Abstract
Stroke causes ischemic brain injury and is a leading cause of neurological disability and death. There is, however, no promising therapy to protect the brain from ischemic stress to date. Here we show an exciting finding that optimal electroacupuncture (EA) effectively protects the brain from ischemic injury. The experiments were performed on rats subjected to middle cerebral artery occlusion (MCAO) with continuous monitoring of cerebral blood flow. EA was delivered to acupoints of “Shuigou” (Du 26) and “Baihui” (Du 20) with different intensities and frequencies to optimize the stimulation parameters. The results showed that 1) EA at 1.0–1.2 mA and 5–20 Hz remarkably reduced ischemic infarction, neurological deficit, and death rate; 2) the EA treatment increased the blood flow by >100%, which appeared immediately after the initiation of EA and disappeared after the cessation of EA; 3) the EA treatment promoted the recovery of the blood flow after MCAO; 4) “nonoptimal” parameters of EA (e.g., <0.6 mA or >40 Hz) could not improve the blood flow or reduce ischemic injury; and 5) the same EA treatment with optimal parameters could not increase the blood flow in naive brains. These novel observations suggest that appropriate EA treatment protects the brain from cerebral ischemia by increasing blood flow to the ischemic brain region via a rapid regulation. Our findings have far-reaching impacts on the prevention and treatment of ischemic encephalopathy, and the optimized EA parameters may potentially be a useful clue for the clinical application of EA.
Keywords: acupuncture, brain protection, infarction, neurological deficits
stroke causes ischemic brain injury and is the leading cause of neurological disability and death in the world. Although prevention and early treatment of this disease are of paramount importance for reducing the devastating effects on individuals and their families, there is no promising therapy to date to protect the brain from ischemic injury. Therefore, finding novel approaches to prevent or treat ischemic injury has attracted the attention of both scientists and clinicians. The umbrella of this mission includes complementary and alternative medicine.
Traditional Chinese medicine has a long history of advocating the use of acupuncture, based on the theory of “meridians” (7, 9, 10), to treat this kind of neurological disorder. The earliest description of the use of acupuncture therapy in stroke appeared in the book of Huangdi Nei Jing (Huangdi's Internal Classic) more than 2000 years ago. More details were described in other ancient traditional Chinese medical books such as Handbook of Prescriptions for Emergencies (Zhou Hou Fang) in the year 281 AD and Essential Prescriptions Worth a Thousand Gold Pieces (Qian Jin Yao Fang) in 680 AD (7). Recently, many medical institutions have reported the use of manual or electroacupuncture (EA) to treat stroke patients effectively (1, 2, 12, 16, 17, 19, 20). Since this treatment modality is relatively convenient and cost efficient, it can be a useful therapeutic option for protecting the brain against stroke or ischemic injury, especially in a case where Western therapy is not immediately available (e.g., at home, during travel, or on the way to the hospital). Due to its repeatability and feasibility of standardization, EA has become more and more popular in both clinical and experimental studies. However, the efficacy of acupuncture treatment for stroke has not yet been subjected to systematic scientific testing with modern techniques. In addition, little is known about its underlying mechanism. In fact, some clinical studies have failed to demonstrate a therapeutic effect of EA/manual acupuncture on stroke (8, 11, 14). Such a major controversy could be attributed to the differences in the parameters (or manner) of acupuncture stimulation, since the selection of proper stimulation parameters is a crucial factor that significantly influences the efficacy of acupuncture. Therefore, it is essential to explore this issue with reliable approaches to determine if EA truly protects the brain from cerebral ischemia with appropriate intensity and frequency of the stimulation.
We therefore proposed this work to address the following three issues. Does EA truly reduce ischemic infarction and improve neurological deficits after cerebral ischemia? Do stimulation intensity and frequency affect EA efficacy? Is the EA efficacy related to the regulation of cerebral blood flow since the primary mechanism of ischemic injury is the insufficient blood supply and the related reperfusion injury? All these fundamental questions remain unanswered because of the understandable limitations of clinical studies.
MATERIALS AND METHODS
Animals.
Adult male Sprague-Dawley rats (250 ± 10 g, ∼postnatal 12 wk) were purchased from the Experimental Animal Center for Shanghai Chinese Academy of Science and housed at an ambient temperature of 24 ± 1°C with free access to food and water. All surgical procedures were performed under anesthesia (chlorate hydrate, 400 mg/kg ip). All animal procedures were approved by the Animal Care and Use Committees of Shanghai Research Center for Acupuncture and Meridians and Fudan University Shanghai Medical College, Shanghai, China.
Monitoring the cerebral blood flow.
A laser-Doppler perfusion monitor (LDPM, PeiFlux5000, Perimed, Jarfalla, Sweden) was used for the measurement of cerebral blood flow. The main procedure was as follows: a little round pore, located 1.5 mm posterior to the bregma and 5 mm lateral to the midline bone seam as described by Nishimura et al. (18), was drilled in the right parietal bone, and then a laser Doppler probe (0.45 mm diameter) was inserted at a depth of 2 mm to approach the superficial microvessels of cerebral pia mater and measure blood perfusion of the cortex as an index of cerebral blood flow. The probe was then fixed on the skull bone. Changes in cerebral blood flow were continuously monitored in all animals starting from at least 5 min before the induction of cerebral ischemia to more than 15 min after reperfusion (until animal revival). According to the manufacturer, change in perfusion values depends on the number of blood cells present in the area illuminated by the probe tip and the speed at which they move. When monitoring with LDPM, dynamic changes in cerebral blood flow in the local area leads to alterations in the blood perfusion, concentration of the moving blood cells (CMBC), and the velocity of blood cells (velocity). Blood perfusion measured by LDPM is automatically expressed as a value of perfusion units (PU), which represent the product of the relative number of moving blood cells and their relative velocities and are the most important index of cerebral blood flow.
Induction of cerebral ischemia.
