Abstract
In the United States, filoviruses (ebolaviruses and marburgviruses) are listed as National Institute of Allergy and Infectious Diseases (NIAID) Category A Priority Pathogens, Select Agents, and Centers for Disease Control and Prevention (CDC) Category A Bioterrorism Agents. In recent months, U.S. biodefense professionals and policy experts have initiated discussions on how to optimize filovirus research in regard to medical countermeasure (ie, diagnostics, antiviral, and vaccine) development. Standardized procedures and reagents could accelerate the independent verification of research results across government agencies and establish baselines for the development of animal models acceptable to regulatory entities, such as the Food and Drug Administration (FDA), while being fiscally responsible. At the root of standardization lies the question of which filovirus strains, variants, or isolates ought to be the prototypes for product development, evaluation, and validation. Here we discuss a rationale for their selection. We conclude that, based on currently available data, filovirus biodefense research ought to focus on the classical taxonomic filovirus prototypes: Marburg virus Musoke in the case of marburgviruses and Ebola virus Mayinga in the case of Zaire ebolaviruses. Arguments have been made in various committees in favor of other variants, such as Marburg virus Angola, Ci67 or Popp, or Ebola virus Kikwit, but these rationales seem to be largely based on anecdotal or unpublished and unverified data, or they may reflect a lack of awareness of important facts about the variants' isolation history and genomic properties.
Standardized procedures and reagents could accelerate the independent verification of research results across government agencies and establish baselines for the development of animal models acceptable to regulatory entities. At the root of standardization lies the question of which filovirus strains, variants, or isolates ought to be the prototypes for product development, evaluation, and validation. The authors discuss a rationale for selection and conclude that filovirus biodefense research ought to focus on the classical taxonomic filovirus prototypes.
The family Filoviridae contains 2 genera. The genus Marburgvirus consists of a single species, Marburg marburgvirus, with 2 member viruses, Marburg virus (MARV) and Ravn virus (RAVV). The genus Ebolavirus contains 5 species: Bundibugyo ebolavirus, Zaire ebolavirus, Reston ebolavirus, Sudan ebolavirus, and Taï Forest ebolavirus, whose members are Bundibugyo virus (BDBV), Ebola virus (EBOV), Reston virus (RESTV), Sudan virus (SUDV), and Taï Forest virus (TAFV), respectively. A third, tentative genus (“Cuevavirus”) has been suggested for a novel filovirus, Lloviu virus (LLOV; species “Lloviu cuevavirus”), which has not yet been isolated in culture (Table 1).1 With the exception of RESTV and possibly LLOV, all of these viruses cause severe and often fatal viral hemorrhagic fever (VHF) upon infection in humans (reviewed in ref 2).
Table 1.
Summary of filovirus taxonomy as recently established by the International Committee on Taxonomy of Viruses (ICTV) Filoviridae Study Group
| New Taxonomy1 | Outdated Taxonomy (Eighth ICTV Report) |
|---|---|
| Order Mononegavirales Family Filoviridae Genus Marburgvirus Species Marburg marburgvirus Virus 1: Marburg virus (MARV) Virus 2: Ravn virus (RAVV) Genus Ebolavirus Species Taï Forest ebolavirus Virus: Taï Forest virus (TAFV) Species Reston ebolavirus Virus: Reston virus (RESTV) Species Sudan ebolavirus Virus: Sudan virus (SUDV) Species Zaire ebolavirus Virus: Ebola virus (EBOV) Species Bundibugyo ebolavirus Virus: Bundibugyo virus (BDBV) Genus “Cuevavirus” (suggested)* Species “Lloviu cuevavirus” (suggested) Virus: Lloviu virus (LLOV) |
Order Mononegavirales Family Filoviridae Genus Marburgvirus Species Lake Victoria marburgvirus Virus: Lake Victoria marburgvirus (MARV) Genus Ebolavirus Species Cote d'Ivoire ebolavirus [sic] Virus: Cote d'Ivoire ebolavirus [sic] (CIEBOV) Species Reston ebolavirus Virus: Reston ebolavirus (REBOV) Species Sudan ebolavirus Virus: Sudan ebolavirus (SEBOV) Species Zaire ebolavirus Virus: Zaire ebolavirus (ZEBOV) |
Taxa not yet approved by the ICTV Executive Committee are placed in quotation marks.
