Abstract
The soft tick Ornithodoros hermsi, which ranges in specific arboreal zones of western North America, acts as a vector for the relapsing fever spirochete Borrelia hermsii. Two genomic groups (genomic group I [GGI] and GGII) of B. hermsii are differentiated by multilocus sequence typing yet are codistributed in much of the vector's range. To test whether the tick vector can be infected via immersion, noninfected, colony-derived O. hermsi larvae were exposed to reduced-humidity conditions before immersion in culture suspensions of several GGI and GGII isolates. We tested for spirochetes in ticks by immunofluorescence microscopy and in mouse blood by quantitative PCR of the vtp locus to differentiate spirochete genotypes. The immersed larval ticks were capable of spirochete transmission to mice at the first nymphal feeding. Tick infection with mixed cultures of isolates DAH (vtp-6) (GGI) and MTW-2 (vtp-5) (GGII) resulted in ticks that caused spirochetemias in mice consisting of MTW-2 or both DAH and MTW-2. These findings show that this soft tick species can acquire B. hermsii by immersion in spirochete suspensions, that GGI and GGII isolates can coinfect the tick vector by this method, and that these spirochetes can be cotransmitted to a rodent host.
INTRODUCTION
Ornithodoros hermsi and other argasid tick species serve as vectors for spirochetal agents of endemic relapsing fever, potentially lethal infections characterized by serial bacteremic episodes in the blood, spleen, and liver facilitated by the antigenic switching of bacterial outer membrane lipoproteins (25, 36). Organ failure can result from the massive antigen burden as immune complexes are cleared from the circulation or from the release of cellular components upon the administration of antibiotic therapy (Jarisch-Herxheimer reaction [20]). The worldwide distribution of relapsing fever Borrelia spp. reflects the corresponding presence of a number of argasid tick species. The basis of this apparent vector-pathogen cospeciation has not been elucidated (3).
A previously reported survey of Borrelia hermsii isolates by sequence analyses and Southern blots of vlp and vsp variable surface antigen genes suggested genetic divergence into at least two separate groups (17). A study of the 16S-23S intergenic spacer region and the p66 gene indicated that nine B. hermsii isolates diverged into at least two separate groups consisting of four distinct types (10). Subsequent comparisons of four conserved chromosomal loci in 31 isolates confirmed the divergence of B. hermsii into two genomic groups (genomic group I [GGI] and GGII); both groups appear to be distributed throughout the vector's range (27). Additionally, the adenine deaminase gene (adeC) is a pseudogene in three examined GGI isolates but is intact in GGII isolates, suggesting a relative deficit in the purine salvage capacity for GGI organisms (24). Selection in enzootic cycles may drive the emergence of B. hermsii variants with increased virulence, with implications for human disease severity.
Our interest in modeling the mixed transmission of GGI and GGII isolates by ticks was initiated by the isolation of GGI and GGII B. hermsii strains from separate human relapsing fever cases at a single infestation site (31, 32). Since O. hermsi and other argasid ticks are multistaged, requiring a blood meal at the larval stage and at 3 to 5 nymphal stages in addition to multiple feedings as adults (14), they may acquire several spirochete genotypes from infected hosts and subsequently deliver these genotypes to a vertebrate host. Individual ticks may transmit a genotypically clonal population or a heterogeneous population of spirochetes that yields a single dominant genotype upon cultural isolation; no human relapsing fever isolates to date have demonstrated heterogeneity in the genotype of the cultured spirochetes. Hard ticks such as Ixodes spp. can be colonized simultaneously by two or more Borrelia burgdorferi sensu lato species (16), and coinfection of wild rodents was reported previously (18), but no reports of similar results from field collections of Ornithodoros spp. are available. This is partly due to the difficulty in the isolation of relapsing fever spirochetes from ticks or human patient blood (15), which may obscure the presence of a heterogeneous population in the source material.
To test the vector competence of O. hermsii with distinct relapsing fever genotypes, we adapted an artificial infection method used with the Lyme disease agent Borrelia burgdorferi and the ixodid (hard-bodied) tick Ixodes scapularis, which involves tick immersion in a suspension of the spirochete (7, 26). This method is adapted here as a means of artificially infecting O. hermsi, an argasid (soft-bodied) tick, with isolates of B. hermsii. After proving this method, we used immersion in mixed cultures of GGI and GGII B. hermsii isolates to determine if the coinfection of ticks results in cotransmission to the mouse host.
MATERIALS AND METHODS
B. hermsii isolates and culture.
All B. hermsii isolates were previously described (32). Spirochetes were cultured in Barbour-Stoenner-Kelly II (BSK-II) medium, prepared as described previously (5), or in BSK-H medium (Sigma-Aldrich, St. Louis, MO) containing 12% normal rabbit serum (nonhemolyzed; Pel-Freez, Rogers, AR) to a density of 5 × 106 to 2 × 107 spirochetes per ml. Suspensions were centrifuged for 10 min at 1.04 × 104 × g and resuspended in fresh or supernatant medium to adjust all isolates to equivalent densities, which are specified for individual experiments.
