A randomized, controlled trial to test the hypothesis that physical exercise reduces fatigue and improves physical performance in cancer patients with advanced and incurable disease is reported. Fatigue was not reduced but physical performance was significantly improved after 8 weeks of physical exercise.
Keywords: Physical exercise, Fatigue, Randomized controlled trial, Advanced cancer
Learning Objectives
After completing this course, the reader will be able to:
Describe the impact of physical exercise on fatigue and physical performance outcomes in cancer patients with advanced and incurable disease.
Identify potential clinical benefits of inclusion of physical exercise in treatment regimens for cancer patients with advanced disease.
This article is available for continuing medical education credit at CME.TheOncologist.com
Abstract
Background.
Physical exercise can improve cancer patients' functioning and reduce their symptom levels. A randomized, controlled trial was launched to test the hypothesis that physical exercise reduces fatigue and improves physical performance in cancer patients with advanced and incurable disease.
Methods.
Cancer patients (n = 231) with a life expectancy ≤2 years were randomized to a physical exercise group (PEG, n = 121) or a control usual care group (UCG, n = 110). The PEG exercised under supervision 60 minutes twice a week for 8 weeks. Assessments were performed before and after the intervention. The primary outcome was physical fatigue (PF) measured by the Fatigue Questionnaire. Physical performance was a secondary outcome measured by the Shuttle Walk Test (SWT) and hand grip strength (HGS) test. Analyses were performed after multiple imputations for missing data. The trial is registered with ClinicalTrials.gov (identifier, NCT00397774).
Findings.
Thirty-six percent of the PEG were lost to follow-up compared with 23% of the UCG, primarily as a result of disease progression. Seventy-eight PEG and 85 UCG patients completed the intervention. Analyses showed no significant between-group effects in PF. However, clinically and statistically significant between-group effects were found for the SWT and HGS test.
Interpretation.
Fatigue was not reduced but physical performance (SWT and HGS test) was significantly improved after 8 weeks of physical exercise. Physical exercise might therefore be a suitable approach for maintaining physical capacity in cancer patients with incurable and advanced disease.
Introduction
Pain, frailty, fatigue, weight loss, and reduced physical function are common among cancer patients with advanced and incurable disease and negatively impact their quality of life (QoL) [1, 2]. Symptom control and maintaining or improving functions are therefore central goals for the treatment of these patients [3].
Systematic reviews and meta-analyses have demonstrated that physical exercise reduces fatigue and improves physical functioning and QoL in cancer patients in general [4–8]. However, the majority of studies were performed in breast cancer survivors, and a 2010 review pointed to a lack of studies on the effects of physical exercise as palliation [9].
In the palliative phase, cancer often has catabolic effects on muscles that may contribute to the development of cancer cachexia with subsequent consequences for physical strength and endurance [10]. Disease-modifying or symptom-relieving treatments might induce fatigue or sedation, leading to physical inactivity and thereby reducing physical functioning and capacity. Loss of mobility may reduce independence in daily life and can lead to hospitalization, thereby further reducing patient autonomy and QoL [11–13]. Theoretically, interventions that enhance physical activity and decelerate the reduction in physical performance might therefore be relevant parts of palliative care programs.
However, a recent systematic review concluded that there is insufficient evidence to support the introduction of physical exercise and activity into routine palliative care practice at present [14]. Six studies were identified, with significant heterogeneity in terms of design, patient characteristics, type of physical exercise, and outcomes [14]. Only one study had a randomized, controlled design and three were case reports. The findings indicated that physical exercise can improve QoL, well-being, physical functioning, and fatigue in cancer patients with incurable and advanced disease. Methodologically rigorous studies with larger samples and appropriate comparison groups were therefore asked for [14].
There is, at present, no commonly agreed-upon definition of what constitutes the palliative phase of a cancer disease trajectory except that the disease is incurable. An increasing number of patients with incurable disease now receive life-prolonging treatment, challenging the common assumption of the palliative phase succeeding a phase of life-prolonging treatment. Additionally, many of these patients also receive palliative treatment for symptoms such as pain. The palliative care population, therefore, becomes heterogeneous, and interventions of long duration are exposed to the effects of unforeseen disease progression. With this background, we first piloted a physical exercise intervention for cancer patients with advanced and incurable disease focusing on feasibility and potential effects [15–17]. We found that patients with a life expectancy <1 year were willing and able to attend a physical exercise program [15]. Fatigue decreased while well-being and physical performance improved after 6 weeks of physical exercise [16].
