Robotic cardiac surgery started in 1997 with the use of a simple, voice-activated, camera-positioning robot (Aesop™).1 Early mitral valve repairs were performed in Paris and Leipzig with use of a prototype of the da Vinci™ surgical system (Intuitive Surgical, Inc.; Sunnyvale, Calif). In the United States, our group purchased the first da Vinci system in 1999, and in 2000 we began robotic mitral valve trials that led to the approval of the system by the U.S. Food and Drug Administration.2 Since then, our unit has performed nearly 700 robotic mitral valve repairs.3,4 This platform has been adopted, with excellent results, by several major centers that now have extensive experience.5 Up-to-date series have proved that durable, complex repairs can be made with acceptable perfusion and arrest times and with low mortality and complication rates. Robotic coronary surgery has not achieved the same level of success or adoption as has mitral valve surgery. Robotic coronary operations are more difficult to perform, and internal thoracic graft patency has not met the open-chest standard. Moreover, the development of efficient arterial connectors has not come to fruition. Finally, on-table graft patency is more difficult to determine with the use of transesophageal echocardiography than is the success of mitral surgery. Nevertheless, several centers perform robotic coronary surgery very well.6
Where Are We with Robotic Cardiac Surgery in 2011?
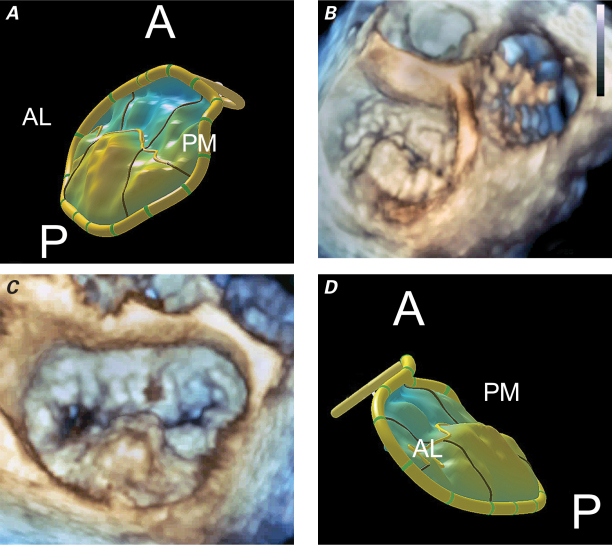
In the United States, several centers for specialized robotic heart surgery are known for receiving a high volume of referrals and achieving high-quality outcomes for particular cardiac operations. It has become evident that the success of a program, whether chiefly focused on mitral valve surgery or coronary surgery, is not predicated solely on having the latest robotic systems, but on fielding dedicated robotic operating teams and the best surgeons. In addition, centers and individual surgeons must have a substantial volume of referred patients in order to attain efficiency and proficiency on a daily basis. Finally, intraoperative 3-dimensional (3-D) echocardiographic imaging must be at the highest level in order to generate “repair blueprints.” We plan robotic mitral repairs by using multiple planar echo views and measurements with derived topographic valvular models (Fig. 1). For robotic coronary operations, surgeons do best in a hybrid operating room, where on-table angiography can be performed to verify graft patency and simultaneous percutaneous revascularization is possible.
Fig. 1 A) Topographic model of P2 and P3 (posterior leaflet prolapse). Posteromedial (PM)-to-anterolateral (AL) projection shows the right fibrous trigone (PM) and left fibrous trigone (AL) in systole. B) Three-dimensional transesophageal echocardiographic reconstruction in the same projection shows the aortic valve just beginning to open after the posterior mitral leaflet prolapses in systole. The tricuspid valve is on the right. C) Three-dimensional transesophageal echocardiographic reconstruction (left atrial frontal view) shows a nearly 3-cm prolapsing segment of P2. D) Topographic model of P2 and P3 (posterior leaflet prolapse): AL-to-PM projection is shown in systole.
A = anterior; P = posterior
We are at a tipping point with regard to robotic cardiac surgery. During the last 10 years, technological advances have been remarkable—we now are using a 3rd-generation robotic device in cardiac surgery. However, total acceptance by surgeons is distant, even though patients are increasingly more aware of the recovery benefits afforded by endoscopic cardiac surgery. As of 2008, although only 20% of mitral valve repairs were performed with the use of any minimally invasive technique, 35.5% of those were robotic. Fewer than 10 centers then performed any more than 20 robotic mitral repairs per year. What are the crucial barriers? In time, robotic technology may transcend the limitations inherent in the surgeon's eye and hand, yielding “augmented human efficacy.” There is no doubt that advances in robotic instrumentation will be very important for progress, but the instrumentation alone will not attain routine use in cardiac surgery.
