Abstract
Purpose/Background:
Specific movement patterns have been identified as influential in ACL injury; however several key kinematic variables that might be predictive of future performance have not been fully investigated. The purpose of this research was to: 1) determine if subjects with ACL reconstruction display different displacement, velocity, and time to peak ground reaction force (GRF) during cutting activities than healthy subjects, 2) observe if subjects with visual disruption display differences in these variables, and 3) determine if visual disruption alters these variables in subjects with ACL reconstruction relative to healthy subjects.
Methods:
Seventeen healthy female subjects and 17 female subjects with unilateral ACL reconstruction (ACLR) performed 40 trials of a cutting movement during which knee position was measured via a 3D electromagnetic system. Visual conditions were randomized to disrupt vision for 1 second as the subject began the cutting movement, or allow full vision for movement duration. Independent variables were lead/push off leg (ACLR limb or healthy non-dominant limb) and vision (disrupted or full). 2-way ANOVAs were utilized to determine differences between knee kinematics using dependent variables of displacement (m), absolute velocity (m/sec), and time to reach peak GRF (% of cut).
Results:
Knee displacement was significantly less for ACLR (.76±.11; .75±.16) than non-dominant (.85±.08; .87±.12). Knee velocity was significantly slower for ACLR (.81±.14; .84±.16) than non-dominant (.92±.11; .97±.14). A significant interaction was noted for displacement and average velocity (p<.05). Time to reach peak GRF was significantly longer for ACLR (79.41±2.28) than non-dominant (76.65±4.41).
Conclusions:
Subjects with ACLR displayed less knee displacement, slower velocity, and an increased time to reach peak GRF relative to healthy subjects' non-dominant knee. Visual disruption appeared to have some effect on movement, as noted by interaction effects. These movement adjustments may be indicative of an altered motor program that allows for successful and safe task completion while reducing the forces and load on the knee.
Level of Evidence: Level 2
Keywords: ACL reconstruction, Female, Kinematics, Lower extremity, Movement patterns
INTRODUCTION
Non-contact ACL injuries frequently occur in females. Females participating in sports that include pivoting and jumping maneuvers suffer 4-to-6-times greater rates of ACL injury than their male counterparts.1 Many studies have investigated why female athletes incur a disproportionate number of ACL injuries. Much of the literature has focused on neuromuscular and biomechanical factors. Increasing evidence suggests that poor or abnormal neuromuscular control of lower extremity biomechanics, especially during athletic maneuvers such as cutting and landing, is a major contributor to the mechanism of non-contact ACL injury.2,3 The ACL may experience potentially dangerous forces during landing and twisting if the muscles controlling the knee do not sufficiently dissipate the forces and torques.
Known biomechanical and neuromuscular risk factors include the following for females: greater knee valgus angles and moments during cutting, landing, and squatting tasks,4,5 decreased knee flexion angles and knee flexion stiffness6 during cutting tasks; and greater hip adduction angles during a variety of activities.7,8 Other important findings include that there is an association between hip transverse and frontal plane angles and knee valgus moments during cutting tasks4,9 and that knee frontal and sagittal plane moments at both slow and fast speeds are influenced by the ability to preplan movement as opposed to making an unanticipated cutting maneuver.10,11
Hiemstra et al., Mackey et al., and Mattacola et al. demonstrate that ACL reconstructed subjects produced significantly less extension and/or hamstring torque on their reconstructed leg than their uninvolved leg even up to 18 months post-surgery.12,22,42 Even greater knee extension and hamstring strength deficits have been noted when the ACLR knee is compared to the knees of uninjured peers rather than their non-surgical limb.12 The greater difference between the uninjured control group and the subjects with ACL reconstruction suggests a negative effect of the surgery on the contralateral limb or perhaps the presence of a previous deficit, thus implying that it should not be used as the only comparison limb.12,13 Paterno, Ford, Myer, Heyl, and Hewett14 support the existence of limb asymmetries in the lower extremities of ACLR patients during landing and jumping two years following ACL reconstruction.
Okuda et al. and Ferber et al. also suggest that proprioceptive dysfunction may occur secondary to ACL injury and reconstruction along with disruption and/or changes in movement patterns during gait and other simple activities.15,20 When athletes move their lower extremities, they are constantly interacting with their environment, often with large resultant impact forces. The central nervous system modulates and controls movement with input from receptors and vision. If there is a mismatch between what the athlete anticipates and how they react, the potential for injury increases. Vision is expected to play a large role in the ability to adapt to various environments; however this may not be the case. Research suggests that continual visual input to complete tasks successfully may not be necessary; especially when falls or movements are self-initiated.17 Unexpected falls display different muscle activation patterns and ground reaction forces (GRF). It appears that having an internal representation of the task requirements allows subjects to respond similarly to the task as if vision was present.17
The intent of this current investigation was to fill a gap in the literature regarding reliance on sensorimotor and visualmotor systems for movement of subjects with ACL reconstruction performing an athletic, functional-type activity. Given that athletes rely not only on the somatosensory system to provide feedback to stabilize their system, but also upon their visual and vestibular systems, it is important to study what would happen if one of these systems were not allowed to have an influence. The authors of the current study are unaware of any research that attempts to mimic an athletic situation while inducing a temporary loss of vision in subjects with ACL reconstruction. Requiring subjects to incur a distraction, such as catching a ball, just prior to movement and move into an unplanned direction while denying vision during a certain phase of movement should produce different and perhaps faulty movement patterns in those with ACL reconstruction compared to healthy subjects. The purpose of this research was to 1) determine if subjects with ACL reconstruction display different knee displacements, velocities, and time to peak GRF during cutting activities than healthy subjects, 2) observe if subjects with visual disruption display differences in these variables than with vision available, and 3) determine if visual deprivation alters these same variables in subjects with ACL reconstruction more significantly than in healthy subjects. Additionally, limb to limb comparisons will be completed within the ACLR group and healthy group to determine whether asymmetries exist between surgical and non-surgical or dominant and non-dominant extremities, respectively.
