Abstract
OBJECTIVES
To examine whether consistent low-risk drinking is associated with lower risk of developing functional limitations among older adults.
METHODS
Data were obtained from five waves of the Health and Retirement Study. Function was assessed by questions measuring four physical abilities and five instrumental activities of daily living. Five different drinking patterns were determined using data over two consecutive survey periods.
RESULTS
Over the follow-up periods, 38.6% of older adults developed functional limitations. Consistent low-risk drinkers had lower odds of developing functional limitations compared to consistent abstainers, and the effect of consistent low-risk drinking was greater among those 50–64 years compared to those ≥65 years. Other drinking patterns were not associated with lower odds of incident functional limitation.
DISCUSSION
Consistent low-risk drinking was associated with lower odds of developing functional limitations, and this association was greater among older middle-aged adults 50–64 years of age.
Keywords: alcohol, drinking patterns, functional limitations
Introduction
Many observational studies have evaluated links between alcohol consumption and a variety of health outcomes. The beneficial effect of low to moderate alcohol use has been observed in cardiovascular disease (Corrao et al., 2000; Mukamal et al., 2010), myocardial infarction (Beulens et al., 2007; Mukamal et al., 2003), ischemic stroke (Elkind et al., 2006; Sacco et al., 1999), diabetes (Djousse et al., 2007), cognitive impairment (Mukamal et al., 2003; Stott et al., 2008), and all-cause mortality (Jackson et al., 2003; Thun et al., 1997). The preservation of independent functional ability is an important goal for many older adults, and there is a growing interest in the connection between alcohol consumption and physical and mental functioning among the older adult population. Although results from earlier studies on the association between alcohol use and functional disabilities were mixed (Reid et al., 2002), findings from more recent publications have been more consistent in suggesting the association between low to moderate alcohol use and lower risk of functional impairments among older adults (Cawthon et al., 2007; Chen & Hardy, 2009; Karlamangla et al., 2009; Lang et al., 2007; Lee et al., 2009; Maraldi et al., 2009; Sun et al., 2009; Wang et al., 2002).
A potential limitation in most studies evaluating the association of alcohol consumption and health outcomes is that the assessment of quantity and frequency of alcohol use is measured at a single time point. Studies evaluating drinking patterns have suggested that the amount of an individual’s alcohol consumption changes over time. A longitudinal, population-based study of patterns of alcohol use found that 26% of the general U.S. adult population changed their drinking patterns over a 20 year period, either by becoming abstainers or by changing their drinking and abstention status more than once (Moore et al., 2005). Another study found that 20.6% of adults aged >50 years changed their drinking patterns over a 14-year follow-up period (Platt et al., 2010).
Findings from both cross-sectional and longitudinal studies have suggested that various factors, including age, gender, ethnicity, health status, heavier alcohol use, and previous drinking problems, were associated with changes in alcohol consumption over time (Brennan et al., 2010; Eigenbrodt et al., 2001; Fillmore et al., 2003; Kerr et al., 2002; Moore et al., 2005; Platt et al., 2010). A few studies that evaluated the association of alcohol use over time with health outcomes have found that abstainers have poorer health and more serious illnesses compared to consistent moderate drinkers, and that a stable pattern of light to moderate alcohol use was associated with lowest all-cause mortality (Emberson et al., 2005; Fillmore et al., 2003; Gronbaek et al., 2004). One study compared the effect estimates of alcohol use on cardiovascular outcomes and mortality when using only baseline alcohol consumption as predictor and when using longitudinal patterns of alcohol consumption over a 20-year period as predictor. Compared to the baseline alcohol consumption variable, the longitudinal alcohol consumption variable decreased risk of cardiovascular outcomes and mortality among those who were nondrinkers compared to light alcohol drinkers and increased the risks of these outcomes among those who were regular heavy drinkers compared to light drinkers (Emberson et al., 2005). This finding suggested the importance of considering drinking patterns over time to more accurately evaluate the associations of alcohol use with variety of health outcomes.
To address the association of longitudinal patterns of drinking and incident functional limitation among older adults, we examined data from U.S. adults 50 years and older who participated in the Health and Retirement Study (HRS). We hypothesized that consistent pattern of low-risk drinking is associated with lower risk of developing functional limitations among older adults.
Methods
The HRS is a biennial survey of a nationally representative sample of all community-dwelling adults in the contiguous United States. We examined drinking patterns and development of functional limitations over two 4-year periods using data from 5 waves of the HRS (1998–2006). Alcohol consumption in 1998 and 2000 was used as a predictor for incident functional limitation between 2000 and 2002 (first period) and alcohol consumption in 2002 to 2004 was used as a predictor for incident functional limitation between 2004 and 2006 (second period).