Where Will Robotic Cardiac Surgery Be in 2031?
Cardiac surgery and cardiology will have changed dramatically by 2031. Only cardiovascular-disease specialists will exist. Many surgical centers are now forming partnerships with cardiologists, and this trend will expand, especially because value-based outcomes will drive reimbursement of costs to a synergistic single entity. This means that care will be delivered through a combination of percutaneous, robotic, and open procedures. We are seeing a re-emerging interest in hybrid coronary operations, wherein the left anterior descending coronary artery is grafted either robotically or through a limited incision, and the remaining vessels are revascularized by means of percutaneous coronary intervention and stenting.6 I predict that robotic cardiac surgery will expand in the next 20 years because of the following:
A new type of cardiovascular specialist
The expansion of hybrid coronary and valvular operations
Advances in robotic technology, such as haptic feedback, smaller instruments and carts, improved or holographic 3-D vision, and catheter-based robots
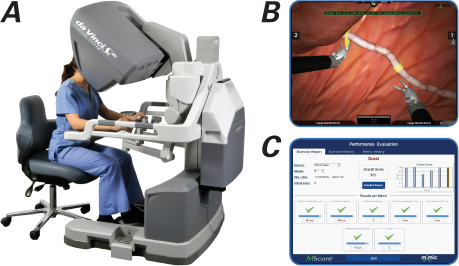
Effective simulation platforms for training and operative planning (Fig. 2)
Advanced 3-D echocardiographic modeling of mitral dysfunction with congruent image registration as a guiding blueprint
Nanotechnology
Faster and smaller computer circuits that will enable faster data transfer.
Fig. 2 A) Surgical trainee operates a da Vinci Si™ robotic simulator. B) The simulator presents various ergonomic challenges that commonly occur during a surgical procedure. C) These movements are scored at the end of the exercise, and the trainee is given opportunities to improve. A learning-curve course can be displayed. (Courtesy of Intuitive Surgical, Inc.; Sunnyvale, Calif)
Predicting the future of robotic cardiac surgery is like forecasting the eventuality of intergalactic space travel: we don't know! However, by analyzing the progress of individual technologies that are needed to achieve full potential, we can infer that cardiac surgical robots will be even more important in 20 years. There is no doubt that in 2031, robotic medical and surgical platforms, as well as cardiovascular specialists, will be completely different from those of today—and this, we can predict!
Footnotes
Address for reprints: W. Randolph Chitwood, Jr., MD, Director, East Carolina Heart Institute, 115 Heart Dr., Greenville, NC 27834
E-mail: chitwoodw@ecu.edu
★ CME Credit
Presented at the 8th Current Trends in Aortic and Cardiothoracic Surgery Conference; Houston, 29–30 April 2011.
References
- 1.Falk V, Walther T, Autschbach R, Diegeler A, Battellini R, Mohr FW. Robot-assisted minimally invasive solo mitral valve operation. J Thorac Cardiovasc Surg 1998;115(2):470–1. [DOI] [PubMed]
- 2.Nifong LW, Chitwood WR, Pappas PS, Smith CR, Argenziano M, Starnes VA, Shah PM. Robotic mitral valve surgery: a United States multicenter trial. J Thorac Cardiovasc Surg 2005;129(6):1395–404. [DOI] [PubMed]
- 3.Chitwood WR Jr, Rodriguez E, Chu MW, Hassan A, Ferguson TB, Vos PW, Nifong LW. Robotic mitral valve repairs in 300 patients: a single-center experience. J Thorac Cardiovasc Surg 2008;136(2):436–41. [DOI] [PubMed]
- 4.Nifong LW, Rodriguez E, Chitwood WR Jr. 540 consecutive robotic mitral repairs and concomitant atrial fibrillation ablation. Ann Thorac Surg. In press. [DOI] [PubMed]
- 5.Mihaljevic T, Jarrett CM, Gillinov AM, Williams SJ, DeVilliers PA, Stewart WJ, et al. Robotic repair of posterior mitral valve prolapse versus conventional approaches: potential realized. J Thorac Cardiovasc Surg 2011;141(1):72–80. [DOI] [PubMed]
- 6.Bonatti J, Schachner T, Bonaros N, Jonetzko P, Ohlinger A, Ruetzler E, et al. Simultaneous hybrid coronary revascularization using totally endoscopic left internal mammary artery bypass grafting and placement of rapamycin eluting stents in the same interventional session. The COMBINATION pilot study. Cardiology 2008;110(2):92–5. [DOI] [PubMed]