O. hermsi artificial infection by immersion.
Colonies of O. hermsi were maintained at room temperature (RT) at a relative humidity (RH) of 89% in desiccator jars containing a saturated KCl solution in their reservoirs. Larvae (8 to 12 weeks postemergence) were divided as groups of 20 to 40 into 1.5-ml screw-cap microcentrifuge tubes (Sarstedt, Inc., Newton, NC). To attempt an enhancement of rehydration behavior during immersion, we preexposed larvae to a range of reduced RH values, below the colony maintenance level of 89%. Caps of tubes were punctured several times with a 30-gauge syringe needle, and larvae were exposed to one of six RHs using the following saturated salts: KCl (RH, 89%), Mg(C2H3O2)2 (RH, 76%), KCl-NaCl (RH, 76%), NaNO2 (RH, 66%), MnCl2 (RH, 56%), and K2CO3 (RH, 42%). Salts were selected on the basis of previously reported RH values (39), and RH was monitored by use of an RH meter (Traceable Digital Humidity/Temperature meter, catalog number 4096; Control Co., Friendswood, TX). Larvae were then exposed to B. hermsii isolates by the addition of suspensions in BSK-II medium containing 12% normal rabbit serum, the replacement of the perforated cap with an intact cap, and tick dispersion by gentle agitation. Tubes were incubated at 32°C for 1.5 h, with mixing every 15 min to maintain the dispersion of ticks. After incubation, tubes were centrifuged at RT at 200 × g for 30 s, and supernatant medium was aspirated with a 200-μl gel loading tip (Genemate MultiFlex; BioExpress, Kaysville, UT). Ticks were washed twice with 500 μl phosphate-buffered saline (PBS) to remove the spirochete suspension from the tick exoskeleton and the interior of the tubes, with centrifugation and aspiration following each wash. Larvae were held at least 2 weeks at an RH specified by the experiment to allow the loss of body volume from fluid acquired during immersion and were then fed on 5- to 6-day-old RML mice, an outbred Swiss-Webster strain, or IRW mice, an inbred strain derived from Swiss-Webster mice (11). Mouse experiments and rabbit immunization (see below) were done at Rocky Mountain Laboratories in compliance with Institutional Animal Care and Use Committee guidelines. Engorged larvae were held in incubation jars until molting for subsequent feeding as nymphs.
Transmission of B. hermsii to mice.
Nymphs were allowed to feed to repletion (≤1 h) on the shaved abdomens of pentobarbital sodium-anesthetized adult female IRW mice. Mice were tested daily for the presence of spirochetes in fresh mounts of blood from the tail vein, up to 1 week postfeed. Mice were sacrificed on the second day of the initial spirochetemia or on the seventh day postfeeding for those mice showing no detectable spirochetemia. Blood was collected at sacrifice by cardiac puncture under isoflurane anesthesia and extracted for total nucleic acids as recommended by the manufacturer (DNeasy; Qiagen, Inc., Valencia, CA).
Immunofluorescence assay (IFA) of tick tissue.
A polyclonal rabbit antiserum, J5750, was generated against the recombinant B. hermsii DAH flagellin (FlaB) protein. The 1,005-nucleotide (nt) full-length flaB chromosomal open reading frame (GenBank accession number CP000048) was PCR amplified from 100 ng DAH DNA with primers BhflaBpet5′ (GAAACTCGAGATGATCATAAATCATAATACGTCAGC) and BhflaBpet3′ (GCCGGATCCATTTATCTAAGCAATGATAATACATATTGAGG) (the noncoding linker sequences are underlined) in a 50-μl reaction mixture (GoTaq Flexi DNA polymerase; Promega, Madison, WI). PCR conditions were as follows: 1 cycle at 96°C for 3 min and 35 cycles at 94°C for 30 s, 60°C for 30 s, and 72°C for 2 min, followed by 1 cycle at 72°C for 7 min. The product was isolated by use of a QIAquick PCR purification kit (Qiagen), digested with the restriction enzymes BamHI and XhoI (New England BioLabs, Waverly, MA) according to the supplier's recommendations, and purified by QIAquick PCR purification. The BamHI- and XhoI-digested pET15b vector (EMD Novagen, Madison, WI), purified by agarose gel electrophoresis and QIAquick gel extraction (Qiagen) and ligated with flaB DNA (T4 DNA ligase; New England BioLabs) as recommended by the manufacturer, was used to transform BL21 Star(DE3) OneShot chemically competent Escherichia coli cells (EMD Novagen). An ampicillin-resistant (50 μg/ml) colony from Luria-Bertani (LB) plates, which screened positive for flaB DNA by PCR, was expanded in LB broth for the induction of protein. N-terminally His-tagged FlaB was isolated with Ni-nitrilotriacetic acid (NTA) His-Bind resin as recommended by the manufacturer (EMD Novagen). The eluted protein, mixed with adjuvant as recommended by the manufacturer (RAS R-730; Corixa Corp., Seattle, WA), was used to immunize a New Zealand White rabbit, with a 4-week interval before the second immunization and a 6-week interval before the third immunization. Antiserum was collected 2 weeks after the third immunization and verified for specificity by a Western blot reaction to FlaB recombinant and total DAH proteins (data not shown). Tick midguts and salivary glands were dissected in PBS on 12-well, polytetrafluoroethylene-printed microscope slides (Electron Microscopy Sciences, Hatfield, PA). Midgut tissue was macerated, and supernatant PBS was removed. Salivary glands were removed into a separate well, dispersed as clusters of acini, and rinsed once with PBS to remove extraneous tissue and spirochetes and once with H2O to reduce salt deposition. Slides were air dried, fixed for 10 min in acetone, and stored at −20°C. Tissue was rehydrated in PBS for 10 min, blocked with PBS–0.75% bovine serum albumin (PBSA) for 30 min, reacted with J5750 antiserum in PBSA for 30 min, washed with PBS, reacted with Alexa Fluor 488 goat anti-rabbit IgG antiserum (Molecular Probes, Invitrogen Corp., Carlsbad, CA) in PBSA, washed with PBS, and air dried. Coverslips were mounted with Vectashield medium (Vector Laboratories, Burlingame, CA) and viewed with a 40× objective on a Nikon Eclipse E800 fluorescence microscope (Nikon Instruments, Melville, NY); images were captured with a 100× objective and oil immersion with a DXM1200C digital camera and ACT-1C software, version 1.0.1.5 (Nikon).