In the U.S., filoviruses are classified as Select Agents,3 NIAID Category A Priority Agents,4 and CDC Category A Bioterrorism Agents5 due to the absence of FDA-approved prophylaxis or treatment regimens, their high lethality (up to 90% in larger outbreaks), their high infectivity (LD50=1 virion in rodent models), and their stability in artificial aerosols.2,6,7 Research on infectious (“live”) filoviruses, which are classified as Risk Group 4 agents, requires Biosafety Level 4 (BSL-4) laboratories.8–10 Consequently, any research with infectious filoviruses is currently confined to only 6 facilities in the U.S. and a very limited number of people, who have to be properly cleared and trained to obtain access rights.
The various U.S. filovirus research programs are currently not optimally coordinated for the concerted development of medical countermeasures. There is merit to the suggestion that the U.S. filovirus research programs should at least be based on common standards, including identical filovirus variant prototypes, animal models, and virus quantification and characterization assays.
Unfortunately, such common standards have yet to be established. Experiments are currently performed with disparate filovirus strains, variants, or isolates with varying and often unknown passaging and acquisition history in animals of different origin, age, gender, or immunological background. Independent verification of results is often difficult because the particular virus, animal model, and/or assay used in one facility are not available or established in another. Nevertheless, individual research groups using very different research conditions sometimes present results side-by-side in program evaluations, thereby possibly creating the illusion that all presented results can be compared.
The first step in standardizing filovirus medical countermeasure development is to ensure that experiments are based on the same prototype filoviruses. To do so, consensus must be reached regarding which filoviruses should be considered prototypes.
General Considerations
In this article, we address only biodefense research and not public health research, as in our opinion filovirus variant standardization only makes sense for countermeasure development. Biodefense research seeks to mitigate the impact of an attack with a bioweapon. An attack with filoviruses could have dramatic consequences, including widespread panic and/or loss of many human lives.11 The usual assumption is that the result of an attack (ie, the number of infected people and with it the burden on national healthcare institutions or the work force) would develop explosively and possibly at multiple sites rather than gradually, as in a natural outbreak. Standard, usually effective public health responses to filovirus disease outbreaks, such as quarantine and barrier nursing, would be overwhelmed by the rapid onset and the sheer numbers of cases.11 This scenario demands swift intervention with medical countermeasures (MCMs), such as antivirals to terminate the multiple filovirus transmission chains caused by simultaneous infection of many people in the initial attack. Vaccines might be needed to protect nonexposed populations outside the immediate impact zone. However, medical countermeasure development can take decades and cost hundreds of millions of dollars. It is therefore crucial to streamline this process to create a baseline for drug evaluation and validation. Streamlining should include standard (prototype) filovirus variants to ensure rapid research progress. At some point it will be necessary to test MCM efficacy against other variants to confirm more generic applicability.
Standardization of reagents, methods, or models may be controversial, since some research organizations may have heavily invested in alternative variants and specialized reagents. It is important to note that any change of variables (such as the identity of a virus variant) in any given experiment might dramatically alter the performance of the test materials including drugs, vaccines, and diagnostic assays. It is also important to remember that individual researchers may favor particular standardization decisions because they are suited to their personal research interests.
We therefore want to raise awareness among program administrators and other decision makers currently engaged in standardization discussions that important programmatic decisions with far-reaching organizational and financial consequences, such as the selection of standardized filovirus variants, must be approached systematically. Ideally, such decisions should be based solely on scientific facts that have been published in properly peer-reviewed journals and corroborated by independent research groups. If such published data are not available for a particular filovirus variant, then this variant should not be considered for experimental standardization.
Specific Considerations
Filovirus Variants, Not Isolates
Filovirus variants, not filovirus isolates, should be considered in the discussion on filovirus standardization. A complete list of filovirus publications and summaries thereof through 2008 is available.2 These summaries are often short and do not in all cases point out which filovirus variants have been used in the past for particular experiments and what the justification was for their use. Such information would, however, be pertinent for filovirus variant prototype selection. Decision makers and next-generation filovirologists are often not aware of certain filoviruses, such as MARV Hartz, MARV Lüdicke, EBOV E718, or EBOV ME, although they were used frequently during the first 15 years of filovirus research.
Unfortunately, comprehensive lists of all filoviruses do not yet exist, and the terms strain, variant, and isolate have not yet been defined explicitly for filoviruses. Currently, the 3 terms are used interchangeably by many, with far-reaching, ill-advised conclusions—for example, that MARV Angola is a different “strain” than the commonly used MARV Musoke and therefore ought to be singled out, when in fact these viruses are very closely related to each other. In fact, as we also discuss below, there are no published data available that demonstrate a statistically significant difference in the phenotype of infections with either virus.
Members of the International Committee on Taxonomy of Viruses (ICTV) Filoviridae Study Group are currently working on establishing filovirus variant lists and establishing proper definitions for the terms filovirus strain, filovirus variant, and filovirus isolate. The publication of these lists and definitions should precede any final discussions on prototype choice. In the meantime, discussions can be guided by the fact that virus taxonomy is constructed similarly to other taxonomic schemes, with terminology being roughly equivalent (see Table 2).