The model of focal cerebral ischemia was established by performing middle cerebral artery occlusion (MCAO) based on the methods of Longa et al. (4, 15, 24). In brief, rats under anesthesia were surgically operated to expose the right common carotid artery, the external carotid artery, and the internal carotid artery. After ligating the distal end of the right external carotid artery, it was incised and a segment of 4–0 monofilament nylon suture (30 mm length, 0.18 mm diameter with a 0.24 mm diameter round tip, MONOSOF, SN-1699G) was inserted from the right external carotid artery into the right internal carotid artery for a length of ∼20 mm (reaching the origin of the right middle cerebral artery) to occlude the blood flow of the right middle cerebral artery.
To standardize our experimental conditions for all groups, we constantly monitored the blood flow in all animals to make sure that a relatively uniform level of cerebral ischemia existed before the experiments. The blood flow was controlled by adjusting the suture in the artery for the induction of ischemia. The ischemic rats that showed a stable drop of ∼85% in PU compared with the baseline level (before MCAO), i.e., reaching a level of ∼15% of the baseline PU, were used for further experimentation. This ischemic condition was kept constant with minor fluctuations during the whole ischemic period without any significant change except during EA application. After the occlusion, reperfusion of the ischemic area was allowed by withdrawing the suture from the right external carotid artery. Changes in the cortical blood flow were constantly monitored in all animals beginning at least 5 min before MCAO and continuing up to 15 min after reperfusion (until animal recovered from the anesthesia). This period included the entire course of MCAO as well as the full length of EA.
Body temperature was monitored by a rectal thermometer and maintained at 36.5 ± 0.5°C from the initiation of the surgical procedures till the animal recovered from anesthesia. After the reperfusion, the animals were housed for 24 h at an ambient temperature of 24 ± 1°C. In a sham-operation group, the same surgical procedures were carried out, excluding occlusion of the artery.
Application of electroacupuncture.
EA was applied to “Shuigou” and “Baihui” (Du 26 and Du 20 according to WHO standard names, respectively) since they were proven to be effective in our pilot study (26). Specifically, Shuigou (Du 26) is in the center of the upper lip, a point at a distance of 2/3 from the mouth to the nose, and Baihui (Du 20) is in the midline of the head, approximately at the midpoint of the line connecting the apexes of the two auricles. The depth of needle on Du 26 is 1 mm vertically to the skin and Du 20 is 2 mm obliquely. EA was started at 5 min after the onset of MCAO and was continued for 30 min. It was delivered through stainless steel filiform needles (15 mm length with 0.3 mm in diameter, Suzhou Medical Apparatus Limit) by an EA apparatus (Model G-6805-II, Shanghai Medical Instruments High-Tech, Shanghai). This EA apparatus has been widely used in the practice of clinical acupuncture in traditional Chinese medicine. The intensity and frequency of the output waves, with negative-going pulse on the posterior border (pulse width = 0.5 ± 0.1 ms; component of direct current = 0), were monitored via a general oscillograph (Model XJ4210A, Shanghai XinJian Instrument and Equipment). Different intensities (0–1.2 mA) and frequencies (1–100 Hz) were used to differentiate their effects on cerebral ischemia. Each parameter was tested more than 12 times in at least six independent rats. Finally, to achieve a strict control, we applied comparable EA on sham-ischemic rats and detected changes in cerebral blood flow (n = 8) to investigate if EA has an effect on cerebral blood flow in nonischemic brains.
Evaluation of death rate and neurological deficits.
In our experiments, some ischemic rats died between 2 and 20 h after reperfusion. The death rates were calculated based on the number of dead rats within this period and the total number of rats in a given group. Although the death could be attributed to multiple causes including hemorrhage, we did not investigate the cause of death during this particular work as our aim here was to compare the death rates among various groups.
Neurological behaviors were evaluated in all groups, excluding the rats that died within 24 h after MCAO. Neurological deficits were evaluated at 24 h after the reperfusion (right before sampling brain tissue for detection of ischemic infarction). The evaluation of neurological deficits was blinded, i.e., the one who judged and scored the degree of neurological deficits according to the pre-set criteria did so without any knowledge about the grouping and treatments. The degree of neurological deficits was graded from 0 to 7 (5, 25). The criteria were set as follows: grade 0 (“normal”), symmetrical movement without any abnormal sign; grade 1, incomplete stretch of the left anterior limb when the tail was lifted up; grade 2, doddery crawl in addition to the signs of grade 1; grade 3, kept the left anterior limb close to the breast when the tail was lifted up; grade 4, left turn when crawling; grade 5, left anterior claw pushed backward along with signs of grade 4; grade 6, repeated rotational motion with an immotile posterior left limb; and grade 7, left recumbent position because of body supporting incapability.
Measurement of cerebral infarct volume.
Following the evaluation of neurological deficits at 24 h after reperfusion, the rats were killed rapidly under anesthesia and their brains were sliced into 2.0-mm sections. The brain slices were incubated in a solution of triphenyltetrazolium chloride (20 g/l) for 30 min at 37°C and then transferred into paraformaldehyde solution (40 g/l) to fix the area of infarct. The infarct region presented as white in color while “normal” tissue showed up in red (3, 9). The images of the brain slices were taken with a digital camera attached to a computer system. The area/volume of infarct was analyzed by a computer-assisted image system with ACT-2U software (Nikon). Relative infarct ratio was calculated using the following equation (22): {2·[left hemisphere area (nonischemic side) of whole brain slices − noninfarct area of whole brain slices]/2·left hemisphere areas}·100%. This equation excludes the factors that could result in an inaccurate calculation of the infarct volume (such as edema).
Data analysis.
Cerebral blood flow was determined by the measurements of PU, CMBC, and velocity. All the values in each animal were compared with the base values, measured before MCAO, which was considered as 100% (control level). Then the grouped values were compared among various groups. Neurological deficits were evaluated and expressed as an average value of the grade per group. Cerebral infarct volume was expressed as a percentage of the whole cerebrum.
All data are presented as means ± SD and subjected to statistical analysis. The rate of death was compared using Chi-square test. All other data were subjected to ANOVA, t-test, rank sum test, and/or Chi-square test. The changes were considered as significant if the P value was <0.05.