Quantitative PCR (qPCR) of infected mouse blood.
A consensus 16S rRNA gene (rrs) sequence was compiled with MacVector (version 11.1.2; MacVector, Inc., Cary, NC), with sequences from the following GGI and GGII isolates (accompanied by their GenBank accession numbers in parentheses): HS1 (AY597656), DAH (AY597657), MAN (AY597673), SIS (AY597668), CON (AY597661), YOR (AY597686), LAK-2 (AY597679), CMC (AY597675), REN (AY597685), MTW-1 (EU203149), and MTW-2 (EU203150). Consensus sequences for the vtp-6 allele, with sequences from isolates DAH (GenBank accession number AY597747.1), HS1 (accession number AY597746.1), HAL (accession number AY597750.1), and MIL (accession number AY597748.1), and for the vtp-5 allele, with sequences from isolates MTW-2 (accession number EU194847.1) and YOR (accession number AY597776.1), were likewise compiled with MacVector. Oligonucleotide primers and fluorescent probes for these targets were identified with ABI Primer Express software (version 2.0.0; Applied Biosystems, Foster City, CA) and validated as targets for B. hermsii isolates by alignment with MacVector and the NCBI search tool blastn (1). The primer sequences for rrs were as follows: forward primer GGAGGCAGCAGCTAAGAATCTTC, probe 6-carboxyfluorescein (FAM)–CTCCGTCAGGCTTTCGCCCATTG–6-carboxytetramethylrhodamine (TAMRA), and reverse primer CCTTCTTCGTTCACGCAGTGT. The primer sequences for vtp-6 were as follows: forward primer AGTTTGCTGGACTAAAGGAAAAGG, probe FAM-AAGAAATCATCACTTCCCTTCTTAGCAGCAACA-TAMRA, and reverse primer TTATGCTGCGCTTTTACTTTGG. The primer sequences for vtp-5 were as follows: forward primer AGGAGCAAGTGGTGATCTTGGT, probe FAM-CTATAGCTTTTTTTGCATCATCACTCTTAGCAGCAG-TAMRA, and reverse primer CTTTTGCGCCATTTTTTCG. Target sequences in triplicate aliquots for each mouse blood DNA sample were detected with an ABI Prism 7900HT sequence detection system (Applied Biosystems) by using Brilliant II QPCR Master Mix (Agilent Technologies, Santa Clara, CA) as recommended by the supplier and 300 nM primer and 50 nM probe concentrations. Thermal cycling parameters were 1 cycle each for 2 min at 50°C and 10 min at 95°C, followed by 40 cycles of 15 s at 95°C and 1 min at 60°C. All reported values were determined by assays in which the amplification efficiency was at least 90% (slope of the threshold cycle [CT] versus the log copy number of ≥−3.6), using purified DAH and MTW-2 DNAs as gene copy number standards.
Statistical analysis of tick infection rates.
GraphPad Prism for Mac OS X (version 5.0c; GraphPad Software, Inc., La Jolla, CA) was used for regression analysis and analysis of significant differences between groups, as specified in individual experiments.
RESULTS
Relative humidity and acquisition of spirochetes.
In an initial test of spirochete uptake, O. hermsi larvae were exposed to 76% RH for 2 days prior to immersion in 2.5 × 107 spirochetes per ml of B. hermsii YOR, a GGII isolate, for 1.5 h. After washing as described above (see Materials and Methods), ticks were held at 89% RH. Midgut tissue from four larvae was examined at 6 days postimmersion by IFA for the presence of spirochetes. Two ticks showed the presence of multiple bacteria. To see if rates of spirochete acquisition in O. hermsi were enhanced by exposure to a lower RH preimmersion, we exposed recently hatched larvae to 89%, 76% (two saturated salt solutions), 67%, and 56% RHs for 48 h before the addition of 1 × 107 spirochetes per ml of B. hermsii YOR to each tube, followed by recovery from the medium and storage for 10 days at 89% RH and 4 days at 76% RH. At 2 weeks postimmersion, each group of ticks was exposed to a naïve mouse to allow feeding. Four weeks after this feeding, all viable ticks were tested for spirochete uptake. Salivary gland and midgut tissues were tested by IFA for spirochetes; six nonimmersed, colony-derived larvae, fed separately, were all negative for spirochetes in this IFA. Linear regression analysis showed a negative correlation between the RH value before immersion in YOR and the percentage of IFA-positive ticks after mouse feeding (two-tailed P value = 0.0132; R2 = 0.9030) (Fig. 1). Survival for each group was not correlated to RH exposure before immersion by linear regression analysis (two-tailed P value = 0.1511; R2 = 0.5506). These data indicate an enhancement of the artificial infection rate if ticks are exposed to a reduced RH prior to immersion.