Table 2.
Analogy of zoological and virological taxonomy schemes to exemplify the difference between taxon, member, and individual
| Zoological Taxonomy | Virological Taxonomy |
|---|---|
| Order Carnivora (all carnivores) Family Canidae (all dogs) Genus Vulpes (all true foxes) Species Vulpes vulpes (all red foxes) Pack: 1 (set of related red foxes) Individuals: red fox 1 (“Tod”), 2 (“Sheila”) … |
Order Mononegavirales (all mononegaviruses) Family Filoviridae (all filoviruses) Genus Ebolavirus (all ebolaviruses) Species Sudan ebolavirus (all Sudan viruses) Variant: 1 (“Yambio”) (set of related Sudan viruses) Individuals: Sudan virus 1 (“0401”), 2 (“0402”) … |
Importantly, all taxonomic schemes are constructed around taxa and other classes that represent groups of organisms, rather than single organisms, until the lowest possible level (individual in zoology, isolate in virology). It makes little sense to develop products against filovirus isolates, such as MARV Ci67 or SUDV Yambio-0401. It is also important to remember that even a skilled filovirologist is currently unable to observe an infection in nonhuman primates and state with certainty that the animals are infected with MARV Musoke or MARV Angola variants. The product should therefore target the virus. Nevertheless, a prototype filovirus variant, such as Musoke or Angola, needs to be chosen for the development and evaluation of MCMs, as it is impossible to work with all variants at the same time. The following section will therefore address why particular variants should be chosen over other ones.
Experimental Continuity
Experimental continuity is the most important aspect in filovirus standardization. In most taxonomic frameworks, individual taxa are assigned “type” taxa and members. This means that a taxon will have a member that is generally accepted as a reference specimen to which other, newly discovered entities can be compared. The type member is often the first specimen that was discovered and described. Although official virus taxonomy currently endorses neither type taxa nor type members (with the one exception of type species), types are de facto accepted in the field.
Ebolavirus Isolates Used in Research
The majority of ebolavirus experiments reported were performed with the EBOV Mayinga isolate, a representative of the unnamed EBOV variant that caused the first reported EBOV disease outbreak in 197612 (also represented by isolates Ecran, ME, and E718, among others). This encompasses basically all EBOV experiments reported from countries other than the U.S. and the majority of EBOV experiments within the U.S.2 A small percentage of experiments were performed with isolates of the EBOV Kikwit (“Zaire 1995”) variant (almost exclusively at 1 institute) or with isolates of other ebolaviruses (predominantly RESTV Pennsylvania, SUDV Boniface, and SUDV Gulu).2
Marburgvirus Isolates Used in Research
In the case of marburgviruses, the majority of experiments until the mid-1980s were performed with the unnamed MARV variant that caused the 1967 disease outbreaks in West Germany and Yugoslavia (represented by isolates Cieplik [“Ci67”], Flak, Hartz, Hilberger, HO, Kliebe, Lüdicke, Ratayczak, Popp, and Voege).2,13,14 Western researchers later switched to the Musoke variant, whereas Soviet/Russian scientists continued to work exclusively with Popp- and Voege-derived viruses.2 The Western switch to “Musoke” most likely occurred because its history and origin were known, whereas the history of the 1967 variant often involved passaging to various extents in rodents without adequately keeping track of which partner institution received which particular isolate. Recently, a few U.S. groups reported the use of a MARV Cieplik-derived isolate (see, eg, refs 15–19).
The almost exclusive use of MARV isolate Musoke or EBOV isolate Mayinga means that almost all molecular and virological characterizations—and the majority of vaccine and antiviral candidates, diagnostic assays, and specific reagents available today—are based on 2 filovirus variants.2 Replacing them with different variants would mean that all established methods de facto need to be reevaluated and possibly even reestablished—after all, the argument for switching to a different variant is based on the idea that it behaves differently from the standard variant. Such a switch must therefore be well justified, as it may result in a huge burden on laboratories.
Access to Filovirus Isolates
General access to particular virus variants is also an important aspect of filovirus standardization. Since an official filovirus depository does not exist, laboratories depend on virus sharing. In practice, sharing is often hindered by export and import regulations between countries; biosafety and biosecurity considerations regarding transport and handling even within a country; liability; administrative red tape, especially across agencies; and, unfortunately, the self-serving interests of individual researchers. Prototype standardization for product development should therefore involve variants that are widely distributed, rather than focusing on variants that exist only in individual facilities, and, of course, the viruses that were used for most experiments are also those that are most widely distributed. All arguments brought forward in favor of standard filoviruses different from the most used and distributed variants therefore must always be considered in light of the possible negative impact on research efficiency and progress caused by necessary verification and/or reestablishment of assays and reagents.