RESULTS
MCAO-induced brain injury increased with ischemic duration.
To yield reliable data in the model of local cerebral ischemia, we first performed a number of experiments to establish the standard experimental conditions. We observed that a reduction of blood flow by ∼85% caused consistent injury to the brain and an increasing degree of injury with an increase in the ischemic duration from 30 to 60 min (Table 1 and Fig. 1).
Table 1.
Effect of MCAO durations on ischemic brain injury
| Group | Neurological Deficit | Infarct Volume | Death Rate |
|---|---|---|---|
| MCAO-30min | 1.0 ± 0.5 (0∼2) (n = 12) | 9.5%±2.2% (n = 12) | 0 (0 out of 12) |
| MCAO-45min | 4.0 ± 1.0 (3∼5) (n = 30)Δ | 22.6%±2.7% (n = 12)☆ | 0 (0 out of 30) |
| MCAO-60min | 6.0 ± 1.0 (5∼7) (n = 25)Δ | 33.4%±3.1% (n = 12)☆ | 16.7% (5 out of 30)▾ |
ΔP < 0.01 vs. middle cerebral artery occlusion (MCAO)-30 min (rank-sum test). ☆P < .0.01 vs. MCAO-30min (t-test). ▾P < .0.01 vs. MCAO-30 min (χ2 test). Note that the death rate, neurological deficit, and infarct volume increased with the duration of MCAO.
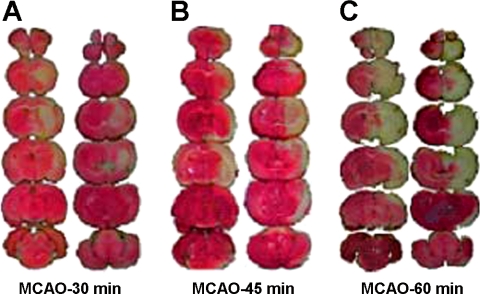
Fig. 1.
The infarct volume increased with the duration of middle cerebral artery occlusion (MCAO). The brain slices were subjected to triphenyltetrazolium chloride (TTC) staining at 24 h after reperfusion following MCAO and the ischemic infarct volume was quantified by a computerized image system. The slices on the right of each column show the backside of the left slices. Note that the infarct regions (pale white portion) were mainly located in the striatum and frontoparietal cortex in the right hemisphere and the volume of the ischemic infarction was largely enlarged when MCAO was extended from 30 min (A) to 60 min (C). After 60 min of MCAO, the infarction volume was >1/3 of the whole brains.
In the rats exposed to MCAO for 30 min (MCAO-30min, n = 12), none of the 12 animals died within 24 h after the reperfusion. They demonstrated an average volume of ischemic infarction of 9.5 ± 2.2% (n = 12) with a slight neurological deficit (grades 0∼2, n = 12; Table 1 and Fig. 1A). The infarct area was mainly localized in the striatum along with a small portion of the frontoparietal lobe of the cortex in the right hemisphere (ischemic side, Fig. 1A).
In the group of rats exposed to MCAO for 45 min (MCAO-45min, n = 30), although all 30 rats survived, the infarct volume increased to 22.6 ± 2.7% (P < 0.01 vs. MCAO for 30 min, n = 12) with a moderate increase in severity of neurological deficits (grades 3∼5, n = 30). The infarct area extended to most of the regions of the frontoparietal lobe of the ischemic side (Fig. 1B).
After 60 min of MCAO (MCAO-60min, n = 30), 16.7% of the rats (5/30) died within 2–20 h after reperfusion. At 24 h after the reperfusion, the remaining alive rats showed serious neurological deficits (grade 6.5 ± 0.5, n = 25) with the area of the brain infarction around one-third of the whole brain (33.4 ± 3.1%, n = 12, P < 0.01 vs. MCAO-30min; P < 0.01 vs. MCAO-45min; Table 1 and Fig. 1C). The ischemic side was found to be very swollen (Fig. 1C).
Blood flow recovery after reperfusion was dependent on ischemic duration.
We characterized the changes in the blood flow in our models after reperfusion. When the suture was adequately sutured, an immediate decrease in blood perfusion by ∼85% (from 100 ± 20 to 13 ± 2 PU) was noted. During the whole period of occlusion, the blood flow was kept at this low level with minor fluctuations. As the blood perfusion was mainly determined by the concentration of moving blood cells (CMBC) and the velocity of the blood cells (velocity), we also monitored the changes in these values and found that CMBC dropped by 80% with a relatively slight deceleration in blood cell movement (25% of the base value). These changes suggest that the MCAO-induced reduction in blood volume was greater than the decrease in blood cell velocity during MCAO (Fig. 2).
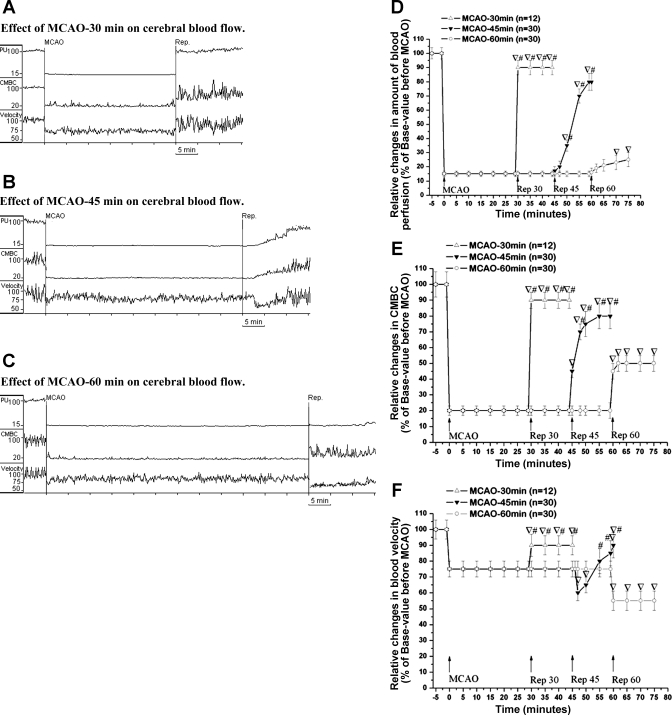
Fig. 2.