Study Sample
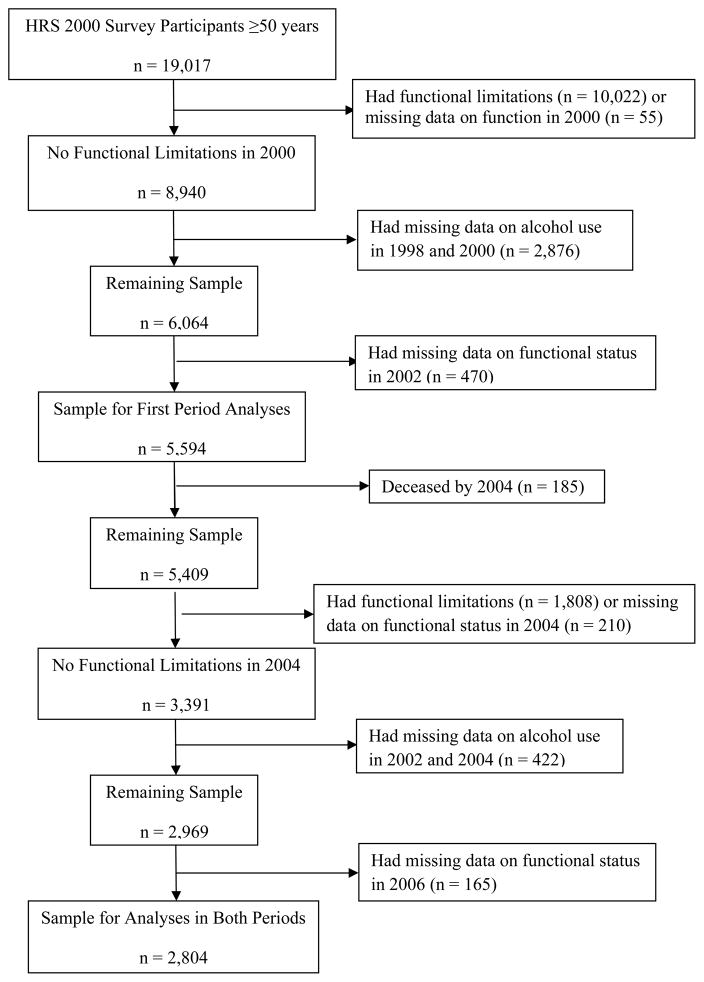
For the 2000 wave of the HRS, 19,017 community-dwelling adults 50 years and older were surveyed primarily through telephone interviews, and the overall response rate was 86.8% (http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf). The analytic sample for this study included 5,594 participants in the 2000 wave who had no functional limitations in 2000, had data on alcohol use in 1998 and 2000, and had data on functional status in 2002 (Figure 1). Data from these individuals contributed to the first period analyses. Of these participants, 2,969 individuals remained free of functional disability in 2004, and 2,804 of them had data on functional status in 2006, and their data contributed to the second period analyses. These two period samples were merged for the final regression analyses.
Figure 1.
Flow diagram describing study sample who were ≥50 years in the HRS 2000 survey.
Study Variables
Outcome: Development of Functional Limitations
The outcome for this study was development of functional limitations in 2002 or 2006. Function was assessed by the ability to complete nine activities consisting of four questions measuring physical abilities (e.g. walking several blocks, climbing several flights of stairs, pushing or pulling heavy objects, and lifting 10 pounds) and five questions measuring ability to perform instrumental activities of daily living (IADLs) (e.g. using the telephone, preparing meals, shopping, taking medications, and managing money). Individuals were considered to have functional limitation if they had difficulties performing any of the nine tasks.
Main Predictor: Drinking Patterns
HRS gathered alcohol use information by first asking the participants whether they ever drank any alcoholic beverages. Those who did were then asked how many days per week they consumed alcohol, and how many drinks they consumed on days they drank in the last 3 months. Binge drinking was assessed by asking how many days they consumed ≥4 drinks on one occasion in the last 3 months. Average weekly alcohol use was calculated by multiplying the number of days per week and number of alcoholic drinks per drinking day. Three drinking risk categories were determined based on recommendation by the National Institute of Alcohol Abuse and Alcoholism, which defined the low-risk drinking limit as 1) ≤14 drinks/week for men <65 years, 2) ≤7 drinks/week for women and men ≥65 years, and 3) no binge drinking for men and women of all ages. Subjects who never drank any alcoholic beverages or who had no alcohol use in past 3 months were classified as abstainers; subjects who drank below the drinking limit were classified as low-risk drinkers; subjects who drank above the drinking limit were classified as high risk drinkers. Drinking patterns for year 2000 were determined by the drinking risk categories in 1998 and 2000, and drinking patterns for year 2004 were determined by drinking risk categories in 2002 and 2004. The five drinking patterns were: 1) consistent abstainers (abstainer for both periods), 2) consistent low-risk drinkers (low-risk for both periods), 3) consistent high risk drinkers (high risk for both periods), 4) recent quitters (drinker in first period and abstainer in second period), and 5) other mixed patterns (different drinking risk categories in the two periods). These drinking patterns were defined to be mutually exclusive.