In the present randomized, controlled trial (RCT) on the effects of a physical exercise program administered to patients with advanced and incurable cancer, the intervention group was allocated to an 8-week physical exercise program and the control group was allocated to care as usual. In designing the exercise program, one key factor was to introduce a program transferable to ordinary clinical practice. It was hypothesized that the exercise program would reduce fatigue and improve physical performance.
Patients and Methods
Settings and Participants
This study was performed as a Norwegian multicenter study between October 2006 and May 2009. Two hundred thirty-one cancer patients were recruited from day care palliative care units (PCUs) and from outpatient oncological units/departments at local/regional hospitals (OUs). Generally, patients are referred to PCUs because of symptom burden and/or psychosocial needs. PCUs have access to palliative multidisciplinary teams. Those recruited from the outpatient OUs attended these for routine follow-up care. The patients were recruited at the following sites: St. Olavs University Hospital (n = 86) (from OUs and PCUs), Hospice Lovisenberg (n = 58) (from PCUs), Oslo University Hospital (n = 42) (from PCUs and OUs), Telemark Hospital (n = 20) (from PCUs and OUs), Sunniva Clinic for Palliative Care (n = 19) (from PCUs), and Haukeland University Hospital (n = 6) (from OUs).
The patients were eligible for inclusion if they had incurable and metastatic cancer (either locoregional or distant metastases), a life expectancy of 3 months to 2 years, a Karnofsky performance status (KPS) score ≥60, adequate pain relief (pain intensity ≤3 on a 0–10 numerical rating scale), the ability to walk, and unimpaired cognitive function.
Design and Procedures
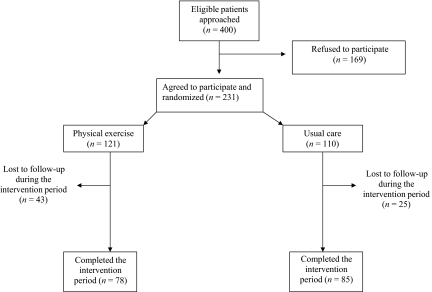
This was a prospective, two-armed RCT (Fig. 1). Eligible patients were identified by their attending physician, physiotherapist, or nurse, and hence the patients must be considered a sample of convenience. At St. Olavs Hospital, the medical journals of all patients attending the outpatient clinic were screened manually to identify patients who met the inclusion criteria. At the other centers, the health personal recruited patients they judged to meet the inclusion criteria based upon their clinical evaluation. The patient's physician for each treatment then received a written request as to whether or not the patient met the inclusion criteria.
Figure 1.
Patient flowchart showing numbers of patients eligible, refused to participate, recruited, randomized, lost to follow-up, and completed.
Randomization
The participants were stratified by age (>65 years or <65 years), gender, place of inclusion, and KPS score (>80 or <80) and were randomly (block randomization) assigned to a usual care group (UCG) or to a physical exercise group (PEG).
Physical Exercise Intervention
The exercise group had two exercise sessions per week over an 8-week period. The exercises were performed in groups of two to eight patients supervised by a physiotherapist. Each session lasted 50–60 minutes and included a warm-up (10–15 minutes), circuit training with six stations (30 minutes), and stretching/relaxation (10–15 minutes). The exercise program was tailored to the individual patient's level of physical functioning. The content was feasible and relevant for the population according to the findings in the pilot study and is described in detail in two earlier publications [15, 16].
Warm-Up Session
The warm-up session lasted for 10–15 minutes and was aerobic exercise using large muscle groups in an upright or sitting position; alternatively, stationary bicycling was performed.
Circuit Training
At each of the six circuit stations, exercise was performed for 2 minutes, with a 1-minute interval in which the patients moved to the next station, continuing for 30 minutes in total. Music was used as a time indicator. The main focus for the exercises was on lower and upper limb muscle strength, standing balance, and aerobic endurance. Each station had a core series of exercises, with the possibility for adjustments according to the individual patient's physical function. The six stations in the circuit program were as follows. Station 1: Strengthening of the lower limb: step up and down on a step. Station 2: Balance: stand on either a trampoline or a thick mat, first maintain balance, then as a progression weight transfer. Station 3: Strengthening of the upper limb: use a pulley or elastic resistance band and pull down. Station 4: General functioning: start in the standing position, descend to the floor, lie on back, then roll from side to side, and stand up again. For patients who were able to, abdominal and back exercises were included. Station 5: Strengthening of the lower limb: sit on a bench/chair, stand up, and sit down. Station 6: Aerobic endurance: stationary bicycling or treadmill walking.
Stretching and Relaxation
The last part of the program included stretching of the muscles used during the circuit training and 5 minutes of relaxation to calm music.