Prolonged MCAO delayed the recovery of blood flow to the brain after MCAO. A–C: trace recordings of the blood flow in the ischemic brains. D–F: statistical data in all groups. Blood perfusion (PU), concentration of moving blood cells (CMBC), and velocity of blood cells (Velocity) were measured in the ischemic brains exposed to MCAO for 30 min, 45 min, and 60 min, respectively. ∇P < 0.01, reperfusion vs. MCAO; #P < 0.01, reperfusion in groups of MCAO-30min and MCAO-45min vs. that of MCAO-60 min. Note that MCAO immediately decreased PU to ∼15% and CMBC to 20% of the base value with a slight decrease in the Velocity (−25%) in all groups. The blood flow was relatively stable at a low level during the whole period of MCAO. After the onset of reperfusion, the blood flow rapidly increased to the preischemic level in the group of MCAO-30min. However, this increase was much slower in the MCAO-45min group. After a prolonged period of MCAO (60 min), the blood flow was still very low in the first 15 min after reperfusion. Rep 30, Rep 45, Rep 60, reperfusion after 30 min, 45 min or 60 min of MCAO.
All the groups, whether MCAO-30min, MCAO-45min, or MCAO-60min, showed identical changes in the blood flow during MCAO (Fig. 2). However, a major difference was observed during the recovery after reperfusion (Fig. 2). In the group of MCAO-30min, the blood flow recovered quickly and almost immediately reached a level that was >90% of the preischemic level of all the measured parameters (PU, CMBC, and velocity, Fig. 2A and D–F). In the MCAO-45min group, the blood flow was low during the first 5 min after reperfusion and then gradually increased to the level 80% of the preischemic level at 15 min after the reperfusion (Fig. 2, B and D–F). In contrast, after 60 min of MCAO, the recovery of the blood flow was largely delayed with the blood flow reaching ∼25% of the preischemic values in the first 30 min of reperfusion (Fig. 2, C and D). At the same time, the recovery of CMBC increased to ∼50% (Fig. 2, C and E) of the preischemic level and the velocity decreased from 75 to 50% of the preischemic level (Fig. 2, C and F, P < 0.01). These results suggest that the longer the duration of MCAO the slower the recovery of blood flow after reperfusion. Because MCAO-60min led to a stable death rate, neurological deficit, and brain infarction, we chose to study the EA effect under these ischemic conditions.
EA increased blood flow in the ischemic brain.
Since the primary cause of ischemic injury is insufficient blood flow to the affected brain region, we therefore asked if EA can accomplish neuroprotection against cerebral ischemia through the regulation of the blood supply to ischemic region. As intensity and frequency were two important parameters of EA, we compared various intensities and frequencies of EA in terms of their effects on the blood flow in the ischemic brain.
First, we examined the effects of EA intensity on the blood flow (Fig. 3) and found that an intensity of <0.6 mA with 5/20 Hz did not induce any significant change in the blood flow. When the intensity was enhanced from 0.6 to 0.8 mA, there was a significant increase in the blood flow with EA. The blood flow further increased when the intensity was enhanced to 1.0 mA. As shown in Fig. 3C, PU during EA were more than 100% higher than that during the non-EA period (P < 0.05). However, the intensity at 1.2 mA failed to boost a further increase in the blood flow (Fig. 3). The EA-induced increase in the blood flow was isochronous to the current impulse in response to EA stimulation and disappeared immediately after discontinuing EA. These data suggest that EA induces a temporal increase in the blood flow, with an intensity between 1.0 and 1.2 mA being the optimal range.
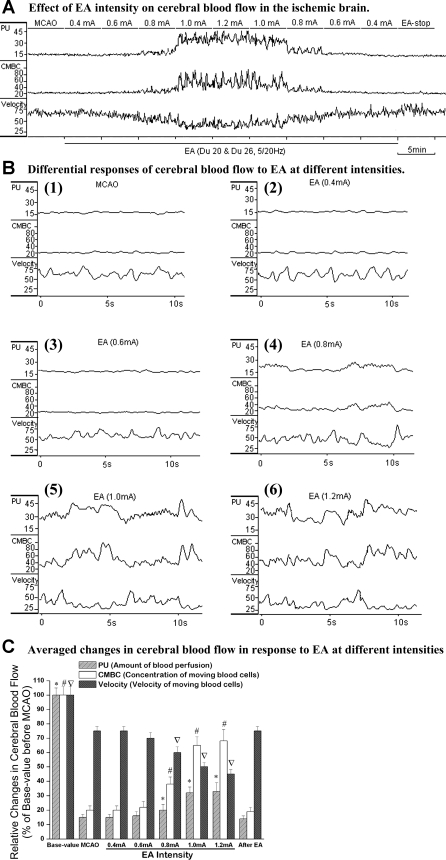
Fig. 3.
The electroacupuncture (EA)-induced changes in the blood flow varied with EA intensity. A: comparative view of changes in CBF. B: changes in the blood flow in response to EA at different intensities. C: statistical summary of the changes in the blood flow in response to EA stimuli. *P < 0.01, MCAO vs. MCAO plus EA (PU). #P < 0.01, MCAO vs. MCAO plus EA (CMBC). ∇P < 0.01, MCAO vs. MCAO plus EA (Velocity). The frequency of EA was 5/20 Hz. Note that EA at >0.6 mA could induce an isochronous increase in PU and CMBC with a decrease in Velocity. Within the ranges of 0.6∼1.2 mA, the EA-induced increase in the blood flow was proportional to the increase in the EA intensity.