Study Covariates
Other covariates that were included in the analyses were selected based on known associations with alcohol consumption and impairment of functional abilities. Sociodemographic variables included age, gender, race/ethnicity (non-Hispanic white vs. Hispanic or non-white), living situation (coupled or partnered vs. not coupled or partnered), education (less than high school vs. high school or more), annual household income (less than median of $18,000 vs. more than $18,000), and employment status (working vs. not working). Health-related variables included self-rated health (fair or poor vs. good or very good or excellent), current smoker (yes vs. no), and nine possible medical conditions reported by the subjects including hypertension, diabetes, cancer, chronic lung disease, heart disease, congestive heart failure, stroke, arthritis, and psychiatric conditions (yes vs. no for each comorbidity). Medical conditions were categorized into 0, 1, 2, or ≥3 comorbidities.
Statistical Analyses
Descriptive statistics of sociodemographic and health-related variables were calculated by drinking patterns using means and standard deviations for continuous variables, and frequencies and weighted percentages for categorical variables. Percentages were weighted by the HRS respondent weights. These variables were compared by drinking patterns using analysis of variance for continuous variables and chi-square tests for categorical variables.
The random-effects multivariate logistic regression method was used to study association of drinking patterns with the development of functional limitations over the two 4-year study periods (drinking patterns in 1998–2000 as the predictor for incident functional limitation in 2002 and drinking patterns in 2002–2004 as the predictor for incident functional limitation in 2006). With this longitudinal method, we allowed some covariates, such as age, self-rated health status, smoking status, and number of chronic conditions, to vary according to the answers provided to the different survey periods to account for possible changes in the value of these variables over time within an individual. Unweighted data were used to generate results from the regression analyses. To evaluate for effect-measure modification (Rothman, Greenland, & Lash, 2008), which examined whether the effect of alcohol use differed between different levels of certain covariates, we tested interactions between drinking patterns with gender, self-rated health status, and age (50–64 years and ≥65 years). These covariates were chosen because several studies have suggested that the magnitude of effect of alcohol use on mortality and functional disabilities differed by gender and self-rated health status (Karlamangla et al., 2009; Sun et al., 2009; Wang et al., 2002). Also, some studies on alcohol use and functional disabilities included individuals between 50–64 years of age (Chen & Hardy, 2009; Karlamangla et al., 2009; Lee et al., 2009; Moore et al., 2003; Perreira & Sloan, 2002), while other studies included only individuals ≥65 years of age (Cawthon et al., 2007; Lang et al., 2007; Maraldi et al., 2009; Sun et al., 2009). Therefore, we decided to test whether the effect of alcohol consumption differed between those 50–64 years and those ≥65 years. Stratified analyses were performed if significant interactions were detected. The stata command XTLOGIT was used to implement the random-effects logistic regression analyses. All analyses were conducted using SAS version 9.1 and Stata/SE version 10.1. The research protocol received ethical review and approval from the Veterans Administration Greater Los Angeles Healthcare System Institutional Review Board.
Results
Sample Drinking Patterns
Close to half of the sample were consistent abstainers (48.3%), 20.5% were consistent low-risk drinkers, 14.6% were consistent high risk drinkers, 4.3% were recent quitters, and 12.4% were mixed pattern drinkers (Table 1).
Table 1.
Baseline Characteristics of Study Sample by Drinking Patterns.