Fig. 1.
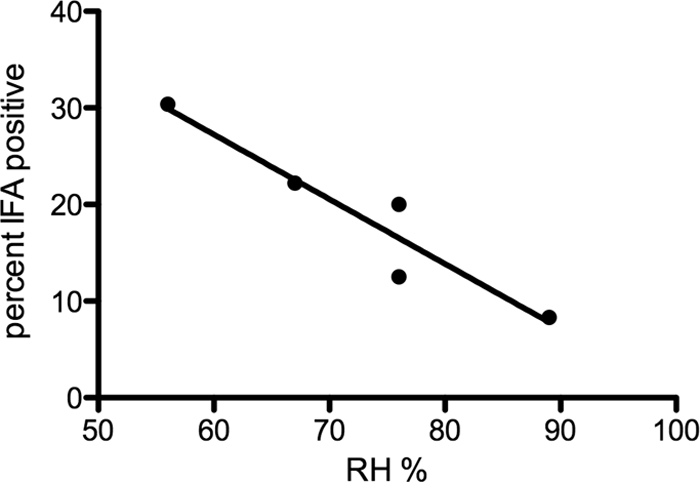
Regression analysis of relative humidity prior to immersion in spirochete suspensions and percentage of O. hermsi ticks positive for B. hermsii infection by IFA. The relative humidities (RH %) for five saturated salt solutions are shown along with the percentages of ticks showing detectable spirochete infection after exposure to these conditions and immersion in suspensions of B. hermsii YOR (see Materials and Methods). A 76% RH corresponds to Mg(C2H3O2)2 (20% positive) and to KCl-NaCl (12.5% positive) salt solutions.
Artificial infection by GGI and GGII isolates and transmission to mice.
O. hermsi larvae were immersed in multiple GGI and GGII isolates to test vector competence with the two genomic groups. We pretreated larvae at 42% RH for 48 h as an extension of the above-described results for YOR, because the pretreatment RH of 56% produced only a 30.4% infection rate. Five GGI isolates (DAH, BRO, MIL, CAR, and SIS) and two GGII isolates (LAK-2 and MTW-2) were adjusted to equal densities of 2 × 107 spirochetes per 0.5 ml and added to tubes containing larvae. The larval ticks were again allowed to recover for 2 weeks postimmersion before feeding on mice but were held at 56% RH for 6 days, followed by 42% RH for 8 days. We anticipated that exposure to a reduced RH postimmersion would increase the evaporative loss of water from imbibed spirochete culture medium, allow larval feeding to repletion on mouse blood, and allow development through ecdysis. In comparison to the preceding experiment (89% and 76% RHs), the lower RH for the postimmersion period (56% and 42% RHs) appeared to increase the rate of ecdysis after larval feeding from approximately 20% to over 90%, without internal controls to verify this correlation. At 6 weeks after larval feeding, the newly developed nymphs were tested for their ability to transmit spirochetes to mice, a time point at which spirochetes are known to be present in salivary glands (30). Ten nymphs from each group were placed onto separate mice and allowed to feed. Mouse blood samples were examined daily for 7 days by dark-field microscopy for the presence of spirochetes. Spirochetemias were observed for mice fed upon by ticks exposed to isolates DAH, BRO, and CAR from GGI and isolates MTW-2 and LAK-2 from GGII. GGI isolates SIS and MIL were not transmitted, based on this method of detection. No attempt was made to produce axenic cultures from the blood of spirochetemic mice. After molting to second-stage nymphs, dissected tick midguts and salivary glands were examined by IFA to determine spirochete infection frequencies for each group (Table 1). The frequency of tick infection (nymphs positive by IFA as a percentage of fed nymphs) varied between 0 and 90% among the experimental groups. The acquisition of spirochetes, as judged by percent infection in nymphal ticks, was not correlated to the culture density of isolates prior to adjustment for immersion (P = 0.6397 by Pearson test); however, MIL was the least dense culture, and spirochete aggregation upon centrifugation and resuspension may have limited the larval uptake of these spirochetes. SIS-infected ticks were observed to have relatively few spirochetes in salivary gland tissue, suggesting that this isolate may also have a lower transmission efficiency than those of the other tested isolates. In contrast, a single infected tick transmitted the DAH isolate. The aggregate rate of infection was 31.8% (22 IFA-positive ticks per 69 tested) for these tick larvae preexposed to 42% RH, compared to 30.4% in the 56% RH group, as shown in Fig. 1. Thus, both GGI and GGII B. hermsii isolates were capable of infecting larvae by immersion, and members of both GGI and GGII were transmitted to mice upon nymphal feeding.
Table 1.
O. hermsi acquisition and transmission of GGI and GGII isolates of B. hermsii
| Genomic group | Isolate | No. of spirochetes/ml preimmersion | No. of fed nymphs | Presence of mouse spirochetemia | No. of nymphs positive by IFA |
|---|---|---|---|---|---|
| I | DAH | 3.8e+07 | 10 | + | 1 |
| BRO | 1.1e+07 | 10 | + | 4 | |
| CAR | 1.5e+07 | 10 | + | 9 | |
| MIL | 0.5e+07 | 10 | − | 0 | |
| SIS | 3.6e+07 | 10 | − | 3 | |
| II | LAK-2 | 3.9e+07 | 10 | + | 2 |
| MTW-2 | 2.2e+07 | 9 | + | 3 |
Transmission by GGI- and GGII-coinfected ticks.