The patients were encouraged to be physically active in their everyday life, but were not given any specific exercises to do at home.
Assessments
Pre- and postintervention assessments were performed at baseline and immediately after the intervention period. Demographic data were collected by patient self-report and medical data were collected from medical records. The patient's body weight was measured and height was self-reported. Adherence was registered by the physiotherapists supervising the exercise sessions.
Patient-Reported Outcomes
Fatigue was assessed by the Fatigue Questionnaire (FQ) [18]. The FQ measures physical fatigue (PF), mental fatigue (MF) (four items), and total fatigue (TF). Each item has four response alternatives. Higher scores imply more fatigue. The FQ was originally validated in primary care and has been shown to have good face and discriminant validity and good and stable psychometric properties across populations [18, 19]. No specific validation study has been performed in cancer patients, but the instrument has been recommended for use in cancer patients [20]. It has been used in different cancer populations and has demonstrated stable and acceptable psychometric properties similar to reports from noncancer populations.
Physical activity prior to the intervention was assessed by one question asking about physical activity during leisure time over the past year. Two levels of physical activity were specified: (a) a low level of activity (not sweaty and breathlessness) and (b) a high level of activity (sweating and breathlessness). Each level had three response alternatives: (a) none, (b) <1 hour/week, and (c) 1–2 or 3 hours/week. This item is identical to the one used in the North-Trøndelag health study in Norway (http://www.hunt.ntnu.no). This item has been validated and has been demonstrated to have good test–retest reliability. It is therefore judged as a useful measure of leisure-time physical activity and well suited for use in epidemiological studies [21].
Motivation was measured on a 0–10 numerical rating scale (10, maximal motivation). This question was designed specially for this study and has not been formally tested for its measurement capabilities.
Physical Performance Tests
The following four tests were employed to measure physical performance. (a) Sit to stand—an indirect measure of strength in the lower limbs. The test measures how many times the patient manages to stand up and sit down from a chair in 30 seconds [22]. (b) Grip strength—a valid indicator of general health status, which was measured using a Jamar grip dynamometer [23]. (c) Maximal step length—an assessment of balance. The patient was asked to step out as far as possible with one leg in a forward direction while maintaining the stance leg in the initial position, then return to the initial stance position [24]. (d) The Shuttle Walk Test (SWT)—an indirect measure of functional capacity. The SWT is a performance-based, externally paced, progressive walk test and measures how far and how fast the patient is able to walk [25, 26].
Statistical Analyses
The primary endpoint was PF as measured by the FQ. This was chosen based on the results of the pilot study. A two-point difference (10% of the maximum score) was considered clinically significant according to Osoba et al. [27]. Seventy-seven participants per group with 80% power were needed to detect a two-point difference in the PF score (standard deviation, 4.4) with a significance level of .05 (two sided).
The effects of the intervention on each endpoint variable were analyzed using analysis of covariance, that is, linear regression analysis with the post-treatment value as the dependent variable and the intervention and baseline values as covariates. Normal distributions of the residuals were confirmed by visual inspection of Q-Q plots.
Time to survival was measured to control for a possible difference between groups. Survival was compared using the Kaplan–Meier estimator and the log-rank test. Survival was analyzed in separate analyses for all patients, for patients lost to follow-up, and for completers. The effect of treatment on survival was analyzed by Cox proportional hazards regression with intervention as a covariate, without and with adjustment for age, gender, and KPS score. Estimates, 95% confidence intervals (CIs), and two-sided p-values are reported when appropriate.
First, all analyses were done by analyzing only the complete cases (CC analysis). After an analysis for patterns of dropouts, we found a significantly higher dropout rate in the PEG than in the UCG. Hence, data were clearly not missing completely at random (MCAR). Multiple imputation (MI) produces unbiased results provided that data are missing at random (MAR), which is a weaker assumption than MCAR. If data are not MAR, MI generally produces less biased results than CC analysis [28, 29]. Therefore, MI was used for the main analyses. All variables used in the analyses were included in the imputation procedure. The statistician was not blinded to group status.
MIs were performed using imputation by chained equations implemented in Stata with m = 1,000 imputations. Monte Carlo error computations were used to ensure that the number of imputations was sufficient. The imputation model included all variables to be used in the analyses, as well as age, KPS score, and the number of completed exercise sessions. Statistical analyses were performed using SPSS statistical software, version 15.0 (SPSS Inc., Chicago, IL) and Stata 10.1 (StataCorp LP, College Station, TX).