To clarify the relationship between EA frequency and the blood flow, we determined effects of EA at different frequencies (2–100 Hz) on the blood flow in the ischemic brain. Based on the above data, the EA intensity was used at 1.0 mA. The EA-induced increase in the blood flow was dependent on EA frequency. EA given at a frequency up to 40 Hz could increase blood flow with a significant effect seen between 2 and 20 Hz. When the frequency changed from 2 to 20 Hz, EA induced an increase in PU and CMBC with an accompanying decrease in velocity. However, when the frequency was changed from 30 to 40 Hz, the EA-induced change in PU and CMBC greatly reduced with a much less decrease in velocity. Furthermore, EA at 40 Hz induced only a marginal increase in the blood flow, while EA at more than 40 Hz led to no/little change in the blood flow (Fig. 4). These results suggest that the EA-induced increase in the blood flow is very sensitive to electrical frequency, with 5–20 Hz being the optimal frequency.
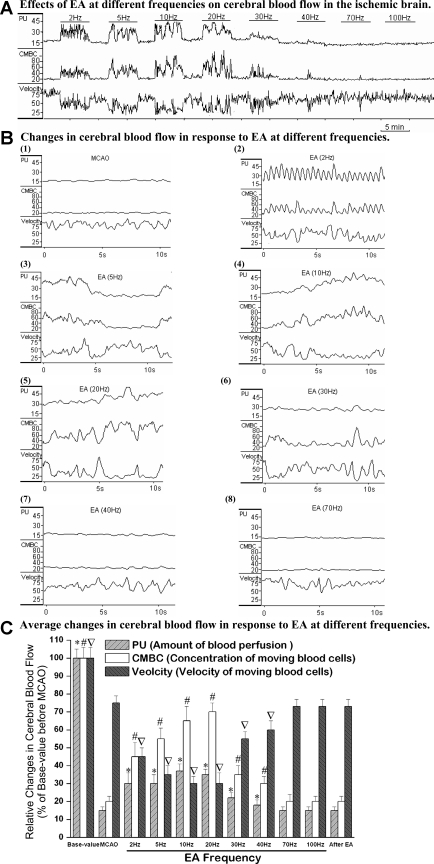
Fig. 4.
The EA-induced change in the blood flow was dependent on frequency of EA stimulation. A: comparative view of the blood flow during EA stimulation with different current frequencies. B: changes in the blood flow in response to EA at different frequencies. C: statistical summary of the changes during the EA treatment. *P < 0.01, MCAO vs. MCAO plus EA (PU). #P < 0.01, MCAO vs. MCAO plus EA (CMBC). ∇P < 0.01, MCAO vs. MCAO plus EA (Velocity). Note that EA at <30 Hz significantly increases the CBF with the best effect seen between 2 and 20 Hz, while a higher frequency (>40 Hz) did not induce any appreciable increase in the blood flow.
EA protection against cerebral ischemia depended on stimulation intensity and frequency.
Since the EA-induced increase in the blood flow of the ischemic brain was dependent on appropriate EA intensity and frequency, we further asked whether the “optimal” parameters resulted in a better neuroprotection against cerebral ischemia by comparing the three EA parameters and determining their effects on ischemic injury. These parameters were as follows: 1) “optimal” intensity and frequency (1.0 mA, 5–20 Hz), 2) “optimal” intensity and “nonoptimal” frequency (1.0 mA, 70 Hz), and 3) “nonoptimal” intensity and “optimal” frequency (0.4 mA, 5–20 Hz).
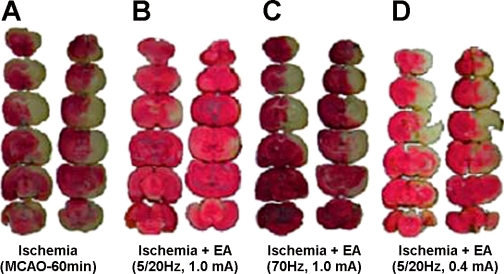
As shown in Table 2 and Fig. 5, the optimal intensity and frequency remarkably reduced the neurological deficits from grade 6.0 ± 1.0 (n = 25) to 1.0 ± 1.0 (n = 28; P < 0.01), the death rate from 16.7% (5/30) to 6.7% (2/30; P < 0.01), and the infarct volume from 33.4 ± 3.1% (n = 12) to 4.9 ± 1.2% (n = 12; P < 0.01). In sharp contrast, the optimal intensity with nonoptimal frequency and nonoptimal intensity with optimal frequency did not induce significant changes in neurological deficit, death rate, and the infarct volume.
Table 2.
Effects of EA at different parameters on cerebral ischemia
| Group | Neurological Deficit | Infarct Volume | Death Rate |
|---|---|---|---|
| Ischemia | 6.0 ± 1.0 (5 ∼ 7) (n = 25) | 33.4 ± 3.1% (n = 12) | 16.7% (5 out of30) |
| Ischemia+EA | 1.0 ± 1.0 (0 ∼ 2) (n = 28)Δ | 4.9 ± 1.2% (n = 12)☆ | 6.7% (2out of 30)▾ |
| Ischemia+EA (0.4 mA) | 6.0 ± 1.0 (5 ∼ 7) (n = 10) | 32.3 ± 4.5% (10) | 16.7% (2 out of 12) |
| Ischemia+EA (70 Hz) | 6.0 ± 1.0 (5 ∼ 7) (n = 10) | 34.3 ± 5.4% (10) | 16.7% (2 out of 12) |
Ischemia, rats were subjected to right MCAO for 1 h and reperfusion for 24 h. Ischemia+EA, electroacupuncture (EA; 1.0 mA, 5/20Hz, sparse-density wave) was delivered to the acupoints of Baihui (Du 20) and Shuigou (Du 26) of the ischemic rats for 30 min. Ischemia+EA (0.4mA): EA (0.4 mA, 5/20 Hz, sparse-density wave) was delivered to the acupoints of Baihui (Du 20) and Shuigou (Du 26) of the ischemic rats for 30 min. Ischemia+EA (70 Hz): EA (1.0 mA, 70 Hz) was delivered to the acupoints of Baihui (Du 20) and Shuigou (Du 26) of the ischemic rats for 30 min. All EA treatments started at 5 min after the onset of MCAO. ΔP < 0.01 vs. Ischemia (rank-sum test). ☆P < 0.01 vs. Ischemia (t-test). ▾P < 0.01 vs. Ischemia (χ2 test). Note that EA with suitable parameters significantly reduced the neurological deficit, brain infarct volume, and death rate but EA with lower intensity or higher frequency did not reduce the neurological deficit, brain infarct volume and death rate.