We chose GGI isolate DAH and GGII isolate MTW-2 to attempt cotransmission to mice because they demonstrated acquisition and transmission by immersed ticks and because they possess distinct vtp alleles that could be used to differentiate spirochetes in mixed infections (see below). Three larval groups were preexposed to 42% RH and three groups were exposed to 56% RH for 72 h, and one group from each preexposure condition was immersed in suspensions of DAH or MTW-2, each adjusted to 1 × 107 spirochetes per ml, or a suspension containing equal DAH and MTW-2 densities of 5 × 106 spirochetes per ml. After 14 days of postimmersion recovery at 56% RH, larvae were fed on mice and allowed to molt, and groups of three molted nymphs were fed on mice. In Table 2, the ticks preexposed to 42% RH represent the first DAH immersion group, the first MTW-2 immersion group, and the first three DAH-plus-MTW-2 immersion groups; the ticks preexposed to 56% RH are the remaining groups for each immersion condition. There was no significant difference when transmission rates (2 of 5 versus 3 of 5 ticks) between the 42% and 56% RH pretreatment groups were compared by Fisher's exact test (P = 1.00), and thus, they are arranged in Table 2 by spirochete immersion condition. Each mouse was exposed to three ticks, but actual engorgement varied from one to three ticks per mouse. The mice were monitored as described above for spirochetemia. Based on the detection of spirochetes in blood, only one of four tick groups exposed to either DAH or MTW-2 alone, MTW-2 group 2, transmitted spirochetes to mice; four of six DAH-plus-MTW-2 tick groups, groups 1, 3, 5, and 6, transmitted spirochetes to mice. A 0.1-ml sample of blood from each mouse was inoculated into 5 ml BSK-II culture medium; spirochete cultures were obtained from the MTW-2 group 2 mouse and from DAH-plus-MTW-2 group 5 and 6 mice. However, we did not characterize the spirochete genotypes in these cultures by qPCR (see below). After feeding on mice, tick salivary glands were examined by IFA for the presence of spirochetes. In all cases in which IFA-positive ticks fed on mice, there was transmission, as detected by spirochetemia and B. hermsii gene copy numbers in blood. Mouse blood DNA was tested by qPCR for rrs, vtp-6, and vtp-5 gene copy numbers to determine the representation of DAH plus MTW-2, DAH, and MTW-2, respectively. The B. hermsii genome contains a single gene encoding the 16S rRNA subunit gene (rrs) (34). The rrs gene diverges between GGI and GGII, but a conserved sequence allows a qPCR oligonucleotide design that recognizes members of both groups (see Materials and Methods). The vtp gene encodes a lipoprotein that varies between B. hermsii isolates and was used to differentiate DAH and MTW-2 because these isolates carry the vtp-6 and vtp-5 alleles, respectively (27, 33). Three mice exposed to DAH-plus-MTW-2 tick groups 1, 5, and 6 showed evidence by qPCR of DAH (vtp-6) and MTW-2 (vtp-5) cotransmission. For two of three mice showing vtp-6 and vtp-5 gene copies in blood, IFA results indicated that one tick per mouse acted as the transmitting agent (groups 1 and 6). Therefore, individual ticks exposed to mixed GGI and GGII spirochetes by immersion are capable of transmitting this mixed infection to a mouse host. However, no conclusion can be made regarding the predominance of MTW-2 or DAH transmission with this sample size.
Table 2.
Immersion of O. hermsi larvae in a mixed suspension and nymphal transmission to mice
| B. hermsii isolate used for immersion | Tick group | No. of ticks positive by IFA/total no. of ticks fed | Presence of mouse spirochetemia | Mean gene copy no. ± SDa |
||
|---|---|---|---|---|---|---|
| rrs | vtp-6 | vtp-5 | ||||
| DAH | 1 | 0/3 | − | 0 | 0 | 0 |
| 2 | 0/1 | − | 0 | 0 | 0 | |
| MTW-2 | 1 | 0/3 | − | 0 | 0 | 0 |
| 2 | 1/3 | + | 950.4 ± 11.7 | 0 | 921.2 ± 129.5 | |
| DAH + MTW-2 | 1 | 1/3 | + | 5,822.3 ± 417.8 | 2.4 ± 0.8 | 3,333.4 ± 241.2 |
| 2 | 0/3 | − | 0 | 0 | 0 | |
| 3 | 1/2 | + | 1,416.7 ± 133.3 | 0 | 465.9 ± 134.7 | |
| 4 | 0/2 | − | 0 | 0 | 0 | |
| 5 | 2/3 | + | 421.8 ± 56.6 | 6.4 ± 0.6 | 60.4 ± 11.4 | |
| 6 | 1/2 | + | 2,305.7 ± 27.3 | 991.5 ± 150.6 | 794.3 ± 22.5 | |
Determined by qPCR of mouse blood. The assay represents gene copies per 2.5 ng total nucleic acid.
Transmission competence of artificially infected larvae.