Ethical Considerations
The study was conducted according to the guidelines of the Helsinki Declaration. Data were stored according to regulations set forth by the Norwegian Social Science Data Services. The study was approved by the Regional Committee for Medical and Health Research Ethics, Central Norway. Written informed consent was obtained from all participants.
Results
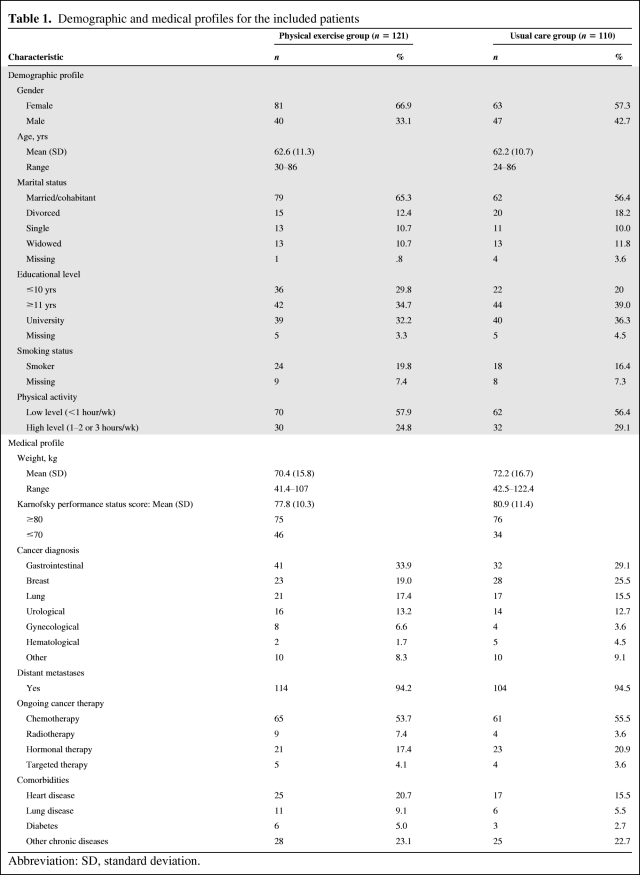
The study flow is presented in Figure 1. In total, 400 patients of convenience were invited to participate between October 2006 and May 2009. In total, 231 agreed to participate and were enrolled and randomized to the PEG (n = 121) or the UCG (n = 110). The numbers of participants in the two groups were unequal as a result of the block randomization. No significant differences were found in terms of gender, age, and KPS score between those who agreed to participate and those who did not. At baseline, the groups were well balanced with respect to demographics, level of physical activity over the past year, and medical characteristics such as diagnosis, ongoing chemotherapy and radiation treatment, and comorbidities (Table 1).
Table 1.
Demographic and medical profiles for the included patients
Abbreviation: SD, standard deviation.
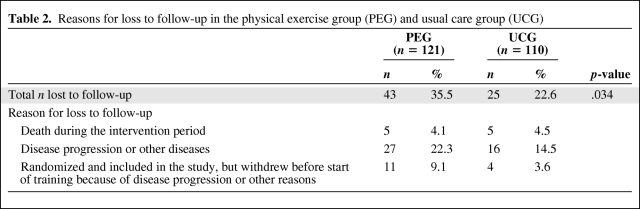
Completion of Intervention
Seventy-eight patients from the PEG and 85 patients from the UCG completed the study. The proportion of patients lost to follow-up was higher in the PEG (35.5%) than in the UCG (22.7%) (p = .034). Reasons for withdrawal are presented in Table 2.
Table 2.
Reasons for loss to follow-up in the physical exercise group (PEG) and usual care group (UCG)
All patients lost to follow-up (n = 68), regardless of group, had significantly lower KPS scores (mean, 75 versus 81; p = .001), lower mean scores on all performance tests (SWT, 287 m versus 393 m: sit-to-stand, 10 times versus 12 times per 30 seconds; grip strength, 25.2 kg versus 28.7 kg; maximal stepping, 83.3 cm versus 90.8 cm) (all p < . 01) and lower motivation (7.3 versus 7.9; p = .06) at baseline than those completing the intervention and the final assessment.
The KPS score (mean, 75), age (mean, 64 years), and physical performance did not differ for those not completing the final assessment between the two groups (PEG versus UCG). Dropouts in the PEG tended to report lower levels of TF (difference, 2.6 points; p = .14) than dropouts in the UCG.