| Drinking Patterns (n = 5,594) | |||||
|---|---|---|---|---|---|
| Consistent Abstainers (n = 2,916) | Consistent Low-risk (n = 1,059) | Consistent High Risk (n = 745) | Recent Quitters (n = 246) | Other Mixed Patterns (n = 628) | |
| Age in years, mean (SD) | 66.4 (9.2) | 65.1 (8.7) | 63.4 (8.2) | 66.8 (9.4) | 64.0 (8.2) |
|
| |||||
| Gender, n (%) | |||||
| Male | 1235 (44.8) | 587 (57.8) | 548 (76.5) | 135 (57.2) | 402 (66.1) |
| Female | 1681 (55.2) | 472 (42.2) | 197 (23.5) | 111 (42.8) | 226 (33.9) |
|
| |||||
| Race/Ethnicity, n (%) (n=5,857) | |||||
| Non-Hispanic White | 2139 (79.1) | 957 (93.2) | 666 (90.1) | 197 (80.4) | 519 (86.5) |
| Hispanic/Non-white | 776 (20.9) | 102 (6.8) | 79 (9.9) | 49 (19.6) | 109 (13.5) |
|
| |||||
| Living situation, n (%) | |||||
| Not coupled or partnered | 900 (34.1) | 203 (21.0) | 133 (22.6) | 59 (27.7) | 147 (26.0) |
| Coupled or partnered | 2016 (65.9) | 856 (79.0) | 612 (77.4) | 187 (72.3) | 481 (74.0) |
|
| |||||
| Education, n (%) (n=5,857) | |||||
| Less than high school | 854 (26.0) | 95 (7.4) | 89 (9.4) | 46 (17.0) | 103 (13.7) |
| High school or more | 2062 (74.0) | 964 (92.6) | 656 (90.6) | 200 (83.0) | 525 (86.3) |
|
| |||||
| Annual Household Income, n (%) | |||||
| ≤$18,000 (Median) | 1590 (51.8) | 420 (36.3) | 287 (34.1) | 120 (42.4) | 233 (32.9) |
| >$18,000 | 1326 (48.2) | 639 (63.7) | 458 (65.9) | 126 (57.6) | 395 (67.1) |
|
| |||||
| Employment, n (%) | |||||
| Working | 1152 (44.0) | 474 (51.1) | 379 (57.7) | 101 (50.5) | 323 (57.7) |
| Not working | 1764 (56.0) | 585 (48.9) | 366 (42.3) | 145 (49.5) | 305 (42.3) |
|
| |||||
| Self-rated health, n (%) (n=5,854) | |||||
| Fair/Poor | 378 (11.8) | 50 (3.9) | 47 (6.0) | 26 (12.4) | 51 (7.5) |
| Good/Very good/Excellent | 2537 (88.2) | 1009 (96.1) | 698 (94.0) | 220 (87.6) | 577 (92.5) |
|
| |||||
| Number of comorbidities, n (%) | |||||
| 0 | 738 (28.6) | 291 (30.8) | 207 (30.7) | 64 (28.3) | 161 (29.2) |
| 1 | 960 (32.2) | 396 (36.9) | 280 (37.9) | 77 (31.1) | 225 (36.9) |
| 2 | 712 (23.2) | 251 (22.0) | 170 (20.7) | 63 (26.1) | 150 (21.4) |
| ≥3 | 506 (15.9) | 121 (10.2) | 88 (10.7) | 42 (14.5) | 92 (12.4) |
| Current smoker, n (%) | 367 (13.3) | 94 (8.8) | 172 (23.9) | 32 (11.8) | 110 (19.0) |
Incident Functional Limitation
Over the follow-up periods, 38.6% of the older adults developed functional limitations. Among those with functional limitations, 83.4% had limitations due only to inability to perform at least one of the four physical tasks, 6.7% had limitations due only to performing at least one of the IADLs, and 9.9% had difficulties in both physical tasks and IADLs. The most common deficit was the inability to push or pull heavy objects.
Associations of Drinking Patterns and Development of Functional Limitations
In the random-effects multivariate logistic regression models, adjusted for the relevant sociodemographic and health-related variables, individuals who were consistent low-risk drinkers had 31% lower odds of developing functional limitations compared to consistent abstainers. The other drinking patterns, especially recent quitters, were not associated with lower odds of incident functional limitation compared to consistent abstainers (Table 2).
Table 2.
Associations Between Drinking Patterns and Development of Functional Limitations Among the Entire Samplea
| Unadjusted OR (95% CI) | p-value | Adjusted ORb (95% CI) | p-value | ||
|---|---|---|---|---|---|
| Drinking Patterns | |||||
| Consistent abstainers | 1.0 | 1.0 | |||
| Consistent low-risk | 0.48 (0.39–0.58) | <.001 | 0.69 (0.57–0.83) | <.001 | |
| Consistent high risk | 0.56 (0.45–0.69) | <.001 | 0.90 (0.73–1.11) | 0.33 | |
| Recent quitters | 0.99 (0.70–1.39) | 0.95 | 1.14 (0.81–1.59) | 0.45 | |
| Other mixed patterns | 0.59 (0.47–0.74) | <.001 | 0.86 (0.69–1.07) | 0.18 | |
Analyses included 8740 observations.
Adjusted for age, gender, marital status, race/ethnicity, education, employment status, income, self-rated health, smoking status, and chronic conditions.