The reproducibility of transmission by molted nymphs suggested that larvae may be capable of transmission during the initial blood meal after immersion. We tested this with three larval groups exposed to 42% RH for 72 h and immersed in DAH or MTW-2 suspensions adjusted to 2 × 107 spirochetes per ml or a DAH–MTW-2 mixed suspension with 1 × 107 spirochetes of each isolate per ml. After recovery for 10 days at 56% RH and 7 days at 42% RH, larvae in groups of 7 to 11 were exposed to adult mice. Larval ticks that successfully engorged were tested by IFA at 4 weeks postfeeding (Table 3). Nine larvae of 42 total were positive for spirochetes by IFA. Mice were monitored for spirochetemias for 1 week postfeeding; none of the eight mice showed spirochetemia, including the six fed upon by IFA-positive larvae. Immersion-infected O. hermsi appears to be less efficient or incapable of larval-stage transmission to mice compared to nymphs derived from these immersed larvae.
Table 3.
Immersion of O. hermsi larvae in a mixed suspension and transmission to mice prior to molting
| B. hermsii isolate used for immersion | Tick group | No. of ticks positive by IFA/total no. of ticks fed | Mouse spirochetemia |
|---|---|---|---|
| DAH | 1 | 2/3 | − |
| 2 | 2/5 | − | |
| MTW-2 | 1 | 1/3 | − |
| 2 | 0/6 | − | |
| 3 | 2/4 | − | |
| DAH + MTW-2 | 1 | 1/11 | − |
| 2 | 1/7 | − | |
| 3 | 0/3 | − |
DISCUSSION
The survey of tick infection with GGI and GGII isolates showed that artificial uptake by larvae is generally applicable to B. hermsii isolates but does not define which isolates are most likely to be internalized by larvae. Despite exposure to low RH before immersion, only a minority of larvae became infected by this artificial method. In contrast, a previous report found that O. hermsi nymphal acquisition from infected animals resulted in a transmission rate of 65% (14). A recent report indicated that O. hermsi nymphs feeding on spirochetemic mice showed 100% acquisition (22). Immersion-mediated O. hermsi infection with B. hermsii depends on simple procedures, but parameters should be further developed to use the limited tick resource more effectively. An RH of ≤42% for 48 h preimmersion and for at least 14 days postimmersion appears to be useful for increasing the larval infection rate and feeding success. Since spirochete densities in mouse blood reach densities similar to those in suspensions in these artificial infections, the physiology of spirochetes as they exist in blood or blood components or tick responses to the blood meal may be involved in greater spirochete uptake or higher survival rates during natural tick feeding. A modification of the immersion medium to include a higher spirochete density and blood supplementation may help increase acquisition by the larvae.
Without tracking fluid intake in these larvae, we refer to previous work on tick physiology to suggest the route of artificial infection. The tick integument protects ticks from transient reductions in the RH, but behavioral measures are also used to replace water and maintain electrolyte balance. A reduction in the ambient RH from optimal values causes ixodid ticks to dehydrate and induces liquid uptake via the mouthparts upon exposure to high water vapor levels (29). We therefore used preexposure to a reduced RH to enhance artificial infection rates in I. scapularis larvae (7). Argasid ticks also rehydrate after exposure to reduced RH (4, 9, 12, 35). Ornithodoros moubata nymphs apparently use spiracular respiration as a method of increasing water uptake after exposure to low humidity (21). Except for Argas arboreus (28), spiracles have not been observed for argasid tick larvae, nor have they been observed for O. hermsi larvae in particular (19); without spiracles, their mode of fluid uptake is most likely via the oral cavity. This observation alone is a rationale for the use of the larval stage in this study of infection by immersion. However, a similar method may be applied to direct nymphal infection, if they rehydrate using the oral cavity. Once they take up spirochetes, larvae appear to be incompetent to transmit until they molt. This finding is a significant difference from I. scapularis immersion-infected larvae, which are competent to transmit B. burgdorferi prior to molting (26). Transovarially infected O. hermsi larvae can transmit B. hermsii at a low frequency (38), but nymphal O. hermsi ticks do not transmit efficiently until ecdysis (14). Successful migration to salivary gland acini seems to require interactions between spirochetes and tick tissue that can occur only during this developmental transition.
Isolates DAH and MTW-2 were taken up by larval ticks by immersion, persisted through the initial feeding on mice and transstadially to the first nymphal stage, and were then transmitted to mice. We utilized divergent vtp-6 and vtp-5 alleles to track DAH and MTW-2, respectively, in mouse blood. Building on extensive studies of antigenic variation in B. hermsii (6, 36), a study of spirochete variable surface proteins in the mouse-tick cycle showed that Vtp is produced as spirochetes disseminate from the midgut during tick colonization but repressed after they enter the mouse host: the expression of the antigenic variation locus vmp is induced after transmission to the mouse (30). The latter study found that the same Vmp antigen was present when spirochetes were isolated from the previous mouse host. The specific protein product of this locus may play a role in tissue tropism and disease severity in the host (23); however, the identity of the sequences present at vmp before or after artificial infection in the present study was not determined.