Using Filovirus Isolates to Develop Antivirals
In filovirology, the evaluation of potential antivirals usually occurs in 4 stages. A potential antiviral is first tested for its inhibitory properties in vitro (ie, in tissue culture). If results are promising, the experiments are extended to laboratory mice, using a laboratory mouse–adapted filovirus, since natural filoviruses do not cause disease in adult rodents. Experiments are often extended to guinea pigs using a guinea pig–adapted virus if the compound protects mice from death and other parameters are favorable. Finally, if efficacy is demonstrated in rodent models, nonhuman primates are infected with a natural (wild-type) virus and treated with the drug. The rationale for this includes:
statistics—a higher number of animals means higher statistical power, and it is more feasible to keep more small animals than large animals given space constraints;
cost—it is less expensive to maintain smaller animals;
ethical concerns—there should be evidence for the principal possibility of drug efficacy before involving nonhuman primates; and
genetics—nonhuman primates are evolutionarily closer to humans and therefore considered most predictive of drug efficacy in humans.20
To limit confounding variables in these successive experiments, it is crucial that the filovirus variants used are as close to identical to each other as possible. It makes little scientific sense to perform, for instance, mouse and rodent experiments with rodent-adapted EBOV Mayinga and then switch to wild-type EBOV Kikwit (“Zaire 1995”) when moving into primates, unless “Kikwit” offered some definite advantages over “Mayinga.” EBOV Mayinga and MARV Musoke are the only natural filovirus variants that cause 100% lethality in well-established nonhuman primate models and that also have been adapted to cause close to 100% lethality both in mice and guinea pigs.6,16,21–24 A switch to different variants therefore would require the establishment of novel rodent models.
Filovirus Sequence Variability
The development of diagnostic assays based on polymerase chain reaction (PCR), as well as the very promising development of antisense therapeutics,25,26 requires the knowledge of the genomic sequence of a target particular virus/virus variant/isolate. Sequence comparisons would also be the stepping stone to identifying the reason for different phenotypes of individual variants, if such is ever detected. It could be problematic to establish a variant prototype that has not yet been sequenced, such as SUDV Boniface, the current taxonomic SUDV type variant.
Of course, virus genomic sequences can now be obtained relatively easily given that (1) one discounts the very 3′ and 5′ termini of filovirus genomes (which thus far have rarely been determined, with the notable exceptions of MARV Musoke and Popp, BDBV Bundibugyo, EBOV Mayinga, and SUDV Gulu and Yambio), and (2) one has access to an assured wild-type virus population that is as homogeneous as possible (which, for instance, has not been the case for TAFV). Since the 3′ and 5′ termini contain important regulatory signals for filovirus genome replication, transcription, and packaging, it is important to know their sequences. Switching of virus prototypes might therefore result in the need for sequencing projects. But once a sequence is available, it is important to ascertain that it is actually correct. For instance, the near-complete genomic sequence of EBOV Kikwit (“Zaire 1995”) differs from all other known wild-type EBOV genomic sequences in that it contains an additional U residue in the GP gene editing site. Either this is a mistake (possible, as this site causes stuttering of polymerases and therefore may cause sequencing artifacts27,28) or it is a true mutation (also possible, as such mutations have been observed in some rodent-adapted viruses29 and seem to be typical for EBOV tissue culture adaptation30). This mutation has a potentially far-reaching consequence, which is to reverse the normal 1:4 ratio of expressed spike glycoprotein (GP1,2) to secreted glycoprotein (sGP).27,28 The function of sGP is currently unknown, which makes it difficult to evaluate the effect of decreased expression on pathogenesis, and side-by-side comparisons of EBOV variants containing and not containing the mutation have not yet been reported. In any case, the additional U residue certainly suggests that, at least for now, EBOV Kikwit should be regarded with caution in standardization discussions.
Lastly, the evaluation of novel candidate drugs in vitro benefits tremendously from the existence of reverse genetics systems (which allow the creation of filoviruses from DNA plasmids) and low-containment surrogate systems, such as so-called minigenome and other replicon systems or transcription- and replication-competent virion-like particles (trcVLPs). Replicon systems and trcVLPs have the additional advantage that they can also be used for screening for the identification of inhibitors outside of maximum containment laboratories, thereby increasing throughput. Reverse genetics systems and surrogate systems currently exist only for EBOV Mayinga and MARV Musoke.31–35 A switch to different prototypes would therefore require the reestablishment of these tools.