The median survival times for all included patients were 11.1 months (95% CI, 8.1–14.0 months) in the PEG and 12.3 months (95% CI, 8.0–16.5 months) in the UCG (p = 0.18). The median survival times for the dropouts in the PEG and the UCG did not differ significantly—PEG, 6.2 months (95% CI, 3.3–9.2 months); UCG, 5.1 months (95% CI, 3.1–7.1 months) (p = 0.63). Among the patients who successfully completed the intervention, the median survival times were: PEG, 16.3 months (95% CI, 12.6–19.9 months); UCG, 17.1 months (95% CI, 9.7–24.5 months) (p = .39).
The unadjusted hazard ratio for survival (PEG versus UCG) was 1.24 (95% CI, 0.90–1.70; p = .18). After adjustment for age, gender, and KPS score, the hazard ratio was 1.19 (95% CI, 0.86–1.63; p = .30). In the adjusted model, only the KPS score was a significant predictor, with a hazard ratio per 10 points in KPS score of 0.77 (95% CI, 0.66–0.90; p = .001).
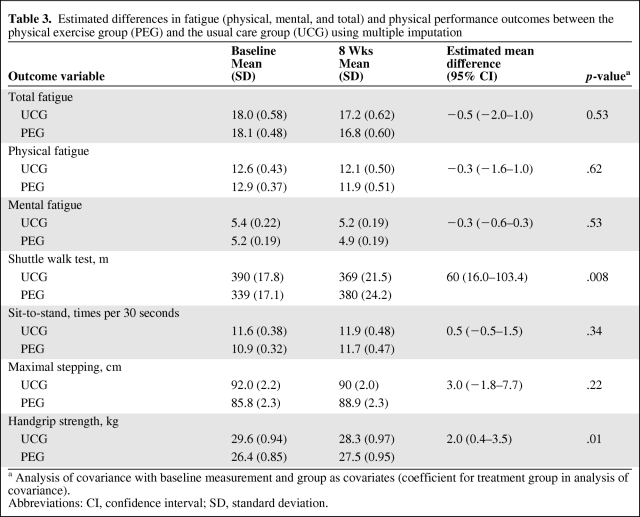
Effects on Fatigue and Physical Performance
After MI for missing data, the regression analysis showed no significant between-groups effect in PF (estimated mean difference [EMD], −0.3; 95% CI, −1.6 to 1.0; p = .62), TF (EMD, −0.5; 95% CI, −2.0 to 1.0; p = .53), or MF (EMD, −0.3; 95% CI, −0.6 to 0.3; p = .53). However, clinically and statistically significant between-groups effects were found in the SWT (EMD, 60 m; 95% CI, 16.0–103.4 m; p = .008) and grip strength test (EMD, 2.0; 95% CI, 0.4–3.5; p = .01) (Table 3).
Table 3.
Estimated differences in fatigue (physical, mental, and total) and physical performance outcomes between the physical exercise group (PEG) and the usual care group (UCG) using multiple imputation
a Analysis of covariance with baseline measurement and group as covariates (coefficient for treatment group in analysis of covariance).
Abbreviations: CI, confidence interval; SD, standard deviation.
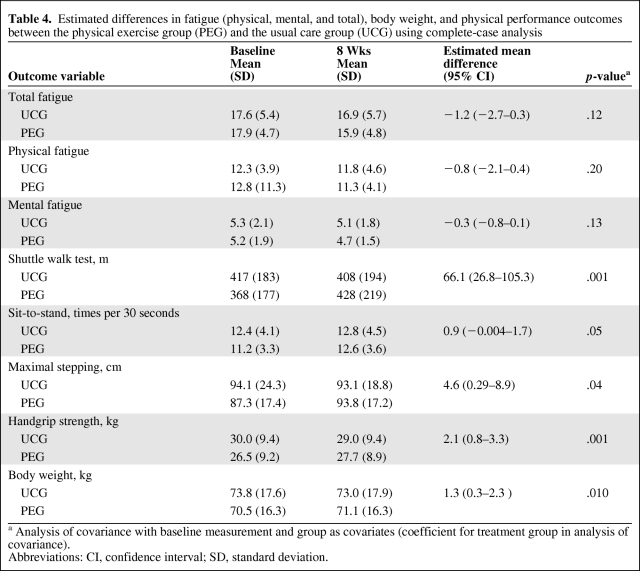
Applying the complete-case approach, the regression analysis showed no significant between-groups effects in either PF (p = .20), TF (p = .12), or MF (p = .13). However, a clinically and statistically significant improvement in physical performance was found for the PEG compared with the UCG for all four performance tests: SWT (p = .001), sit-to-stand test (p = .05), grip strength test (p = .05), and maximal step length (p = .04). There was also a statistically significant difference in change in body weight between the two groups (CC analysis). Patients in the PEG increased their body weight whereas those in the UCG lost weight (p = .01) (Table 4).