The acquisition and transmission of a mixed B. hermsii population by ticks will help us model relative vector competence for GGI and GGII spirochetes in zoonotic cycles. The cotransmission of the two isolates in this instance shows that there is no absolute exclusion of one genotype by another when the vector is artificially infected and is tested for transmission after a single molt. GGII isolate MTW-2 produces severe spirochetemias in Mus musculus, to the extent that mice often require euthanization during the initial stage of infection, but this does not prevent the vector from harboring this isolate transstadially, and it is presumably tolerated by rodent hosts in its endemic locus (33). Virulence phenotypes of relapsing fever isolates in vertebrate hosts may represent gene functions that are not evident in the vector, where the invasion of tissues necessary for transmission may occur without pathogenic effects. If the acquisition and transmission of mixed spirochete populations occur in natural zoonotic cycles, it may allow the expansion of genotypic variants and benefit spirochete replication in the host. Immune challenge by a heterologous mixture of spirochetal Vmp antigens may allow a greater presence in the blood, extended relapses, and an increased probability of acquisition by the tick vector. Relapsing fever spirochetes possess over 50 silent cassettes capable of insertion and expression at the vmp locus (13), but a resolution of infection in mice provides long-lasting B1b cell-mediated immunity to reinfection (2). Relapsing fever maintenance in a tick-host cycle therefore requires transmission to naïve hosts. Vector coinfection in zoonotic cycles may allow recombinant exchange between divergent genotypes, but phylogenetic analyses of existing isolates suggest that this is not common (27).
O. hermsi is one of several argasid ticks in North America acting as relapsing fever spirochete vectors, but surveys of the presence of spirochetes and infection rates in natural populations of these species are limited. These ticks reside in animal nests and burrows; human relapsing fever cases result from habitation in proximity to these locations. Previous reports of Borrelia crocidurae in Ornithodoros erraticus and Ornithodoros sonrai ticks in North and West Africa suggested only limited divergence in the spirochete sequences examined after PCR amplification, and the surveys were not aimed at the detection of multiple genotypes per tick (8, 37). Additional Ornithodoros species are likely capable of infection in the manner described here, in which case qPCR-based methods may facilitate investigations of the cospeciation of vectors and relapsing fever spirochetes.
ACKNOWLEDGMENTS
We thank Brandi Williamson for providing tick larvae for some experiments, Merry Schrumpf for recombinant protein production and purification, and Anita Mora for assistance with figures. We also thank Phil Stewart, Jeff Shannon, and Travis Bourret for review of the manuscript and helpful discussions.
The Intramural Research Program of the NIAID, NIH, supported this research.
Footnotes
Published ahead of print on 30 September 2011.
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1. Altschul S. F., et al. 1997. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 25:3389–3402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alugupalli K. R., et al. 2004. B1b lymphocytes confer T cell-independent long-lasting immunity. Immunity 21:379–390 [DOI] [PubMed] [Google Scholar]
- 3. Assous M. V., Wilamowski A. 2009. Relapsing fever borreliosis in Eurasia—forgotten, but certainly not gone! Clin. Microbiol. Infect. 15:407–414 [DOI] [PubMed] [Google Scholar]
- 4. Balashov Y. S., Fillipova N. A. 1964. Water balance and critical temperature of the epicuticle in argasid ticks. Entomol. Obozr. 42:351–363 (In Russian.) [Google Scholar]
- 5. Barbour A. G. 1984. Isolation and cultivation of Lyme disease spirochetes. Yale J. Biol. Med. 57:521–525 [PMC free article] [PubMed] [Google Scholar]
- 6. Barbour A. G., Dai Q., Restrepo B. I., Stoenner H. G., Frank S. A. 2006. Pathogen escape from host immunity by a genome program for antigenic variation. Proc. Natl. Acad. Sci. U. S. A. 103:18290–18295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Battisti J. M., et al. 2008. Outer surface protein A protects Lyme disease spirochetes from acquired host immunity in the tick vector. Infect. Immun. 76:5228–5237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bouattour A., et al. 2010. Borrelia crocidurae infection of Ornithodoros erraticus (Lucas, 1849) ticks in Tunisia. Vector Borne Zoonotic Dis. 10:825–830 [DOI] [PubMed] [Google Scholar]
- 9. Browning T. O. 1954. Water balance in the tick Ornithodoros moubata Murray, with particular reference to the influence of carbon dioxide on the uptake and loss of water. J. Exp. Biol. 31:331–340 [Google Scholar]
- 10. Bunikis J., et al. 2004. Typing of Borrelia relapsing fever group strains. Emerg. Infect. Dis. 10:1661–1664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chesebro B., Portis J. L., Wehrly K., Nishio J. 1983. Effect of murine host genotype on MCF virus expression, latency, and leukemia cell type of leukemias induced by Friend murine leukemia helper virus. Virology 128:221–233 [DOI] [PubMed] [Google Scholar]
- 12. Cook B. 1973. The effects of repeated desiccation and rehydration on lipid and haemoglobin concentrations in fasting Ornithodoros concanensis (Acarina: Argasidae). Comp. Biochem. Physiol. A Comp. Physiol. 44:1141–1148 [DOI] [PubMed] [Google Scholar]