Filovirus Prototypes from Human Clinical Cases
Laboratory filovirus variants are those that have evolved in experimental settings that most often do not reflect nature. For instance, serial passaging of wild-type filovirus variants in otherwise resistant rodents sometimes leads to the evolution of laboratory variants that cause fatal disease in these animals.36 However, it is unclear which laboratory variants could cause disease in humans, and it is possible that a product developed against such a variant does not work against a natural variant. One laboratory infection of a researcher with a guinea pig–adapted EBOV Mayinga occurred in 2004 and unfortunately resulted in death, thereby demonstrating that at least this particular guinea pig–adapted EBOV variant is pathogenic and highly virulent in humans.37 Another human laboratory infection with a different guinea pig–adapted EBOV Mayinga had occurred in 1976, but in this case the researcher survived.38 There have been no other reported laboratory infections with laboratory variants of any filovirus. This low case number complicates risk extrapolation, especially since there are many different guinea pig–adapted EBOVs that most likely all differ from each other on a genomic level29,39–41 and therefore may behave differently.
Synthetic and tailored filovirus variants are special cases of laboratory variants. In contrast, they are created by directly mutating the genomes of natural or laboratory variants. Tailored viruses created to date have either not been evaluated in nonhuman primates or proven to be attenuated.42 Aggressors could develop bioweapons based on laboratory or tailored variants, but it is unlikely since there is no a priori guarantee that these variants will actually cause fatal disease in humans. From a pragmatic point of view, this means that all filovirus variants of unclear origin should be regarded with utmost caution in the standardization discussion, as they may be “irrelevant threats.” This includes, in particular, the MARV variant that emerged in West Germany and Yugoslavia in 1967 (including isolates Cieplik, Flak, Hartz, Hilberger, HO, Kliebe, Lüdicke, Ratayczak, Popp, and Voege).36 Based on the published literature, it is close to impossible to judge whether the still-circulating cultures of these viruses were obtained through guinea pig culture or not. SUDV Boniface may be a similar case, as the literature on the isolation history of this virus is similarly convoluted.
Standardization discussions should therefore focus on natural filovirus variants—that is, those that were isolated during disease outbreaks or from reservoir hosts in nature. R&D should not be based on a natural variant stemming from a filovirus reservoir host, because it would be unclear whether the variant actually could cause disease in humans. Consequently, research should be based on a natural variant isolated from sick or deceased humans, because its pathogenicity is self-evident.
Whether a filovirus prototype is derived from a sick or a lethal human case is irrelevant, as are filovirus disease case numbers and case-fatality rates of individual outbreaks. In 1980, a Frenchman became infected with a MARV variant in Nzoia, Kenya. The patient collapsed after admission to a hospital, and a physician infected himself while attempting to resuscitate the patient. The patient died 6 hours after admission, but the physician survived.43 Virus was isolated from the physician and became the standard experimental MARV mentioned above, Musoke. It is now argued by some that “Musoke” should not be an R&D prototype because it stems from a survivor.
This thinking is flawed. An isolate is only an instance of virus. There are currently no data suggesting that a second isolate, had it been obtained from the patient, would be genomically different from the physician isolate in any significant way. Indeed, all phylogenetic data currently available emphasize that filoviruses do not mutate considerably within a human epidemic transmission chain.44 For instance, the genomic difference between 11 MARV Angola isolates obtained from different patients is 0-0.07%. Ten of them had 5 nucleotide changes (in a total genomic length of 19,114 nucleotides) or fewer compared to the reference isolate.44 This implies that in 1980 both the patient and the physician were infected with the same entity and not that the patient was infected with a more virulent one that unfortunately was not isolated.
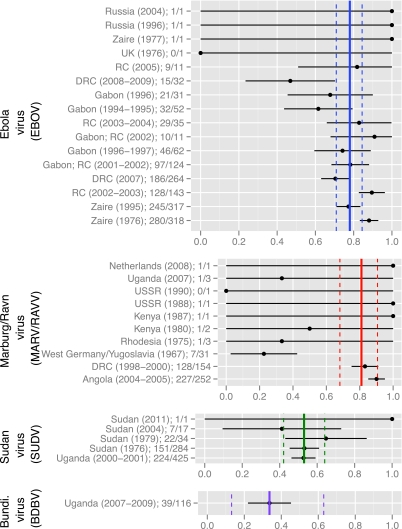
The severity of infectious disease is always a function of both virus virulence and host response. Indeed, every large filovirus disease outbreak had a lethality of less than 100%—that is, there always were survivors (Figure 1). This of course is also true for the large MARV disease outbreak in Angola. No one currently argues that the few survivors of this outbreak were infected with a less lethal virus. In fact, as recent studies demonstrate, survivors of filovirus infections seem to differ in their genetic disposition from those that succumb to infection, which results in different immune responses to infection.45,46
Figure 1.
