Scholar]
- 9. Maurer N., Wong K. F., Hope M. J., Cullis P. R. 1998. Anomalous solubility behavior of the antibiotic ciprofloxacin encapsulated in liposomes: a 1H-NMR study. Biochim. Biophys. Acta 1374: 9–20 [DOI] [PubMed] [Google Scholar]
- 10. Meletiadis J., et al. 2001. Colorimetric assay for antifungal susceptibility testing of Aspergillus species. J. Clin. Microbiol. 39: 3402–3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Meletiadis J., et al. 2006. Triazole-polyene antagonism in experimental invasive pulmonary aspergillosis: in vitro and in vivo correlation. J. Infect. Dis. 194: 1008–1018 [DOI] [PubMed] [Google Scholar]
- 12. Meletiadis J., Verweij P. E., TeDorsthorst D. T., Meis J. F., Mouton J. W. 2005. Assessing in vitro combinations of antifungal drugs against yeasts and filamentous fungi: comparison of different drug interaction models. Med. Mycol. 43: 133–152 [DOI] [PubMed] [Google Scholar]
- 13. Pascoe J., Steven N. 2009. Antibiotics for the prevention of febrile neutropenia. Curr. Opin. Hematol. 16: 48–52 [DOI] [PubMed] [Google Scholar]
- 14. Petraitis V., et al. 2009. Combination therapy in treatment of experimental pulmonary aspergillosis: in vitro and in vivo correlations of the concentration- and dose-dependent interactions between anidulafungin and voriconazole by Bliss independence drug interaction analysis. Antimicrob. Agents Chemother. 53: 2382–2391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Poch G., Dittrich P., Holzmann S. 1990. Evaluation of combined effects in dose-response studies by statistical comparison with additive and independent interactions. J. Pharmacol. Methods 24: 311–325 [DOI] [PubMed] [Google Scholar]
- 16. Sau K., et al. 2003. The antifungal drug amphotericin B promotes inflammatory cytokine release by a Toll-like receptor- and CD14-dependent mechanism. J. Biol. Chem. 278: 37561–37568 [DOI] [PubMed] [Google Scholar]
- 17. Segal B. H. 2009. Aspergillosis. N. Engl. J. Med. 360: 1870–1884 [DOI] [PubMed] [Google Scholar]
- 18. Shen L. L., Baranowski J., Fostel J., Montgomery D. A., Lartey P. A. 1992. DNA topoisomerases from pathogenic fungi: targets for the discovery of antifungal drugs. Antimicrob. Agents Chemother. 36: 2778–2784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Simitsopoulou M., et al. 2005. Differential expression of cytokines and chemokines in human monocytes induced by lipid formulations of amphotericin B. Antimicrob. Agents Chemother. 49: 1397–1403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Simitsopoulou M., Roilides E., Georgiadou E., Paliogianni F., Walsh T. J. 2011. Differential transcriptional profiles induced by amphotericin B formulations on human monocytes during response to hyphae of Aspergillus fumigatus. Med. Mycol. 49: 176–185 [DOI] [PubMed] [Google Scholar]
- 21. Steinbach W. J. 2010. Epidemiology of invasive fungal infections in neonates and children. Clin. Microbiol. Infect. 16: 1321–1327 [DOI] [PubMed] [Google Scholar]
- 22. Stergiopoulou T., et al. 2009. Comparative pharmacodynamic interaction analysis between ciprofloxacin, moxifloxacin and levofloxacin and antifungal agents against Candida albicans and Aspergillus fumigatus. J. Antimicrob. Chemother. 63: 343–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stergiopoulou T., et al. 2008. Isobolographic analysis of pharmacodynamic interactions between antifungal agents and ciprofloxacin against Candida albicans and Aspergillus fumigatus. Antimicrob. Agents Chemother. 52: 2196–2204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sugar A. M., Liu X.-P., Chen R. J. 1997. Effectiveness of quinolone antibiotics in modulating the effects of antifungal drugs. Antimicrob. Agents Chemother. 41: 2518–2521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. van Zanten A. R., et al. 2008. Ciprofloxacin pharmacokinetics in critically ill patients: a prospective cohort study. J. Crit. Care 23: 422–430 [DOI] [PubMed] [Google Scholar]
- 26. Zaoutis T. E., et al. 2010. Risk factors and predictors for candidemia in pediatric intensive care unit patients: implications for prevention. Clin. Infect. Dis. 51: e38–e45 [DOI] [PMC free article] [PubMed] [Google Scholar]