In examining for effect-measure modification, the results suggested that the benefit of consistent low-risk drinking had a larger protective effect for adults 50–64 years compared with adults ≥65 years of age (Pinteraction=0.03). The interactions of drinking patterns with gender (Pinteraction=0.72) and self-rated health status (Pinteraction=0.98) were not significant. Because of these findings, we conducted additional multivariate analyses stratified by age (50–64 years and ≥65 years). Individuals 50–64 years who were consistent low-risk drinkers had a 51% decrease in odds of developing functional limitations compared to consistent abstainers, whereas adults ≥65 years who were consistent low-risk drinkers had a 24% decrease in odds of developing functional limitations compared to consistent abstainers (Table 3). Again, other drinking patterns were not associated with decrease in odds of incident functional limitation compared to consistent abstainers. Among adults ≥65 years of age, the effect estimate for recent quitters suggested a non-significant but possible increase in odds of incident functional limitation compared to consistent abstainers.
Table 3.
Associations Between Drinking Patterns and Development of Functional Limitations, Stratified by Agea
| Adults 50–64 yearsb | Adults ≥65 yearsc | |||
|---|---|---|---|---|
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Drinking Patterns | ||||
| Consistent abstainers | 1.0 | 1.0 | ||
| Consistent low-risk | 0.49 (0.34–0.73) | <.001 | 0.76 (0.61–0.95) | 0.02 |
| Consistent high risk | 1.05 (0.74–1.50) | 0.77 | 0.79 (0.62–1.03) | 0.09 |
| Recent quitters | 0.85 (0.44–1.65) | 0.64 | 1.25 (0.84–1.86) | 0.27 |
| Mixed patterns | 0.76 (0.51–1.13) | 0.17 | 0.92 (0.70–1.19) | 0.51 |
Random-effects logistic regressions adjusted for age, gender, marital status, race/ethnicity, education, employment status, income, self-rated health, smoking status, and chronic conditions.
Analysis included 3159 observations.
Analysis included 5581 observations.
Discussion
In a population-based sample of U.S. adults 50 years and older who had no functional limitations at baseline, this study found that slightly less than 1/2 of the individuals were consistent abstainers and approximately 1/5 of the individuals were consistent low-risk drinkers. Compared to consistent abstainers, consistent low-risk drinking was associated with lower odds of developing functional limitations. The association of consistent low-risk drinking and lower odds of functional limitations was found to be greater among adults 50–64 years of age than among adults older than 65 years of age.
Among the older drinkers in this study, 16.7% were either recent quitters or mixed pattern drinkers over a 2-year span, indicating that a significant number of older drinkers did not have stable drinking patterns. This finding of changes in alcohol consumption over time was in accordance with other studies that found only 54.3% of older adults remained in the same drinking category over a 2-year span (Chen & Hardy, 2009), and that changes in drinking behavior do occur after the age of 50 where 30% of the older adults were sporadic drinkers, 20.7% steady drinkers, 18.4% decreasing drinkers, and 2.2% increasing drinkers (Platt et al., 2010). Although the exact mechanisms underlying the beneficial effects of alcohol are unclear, the benefits through potential biological mechanisms, such as decreased platelet aggregation, improved endothelial function, and increased high-density lipoprotein cholesterol (de Jong et al., 2008; Mann & Folts, 2004), are likely associated with longer term rather than short term exposure. Therefore, taking into account alcohol patterns over time may be important to capture individuals who are more likely to accrue the benefits from light to moderate alcohol use.