Table 4.
Estimated differences in fatigue (physical, mental, and total), body weight, and physical performance outcomes between the physical exercise group (PEG) and the usual care group (UCG) using complete-case analysis
a Analysis of covariance with baseline measurement and group as covariates (coefficient for treatment group in analysis of covariance).
Abbreviations: CI, confidence interval; SD, standard deviation.
The adherence rate for the participants in the PEG who completed the pre- and post-tests was, on average, 69% (11 of 16 scheduled sessions). No exercise-related minor or serious adverse events, such as cardiovascular events or falls with fractures, were reported during or immediately after the sessions.
Discussion
This randomized trial investigating the effects of physical exercise in patients with incurable cancer and a life expectancy of 3 months to 2 years showed improvement in their physical performance as assessed by a hand grip strength test and the SWT, whereas fatigue, the predefined primary endpoint, was not significantly reduced.
The improvements in the physical performance tests indicate that physical exercise can contribute to maintain physical function for at least some time in patients with advanced and progressive disease. Thus, physical exercise is an encouraging intervention to be tested in future studies and possibly also as a part of a treatment program for early cancer cachexia, wherein muscle wasting is considered to be one of the main components of the cachexia syndrome. At present, physical inactivity is assumed to be a contributing factor in this syndrome [10].
All patients had incurable disease and a short life expectancy, and many experienced disease progression over the 8-week intervention period, which might explain why fatigue was not affected. The patients in our cohort had higher levels of fatigue and poorer physical and social functioning at baseline than the patients included in a recently published RCT [8]. In that RCT, a multimodal exercise intervention during cancer treatment reduced fatigue and improved self-reported physical and role functioning [8].
These observations may be an argument to include patients early in the disease trajectory in studies when physical exercise is expected to improve physical function and daily activity and prevent muscle loss.
Fatigue is a complex phenomenon, prevalent in advanced cancer and hypothesized to be influenced by several biological and psychological factors [20]. The mechanism through which exercise reduces fatigue is not fully understood, but a positive effect is probably counteracted by disease progression. In line with this, a recent Cochrane review demonstrated that the strongest effect of exercise on cancer-related fatigue was in patients who were off treatment [7]. In the present study, fatigue was chosen as the primary endpoint based on findings from the pilot study [16]. Theoretically, the lack of a difference between the groups for the primary outcome can be related to the capability of the FQ to detect changes. The level of PF was comparable between these two studies. Choosing fatigue as the primary endpoint was perhaps overoptimistic given the complexity of this symptom. Appropriate physical performance measures are probably more relevant outcomes for future studies of physical exercise in advanced cancer patients.
For ethical reasons, patients could terminate the exercise program at any time without giving any reason. A relatively high proportion of patients were lost to follow-up and significantly more from the exercise group than from the control group were lost to follow-up (35% versus 22%). In exercise interventions for cancer patients with curable disease, dropout rates are in the range of 0%–34% [29]. Based on the findings from our pilot study, we expected a relatively high dropout rate [15]. Alterations in disease manifestations may come abruptly as death approaches. The most common reason for aborting the intervention was disease progression or other serious disease manifestation, and the survival time was significantly shorter for those who did not complete the program than for those who did. Disease progression or altered disease manifestations interfere with the capacity to continue with the training, but to a lesser degree also interfere with the capacity to attend one follow-up assessment, as was the case for the control patients. When the patients left the training because of disease progression, they were also lost to follow-up. We felt it was an unnecessary strain and therefore unethical to assess these patients at that point in time. However, one may also argue that it is necessary to make as complete a follow-up as possible, even in patients with a short life expectancy. In future similar studies and in research on patients with advanced cancer, ethical debates related to complete follow-up should be raised. Data were considered to be not MCAR. Therefore, we found imputation for missing data preferable to the complete-case approach [30].
The randomization was successful in that the two groups were well balanced with respect to variables that might have affected outcomes, such as physical activity level last year and disease and treatment variables. The eligibility criteria were relatively wide, resulting in a heterogeneous sample with respect to performance status and functioning. This is a common feature of the palliative care cancer population. On average, the survival time was about 1 year, but it was only about half a year for those who dropped out. The completers also had significantly better functioning at baseline than those who dropped out. These findings indicate that this specific exercise intervention is less feasible for patients with a life expectancy <6 months.
