Abstract
We report an unusual case of extraintestinal infection with adult Enterobius vermicularis worms in the nares and ocular orbit of a 14-year-old girl in Illinois. Only one other similar case has been reported in the English-language literature.
CASE REPORT
A 14-year-old Caucasian girl presented to the local emergency department (ED) after having removed and discarded what she described as a small motile worm from her eye the night before. On physical examination, she appeared well and her vision was normal. Ocular exam by a nurse revealed a single motile worm beneath the right lower lid in the inferior conjunctival sac which was removed on a cotton swab. The patient was also seen by a physician's assistant who identified and removed three additional worms over a 60-min period. The patient was then seen by an ED physician, and ophthalmology and infectious diseases specialists were consulted. Based on the evaluation, the patient was discharged home with ciprofloxacin ophthalmic solution (1 to 2 drops to each eye applied twice per day) and instructed to follow up with the on-call ophthalmologist in 2 days. However, the patient returned to the ED within 1 h of discharge and two additional worms were identified and removed from the anterior surface of the right eye and inferior conjunctival sac. Further examination of the superior conjunctival sacs (with lid eversion), the medial canthus, the medial punctum, and the nares bilaterally did not reveal the presence of other worms. No additional treatment or follow-up was recommended at this time, and the patient was again discharged home. The following day, the patient reported a worm crawling out of her nose, which she discarded. She denied any additional symptoms, such as nocturnal perianal pruritus or worms in her stool, and denied any travel outside the United States or known exposure to individuals with helminth infections. A perianal cellulose tape preparation was not obtained but a stool parasite examination obtained 2 days after her ED visit by her primary care physician revealed ova of Enterobius vermicularis. Based on this result, she was treated with a 3-day course of mebendazole (300 mg twice daily) but reported mucous nasal and ocular discharge. Therefore, a computed tomography scan of her sinuses and an orbital MRI were performed 12 days after her visit to the ED and were interpreted as normal. On the advice of an infectious diseases specialist, the primary care physician prescribed a repeat course of oral mebendazole (300 mg twice daily for 3 days), which was followed by complete resolution of her symptoms.
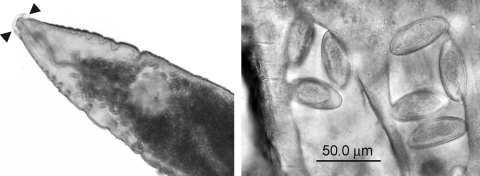
Six worms isolated from the patient's eye on both visits to the ED were collected in saline and submitted for identification to the Parasitology Laboratory at the Mayo Clinic in Rochester, MN. On macroscopic examination, the worms were white-tan and ranged in length from 4 to 10 mm. Microscopic examination of a representative worm revealed structures consistent with an adult female Enterobius vermicularis, including lateral alae, bulbous and muscular esophagus, gravid uterus containing characteristic eggs, and pointed tail (Fig. 1).
Fig. 1.
Gravid female (left) demonstrating lateral alae (arrowheads, unstained worm, 40× original magnification). Higher magnification of the worm (right) reveals characteristic eggs of Enterobius vermicularis (unstained, 400× original magnification).
Enterobius vermicularis, often referred to as pinworm, is an intestinal nematode which commonly infects children throughout the world. Transmission of E. vermicularis eggs occurs through the fecal-oral route, with eggs being directly inoculated from the fingers into the mouth. Fomites may also play a role in transmission. The eggs are infective shortly after being laid, making autoinfection a common route of intestinal infection. Following ingestion, the embryonated eggs hatch in the small intestine and develop into adult worms that reside in the cecum, appendix, colon, and rectum. Male and female worms mate in the human intestinal tract, and the gravid female worm migrates to the anus to lay partially embryonated eggs on the perianal and perineal surfaces. The migration of the female worm to the anus causes pruritus, which is the most common symptom of pinworm infection (2, 9). Less commonly, the presence of adult worms in the appendix can lead to obstruction, inflammation, and resultant appendicitis (8, 11). Rarely, the adult worms can become lodged in the intestinal mucosa and cause intestinal abscess.
Extraintestinal presentation is also very rare. The most common extraintestinal site is the female reproductive tract (vagina, uterus, ovaries, and fallopian tubes) due to migration of the female worm from the anus (6, 15, 16). The female worm can also enter the urinary tract (17), kidneys (4), and biliary tract and liver (12). Finally, there are isolated case reports of infection involving the salivary glands (10), nasal mucosa (14), skin (1), and lungs (3), presumably due to autoinoculation of these sites with eggs or adult worms from the intestinal tract.
A review of the English-language literature revealed only one other case of E. vermicularis infection in the eye (7). This case from 1976 shows a remarkable similarity to the current case, as it describes an infection of a 15-year-old girl with a 7-day history of worms “crawling out of her eyes.” Her vision was normal and she continued to expel worms for approximately 3 weeks, with a total number of 42 worms identified. This patient did not have any other complaints, and stool exams were negative for worms. One difference between this case and ours is the fact that the patient never reported worms emerging from her nose. There was no indication in the previous report that a cellulose tape test was done.
According to the CDC guidelines (13), the recommended treatment for pinworm infection is oral pyrantel pamoate, given at a dose of 11 mg/kg of body weight. Alternatively, patients may be given one dose of mebendazole (100-mg tablet). A second dose may be given in cases where the infection persists—typically the result of autoinoculation. Testing and/or treatment should also be considered for household contacts, since environmental contamination with infective eggs is common. In this case, other members of the household were not tested or treated for pinworm infection, but recommendations for environmental cleaning were given.