METHODS
Subjects
Thirty-four female volunteer subjects between the ages of 18 and 45 years, 17 subjects with unilateral ACL reconstructions and 17 control subjects with no recent history of knee problems were recruited for this study. Subjects were recruited from the University of Minnesota and metropolitan area athletic performance training centers. This age range was utilized to enhance subject recruitment, keeping in mind that differences may be inherent within this age group. However, only two of the subjects were between the ages of 35 and 45. These subjects demonstrated equivalent activity levels as the younger subjects. Inclusion criteria required that subjects with ACL reconstruction met the following: (a) diagnosis of complete ACL rupture, with no severe or complex meniscus or collateral ligament damage or continued knee dysfunction; (b) subsequent unilateral ACL reconstruction (average duration post-operatively was 4.6 years); (c) female, age 18-45; (d) no history of visual, vestibular, or neurological problems; (e) no knee pain, effusion (within 2 cm measured at the joint line as compared to the opposite side was considered acceptable18) or back pain that required physician care at the time of measurement; and (f) successful completion of functional tests to ensure they could complete the required experimental task (85% or greater mean limb symmetry). Functional tests included a one-legged triple hop test for distance and a one-legged crossover hop for distance.19 These tests were only completed by the subjects in the ACLR group to ensure they could complete the tasks required during the study and were not used in any analysis. Each knee was also evaluated for swelling and range of motion, tibiofemoral and patellofemoral crepitus, and for laxity using the pivot shift test and the KT-1000 test. Exclusion criteria included the following: swelling of the post surgical knee greater than 2 cm as measured at the joint line, positive pivot shift test, side-to-side difference of 3 mm or more between the injured and uninjured knee as measured by the KT-1000 Arthrometer, and less than 85% limb symmetry as measured by hop tests.
Healthy subjects were included if they had no history of vestibular, visual, or neurological problems, and no recent or present lower limb injuries, or back pain that necessitated care by a physician. All subjects completed an informed consent process approved by the Institutional Review Board at the University of Minnesota to participate in the study. Subjects also signed the University of Minnesota Academic Health Center's Authorization for Photography, Filming, or Interviewing because all trials were videotaped and linked to the Motion Monitor system for review and data reduction.
Instrumentation
Three-dimensional lower extremity kinematic data was collected using The Motion Monitor integrated system (Innovative Sports Training, Inc., Chicago, IL) with Ascension's Flock of Birds electromagnetic motion capture system (Ascension Technology Corporation, Burlington, VT). The reliability and validity of electromagnetic motion capture systems in gathering 3-D movements has been previously documented as acceptable.20,21,22,23,24,25 A Bertec force plate (Bertec Corporation, Columbus, OH) was linked to the Motion Monitor system through an A/D interface panel (Measurement Computing's PCIM 1602) for measurement of ground reaction forces. A T- Bayonet Neill-Concelman Connector adaptor allowed another connection to an Analog to Digital conversion (A/D) board (National Instruments Corporation, Austin, TX) to trigger the shutter glasses mechanism (Durfee Design, Minneapolis, MN/VRex, Hawthorne, NY) to disrupt vision. A second connection off the separate A/D board was connected back to the Motion Monitor A/D interface panel to pick up the voltage drop when the glasses shuttered down. These shutter glasses allowed full vision in the open position, but were capable of being triggered at pre-selected phases of movement (based on force plate data) to shut down and block vision from anywhere between 0.1–2.0 seconds by a LabVIEW program set up on a computer that was also connected to the external A/D board via a Peripheral Component Interconnect (PCI) card. Adjustable parameters available on this program included percentage of bodyweight to trigger vision disruption and duration subject cannot see. Another computer was used to trigger a high or low tone indicating which direction the subject needed to cut. This computer was linked to the Motion Monitor system to allow for data capture of the sound impulse. Processing of kinematic and kinetic data was performed by The Motion Monitor software (Innovative Sports Training, Inc., Chicago, IL).
Procedures
Leg dominance was determined by asking each subject to pretend to kick a ball. The leg self-selected by the subject was assigned as the dominant leg for the remainder of the study. For kinematic assessment, electromagnetic sensors were affixed to the skin with double-sided adhesive tape to both the posterior head via attachment to a thermoplastic molded headband and at sacral level two. Four other sensors were attached to each distal lateral thigh near the iliotibial band (ITB) and to the mid shank of each tibia. To determine the local coordinate system, anatomic bony landmarks on the pelvis, thigh, and shank were digitized for data capture of lower extremity movement using International Society of Biomechanics (ISB) recommendations for the hip and ankle26,27 and Grood and Suntay recommendations for the knee.28 The Leardini method was used to determine the location of hip joint centers.29 The local coordinate system for the pelvis was determined using points on the ASIS and PSIS; the thigh was set up using the greater trochanter and medial/lateral femoral epicondyles; and the shank was determined using lateral/medial epicondyles, medial and lateral malleoli, and medial/lateral joint lines.26,27 The global reference system was defined using the right hand rule for all body segments with the positive x-axis defined as the posterior to anterior axis, the positive z-axis defined as the inferior to superior longitudinal axis, and the positive y-axis as right to left. See Figure 1 for sensor placement.
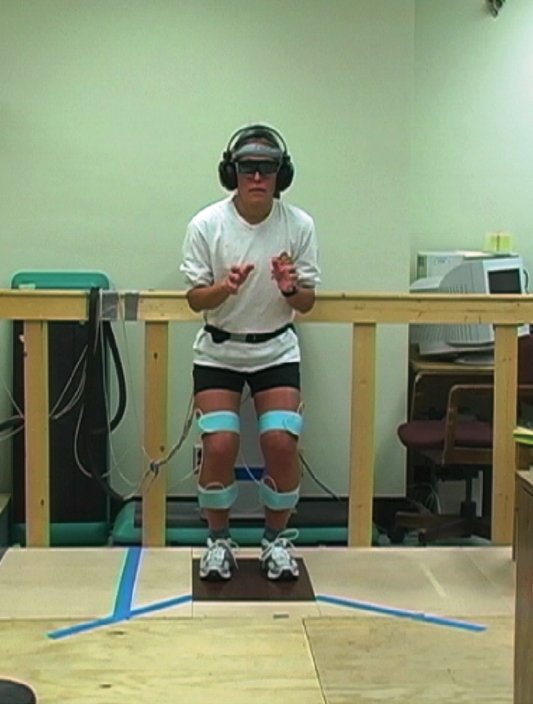
Figure 1.
Laboratory and subject set up.
The task consisted of an open cutting maneuver from a static athletic stance position. Subjects stood on a force platform with equal weight bearing across limbs. When ready, a ball was pitched from an automatic pitching machine directly to the subject from a distance of 15 feet. On the count “one and two and,” a high or low pitch tone was heard in the headphones, indicating which direction the subject was to cut. Visual conditions were randomized so that the glasses either disrupted vision for one second as the subject began the cutting movement, or remained open for the duration of movement. This duration was determined through pilot testing to ensure that visual disruption was of sufficient length to last the entire cutting motion. The timing was consistent subject to subject. Subjects were instructed to catch the ball and cut immediately to the direction indicated by the tone. A taped line angled at approximately 40 degrees to the right and left was secured on the testing platform to guide subjects. This angle is in accordance with values typically seen in a sporting context.30 Subjects were instructed to cut along the line of tape at a distance that was comfortable for them. See Figure 1 for the laboratory set up with a subject in ready position.