The length and frequency of the intervention were a compromise between expected disease progression and the minimum amount of exercise required to gain an effect. The content was designed to ensure ease of performance at home and did not presuppose special equipment. The average adherence rate was 69%. Exercise interventions among curable cancer patients have reported adherence rates of 72%–100% [29]. In this context, a 69% adherence rate is regarded as satisfactory, but it also illustrates the specific challenges related to performing regular exercise over time in patients with progressive disease. During the exercise sessions at the hospital, the patients were followed by a physiotherapist to ensure that they performed their program.
Conclusions
Physical performance was clinically and statistically significantly improved after 8 weeks of physical exercise. Physical exercise is an encouraging approach to be applied in future large-scale randomized studies in cancer patients with incurable disease.
Acknowledgments
The study was supported by grants from the Norwegian Foundation for Health and Rehabilitation and the Norwegian Cancer Society.
Line M. Oldervoll and Jon H. Loge share first authorship.
Footnotes
- (C/A)
- consulting/advisory relationship
- (RF)
- Research funding
- (E)
- Employment
- (H)
- Honoraria received
- (OI)
- Ownership interests
- (IP)
- Intellectual property rights/inventor/patent holder
Author Contributions
Conception/Design: Line M. Oldervoll, Jon H. Loge, Stein Kaasa
Provision of study material or patients: Line M. Oldervoll, Jon H. Loge, Hanne Paltiel, May B. Asp, Unni V. Nygaard, Elisabeth Oredalen, Tone L. Frantzen, Ingvild Lesteberg, Lise Amundsen, Dagny F. Haugen, Ørnulf Paulsen, Stein Kaasa
Collection and/or assembly of data: Line M. Oldervoll, Hanne Paltiel, May B. Asp, Unni V. Nygaard, Elisabeth Oredalen, Tone L. Frantzen, Ingvild Lesteberg, Lise Amundsen, Dagny F. Haugen, Ørnulf Paulsen
Data analysis and interpretation: Line M. Oldervoll, Jon H. Loge, Stian Lydersen
Manuscript writing: Line M. Oldervoll, Jon H. Loge, Stian Lydersen, Hanne Paltiel, Marianne J. Hjermstad, Dagny F. Haugen, Stein Kaasa
Final approval of manuscript: Line M. Oldervoll, Jon H. Loge, Stian Lydersen, Hanne Paltiel, May B. Asp, Unni V. Nygaard, Elisabeth Oredalen, Tone L. Frantzen, Ingvild Lesteberg, Lise Amundsen, Marianne J. Hjermstad, Dagny F. Haugen, Ørnulf Paulsen, Stein Kaasa
References
- 1.Jordhoy MS, Fayers P, Loge JH, et al. Quality of life in palliative cancer care: Results from a cluster randomized trial. J Clin Oncol. 2001;19:3884–3894. doi: 10.1200/JCO.2001.19.18.3884. [DOI] [PubMed] [Google Scholar]
- 2.Teunissen SC, Wesker W, Kruitwagen C, et al. Symptom prevalence in patients with incurable cancer: A systematic review. J Pain Symptom Manage. 2007;34:94–104. doi: 10.1016/j.jpainsymman.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Geneva: WHO; 1990. Cancer Pain Relief and Palliative Care: Report of a WHO Expert Committee; pp. 1–75. [PubMed] [Google Scholar]
- 4.Schmitz KH, Holtzman J, Courneya KS, et al. Controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2005;14:1588–1595. doi: 10.1158/1055-9965.EPI-04-0703. [DOI] [PubMed] [Google Scholar]
- 5.Conn VS, Hafdahl AR, Porock DC, et al. A meta-analysis of exercise interventions among people treated for cancer. Support Care Cancer. 2006;14:699–712. doi: 10.1007/s00520-005-0905-5. [DOI] [PubMed] [Google Scholar]
- 6.McNeely ML, Campbell KL, Rowe BH, et al. Effects of exercise on breast cancer patients and survivors: A systematic review and meta-analysis. CMAJ. 2006;175:34–41. doi: 10.1503/cmaj.051073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cramp F, Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2008;(2):CD006145. doi: 10.1002/14651858.CD006145.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Adamsen L, Quist M, Andersen C, et al. Effect of a multimodal high intensity exercise intervention in cancer patients undergoing chemotherapy: Randomised controlled trial. BMJ. 2009;339:b3410. doi: 10.1136/bmj.b3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Speck RM, Courneya KS, Mâsse LC, et al. An update of controlled physical activity trials in cancer survivors: A systematic review and meta-analysis. J Cancer Surviv. 2010;4:87–100. doi: 10.1007/s11764-009-0110-5. [DOI] [PubMed] [Google Scholar]