Fig. 5.
The EA-induced reduction of the infarct volume was dependent on appropriate EA parameters. The brain slices were subjected to TTC staining. Note that the infarct region (pale white portion) was mainly located in the striatum and frontoparietal cortex in the right hemisphere. The MCAO-caused infarction (A) was significantly reduced by EA treatment at “optimal” parameters (B). In contrast, inadequate parameters of EA, e.g., high frequency (C) and low intensity (D) had no protection from the cerebral infarction.
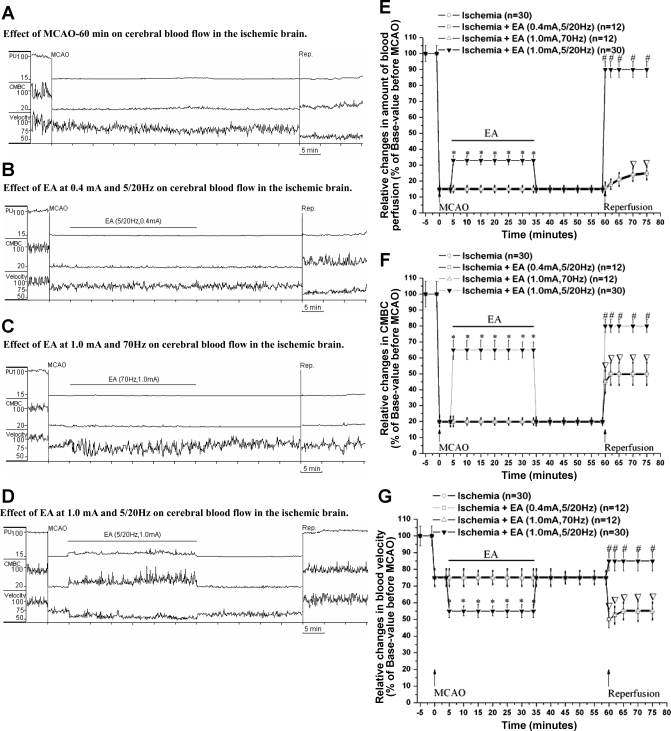
In these groups, the blood flow changes paralleled the efficacy of the EA-induced protection. With optimal intensity and frequency, EA induced a significant increase in PU (from ∼15 to ∼30% of base level) and CMBC (from ∼20 to ∼65% of base level; P < 0.01 vs. MCAO without EA) with a significant decrease in velocity (from ∼75% of base level to ∼55%). Although this effect immediately disappeared after the termination of EA, during reperfusion the EA group showed a faster recovery of blood flow to the preischemic level (Fig. 6). In the group of optimal intensity and nonoptimal frequency (1.0 mA, 7 0 Hz) and that of nonoptimal intensity and optimal frequency (0.4 mA, 5/20 Hz), we did not observe these positive changes in the blood flow (Fig. 6).
Fig. 6.
Different EA parameters differentially alter the cerebral blood flow. PU, CMBC, and Velocity were measured in the ischemic rats by a Laser Doppler Perfusion Monitor system. A, MCAO-60min; B, EA at 0.4 mA and 5/20 Hz; C, EA at 1.0 mA and 70 Hz; D, EA at 1.0 mA and 5/20 Hz. E–G: summary data of PU, CMBC, and Velocity in all groups. *P < 0.01, MCAO+EA vs. MCAO. ∇P < 0.01, reperfusion vs. MCAO. #P < 0.01, reperfusion in MCAO+EA group vs. reperfusion in MCAO group. Note that the PU and CMBC decreased immediately after MCAO. Neither EA at 0.4 mA and 5/20 Hz nor EA at 1.0 mA and 70 Hz induced any significant change in the blood flow during and after MCAO. In contrast, EA at 1.0 mA and 5/20 Hz increased PU by 2∼3-fold and CMBC by 3∼4-fold with a decrease in Velocity to 50% of that in MCAO. In addition, the “optimal” EA promoted PU, CMBC and Velocity to return to the preischemic level.
EA had no appreciable effect on cerebral blood flow in the nonischemic brain.
Since EA significantly increased the blood flow in the ischemic brain, we wondered whether this is a general response of the brain to EA stimulation or a specific reaction of the ischemic brain to EA. We applied EA at 1.0 mA with different frequencies (2–70 Hz) on the age-matched naive rats and measured changes in the cerebral blood flow (n = 8). Interestingly, we found that EA, at the parameters used in the ischemic rats, had no significant effect on the cerebral blood flow in the naive animals (Fig. 7).
Fig. 7.
EA had no significant effect on cerebral blood flow in the naive brain without ischemia. PU, CMBC, and Velocity were measured in the brain in the same way as in the ischemic brain. A: effects of EA at 1.0 mA with different frequencies (2–70 Hz) on the CBF. B: statistical summary. Note that EA had no significant effect on PU, with a slight decrease in Velocity in response to EA at different frequencies.
DISCUSSION
This is the first study systemically investigating the effects of EA at different current parameters on cerebral ischemia. We have reported two major findings: 1) EA at an appropriate intensity and frequency could reduce ischemic infarction, neurological deficit, and death rate and 2) EA at optimal parameters, increased cerebral blood flow in the ischemic brain but not in the naive brain. These exciting observations suggest that appropriate EA treatment protects the brain from cerebral ischemia by increasing blood flow to the ischemic brain region.