Data was captured at 100 Hz and low pass filtered at 30 Hz using a Butterworth 4th order zero phase shift filter. Force plate data was sampled at 1000 Hz with an analog anti-aliasing filter of 500 Hz. Given the speed of the cutting movement, the shutter glasses were triggered to close during movement at a point when the force plate was unloaded at 5% of the subject's bodyweight or conversely when the weight of the subject was 95% of their maximum body weight as measured during calibration of the LabVIEW shutter glass program. The glasses shuttered down and remained off for one second. Subjects performed five practice trials to gain familiarity with the task and equipment worn during testing. Data was analyzed for the movement interval for which vision was disrupted and compared to the same interval of movement when vision was available for all variables except time to reach peak GRF. The entire movement was used for that analysis. Subjects completed 40 successful cutting trials in total, randomized for direction and vision, resulting in 10 trials for each condition. Typical duration between trials was two minutes, which allowed sufficient rest time.
Data Processing
Final outcome variables included: absolute knee displacement, peak and average absolute knee velocities, and time to peak GRF as a percentage of cutting movement. Peak absolute knee displacement was determined by using x, y, and z components of displacement and was descriptive of the overall movement of the knee joint in length from start to finish of the resultant vector. Peak and average knee absolute linear velocities used x, y, and z components of velocity data and were descriptive of how fast the knee joint movement occurred along the resultant vector. Time to peak force was converted to a percent of cutting movement for normalization and gave an indication of push off capability from the force plate during the cutting activity.
Statistical Analysis
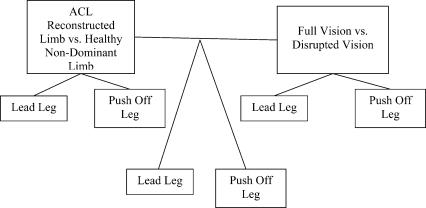
Based on the lowest estimation of effect size of all variables (.60), power analysis of pilot data determined that a sample size of 17 per group, for a total of 34 subjects, was necessary to achieve sufficient power. Independent variables included knee (ACL reconstructed, healthy non-dominant) and vision (full vision, disrupted vision). The non-dominant limb of the healthy group was matched to the surgical limb of the ACLR group based on the fact that the majority of the surgical limbs were stated as non-dominant by subjects. Two separate 2 x 2 repeated-measures analysis of variance were conducted to compare knees and vision for displacement, velocity, and time to peak GRF. Two separate analyses were necessary given in a cutting movement there is a lead leg and push off leg that requires analysis. Post-hoc Tukey tests were conducted for multiple comparisons of all pair-wise differences. A two-way repeated measures ANOVA was also used to analyze the limbs within the ACLR group and within the healthy group. Kruskal-Wallis non-parametric testing was completed for those variables that violated normality. A critical level of p < 0.05 was considered statistically significant for all other group analyses. Figure 2 displays the study design schematic.
Figure 2.
Schematic of study design for repeated measures analysis of variance (ANOVA).
RESULTS
These results are part of a larger study that included analysis of other variables. Overall, subjects with ACL reconstruction self-reported high functioning, describing good to excellent ratings on average on the Cincinnati Knee Rating Scale (CKRS). Subjects with ACLR also described mostly normal/unlimited activity levels (12/15) and a patient grade of 8.4/10 on the CKRS, indicating good to excellent overall knee ratings at the time of testing. Healthy subjects also described their activity levels as recreationally active and athletic on a consistent basis. Descriptive and clinical data are presented in Table 1 and Table 2. No significant differences existed between the ACL and healthy group for cut length of either leg when standardized to height, and was therefore not influential on the outcome of other analyses. Body weight was significantly different between groups, with healthy subjects weighing less. This may have impacted results; therefore a Pearson Product-Moment correlation was completed to identify any significant relationships between body weight and dependent variables. No variables reported here displayed a significant correlation with bodyweight.
Table 1.
Demographic data for healthy subjects (n = 17) and subjects with ACL reconstruction (n = 17).
| Variables | Healthy Subjects Mean (±SD) | ACL Subjects Mean (±SD) |
|---|---|---|
| Age (yrs) | 25.3 (6.0) | 26.5 (6.3) |
| Height (m) | 1.68 (.06) | 1.70 (.07) |
| Weight (kg) | 59.6 (5.72) | 66 (6.44)* |
| KT Change (mm) | 0.90 (0.74) | 1.70 (0.97)* |
| Cut Length (m) | 0.38 (0.07) | 0.36 (0.08) |
| Limb Dominance | ||
| Right | 16 subjects | 17 subjects |
| Left | 1 subject |
p<0.05
Table 2.
Additional descriptive data for subjects with ACL reconstruction.
| ACL Reconstructed Limb | |
|---|---|
| Right | 4 subjects |
| Left | 13 subjects |
| Type of Surgery | |
| PT | 9 subjects |
| HS | 7 subjects |
| Cadaver PT | 1 subject |
| Mean Years Post Surgery (SD) | 4.6 (2.7) |
| Mean Limb Symmetry Index Triple Hop (SD) | 95.8% (8.3) |
| Mean Limb Symmetry Crossover Hop (SD) | 97.2% (10.8) |
PT = patellar tendon, HS = Hamstring
ACL Reconstructed Limb vs. Healthy Non-Dominant Limb
Lead Leg.
Analysis between subjects with ACL reconstruction leading the cut with their reconstructed limb and healthy subjects leading with their non-dominant limb demonstrated a significant main effect for displacement (p=0.01), peak velocity (p=0.01) and average velocity (p=0.01). For this cutting movement with the reconstructed or non-dominant limb as the lead leg, the ACL reconstructed limb displayed significantly shorter displacement and slower peak and average velocities relative to the non-dominant limb of the healthy group. The ACLR group also reached their peak GRF later in the cutting movement (p=0.06), however, this was not statistically different; rather it displayed a trend toward significance (Table 3).
Table 3.