- 13. Dai Q., et al. 2006. Antigenic variation by Borrelia hermsii occurs through recombination between extragenic repetitive elements on linear plasmids. Mol. Microbiol. 60:1329–1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Davis G. E., Walker M. E. 1940. Ornithodorus hermsi: feeding and molting habits in relation to the acquisition and transmission of relapsing fever spirochetes. Public Health Rep. 55:492–504 [Google Scholar]
- 15. Fritz C. L., et al. 2004. Isolation and characterization of Borrelia hermsii associated with two foci of tick-borne relapsing fever in California. J. Clin. Microbiol. 42:1123–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hildebrandt A., et al. 2003. Prevalence of four species of Borrelia burgdorferi sensu lato and coinfection with Anaplasma phagocytophila in Ixodes ricinus ticks in central Germany. Eur. J. Clin. Microbiol. Infect. Dis. 22:364–367 [DOI] [PubMed] [Google Scholar]
- 17. Hinnebusch B. J., Barbour A. G., Restrepo B. I., Schwan T. G. 1998. Population structure of the relapsing fever spirochete Borrelia hermsii as indicated by polymorphism of two multigene families that encode immunogenic outer surface lipoproteins. Infect. Immun. 66:432–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hofmeister E. K., Glass G. E., Childs J. E., Persing D. H. 1999. Population dynamics of a naturally occurring heterogeneous mixture of Borrelia burgdorferi clones. Infect. Immun. 67:5709–5716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kohls G. M., Sonenshine D. E., Clifford C. M. 1965. The systematics of the subfamily Ornithodorinae (Acarina: Argasidae). II. Identification of the larvae of the Western Hemisphere and descriptions of three new species. Ann. Entomol. Soc. Am. 58:331–364 [DOI] [PubMed] [Google Scholar]
- 20. Larsson C., Andersson M., Bergström S. 2009. Current issues in relapsing fever. Curr. Opin. Infect. Dis. 22:443–449 [DOI] [PubMed] [Google Scholar]
- 21. Lees A. D. 1946. The water balance in Ixodes ricinus L. and certain other species of ticks. Parasitology 37:1–20 [DOI] [PubMed] [Google Scholar]
- 22. McCoy B. N., Raffel S. J., Lopez J. E., Schwan T. G. 2010. Bloodmeal size and spirochete acquisition of Ornithodoros hermsi (Acari: Argasidae) during feeding. J. Med. Entomol. 47:1164–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mehra R., Londono D., Sondey M., Lawson C., Cadavid D. 2009. Structure-function investigation of Vsp serotypes of the spirochete Borrelia hermsii. PLoS One 4:e7597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pettersson J., et al. 2007. Purine salvage pathways among Borrelia species. Infect. Immun. 75:3877–3884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Plasterk R. H., Simon M. I., Barbour A. G. 1985. Transposition of structural genes to an expression sequence on a linear plasmid causes antigenic variation in the bacterium Borrelia hermsii. Nature 318:257–263 [DOI] [PubMed] [Google Scholar]
- 26. Policastro P. F., Schwan T. G. 2003. Experimental infection of Ixodes scapularis larvae (Acari: Ixodidae) by immersion in low passage cultures of Borrelia burgdorferi. J. Med. Entomol. 40:364–370 [DOI] [PubMed] [Google Scholar]
- 27. Porcella S. F., et al. 2005. Variable tick protein in two genomic groups of the relapsing fever spirochete Borrelia hermsii in western North America. Infect. Immun. 73:6647–6658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Roshdy M. A., Banaja A. A., Wassef H. Y. 1982. The subgenus Persicargas (Ixodoidea: Argasidae: Argas). 34. Larval respiratory system structure and spiracle formation in pharate nymphal Argas (P.) arboreus. J. Med. Entomol. 19:665–670 [DOI] [PubMed] [Google Scholar]
- 29. Rudolph D., Knülle W. 1974. Site and mechanism of water vapour uptake from the atmosphere in ixodid ticks. Nature 249:84–85 [DOI] [PubMed] [Google Scholar]
- 30. Schwan T. G., Hinnebusch B. J. 1998. Bloodstream- versus tick-associated variants of a relapsing fever bacterium. Science 280:1938–1940 [DOI] [PubMed] [Google Scholar]
- 31. Schwan T. G., et al. 2003. Tick-borne relapsing fever caused by Borrelia hermsii, Montana. Emerg. Infect. Dis. 9:1151–1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schwan T. G., Raffel S. J., Schrumpf M. E., Porcella S. F. 2007. Diversity and distribution of Borrelia hermsii. Emerg. Infect. Dis. 13:436–442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schwan T. G., et al. 2009. Tick-borne relapsing fever and Borrelia hermsii, Los Angeles County, California, USA. Emerg. Infect. Dis. 15:1026–1031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schwartz J. J., Gazumyan A., Schwartz I. 1992. rRNA gene organization in the Lyme disease spirochete, Borrelia burgdorferi. J. Bacteriol. 174:3757–3765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stark U., Gothe R. 2001. Studies on the critical water mass, rehydration capability and potential, acute chill tolerance and supercooling point of Argas (Persicargas) walkerae (Acari: Argasidae). Onderstepoort J. Vet. Res. 68:11–20 [PubMed] [Google Scholar]
- 36. Stoenner H. G., Dodd T., Larsen C. 1982. Antigenic variation of Borrelia hermsii. J. Exp. Med. 156:1297–1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vial L., et al. 2006. Incidence of tick-borne relapsing fever in West Africa: longitudinal study. Lancet 368:37–43 [DOI] [PubMed] [Google Scholar]
- 38. Wheeler C. M. 1938. Progress of spirochaete infection in the developmental stages of the host tick, Ornithodoros Hermsi, Wheeler. Am. J. Trop. Med. Hyg. 18:413–419 [Google Scholar]
- 39. Winston P. W., Bates D. H. 1960. Saturated solutions for the control of humidity in biological research. Ecology 41:232–237 [Google Scholar]