Plotting of the case-fatality rates (black dots on a scale from 0.0 [0%] to 1.0 [100%]) for each human filovirus disease outbreak broken down by virus [EBOV, MARV/RAVV, SUDV, BDBV], location [country]/year, and overall case numbers/deaths, along with 99% confidence intervals (black horizontal lines). The vertical lines represent the overall case-fatality rate for a particular virus (bold lines), with corresponding 99% confidence intervals (dashed lines). The case-fatality rate of EBOV disease outbreaks is 78% (99.5% CI: 71%, 84%), for MARV/RAVV 82% (99% CI: 68%, 91%), for SUDV 53% (99% CI: 42%, 64%), and for BDBV 34% (99% CI: 13%, 63%). Statistically significant differences in overall case-fatality rates are found in the case of EBOV vs. SUDV (p=<0.0001), MARV vs. SUDV (p=<0.0001), EBOV vs. BDBV (p=<0.0001), and MARV vs. BDBV (p=<0.0001), but not in the case of EBOV vs. MARV, or SUDV vs. BDBV. TAFV is not included in the figure because only one nonlethal human case has been described. DRC, Democratic Republic of Congo; RC, Republic of Congo. Color graphics available online at www.liebertonline.com/bsp
Aside from host immune responses (which also could be influenced by underlying diseases, such as AIDS or malaria), medical care probably has an influence on disease outcome. For instance, the patient in the case described above got infected at an unknown point in time and location in nature and reached a hospital when he was already moribund, whereas the physician infected himself in a hospital and was immediately cared for when symptoms appeared.43 Factors such as immune responses, rapidity and type of medical care, hygiene and quarantine enforcement, and education in all likelihood influence filovirus disease outbreak statistics to a greater extent than the few genomic changes found in different filovirus variants.
According to available data, there is no evidence that a higher human case number is correlated to a more transmissible virus, or that a higher case-fatality rate is correlated to a more virulent virus. Instead, explanations for these numbers can be found in patient behavior and location of the outbreak. For instance, filoviruses cause bona fide nosocomial diseases; in the past they spread rapidly within hospitals because medical personnel had to reuse syringes and needles and thereby distributed the virus among all patients who received injections (see, eg, refs 47–49). Indeed, most filovirus disease outbreaks with large case numbers are associated with spread in hospitals. Urban filovirus outbreaks, of which there have been few so far, also were characterized by large case numbers, most likely because filoviruses spread via direct person-to-person contact and population density is higher in urban areas than in rural areas.
On the other hand, filovirus disease outbreaks with small case numbers most often occurred in rural and secluded areas in which the index patient(s) did not have much contact with others or initially did not seek care in hospitals. A virus variant from a limited outbreak with moderate lethality does therefore not automatically have a “disadvantage” over a variant from a large outbreak with high lethality. Indeed, mathematical analysis demonstrates that there are no statistically significant differences in regard to lethality among individual MARV/RAVN disease outbreaks (with the exception of the first recorded outbreak in 1967), individual EBOV disease outbreaks, or even when MARV/RAVN and EBOV disease outbreaks are compared to each other (Figure 1).
Better Controlled Comparative Pathology Experiments
Better controlled comparative pathology experiments need to be performed to determine whether a new filovirus variant is more or less virulent than others. A common speculation in the filovirology community is that MARV Angola is more virulent than MARV Musoke and therefore should be a research focus. However, there is currently little evidence to support this notion.
There are currently only 3 publications relevant to this discussion.50–52 The first describes the evaluation of a vaccine candidate in 7 crab-eating macaques, which were challenged after intramuscular vaccination with either MARV Musoke, MARV Angola, or RAVV Ravn. Two additional animals served as controls. They were infected with MARV Angola or RAVV Ravn after administration of a mock vaccine, and both died on the same day.51 As is clear from this experimental setup, only MARV Angola and RAVV Ravn could be compared, but the animal number is too low for statistical significance (n=1 for both viruses). Differences in virulence were not observed, and pathology was not reported. That MARV Angola “produces a disease … that is more rapid and severe than that produced by other MARV” variants is referenced as an unpublished observation without supporting data.51(p9660)
The second article reports the evaluation of a potential filovirus inhibitor. Twelve rhesus monkeys were infected intramuscularly with MARV Angola; 6 were then treated and 6 served as controls.50 The controls died after a mean of 7.3 days. The authors assessed that these animals “appeared to progress more rapidly … than has previously been reported for other strains of MARV” because no direct comparison to other MARV variants was performed.50(S372) That historical experiments with MARV Musoke usually resulted in death on days 9 to 12 is interesting, but many factors could have influenced this particular experiment.