Results for absolute displacement, peak absolute velocity, average absolute velocity, and percent of cut to reach peak GRF of female subject's ACL reconstructed limb (ACL) and healthy female subject's non-dominant limb.
| ACL Lead Leg Mean (±SD) | ND Lead Mean (±SD) | ACL Push Off Leg Mean (±SD) | ND Push Off Leg Mean (±SD) | |
|---|---|---|---|---|
| Displ (m) | 0.76 (.11)* | 0.85 (.08) | 0.75 (.16)** | 0.87 (.12) |
| PV (m/sec) | 2.22 (.47)* | 2.62 (.40) | 2.90 (.62) | 3.19 (.82) |
| AV (m/sec) | 0.81 (.14)* | 0.92 (.11) | 0.84 (.16)** | 0.97 (.14) |
| %Cut (%) | 79.45 (3.18)† | 77.09 (4.20) | 79.41 (2.28)** | 76.65(4.14) |
ND = non-dominant limb; ACL = ACL reconstructed limb; Displ = absolute displacement; PV = peak absolute velocity; AV = average absolute velocity; %Cut = percent of cut to reach peak GRF
Significantly different than healthy non-dominant lead leg (p<0.05)
Significantly different than healthy non-dominant push off leg (p<0.05)
Trend toward significant difference from non-dominant lead leg (p<.0.08)
Push Off Leg.
For the cutting motion with subjects with ACL reconstruction pushing off with their reconstructed limb and healthy subjects pushing off with their non-dominant limb, significance differences were present for displacement (p=0.01) and average velocity (p=0.02). Percent of cutting movement to reach peak GRF occurred significantly later in the cutting movement for the ACLR group during this movement as well (p=0.03). Consistent with previous results, the ACL reconstructed limb displayed shorter displacement, slower average velocity, and reached their peak GRF later in the cutting movement (Table 3).
Disrupted Vision vs. Full Vision
No significant main effect occurred for vision when combining the ACL reconstructed and non-dominant limbs.
Group x Vision Interaction
ACL Reconstructed Limb or Non-dominant Limb as Lead Leg.
A significant interaction was noted for displacement, with the non-dominant/full vision condition displaying a greater displacement than all other conditions (p=0.01). A significant interaction was also noted for average velocity of the lead leg, with the non-dominant/disrupted and full vision conditions displaying a faster average velocity than the ACL/disrupted and full vision pairings (p=0.004). A trend toward a statistically significant difference was noted for peak velocity, with the non-dominant/disrupted and full vision conditions displaying a faster peak velocity than the ACL/disrupted and full vision pairings (p=0.05) (Table 4).
Table 4.
Group-by-Vision Interaction for absolute displacement, peak absolute velocity, average absolute velocity, and percent of cut to reach peak GRF.
| Full Vision/Lead Leg Mean (±SD) | Disrupted Vision Lead Leg Mean (±SD) | Full Vision/Push Off Leg Mean (±SD) | Disrupted Vision/Push Off Leg Mean (±SD) | |
|---|---|---|---|---|
| ACL Displ (m) | 0.76 (.12)* | 0.77 (.11)* | 0.75 (.16) | 0.75 (.17) |
| ND Displ (m) | 0.87 (.08) | 0.83 (.09)* | 0.87 (.11) | 0.87 (.14) |
| ACL PV (m/sec) | 2.19 (.50)† | 2.25 (.46)† | 2.88 (.56) | 2.92 (.68) |
| ND PV (m/sec) | 2.65 (.36) | 2.59 (.44) | 3.18 (.72) | 3.19 (.93) |
| ACL AV (m/sec) | 0.80 (.15)** | 0.82 (.14)** | 0.81 (.13) | 0.82 (.13) |
| ND AV (m/sec) | 0.95 (.11) | 0.90 (.10) | 0.91 (.08) | 0.90 (.10) |
| ACL %Cut (%) | 79.45 (2.77) | 79.45 (3.64) | 79.24 (2.36)† | 79.58 (2.25)† |
| ND %Cut (%) | 77.17 (4.62) | 77.00 (3.87) | 77.41 (3.58) | 76.31 (4.69) |
ND = non-dominant limb; ACL = ACL reconstructed limb; Displ = absolute displacement; PV = peak absolute velocity; AV = average absolute velocity; %Cut = percent of cut to reach peak GRF
Significantly different than ND lead/full vision condition (p<0.05)
Significantly different than ND lead/disrupted vision and ND lead/full vision conditions (p<0.05)
Trend toward significant difference from ND/disrupted vision and ND/full vision (p<0.08)
ACL Reconstructed Limb or Non-dominant Limb as Push Off Leg.
The ACL/disrupted and full vision pairings reached their peak GRF sooner than the non-dominant healthy group with disrupted and full vision, however, this was not statistically different; rather it displayed a trend toward significance (p=0.05) (Table 4).
Within Groups
ACL Reconstructed Limb vs. Non-Surgical Limb.
Within the ACL reconstructed group, no significant differences existed between the ACL reconstructed knee and the non-surgical knee or between vision conditions for any variable. There were also no significant interactions.
Healthy Dominant Limb vs. Non-Dominant Limb.
Within the healthy group only, the non-dominant limb as lead leg reached a significantly faster peak velocity than the dominant limb. This indicates that faster movement occurs in the lead leg when pushing off the dominant limb for the healthy subjects versus their non-dominant limb (p<.01) (Table 5). There was also a main effect of vision for displacement for lead and push off legs (p=0.02; p=0.02) and for average velocity of lead legs (p=0.004). With vision disrupted, healthy subjects moved less distance and at a slower average velocity based on the data from their lead and push off legs (Table 6). There was also a significant interaction between the dominant and non-dominant limbs and visual conditions for average velocity of the lead leg during cutting (p=0.04). Pushing off from the dominant limb with vision created a significantly faster lead leg than for other pairings. A trend towards a significant interaction also existed for absolute displacement, with pushing off the dominant limb with disrupted vision having the lower displacement for either leg relative to the same scenario with vision (p=.05) (Table 7).
Table 5.
Healthy female subject's dominant and non-dominant limb data for absolute displacement, peak absolute velocity, average absolute velocity, and percent of cut to reach peak GRF.
| DOM Lead Leg Mean (SD) | ND Lead Mean (±SD) | DOM Push Off Leg Mean (±SD) | ND Push Off Leg Mean (±SD) | |
|---|---|---|---|---|
| Displ (m) | 0.86 (.08) | 0.85 (.08) | 0.87 (.09) | 0.87 (.12) |
| PV (m/sec) | 2.13 (.24) | 2.62 (.40)* | 3.05 (.55) | 3.19 (.36) |
| AV (m/sec) | 0.90 (.09) | 0.92 (.11) | 0.95 (.10) | 0.92 (.14) |
| %Cut (%) | 77.09 (4.20) | 76.65 (4.14) |
DOM = dominant limb; ND = non-dominant limb; Displ = displacement; PV = peak absolute velocity; AV = average absolute velocity; %Cut = percent of cut to reach peak GRF
Significantly different than healthy DOM lead leg (p<0.05)
Table 6.