Certain sociodemographic and health-related factors were found to modify the beneficial effects of light to moderate alcohol consumption. A study found that moderate alcohol use was associated with lower all-cause mortality among Chinese older adults, but the protective effect was more pronounced among men with poorer health status (Sun et al., 2009). Other studies have found that the beneficial effect of alcohol use was stronger in women and those with good or better self-rated health (Karlamangla et al., 2009; Maraldi et al., 2009). We did not find significant interactions between drinking patterns and gender or self-rated health status in our study. However, less than 10% of our sample had fair or poor self-rated health at baseline, and the small sample size in that strata could have limited our ability to detect modification by health status. We did find differences in the magnitude of benefit by age, where consistent low-risk drinkers 50–64 years had more benefit than consistent low-risk drinkers ≥65 years of age. The difference in the effect estimates from the stratified analyses could potentially arise because different cutoffs were used to determine drinking limits for male drinkers 50–64 years and male drinkers ≥65 years of age. Therefore, additional analyses were performed using the same cutoff for drinking limit for all older adults in the sample (low-risk drinking defined as ≤14 drinks per week and no binge drinking), and the results obtained were similar to our main finding. Therefore, this suggested that difference in the magnitude of the beneficial effect of consistent low-risk drinking was not substantially affected by the choice of cutoff for drinking limits. There are some other possible explanations. Studies have found that older adults with poorer health have steeper decline in alcohol use, and having a history of problem or heavy drinking has been associated with less stable and larger changes in alcohol use over time (Brennan et al., 2010; Kerr et al., 2002; Platt et al., 2010). Another study found that 23–38% of heavy drinkers became light to moderate drinkers over a 14–18 year period (Eigenbrodt et al., 2001). Therefore, it is possible that older adults who were classified as consistent low-risk drinkers in this study may have used more alcohol or were problem drinkers when they were younger and may have developed functional limitations due to effects from earlier heavier alcohol use. Also, as older adults age, they have increased sensitivity to the negative effects of alcohol due to age-related physiological changes and increased number of comorbidities and medications use (Moore et al., 2006; Moore et al., 1999; Moore et al., 2007; Vestal et al., 1977), which may diminish the beneficial effects of low-risk alcohol use. These factors may lessen the beneficial effects of consistent low-risk drinking among those ≥65 years of age compared to those 50–64 years of age. Several studies have included adults <65 years in their study sample but did not assess any potential differences between those younger and older than 65 years of age (Chen & Hardy, 2009; Karlamangla et al., 2009; Lee et al., 2009; Moore et al., 2003; Perreira & Sloan, 2002). Future studies should confirm and evaluate other factors that may modify the effects of alcohol consumption on variety of health outcomes.
There are some limitations to this study. Similar to most other observational studies of the association between alcohol consumption and functional disabilities, both alcohol use and functional measures were obtained from self-reports. Inaccurate reporting of alcohol consumption may lead to misclassification of drinking patterns and missing data on alcohol consumption may result in biased estimates. Also, those individuals who may have stopped alcohol use before the survey may be classified as abstainers and not recent quitters, which may also bias the results. Functional limitations were evaluated at discrete time points and development of impairments during the interval periods could not be ascertained, and missing data on functional status may potentially affect the results if participants who developed functional limitations did not participate in subsequent surveys. While this study examined drinking patterns at two time points over a two-year period, assessing alcohol consumption over a longer period of time may provide an even more accurate picture of actual drinking patterns and information about their effects on function. Lastly, individuals in this sample were community-dwelling U.S. older adults who were mostly non-Hispanic white, and results from this study may not be applicable to institutionalized individuals or to older adults who are of different racial or ethnic backgrounds and those in worse health.
In conclusion, we found that consistent low-risk drinking among older adults was associated with lower odds of developing functional limitations compared to consistent abstainers, particularly for older middle-aged adults 50–64 years of age. Almost 20% of older adults changed their drinking patterns over a 2-year span, and the association between alcohol use and functional limitations was not found among those with unstable drinking patterns, especially recent quitters ≥65 years of age, and among consistent high risk drinkers. These findings suggested the importance of evaluating changes in alcohol consumption over time when looking for association of alcohol use and health outcomes. These results add to the growing literature on the effect of alcohol consumption and function, and provide the first evidence of potential association of consistent low-risk drinking pattern and maintaining function among older community-dwelling adults.
Acknowledgments
Funding sources: Special Fellowship in Advanced Geriatrics, VA Greater Los Angeles Healthcare System; and the National Institutes of Health, National Institute on Alcoholism and Alcohol Abuse (AA013937 and AA15957).