The third article is the only one thus far reporting the pathology of MARV Angola infection in any animal (crab-eating macaques). However, the animals were challenged by a different route (aerosol) with different doses. They died around day 9. A direct comparison among MARV variants using aerosol was not undertaken.52 All 3 studies were performed at the same institute and await independent verification.
A direct comparison between different filovirus variants will be experimentally challenging. To compare the virulence of 2 different variants, it will be pertinent to exactly quantify and standardize the virion preparations—that is, it has to be proven without a doubt that 2 nonhuman primate populations receive the exact same amount of infectious virions and potentially confounding materials. Using the same amount of plaque-forming units, as is often done, does not suffice. Cultures of different virus variants plaque differently (and often they are plaqued at different times using slightly varying plaque assay protocols). Cultures most likely contain varying numbers of genome copy numbers and plaque-forming and non-plaque-forming virions, including confounding defective-interfering particles (pseudo virions that are defective in their genome but get propagated with the help of functional viruses).53–57 The composition of a virus culture (and therefore a plaque-forming unit) is dependent on the passaging history of the virus. Since MARV Musoke has been around since 1980, it is likely that stock virus cultures have accumulated a fair share of such particles.
In contrast, the Angola variant is fairly new (2005), and its stock preparations are probably more pure (and also better controlled). This means that virion counts should therefore be undertaken, and the virus preparation should be examined for defective-interfering particles by yield reduction assays and other methods, as these particles could influence the immune response in aggravating ways or by acting as prophylaxes or vaccines.58–60 It would be absolutely critical to prepare both virus variant stocks in the exact same way, using the same culture conditions and harvesting protocol, and especially to ensure that both undergo the same freeze-thaw cycles until use, since thawing inactivates them in a nonlinear manner. This extends to quantifying the virus dose that animals actually received (ie, requantifying virus on the day of animal infection), rather than reporting the administered “target dose.” Since almost none of this has been reported thus far, the currently available data do not justify the assertion that any MARV variant is more virulent than another.
Conclusions
In ongoing discussions on filovirus variant prototype choice among program administrators, it is important to evaluate each available virus and to pinpoint the particular virus that satisfies most requirements for a prototype. In our opinion, there is no doubt that the current taxonomic type filoviruses also ought to be the prototypes for biodefense R&D (Table 3), with the possible exception of SUDV. In the case of MARV, Musoke is clearly the most widely available, most widely used, and best characterized variant, and convincing data demonstrating its inferiority compared to any MARV variant have not been reported, let alone been verified. Mayinga fulfills the same criteria in the case of EBOV.
Table 3.
Current taxonomical filovirus (proto)types1 and suggested prototypes for product R&D
| Virus | Taxonomic (proto)type | Suggested R&D Prototype |
|---|---|---|
| MARV | Musoke | Musoke |
| RAVV | Ravn | Ravn |
| BDBV | Bundibugyo | Bundibugyo |
| EBOV | Mayinga | Mayinga |
| SUDV | Boniface | Gulu or Yambio |
| TAFV | Côte d'Ivoire | Côte d'Ivoire |
The case of SUDV remains to be debated. On the one hand, most published experiments have been performed with variant Boniface. However, the overall number of such publications is small, the origin of Boniface is unclear, and genomic sequence is missing. Variant Gulu may be an alternative, but there is anecdotal data that it may be less virulent than Boniface in nonhuman primates. However, these experiments have not yet been published, and it is doubtful that they have been controlled for quantity of input virus in a manner rigorous enough to come to definite conclusions. Also, there is the possibility that the Boniface virus used was a guinea pig–adapted variant, which, at least in theory, could be more virulent in primates than wild-type virus. An alternative would be the recently reported Yambio variant, but animal experiments with this variant have yet to be described.
Little to no research has been performed with the remaining human filoviruses (BDBV, RAVV, TAFV), which means that prototype choice can be random at this point in time and solely be based on availability.
We do not claim to understand all the intricacies of political decision making in programmatic science discussions. Likewise, we are sure that program administrators do not claim to understand all the intricacies of basic virology. We hope that this article somewhat bridges the gap between 2 communities whose ideas of “common sense” are often widely disparate.