Healthy subject's data for the main effect of vision for absolute displacement, peak absolute velocity, and average absolute velocity
| Full Vision/Lead Leg Mean (±SD) | Disrupted Vision/Lead Leg Mean (±SD) | Full Vision/Push Off Leg Mean (±SD) | Disrupted Vision/Push Off Leg Mean (±SD) | |
|---|---|---|---|---|
| Displ (m) | 0.86 (.07) | 0.84 (.09)* | 0.88 (.09) | 0.85 (.12)* |
| PV (m/sec) | 2.40 (.39) | 2.35 (.43) | 3.16 (.64) | 3.08 (.75) |
| AV (m/sec) | 0.93 (.10) | 0.90 (.10)* | 0.98 (.10) | 0.95 (.13) |
Displ = displacement; PV = peak absolute velocity; AV = average absolute velocity
Significantly different than full vision condition (p<0.05)
Table 7.
Healthy subjects group-by-vision interaction for absolute displacement, peak absolute velocity, average absolute velocity, and percent of cut to reach peak GRF.
| Full Vision/Lead Leg Mean (±SD) | Disrupted Vision Lead Leg Mean (±SD) | Full Vision/Push Off Leg Mean (±SD) | Disrupted Vision/Push Off Leg Mean (±SD) | |
|---|---|---|---|---|
| DOM Displ (m) | 0.86 (.07) | 0.86 (.09) | 0.89 (.08) | 0.84 (.10)** |
| ND Displ (m) | 0.87 (.08) | 0.83 (.09)** | 0.87 (.10) | 0.87 (.14) |
| DOM PV (m/sec) | 2.16 (.24) | 2.10 (.25) | 3.13 (.58) | 2.97 (.53) |
| ND PV (m/sec) | 2.65 (.36) | 2.59 (.44) | 3.18 (.72) | 3.19 (.93) |
| DOM AV (m/sec) | 0.91 (.08) | 0.90 (.10) | 0.98 (.08) | 0.93 (.11) |
| Non-Dom AV (m/sec) | 0.95 (.11)* | 0.90 (.11) | 0.98 (.12) | 0.96 (.15) |
| ND %Cut (%) | 77.41 (3.58) | 76.31 (4.69) | ||
| DOM %Cut (%) | 77.17 (3.87) | 77.00 (4.62) |
DOM = dominant limb; ND = non-dominant limb; ACL = ACL reconstructed limb; Displ = absolute displacement; PV = peak absolute velocity; AV = average absolute velocity; %Cut = percent of cut to reach peak GRF
Significantly different than DOM and ND/disrupted vision conditions (p<0.05)
Trend toward significant difference from DOM/full vision (p<0.08)
DISCUSSION
The purpose of this study was to compare movement trajectories of the knee joint, as described by displacement, velocity, and percent of cut to reach peak GRF, between female subjects' ACL reconstructed knees and healthy subjects' non-dominant knees when vision was disrupted or fully available during an ‘unplanned’ cutting movement and relate these findings to motor planning strategies. Previous research14,25,33,34,35 supports that specific alterations of angles, moments, and EMG patterns have an association with gait, landing, and cutting kinetics and kinematics in females, and subjects with ACL deficiency or ACL reconstruction. McLean et al., Ford et al., Sigward et al., and Besier et al. demonstrated that sidestep cutting maneuvers create kinematics and kinetics that place the knee in a vulnerable position, similar to the kinematics and kinetics suggested as possible mechanisms for ACL injury.3,4,8,9,10,31 The integrity of the ACL during landing requires the proper coordination of lower extremity muscles, especially the quadriceps and hamstrings.32 Decreased knee flexion and trunk flexion, increased knee valgus angles and moments, increased latency of hamstrings, and increased quadriceps activity are common findings relating to the possible mechanisms for increased incidence of ACL injury and subsequent deficiency and/or surgical reconstruction.14,25,33,34,35
A limited number of studies36,37 have compared the velocity of subjects with ACL reconstructed or deficient knees compared to controls, and only in a general sense. None have looked at the absolute displacement and velocity of the knee joint as was identified in this research. Rather, the few36,37 that did simply measured the velocity of movement of the body, i.e. walking or running velocities; or indirectly inferred velocity from measures of other data. In these studies.36,37 the subjects with ACL reconstruction consistently moved at slower velocities than the healthy control subjects. When comparing the ACL reconstructed and healthy non-dominant knees during a cutting movement in this research, displacement and velocity measures consistently displayed significant differences. Regardless of whether the analyzed limb was pushing off or leading, when compared, the ACLR subjects had less displacement and slower velocities than the healthy subjects. Previously authors have suggested that changes in joint kinematics and kinetics following ACL reconstruction, like reducing velocities of movement, are common adaptations to protect the knee.36,37 The faster one travels to eventually collide with a stable surface and stop, the higher the GRF and the more the neuromuscular system must actively dampen these forces. This requires sufficient strength and neuromuscular coordination.38 Reducing velocity will help to reduce the GRF upon landing.17,33,38,39,40,41 This reduction in velocity and distance traveled may be an alteration in movement that reduces their risk and allows for safe completion of the task.
A major component of this research was to identify how well subjects moved into the cutting maneuver. The variable used to capture this concept was the percent of full cutting movement that subjects needed to reach their peak GRF. Each trial was normalized to 100 percent because the duration of each cut was different for each trial and subject. This variable mostly gave an indication of the push off leg's ability to generate force and power when an audible tone sounded to signal the subject to initiate the cut. Sidestep cutting in sports is used as an evasive maneuver at variable speeds. Cutting movements require the integration of several systems for successful performance. Sufficient propulsion and stabilization of the push off leg is necessary to move the lead leg and rest of the body through space. The lead leg must also anticipate the landing by activating specific muscles in a specific sequence to minimize impact forces with the ground.