References
- Beulens JW, Rimm EB, Ascherio A, Spiegelman D, Hendriks HF, Mukamal KJ. Alcohol consumption and risk for coronary heart disease among men with hypertension. Ann Intern Med. 2007;146(1):10–19. doi: 10.7326/0003-4819-146-1-200701020-00004. [DOI] [PubMed] [Google Scholar]
- Brennan PL, Schutte KK, Moos RH. Retired status and older adults’ 10-year drinking trajectories. J Stud Alcohol Drugs. 2010;71(2):165–168. doi: 10.15288/jsad.2010.71.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthon PM, Fink HA, Barrett-Connor E, Cauley JA, Dam TT, Lewis CE, et al. Alcohol use, physical performance, and functional limitations in older men. J Am Geriatr Soc. 2007;55(2):212–220. doi: 10.1111/j.1532-5415.2007.01062.x. [DOI] [PubMed] [Google Scholar]
- Chen LY, Hardy CL. Alcohol consumption and health status in older adults: a longitudinal analysis. J Aging Health. 2009;21(6):824–847. doi: 10.1177/0898264309340688. [DOI] [PubMed] [Google Scholar]
- Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K. Alcohol and coronary heart disease: a meta-analysis. Addiction. 2000;95(10):1505–1523. doi: 10.1046/j.1360-0443.2000.951015056.x. [DOI] [PubMed] [Google Scholar]
- de Jong HJ, de Goede J, Oude Griep LM, Geleijnse JM. Alcohol consumption and blood lipids in elderly coronary patients. Metabolism. 2008;57(9):1286–1292. doi: 10.1016/j.metabol.2008.04.025. [DOI] [PubMed] [Google Scholar]
- Djousse L, Biggs ML, Mukamal KJ, Siscovick DS. Alcohol consumption and type 2 diabetes among older adults: the Cardiovascular Health Study. Obesity (Silver Spring) 2007;15(7):1758–1765. doi: 10.1038/oby.2007.209. [DOI] [PubMed] [Google Scholar]
- Eigenbrodt ML, Mosley TH, Jr, Hutchinson RG, Watson RL, Chambless LE, Szklo M. Alcohol consumption with age: a cross-sectional and longitudinal study of the Atherosclerosis Risk in Communities (ARIC) study, 1987–1995. Am J Epidemiol. 2001;153(11):1102–1111. doi: 10.1093/aje/153.11.1102. [DOI] [PubMed] [Google Scholar]
- Elkind MS, Sciacca R, Boden-Albala B, Rundek T, Paik MC, Sacco RL. Moderate alcohol consumption reduces risk of ischemic stroke: the Northern Manhattan Study. Stroke. 2006;37(1):13–19. doi: 10.1161/01.STR.0000195048.86810.5b. [DOI] [PubMed] [Google Scholar]
- Emberson JR, Shaper AG, Wannamethee SG, Morris RW, Whincup PH. Alcohol intake in middle age and risk of cardiovascular disease and mortality: accounting for intake variation over time. Am J Epidemiol. 2005;161(9):856–863. doi: 10.1093/aje/kwi111. [DOI] [PubMed] [Google Scholar]
- Fillmore KM, Kerr WC, Bostrom A. Changes in drinking status, serious illness and mortality. J Stud Alcohol. 2003;64(2):278–285. doi: 10.15288/jsa.2003.64.278. [DOI] [PubMed] [Google Scholar]
- Gronbaek M, Johansen D, Becker U, Hein HO, Schnohr P, Jensen G, et al. Changes in alcohol intake and mortality: a longitudinal population-based study. Epidemiology. 2004;15(2):222–228. doi: 10.1097/01.ede.0000112219.01955.56. [DOI] [PubMed] [Google Scholar]
- Jackson VA, Sesso HD, Buring JE, Gaziano JM. Alcohol consumption and mortality in men with preexisting cerebrovascular disease. Arch Intern Med. 2003;163(10):1189–1193. doi: 10.1001/archinte.163.10.1189. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Sarkisian CA, Kado DM, Dedes H, Liao DH, Kim S, et al. Light to moderate alcohol consumption and disability: variable benefits by health status. Am J Epidemiol. 2009;169(1):96–104. doi: 10.1093/aje/kwn294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Fillmore KM, Bostrom A. Stability of alcohol consumption over time: evidence from three longitudinal surveys from the United States. J Stud Alcohol. 2002;63(3):325–333. doi: 10.15288/jsa.2002.63.325. [DOI] [PubMed] [Google Scholar]
- Lang I, Guralnik J, Wallace RB, Melzer D. What level of alcohol consumption is hazardous for older people? Functioning and mortality in U.S. and English national cohorts. J Am Geriatr Soc. 2007;55(1):49–57. doi: 10.1111/j.1532-5415.2006.01007.x. [DOI] [PubMed] [Google Scholar]
- Lee SJ, Sudore RL, Williams BA, Lindquist K, Chen HL, Covinsky KE. Functional limitations, socioeconomic status, and all-cause mortality in moderate alcohol drinkers. J Am Geriatr Soc. 2009;57(6):955–962. doi: 10.1111/j.1532-5415.2009.02184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann LB, Folts JD. Effects of ethanol and other constituents of alcoholic beverages on coronary heart disease: a review. Pathophysiology. 2004;10(2):105–112. doi: 10.1016/j.pathophys.2003.10.011. [DOI] [PubMed] [Google Scholar]