The brain is extremely susceptible to ischemia because of the huge energy demands and poor O2 and energy stores (6, 13, 21, 23, 27). A certain period of ischemic stress may cause mismatch between the demand and production of energy, and cause disruption of ionic homeostasis and dysfunction of neuronal excitability and synapse transmission, eventually resulting in neuronal injury and death by triggering intracellular death signals. Consequently, such serious outcomes result in brain edema, infarction, neurological deficits, and even death. It is apparent that the duration and/or severity of ischemia are critical in causing brain injury secondary to cerebral ischemia and also for the reliability of data generated from the ischemic model. A change in the duration or severity of ischemic duration may greatly alter the outcome of the neural injury. In the present study, a stable model of ischemic injury is extremely important for the successful evaluation of EA effect on cerebral ischemia. For this purpose, we spent huge efforts to evaluate the influencing factors and improve the procedures for the animal modeling and thus finally optimized the experimental conditions for a relatively stable outcome of the ischemic model as described in methods and results. A stable model of cerebral ischemia was generated in our strict experimental conditions. Our data showed that the ischemic infarction, neurological deficit, and rate of death were fairly proportional to the duration of MCAO, while EA treatment with appropriate intensity and frequency largely reduced the volume of ischemic infarction with a decrease in the death rate and neurological deficit. The results based on our large database give us great confidence in the fact that EA at suitable electrical parameters can provide protection against injury from cerebral ischemia. This is an exciting finding with potentially far-reaching significance in medical science and the clinical practice because there is no effective strategy for prevention or treatment of ischemic injury in the brain at present.
Although the mechanisms underlying the EA-induced protection involve multiple factors in the brain and may be very complex, e.g., regulation of opioid system (9), our work has shown that an increase in blood supply to the ischemic region plays a key role in the neuroprotection against ischemia. In our experimental model, the blood flow doubled in the ischemic region during the period of EA application. Such an increase is self-explanatory in terms of its significance in neuroprotection from ischemic injury. In addition, EA improved the reperfusion after MCAO and quickly restored the level of cerebral blood flow closer to the baseline, which certainly helps the recovery of the brain from ischemic injury. Our work showed that the blood reperfusion after ischemia seemed to be dependent on the ischemic severity. For example, the blood flow rapidly returned to the preischemia level after reperfusion of the brain exposed to a relative short-term ischemia (e.g., 30 min of MCAO), while the course was much delayed in the brain exposed to long-term ischemia. However, the delayed speed of reperfusion could be increased to a great extent after EA treatment. The mechanism is likely to be related to the increase in the blood flow during EA treatment because it reduced ischemic severity. Clearly, the EA-induced increase in the blood flow is specific to the ischemic brain since it did not show these changes in the naive brains of the control animals.
The EA-induced increase in the blood flow in the ischemic brain is related to a rapid mechanism, though unclear at present, because of the characteristics of the phenomenon, i.e., a rapid and synchronous change with EA application. It is less likely to be mediated by humoral regulation, which is a relatively slow and prolonged process (e.g., blood endothelium or CO2-induced autoregulation of cerebral vessels). Since we inserted the needles at acupoints of Du 20 and Du 26 and the current passed through the two acupoints, we could not exclude the possibility that the current directly stimulated the cerebral vessels. Interestingly, we saw a similar phenomenon in the ischemic brain by stimulating acupoints other than the head acupoints (unpublished data). It has been well recognized that EA signal transmission goes through afferent nerves (18, 28). Therefore, it is reasonable to assume that the EA effect was sensitive to electrical parameters because an under- or overstimulation might not appropriately generate suitable EA signals through the nervous system. More recently, we also found that the EA effect is acupoint specific (unpublished data). However, it is currently unknown if EA stimulation could dilate the blood vessels in the ischemic region via the central integration of afferent and efferent signals. The exact underlying mechanism still remains unclear. On the other hand, the EA neuroprotection against ischemic injury could be a complex process. In addition to increasing cerebral blood flow, EA could also involve and regulate the neurotransmitters in an ischemic brain (9).
Nevertheless, the resultant outcome of EA is beneficial for an ischemic brain. We believe that the optimization of EA parameters at appropriate acupoints could prove to be a suitable platform for future application of EA in the treatment of ischemic brain injury.
Conclusion.
We made novel observations on the effect of acupuncture on cerebral ischemia. Through a systematic study, we found that electroacupuncture at appropriate intensity (∼1.0 mA) and frequency (5–20 Hz) effectively increases the blood flow in the ischemic brain region and improves blood reperfusion after the ischemia, thus reducing ischemic infarction, neurological deficits, and death rate. The EA-induced increase in the blood flow was specific in the ischemic brain because it was not seen in the naive brain. It is our belief that the present data will have a significant and wide-ranging impact on the prevention and treatment of ischemic encephalopathy.