Consistent significant differences existed between the ACLR group and healthy group in ability to reach their peak ground reaction force quickly. Subjects with ACL reconstruction were slower to reach their peak GRF. These results may relate to other research findings reporting that the involved surgical limb showed reduced ability to generate force at takeoff during a drop vertical jump, whereby female athletes displayed side-to-side differences during both the landing and takeoff phase of the drop vertical jump two years later, with the ACL reconstructed limb displaying reduced abilities to accept load quickly on landing and to generate force upon takeoff.14 Other factors that may impact this variable are lower extremity strength, power, neuromuscular coordination, and proprioception. If reduced, as is frequently demonstrated by subjects with ACL reconstruction, subjects may struggle with achieving peak force quickly.42 which may also be reflected in reduced displacement and velocity. Increasing evidence suggests that poor or abnormal neuromuscular control of lower extremity biomechanics, especially during athletic maneuvers such as cutting and landing, is a major contributor to the mechanism of non-contact ACL injury in females.2,3 Increased knee valgus angles and moments, reduced knee flexion angles and increased hip adduction angles all may influence movement patterns in a negative manner that may result in the differences noted between the ACLR group and healthy group of females in this research. Research also suggests that females are weaker than males in measurements of hip strength as well as quadriceps and hamstring strength, even when normalized to body weight.34 Females exhibit different lower extremity muscle activation patterns than males, with hamstrings demonstrating a delay in activation relative to the quadriceps.9,34 Muscle activation also differs during anticipated and unanticipated tasks, where unanticipated events create muscle activation patterns that may be detrimental and increase injury risk.3,6,8,10,11 Therefore, coupling ACL reconstruction with the female gender may increase the strength deficits and dysfunctional neuromuscular patterns noted, given that hip and thigh strength reductions and neuromuscular alterations have been noted in subjects with ACL reconstruction.
Proprioceptive deficits may still persist after ACLR and subsequent rehabilitation; however this cannot be stated definitively in this group of subjects, as it was not tested directly. The subjects push off leg functions essentially in single leg stance as the lead leg is lifted upon movement into the cutting motion. If proprioception is compromised, subjects may have less stability on that leg which would impact their ability to generate force for push off.15 With disruption of the ACL and surrounding tissue, sensory input is altered, affecting proprioception and muscle activation patterns.2,16 Research suggests that proprioceptive dysfunction may occur with ACL injury and reconstruction along with disruption and/or changes in movement patterns during gait and other simple activities.15,16 Thus, for these subjects with ACL reconstruction, taking longer to reach their peak GRF could be reflective of reduced lower extremity strength, power, altered biomechanics, neuromuscular control, or proprioception. Overall, the data from the current investigation showed differences which suggest that subject's strength, timing, and power may be reduced, thus resulting in a decreased ability to generate lower extremity force.
An interesting observation was that healthy subjects demonstrated greater standard deviations across all conditions for percent of cut to reach peak GRF than subjects with an ACL reconstruction. They also demonstrated significant differences between their legs, whereas the ACLR group did not. When comparing the subjects with ACLR separately and analyzing leg-to-leg differences, the ACLR group displayed no significant differences between pushing off with their ACL limb and pushing off with their non-surgical limb. Given these results, it appears that the ACL reconstruction had an impact on movement bilaterally relative to the healthy group. This is demonstrated by the differences between the ACLR group and healthy subjects, yet a lack of differences between the ACL reconstructed limb and non-surgical limb of the ACL subjects. This finding is supported by other studies that suggest that ACL injury and subsequent reconstruction affects both limbs.7,12,14
Within the healthy group, visual disruption did have an impact on knee displacement of the push off limb. The combination of group and vision also had some affect on displacement and peak velocity. Most often the dominant limb reached a faster velocity or had a greater displacement with vision. Average velocity was very close to showing a trend in the same direction at p value of 0.08. This may be suggestive of more variability across trials for healthy subjects, which is more likely to occur for this healthy group based on recent research findings that variability is a necessary component of healthy movement patterns, while a reduction in variability may increase injury risk due to altered motor planning and control.43,44,45,46,47,48 Some variability in movement is necessary for reduction of injury risk. Rigid movement patterns may result in the inability to adjust to complex tasks, which may increase injury risk. It may be that a person with an injury and/or surgery pays more attention to their movement to ensure safe and effective completion of the task, thus repeating the same pattern of movement throughout trials.
Given the results of this research, continual visual input may not be necessary to complete tasks successfully, even when proprioception may also be compromised due to injury/surgery. Given no main effect for vision, these findings support previous research17,38,40 that periodic visual access to the environment and task is sufficient for completion of the task by adoption of a new or different ‘default’ motor program. It is also possible that subjects may have a visual representation of the task which is transformed into movement either directly or via kinesthetic representation, which may be required for more complicated movements or when the visual representation is lost or disrupted.49 Despite the task being somewhat unplanned with several distractions, it must be considered that the task may be a familiar and simple movement pattern for some subjects. Lieberman and Hoffman demonstrated that subjects with more experience in a task respond with less difference in movement patterns when vision is disrupted.50 The results of this present study are consistent with the findings of Lieberman and Hoffman.50
To perform everyday movements and interactions, the central nervous system modulates forces before contact with a landing surface, as well as through the time course of the movement. Controlling an expected collision with the landing surface requires some prediction to anticipate the GRFs that will occur upon impact.17 Other aspects of movement can make this more complicated given the wide variety of task conditions that occur, such as velocity of movement, landing surface, height of drop, or range of movement required. These task constraints can result in larger forces and could lead to serious injury if adaptations are not correctly estimated.17 Thus, continuous vision and predictive control mechanisms has been purported as important for successful and safe task completion. However, this research and results reported by others17,38,40 suggest that the role of vision is not quite as important as originally thought. When subjects are able to visualize the task and environment and perform it with vision, when the time comes to perform the task without vision, minimal EMG, kinematic and kinetic changes occur that are different from when vision was available.17,38,40 Thus in trials where vision was not available, it is possible that vestibular, proprioceptive, and cognitive input all interact in a way to allow for control of movement during the task from beginning to end with minimal change. For subjects with ACL reconstruction, this results in moving in a more rigid pattern that reduces their risk. For the healthy subjects, the result was greater variability in their movements in order to accommodate each situation.
There are several limitations to this study. The use of surface electromagnetic sensors mounted on the skin may allow for skin slippage with movement. Every attempt was made to keep the skin motion artifact low; however slight movement may have occurred. In an attempt to keep this low, sensors were placed on areas that had less underlying muscle or tissue movement. Also, for the calculated variables in this research, movement of the tibia relative to the femur was not used, thus the precision of the electromagnetic sensors in capturing underlying bone motion may not be as important. The pertinent data used was a point within the knee joint moving through space. Also, this surface-based sensor error is usually not systematically different between groups so that the distribution of error should be similar between the two study groups. Also, despite finding significant differences between groups and in combination with visual disruption, confirmation of whether these differences are clinically significant is uncertain.