Treatment of extraintestinal infections is not standardized. In the 1976 report by Dutta and Kalita (7), the patient was treated with a wash solution made of oral piperazine citrate diluted in water. In cases where the worms become lodged in tissue such as the appendix or ovaries (6, 8), surgery is performed to remove the worm, followed by treatment with mebendazole. In our case, the patient was treated with an extended course of mebendazole, following which there was resolution of her symptoms. The presumed failure of the initial 3-day treatment may be due to the relative ineffectiveness of mebendazole toward worms in earlier stages of development (5) or may be due to a relatively protected nonintestinal worm location.
In conclusion, we report here an extremely rare case of E. vermicularis detection in a young girl's eye and, possibly, nose. Although the mechanism by which eggs or worms reached this location is not clear, it is most likely the result of direct inoculation of adult female worms from the perianal skin to the eyes by the child's fingers. Alternatively, eggs could have been inadvertently inoculated, followed by hatching of both male and female worms and fertilization of some of the female worms. Since not all of the worms that were found in the child's nose and eye were submitted for evaluation, we do not know if there were any male worms present (though they would be less likely to migrate). Only gravid females were identified in the laboratory. Both scenarios assume the presence of a primary intestinal infection, which was diagnosed by finding characteristic eggs in the stool of this patient.
Footnotes
Published ahead of print on 28 September 2011.
REFERENCES
- 1. Arora V. K., Singh N., Chaturvedi S., Bhatia A. 1997. Fine needle aspiration diagnosis of a subcutaneous abscess from Enterobius vermicularis infestation. A case report. Acta Cytol. 41:1845–1847 [DOI] [PubMed] [Google Scholar]
- 2. Ash L. R., Orihel T. C. (ed.) 2007. Enterobius vermicularis, p. 191–195 In Ash and Orihel's Atlas of Human Parasitology, 5th ed. ASCP Press, Chicago, IL [Google Scholar]
- 3. Beaver P. C., Kriz J. J., Lau T. J. 1973. Pulmonary nodule caused by Enterobius vermicularis. Am. J. Trop. Med. Hyg. 22:711–713 [DOI] [PubMed] [Google Scholar]
- 4. Cateau E., Yacoub M., Tavilien C., Becq-Giraudon B., Rodier M. H. 2010. Enterobius vermicularis in kidney: an unusual location. J. Med. Microbiol. 59(Pt. 7):860–861 [DOI] [PubMed] [Google Scholar]
- 5. Cho S. Y., Kang S. Y., Kim S. I., Song C. Y. 1985. Effect of anthelmintics on the early stage of Enterobius vermicularis. Kisaengchunghak Chapchi 23:7–17 [DOI] [PubMed] [Google Scholar]
- 6. Craggs B., et al. 2009. Enterobius vermicularis infection with tuboovarian abscess and peritonitis occurring during pregnancy. Surg. Infect. (Larchmt.) 10:545–547 [DOI] [PubMed] [Google Scholar]
- 7. Dutta L. P., Kalita S. N. 1976. Enterobius vermicularis in the human conjunctival sac. Indian J. Ophthalmol. 24:34–35 [PubMed] [Google Scholar]
- 8. Efraimidou E., Gatopoulou A., Stamos C., Lirantzopoulos N., Kouklakis G. 2008. Enterobius vermicularis infection of the appendix as a cause of acute appendicitis in a Greek adolescent: a case report. Cases J. 1:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garcia L. 2007. Enterobius vermicularis, p. 258–261 In Garcia L. S. (ed.), Diagnostic medical parasitology. ASM Press, Washington, DC [Google Scholar]
- 10. Gargano R., Di Legami R., Maresi E., Restivo S. 2003. Chronic sialoadenitis caused by Enterobius vermicularis: case report. Acta Otorhinolaryngol. Ital. 23:319–321 [PubMed] [Google Scholar]
- 11. Isik B., et al. 2007. Appendiceal Enterobius vermicularis infestation in adults. Int. Surg. 92:221–225 [PubMed] [Google Scholar]
- 12. Little M. D., Cuello C. J., D'Alessandro A. 1973. Granuloma of the liver due to Enterobius vermicularis. Report of a case. Am. J. Trop. Med. Hyg. 22:567–569 [DOI] [PubMed] [Google Scholar]
- 13. Medical Letter, Inc 2010. The medical letter on drugs and therapeutics. Drugs for parasitic infections. The Medical Letter, Inc., New Rochelle, NY [Google Scholar]
- 14. Vasudevan B., Rao B. B., Das K. N., Anitha 2003. Infestation of Enterobius vermicularis in the nasal mucosa of a 12 yr old boy-a case report. J. Commun. Dis. 35:138–139 [PubMed] [Google Scholar]
- 15. Worley M. J., Jr., Slomovitz B. M., Pirog E. C., Caputo T. A., Ledger W. J. 2009. Enterobius vermicularis infestation of a hysterectomy specimen in a patient with a colonic reservoir. Am. J. Obstet. Gynecol. 200:e6–e7 [DOI] [PubMed] [Google Scholar]
- 16. Young C., Tataryn I., Kowalewska-Grochowska K. T., Balachandra B. 2010. Enterobius vermicularis infection of the fallopian tube in an infertile female. Pathol. Res. Pract. 206:405–407 [DOI] [PubMed] [Google Scholar]
- 17. Zahariou A., Karamouti M., Papaioannou P. 2007. Enterobius vermicularis in the male urinary tract: a case report. J. Med. Case Reports 1:137. [DOI] [PMC free article] [PubMed] [Google Scholar]