- 10.Fearon KC. Cancer cachexia: Developing multimodal therapy for a multidimensional problem. Eur J Cancer. 2008;44:1124–1132. doi: 10.1016/j.ejca.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 11.Jordhoy MS, Inger Ringdal G, Helbostad JL, et al. Assessing physical functioning: A systematic review of quality of life measures developed for use in palliative care. Palliat Med. 2007;21:673–682. doi: 10.1177/0269216307083386. [DOI] [PubMed] [Google Scholar]
- 12.Axelsson B, Sjödén PO. Quality of life of cancer patients and their spouses in palliative home care. Palliat Med. 1998;12:29–39. doi: 10.1191/026921698676629560. [DOI] [PubMed] [Google Scholar]
- 13.Santiago-Palma J, Payne R. Palliative care and rehabilitation. Cancer. 2001;92(4 suppl):1049–1052. doi: 10.1002/1097-0142(20010815)92:4+<1049::aid-cncr1418>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 14.Lowe SS, Watanabe SM, Courneya KS. Physical activity as a supportive care intervention in palliative cancer patients: A systematic review. J Support Oncol. 2009;7:27–34. [PubMed] [Google Scholar]
- 15.Oldervoll LM, Loge JH, Paltiel H, et al. Are palliative cancer patients willing and able to participate in a physical exercise program? Palliat Support Care. 2005;3:281–287. doi: 10.1017/s1478951505050443. [DOI] [PubMed] [Google Scholar]
- 16.Oldervoll LM, Loge JH, Paltiel H, et al. The effect of a physical exercise program in palliative care: A phase II study. J Pain Symptom Manage. 2006;31:421–430. doi: 10.1016/j.jpainsymman.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Paltiel H, Solvoll E, Loge JH, et al. “The healthy me appears”: Palliative cancer patients' experiences of participation in a physical group exercise program. Palliat Support Care. 2009;7:459–467. doi: 10.1017/S1478951509990460. [DOI] [PubMed] [Google Scholar]
- 18.Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37:147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- 19.Loge JH, Ekeberg O, Kaasa S. Fatigue in the general Norwegian population: Normative data and associations. J Psychosom Res. 1998;45:53–65. doi: 10.1016/s0022-3999(97)00291-2. [DOI] [PubMed] [Google Scholar]
- 20.Stone PC, Minton O. Cancer-related fatigue. Eur J Cancer. 2008;44:1097–1104. doi: 10.1016/j.ejca.2008.02.037. [DOI] [PubMed] [Google Scholar]
- 21.Kurtze N, Rangul V, Hustvedt BE, et al. Reliability and validity of self-reported physical activity in the Nord-Trøndelag Health Study: HUNT 1. Scand J Public Health. 2008;36:52–61. doi: 10.1177/1403494807085373. [DOI] [PubMed] [Google Scholar]
- 22.Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70:113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- 23.Nordenskiöld UM, Grimby G. Grip force in patients with rheumatoid arthritis and fibromyalgia and in healthy subjects. A study with the Grippit instrument. Scand J Rheumatol. 1993;22:14–19. doi: 10.3109/03009749309095105. [DOI] [PubMed] [Google Scholar]
- 24.Medell JL, Alexander NB. A clinical measure of maximal and rapid stepping in older women. J Gerontol A Biol Sci Med Sci. 2000;55:M429–M433. doi: 10.1093/gerona/55.8.m429. [DOI] [PubMed] [Google Scholar]
- 25.Singh SJ, Morgan MD, Scott S, et al. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax. 1992;47:1019–1024. doi: 10.1136/thx.47.12.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Booth S, Adams L. The shuttle walking test: A reproducible method for evaluating the impact of shortness of breath on functional capacity in patients with advanced cancer. Thorax. 2001;56:146–150. doi: 10.1136/thorax.56.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osoba D, Rodrigues G, Myles J, et al. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16:139–144. doi: 10.1200/JCO.1998.16.1.139. [DOI] [PubMed] [Google Scholar]
- 28.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 29.Oldervoll LM, Kaasa S, Hjermstad MJ, et al. Physical exercise results in the improved subjective well-being of a few or is effective rehabilitation for all cancer patients? Eur J Cancer. 2004;40:951–962. doi: 10.1016/j.ejca.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 30.Fielding S, Fayers PM, Loge JH, et al. Methods for handling missing data in palliative care research. Palliat Med. 2006;20:791–798. doi: 10.1177/0269216306072555. [DOI] [PubMed] [Google Scholar]