Time after surgery may be another limitation. ACL subjects were an average of 4.6 years after surgery with a range from barely one year to nine years. This range is quite broad and may be a limitation to the study, in that subjects closer to their ACL reconstruction may have demonstrated more significant differences in movement variables from healthy subjects as compared to those with more time between ACL reconstruction and testing. Narrowing this range would allow for more specific understanding of movement patterns during specific times after ACL reconstruction, especially times when subjects are thought to be more vulnerable to re-injury. Type of ACL surgery was variable as well, which may have implications on outcomes as hamstring and patellar tendon grafts may exhibit different deficits at different follow up periods. The final limitation was the lab environment. The lab set up was such that subjects were unable to run or move into a cutting maneuver and had to start from an athletic stance. This may have been too simplistic to identify many differences between groups. Having the ability to run and cut obviously simulates an athletic maneuver more realistically.
CONCLUSION
This research examined movement patterns of the knee joint during unplanned side-step cutting maneuvers of subjects with ACLR and healthy subjects with random instantaneous vision disruption. Movement patterns were analyzed in new and unique ways relative to what had been reported in much of the research on ACL injury and movement. Previous findings14,34,35,42 may help to explain the movement variations between subjects with ACLR and healthy subject non-dominant knees; i.e. less postural stability and strength of the ACL reconstructed limb may result in an increased time to reach peak GRF and reduced velocity of ACL reconstructed subjects during cutting. With visual input changes (when vision was disrupted), subjects demonstrated minimal changes to their patterns of movement, thus were most likely relying on an internal visual memory of the environment and task characteristics to perform the movement successfully. However, it does appear that a few consistent pattern changes were noted when vision was disrupted. Lack of vision resulted in reduced absolute velocity and displacement, especially for subjects with ACL reconstruction, thus suggesting use of a new or altered ‘default’ motor program. Implications for rehabilitation of patients with ACL reconstruction are inherent in the outcomes of this research given the notable changes in displacement, velocity, and time to reach peak GRF relative to the healthy group. Working on velocity of movement and single leg push off skills would be helpful to improve performance in athletic situations. Knowing that these skills are lacking even over four years after surgical reconstruction indicates areas to consistently focus on athletically to improve performance and reduce injury risk. Rehabilitation programs and skill training may benefit from the addition of activities where vision is disrupted to further challenge patients.51 Overall, this study provides indirect information related to strength, proprioception, power, visual guidance of movement, motor planning, and ACL reconstruction that may affect rehabilitation program development.
REFERENCES
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: A 13-year review. Am J Sports Med. 2005;33(4):524–530 [DOI] [PubMed] [Google Scholar]
- 2.Hewett TE, Paterno MV, Myer GD. Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop. 2002;401:76–94 [DOI] [PubMed] [Google Scholar]
- 3.McLean SG, Lipfert S, van den Bogert AJ. Effect of gender and defensive opponent on the biomechanics of sidestep cutting. Med Sci Sports Exerc. 2004;36:1008–1016 [DOI] [PubMed] [Google Scholar]
- 4.McLean SG, Huang X, van den Bogert AJ. Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech. 2005;20:863–870 [DOI] [PubMed] [Google Scholar]
- 5.Sigward SM, Powers CM. The influence of experience on knee mechanics during side-step cutting in females. Clin Biomech. 2006; 21:740–747 [DOI] [PubMed] [Google Scholar]
- 6.Pollard CD, Heiderscheit BC, van Emmerik RE, Hamill J. Gender differences in lower extremity coupling variability during an unanticipated cutting maneuver. J Applied Biomech. 2005;21:143–152 [DOI] [PubMed] [Google Scholar]
- 7.Ferber R, Davis IM, Williams DS. Gender differences in lower extremity mechanics during running. Clin Biomech. 2003;18:350–357 [DOI] [PubMed] [Google Scholar]
- 8.Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sports Exerc. 2005;37:124–129 [PubMed] [Google Scholar]
- 9.Sigward SM, Powers CM. Loading characteristics of females who exhibit excessive valgus moments during side-step cutting [abstract]. J Orthop Sports Phys Ther. 2007;37(2):A12–A13 [Google Scholar]
- 10.Besier TF, Lloyd DG, Ackland TR, Cochrane JL. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sports Exerc. 2001;33(7):1176–1181 [DOI] [PubMed] [Google Scholar]
- 11.Houck J, De Haven K, Maloney M. Associations between playing time and kinetic variables during an unexpected cut task [abstract]. J Orthop Sports Phys Ther. 2007;37:A14–A15 [Google Scholar]
- 12.Hiemstra LA, Webber S, MacDonald PB, Kriellaars DJ. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft. Clin Biomech. 2007; 22:543–550 [DOI] [PubMed] [Google Scholar]
- 13.Ferber R, Osternig LR, Woollacott MH, Wasielewski NJ, Lee JH. Bilateral accommodations to anterior cruciate ligament deficiency and surgery. Clin Biomech. 2004;19:136–144 [DOI] [PubMed] [Google Scholar]
- 14.Paterno MV, ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258–262 [DOI] [PubMed] [Google Scholar]
- 15.Okuda K, Abe N, Katayama Y, Senda M, Kuboda T, Inoue H. Effect of vision on postural sway in anterior cruciate ligament injured knees. J Orthop Sci. 2005;10:277–283 [DOI] [PubMed] [Google Scholar]
- 16.Wexler G, Hurwitz DE, Bush-Joseph CH, Andriacchi TP, Bach BR., Jr. Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clinical Orthopaedics and Related Research. 1998;348:166–175 [PubMed] [Google Scholar]
- 17.Santello M. Review of motor control mechanisms underlying impact absorption from falls. Gait and Posture. 2005;21:85–94 [DOI] [PubMed] [Google Scholar]
- 18.Houck J, Yack HJ. Associations of knee angles, moments and function among subjects that are healthy and anterior cruciate ligament deficient (ACLD) during straight ahead and crossover cutting activities. Gait and Posture. 2003;18:126–138 [DOI] [PubMed] [Google Scholar]