- Maraldi C, Harris TB, Newman AB, Kritchevsky SB, Pahor M, Koster A, et al. Moderate alcohol intake and risk of functional decline: the Health, Aging, and Body Composition study. J Am Geriatr Soc. 2009;57(10):1767–1775. doi: 10.1111/j.1532-5415.2009.02479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Endo JO, Carter MK. Is there a relationship between excessive drinking and functional impairment in older persons? J Am Geriatr Soc. 2003;51(1):44–49. doi: 10.1034/j.1601-5215.2002.51008.x. [DOI] [PubMed] [Google Scholar]
- Moore AA, Giuli L, Gould R, Hu P, Zhou K, Reuben D, et al. Alcohol use, comorbidity, and mortality. J Am Geriatr Soc. 2006;54(5):757–762. doi: 10.1111/j.1532-5415.2006.00728.x. [DOI] [PubMed] [Google Scholar]
- Moore AA, Gould R, Reuben DB, Greendale GA, Carter MK, Zhou K, et al. Longitudinal patterns and predictors of alcohol consumption in the United States. Am J Public Health. 2005;95(3):458–465. doi: 10.2105/AJPH.2003.019471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Morton SC, Beck JC, Hays RD, Oishi SM, Partridge JM, et al. A new paradigm for alcohol use in older persons. Medical Care. 1999;37(2):165–179. doi: 10.1097/00005650-199902000-00007. [DOI] [PubMed] [Google Scholar]
- Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. Am J Geriatr Pharmacother. 2007;5(1):64–74. doi: 10.1016/j.amjopharm.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am CollCardiol. 55(13):1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am Coll Cardiol. 2010;55(13):1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamal KJ, Conigrave KM, Mittleman MA, Camargo CA, Jr, Stampfer MJ, Willett WC, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348(2):109–118. doi: 10.1056/NEJMoa022095. [DOI] [PubMed] [Google Scholar]
- Mukamal KJ, Kuller LH, Fitzpatrick AL, Longstreth WT, Jr, Mittleman MA, Siscovick DS. Prospective study of alcohol consumption and risk of dementia in older adults. JAMA. 2003;289(11):1405–1413. doi: 10.1001/jama.289.11.1405. [DOI] [PubMed] [Google Scholar]
- Perreira KM, Sloan FA. Excess alcohol consumption and health outcomes:a 6-year follow-up of men over age 50 from the health and retirement study. Addiction. 2002;97(3):301–310. doi: 10.1046/j.1360-0443.2002.00067.x. [DOI] [PubMed] [Google Scholar]
- Platt A, Sloan FA, Costanzo P. Alcohol-consumption trajectories and associated characteristics among adults older than age 50. J Stud Alcohol Drugs. 2010;71(2):169–179. doi: 10.15288/jsad.2010.71.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid MC, Boutros NN, O’Connor PG, Cadariu A, Concato J. The health-related effects of alcohol use in older persons: a systematic review. Subst Abus. 2002;23(3):149–164. doi: 10.1080/08897070209511485. [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- Sacco RL, Elkind M, Boden-Albala B, Lin IF, Kargman DE, Hauser WA, et al. The protective effect of moderate alcohol consumption on ischemic stroke. JAMA. 1999;281(1):53–60. doi: 10.1001/jama.281.1.53. [DOI] [PubMed] [Google Scholar]
- Stott DJ, Falconer A, Kerr GD, Murray HM, Trompet S, Westendorp RG, et al. Does low to moderate alcohol intake protect against cognitive decline in older people? J Am Geriatr Soc. 2008;56(12):2217–2224. doi: 10.1111/j.1532-5415.2008.02007.x. [DOI] [PubMed] [Google Scholar]
- Sun W, Schooling CM, Chan WM, Ho KS, Lam TH, Leung GM. Moderate alcohol use, health status, and mortality in a prospective Chinese elderly cohort. Ann Epidemiol. 2009;19(6):396–403. doi: 10.1016/j.annepidem.2009.01.011. [DOI] [PubMed] [Google Scholar]
- Thun MJ, Peto R, Lopez AD, Monaco JH, Henley SJ, Heath CW, Jr, et al. Alcohol consumption and mortality among middle-aged and elderly U.S. adults. N Engl J Med. 1997;337(24):1705–1714. doi: 10.1056/NEJM199712113372401. [DOI] [PubMed] [Google Scholar]
- Vestal RE, McGuire EA, Tobin JD, Andres R, Norris AH, Mezey E. Aging and ethanol metabolism. Clin Pharmacol Ther. 1977;21(3):343–354. doi: 10.1002/cpt1977213343. [DOI] [PubMed] [Google Scholar]
- Wang L, van Belle G, Kukull WB, Larson EB. Predictors of functional change: a longitudinal study of nondemented people aged 65 and older. J Am Geriatr Soc. 2002;50(9):1525–1534. doi: 10.1046/j.1532-5415.2002.50408.x. [DOI] [PubMed] [Google Scholar]