GRANTS
This work was supported by National Natural Science Foundation of China (30672721), National Basic Research Program of China (12CB518502) Science and Technology Commission of Shanghai Municipality (09DZ1974303, 10DZ1975800), and National Institutes of Health (AT-004422 and HD-034852).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
REFERENCES
- 1. Alexander DN, Cen S, Sullivan KJ, Bhavnani G, Ma X, Azen SP. Effects of acupuncture treatment on poststroke motor recovery, and physical function: a pilot study. Neurorehabil Neural Repair 18: 259–267, 2004 [DOI] [PubMed] [Google Scholar]
- 2. Bai HM, Zhang YL, He JW, Zhang LC, Yang Y. Observation on therapeutic effect of comprehensive therapy for acute large area cerebral infarction. Zhong Guo Zhen Jiu 28: 98–100, 2008 [PubMed] [Google Scholar]
- 3. Bederson JB, Pitts LH, Germand SM. Evaluation of 2,3,5-triphenyltetrazolium chloride as a stain for detection and quantification of experimental cerebral infaction in rats. Stroke 17: 1304–1308, 1986 [DOI] [PubMed] [Google Scholar]
- 4. Borlongan CV, Hayashi T, Oeltgen PR, Su TP, Wang Y. Hibernation-like state induced by an opioid peptide protects against experimental stroke. BMC Biol 17: 7:31, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cai DF. Clinical, and experimental study on Xingnaojing injection in treating acute ischemia cerebral apoplexy. J Emerg Syndromes Chinese Med 9: 45–47, 2000 [Google Scholar]
- 6. Chao DM, Xia Y. Ionic storm in hypoxic/ischemic stress: Can opioid receptors subside it? Prog Neurobiol 90: 439–470, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen YH, Lin XW, Fang JQ. Apoplexy. In: Contemporary Research of Acupuncture and Moxibustion Therapy on Stubborn Diseases, edited by Wu HG, Fang JQ, Wang QQ. Shanghai: Publishing House of Shanghai Science and Technology, 2002 [Google Scholar]
- 8. Gosman-Hedström G, Claesson L, Klingenstierna U, Carlsson J, Olausson B, Frizell M, Fagerberg B, Blomstrand C. Effects of acupuncture treatment on daily life activities, and quality of life: a controlled, prospective, and randomized study of acute stroke patients. Stroke 29: 2100–2108, 1998 [DOI] [PubMed] [Google Scholar]
- 9. Guo JC, Cheng JS, Xia Y. Acupuncture therapy for stroke. In : Acupuncture Therapy for Neurological Diseases: A Neurobiological View, edited by Xia Y, et al. New York: Springer-TUP, 2010, p. 226–262 [Google Scholar]
- 10. Greten J. Kursbuch Traditionelle Chinesische Medizin: TCM Verstehen und Richtig Anwenden. New York: George Thieme Verlag Stuttgart, 2004 [Google Scholar]
- 11. Hopwood V, Lewith G, Prescott P, Campbell MJ. Evaluating the efficacy of acupuncture in defined aspects of stroke recovery: a randomised, placebo controlled single blind study. J Neurol 255: 858–866, 2008 [DOI] [PubMed] [Google Scholar]
- 12. Jeun SS, Kim JS, Kim BS, Park SD, Lim EC, Choi GS, Choe BY. Acupuncture stimulation for motor cortex activities: a 3T fMRI study. Am J Chin Med 33: 573–578, 2005 [DOI] [PubMed] [Google Scholar]
- 13. Jin R, Yang G, Li G. Molecular insights and therapeutic targets for blood-brain barrier disruption in ischemic stroke: critical role of matrix metalloproteinases and tissue-type plasminogen activator. Neurobiol Dis 38: 376–385, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu M. Acupuncture for stroke in China: needing more high-quality evidence. Int J Stroke 1: 34–35, 2006 [DOI] [PubMed] [Google Scholar]
- 15. Longa EZ, Weinstein PR, Carlson S. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20: 84–95, 1989 [DOI] [PubMed] [Google Scholar]
- 16. Magnusson M, Johansson K, Johansson BB. Sensory stimulation promotes normalization of postural control after stroke. Stroke 25: 1176–1180, 1994 [DOI] [PubMed] [Google Scholar]
- 17. Mayer DJ. Acupuncture: an evidence-based review of the clinical literature. Annu Rev Med 51: 49–63, 2000 [DOI] [PubMed] [Google Scholar]
- 18. Nishimura Y, Ito T, Saavedra JM. Angiotensin II AT1 blockade normalizes cerebrovascular autoregulation, and reduces cerebral ischemia in spontaneously hypertensive rats. Stroke 33: 2478–2485, 2000 [DOI] [PubMed] [Google Scholar]
- 19. Shiflett SC. Does acupuncture work for stroke rehabilitation: what do recent clinical trials really show? Top Stroke Rehabil 14: 40–58, 2007 [DOI] [PubMed] [Google Scholar]
- 20. Si QM, Wu GC, Cao XD. Effects of electroacupuncture on acute cerebral infarction. Acupunct Electrother Res 23: 117–124, 1998 [DOI] [PubMed] [Google Scholar]
- 21. Sung JH, Chao DM, Xia Y. Neuronal responses to hypoxia. In: New Frontiers in Neurological Research, edited by Wang Q, Ying WH. Kerala: Research Signpost, 2008 [Google Scholar]
- 22. Swanson RA, Morton MT, Tsao-Wu G. Semiautomated method for measuring brain infarct volume. J Cereb Blood Flow Metab 10: 290–295, 1990 [DOI] [PubMed] [Google Scholar]
- 23. Wang X, Lo EH. Triggers and mediators of hemorrhagic transformation in cerebral ischemia. Mol Neurobiol 28: 229–244, 2003 [DOI] [PubMed] [Google Scholar]
- 24. Yang YL, Xia XW, Zhang Y, Wang Q, Li L, Luo GH, Xia Y. δ-Opioid receptor activation attenuates oxidative injury in the ischemic rat brain. BMC Biol 7: 55, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhang YG, Liu TP, Qian ZY. Influence of total saponins of panax ginseng on infarct size and polyamine contents in rat brain after middle cerebral artery occlusion. Chinese J Pharmacol Toxicol 8: 250, 1994 [Google Scholar]
- 26. Zhou F, Guo JC, Cheng JS, Wu GC, Xia Y. Electro-acupuncture induced protection from cerebral ischemia is dependent on stimulation intensity, and frequency. The Proceedings of 3rd Cell Stress Society International Congress on Stress Responses in Biology and Medicine and 2nd World Conference of Stress Budapest, Hungary 3: 250, 2007 [Google Scholar]
- 27. Zhu H, Fan X, Yu Z, Liu J, Murata Y, Lu J, Zhao S, Hajjar KA, Lo EH, Wang X. Annexin A2 combined with low-dose tPA improves thrombolytic therapy in a rat model of focal embolic stroke. J Cereb Blood Flow Metab 30: 1137–1146, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhu JM, Kennedy DN, Cao XD. Neural transmission of acupuncture signal. In: Acupuncture Therapy for Neurological Diseases: A Neurobiological View, edited by Xia Y, et al. Beijing: Springer-TUP, 2010, p. 23–37 [Google Scholar]