- 19.Barber SD, Noyes FR, Mangine R, DeMaio M. Rehabilitation after ACL reconstruction: function testing. Orthopedics. 1992;15(8):969–974 [DOI] [PubMed] [Google Scholar]
- 20.Ferber R, McClay Davis I, Williams DS, Laughton C. A comparison of within- and between-day reliability of discrete 3D lower extremity variables in runners. Journal of Orthopaedic Research. 2002;20:1139–1145 [DOI] [PubMed] [Google Scholar]
- 21.Kulas AS, Windley TC, Schmitz RJ. Effects of abdominal postures on lower energetics during single leg landings. J Sport Rehabil. 2005;14: 58–71 [Google Scholar]
- 22.Mackey AH, Walt SE, Lobb GA, Stott S. Reliability of upper and lower limb three-dimenstional kinematics in children with hemiplegia. Gait and Posture. 2005;22:1–9 [DOI] [PubMed] [Google Scholar]
- 23.Mills PM, Morrison S, Lloyd DG, Barrett RS. Repeatability of 3D gait kinematics obtained from an electromagnetic tracking system during treadmill locomotion. Journal of Biomechanics. 2007;40:1504–1511 [DOI] [PubMed] [Google Scholar]
- 24.Padua DA, Arnold BL, Carcia CR, Granata KP. Gender differences in leg stiffness and stiffness recruitment strategy during two-legged hopping. J Mot Behav. 2005;37(2):111–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Padua DA, Arnold BL, Perrin DH, Gansneder BM, Carcia CR, Granata KP. Fatigue vertical leg stiffness, and stiffness control strategies in males and female. Journal of Athletic Training. 2006;41(3):294–304 [PMC free article] [PubMed] [Google Scholar]
- 26.Wu G, Cavanaugh PR. ISB recommendations for standardization in the reporting of kinematic data. J Biomechanics. 1995;28(10)1257–1261 [DOI] [PubMed] [Google Scholar]
- 27.Wu G, Siegler S, Allard P, et al. ISB recommendations on definitions of joint coordinate system of various joints for the reporting of human joint motion – part 1: ankle, hip, and spine. J Biomechanics. 2002;35:543–548 [DOI] [PubMed] [Google Scholar]
- 28.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three- dimensional motions: application to the knee. J Biomechanical Engng. 1983;105:136–144 [DOI] [PubMed] [Google Scholar]
- 29.Leardini A, Cappozzo A, Catani F, et al. Validation of a functional method for the estimation of hip joint centre location. J Biomech. 1999;32:99–103 [DOI] [PubMed] [Google Scholar]
- 30.McLean SG, Neal RJ, Myers PT, Walters MR. Knee joint kinematics during the sidestep cutting maneuver: potential for injury in women. Med Sci Sports Exerc. 1999;31:959–968 [DOI] [PubMed] [Google Scholar]
- 31.McLean SG, Myers PT, Neal RJ, Walters MR. A quantitative analysis of knee joint kinematics during the sidestep cutting maneuver. Bulletin Hospital for Joint Diseases. 1998;57(1):30–38 [PubMed] [Google Scholar]
- 32.Cowling EJ, Steele JR. The effect of upper-limb motion on lower limb muscle synchrony. Journal of Bone and Joint Surgery. 2001;83-A(1):35–41 [DOI] [PubMed] [Google Scholar]
- 33.Decker MJ, Torry MR, Wyland DJ, Sterett WI, Steadman J. Gender differences in lower extremity kinematics, kinetics, and energy absorption during landing. Clin Biomech. 2003;18:662–669 [DOI] [PubMed] [Google Scholar]
- 34.Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512–1532 [DOI] [PubMed] [Google Scholar]
- 35.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311 [DOI] [PubMed] [Google Scholar]
- 36.Devita P, Hortobabyi T, Barrier J. Gait biomechanics are not normal after anterior cruciate ligament reconstruction and accelerated rehabilitation. Med Sci Sports Exerc. 1998;29(7): 1481–1488 [DOI] [PubMed] [Google Scholar]
- 37.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech. 2002;17:56–63 [DOI] [PubMed] [Google Scholar]
- 38.Thompson HW, McKinley PA. Landing from a jump: the role of vision when landing from known and unknown heights. NeuroReport. 1995;6:581–584 [PubMed] [Google Scholar]
- 39.Chappell JD, Yu B, Kirkendall DT, Garrett WE. The effect of fatigue on lower extremity kinematics and kinetics during landings of stop jump tasks. Am J Sports Med. 2005;33:1022–1029 [DOI] [PubMed] [Google Scholar]
- 40.Liebermann DG, Goodman D. Effects of visual guidance on the reduction of impacts during landings. Ergonomics. 1991;34(11):1399–1406 [DOI] [PubMed] [Google Scholar]
- 41.Yu B, Lin CF, Garrett WE. Lower extremity biomechanics during the landing of a stop-jump task. Clin Biomech. 2006;21:297–305 [DOI] [PubMed] [Google Scholar]
- 42.Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC. Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. Journal of Athletic Training. 2002;37(3): 262–268 [PMC free article] [PubMed] [Google Scholar]
- 43.Davis I, Ireland ML, Hanaki S. ACL injuries – The gender bias. J Orthop Sports Phys Ther. 2007;37(2):A2. [PubMed] [Google Scholar]
- 44.Moraiti C, Stergiou N, Ristanis S, Georgoulis AD. ACL deficiency affects stride to stride variability as measured using nonlinear methodology. Knee Surg Sports Traumatol Arthrosc. 2007;15:1406–1413 [DOI] [PubMed] [Google Scholar]
- 45.Davids K, Glazier P, Araujo D, Bartlett R. Movement systems as dynamical systems. The functional role of variability and its implications for sports medicine. Sports Med. 2003;33(4):245–260 [DOI] [PubMed] [Google Scholar]
- 46.Stergiou N, Harbourne RT, Cavanaugh JT. Optimal movement variability: a new theoretical perspective for neurologic physical therapy. Journal of Neurologic Physical Therapy. 2006;30(3):120–129 [DOI] [PubMed] [Google Scholar]
- 47.Kurz MJ, Stergiou N, Buzzi UH, Georgoulis AD. The effect of anterior cruciate ligament reconstruction on lower extremity relative phase dynamics during walking and running. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):107–15 [DOI] [PubMed] [Google Scholar]
- 48.Miller RH, Meardon SA, Derrick TR, Gillette JC. Continuous relative phase variability during an exhaustive run in runners with a history of iliotibial band syndrome. J Appl Biomech. 2008. Aug;24(3):262–70 [DOI] [PubMed] [Google Scholar]
- 49.Soechting JF, Flanders M. Sensorimotor representations for pointing to targets in three-dimensional space. Journal of Neurophysiology. 1989;62(2):582–593 [DOI] [PubMed] [Google Scholar]
- 50.Liebermann DG, Hoffman JR. Timing of preparatory landing responses as a function of availability of optic flow information. Journal of Electromyography and Kinesiology. 2005;15:120–130 [DOI] [PubMed] [Google Scholar]
- 51.Williams, Weigelt, Harris, Scott MA. Age-related differences in vision and proprioception in a lower limb interceptive task: the effects of skill level and practice. Res Q Exerc Sport. 2002;73(4):386–395 [DOI] [PubMed] [Google Scholar]