References
- 1.Kuhn JH. Becker S. Ebihara H, et al. Proposal for a revised taxonomy of the family Filoviridae: classification, names of taxa and viruses, and virus abbreviations. Arch Virol. 2010;155(12):2083–2103. doi: 10.1007/s00705-010-0814-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuhn JH. Filoviruses—A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. New York and Vienna: SpringerWien; 2008. [PubMed] [Google Scholar]
- 3.U.S. Centers for Disease Control and Prevention. Select Agent Program. 2011. http://www.cdc.gov/od/sap/ [Sep 27;2011 ]. http://www.cdc.gov/od/sap/
- 4.National Institutes of Health, National Institute of Allergy and Infectious Diseases. NIAID Category A, B and C Priority Pathogens. 2011. http://www.niaid.nih.gov/topics/biodefenserelated/biodefense/research/pages/cata.aspx. [Sep 27;2011 ]. http://www.niaid.nih.gov/topics/biodefenserelated/biodefense/research/pages/cata.aspx
- 5.U.S. Centers for Disease Control and Prevention. Emergency Preparedness and Response—Bioterrorism Agents/Diseases. http://www.bt.cdc.gov/agent/agentlist-category.asp. [Sep 27;2011 ]. http://www.bt.cdc.gov/agent/agentlist-category.asp
- 6.Bray M. Davis K. Geisbert T. Schmaljohn C. Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis. 1999;179(suppl 1):S248–S258. doi: 10.1086/514292. [DOI] [PubMed] [Google Scholar]
- 7.Leffel EK. Reed DS. Marburg and Ebola viruses as aerosol threats. Biosecur Bioterror. 2004;2(3):186–191. doi: 10.1089/bsp.2004.2.186. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services, Public Health Service, U.S. Centers for Disease Control and Prevention, National Institutes of Health (NIH) DHHS Publication No. (CDC) 93-8395. 5th. Washington, DC: DHHS; 2009. [Sep 27;2011 ]. Biosafety in Microbiological and Biomedical Laboratories (BMBL) [Google Scholar]
- 9.World Health Organization. Laboratory Biosafety Manual. 3rd. Geneva, Switzerland: WHO; 2004. [Sep 27;2011 ]. [Google Scholar]
- 10.American Biological Safety Association. Risk Group Classification for Infectious Agents. http://www.absa.org/riskgroups/index.html. [Sep 27;2011 ]. http://www.absa.org/riskgroups/index.html
- 11.Borio L. Ingelsby T. Peters CJ, et al. Hemorrhagic fever viruses as biological weapons—medical and public health management. JAMA. 2002;287(18):2391–2405. doi: 10.1001/jama.287.18.2391. [DOI] [PubMed] [Google Scholar]
- 12.Johnson KM. Webb PA. Lange JV. Murphy FA. Isolation and partial characterisation of a new virus causing acute haemorrhagic fever in Zaire. Lancet. 1977;8011:569–571. doi: 10.1016/s0140-6736(77)92000-1. [DOI] [PubMed] [Google Scholar]
- 13.Siegert R. Marburgvirus-Krankheit. In: Röhrer H, editor. Handbuch der Virusinfektionen bei Tieren. Jena, Thuringia, German Democratic Republic: VEB Gustav Fischer Verlag; 1978. pp. 579–654. [German] [Google Scholar]
- 14.Ellis DS. Stamford S. Lloyd G, et al. Ebola and Marburg viruses: I. some ultrastructural differences between strains when grown in Vero cells. J Med Virol. 1979;4(3):201–211. doi: 10.1002/jmv.1890040306. [DOI] [PubMed] [Google Scholar]
- 15.Fritz EA. Geisbert JB. Geisbert TW. Hensley LE. Reed DS. Cellular immune response to Marburg virus infection in cynomolgus macaques. Viral Immunol. 2008;21(3):355–363. doi: 10.1089/vim.2008.0023. [DOI] [PubMed] [Google Scholar]
- 16.Warfield KL. Alves DA. Bradfute SB, et al. Development of a model for marburgvirus based on severe-combined immunodeficiency in mice. Virol J. 2007;4:108. doi: 10.1186/1743-422X-4-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radoshitzky SR. Warfield KL. Chi X, et al. Ebolavirus Δ-peptide immunoadhesins inhibit Marburgvirus and Ebolavirus cell entry. J Virol. 2011;85(17):8502–8513. doi: 10.1128/JVI.02600-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D. Hevey M. Juompan LY, et al. Complex adenovirus-vectored vaccine protects guinea pigs from three strains of Marburg virus challenges. Virology. 2006;353(2):324–332. doi: 10.1016/j.virol.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 19.Warren TK. Warfield KL. Wells J, et al. Antiviral activity of a small-molecule inhibitor of filovirus infection. Antimicrob Agents Chemother. 2010;54(5):2152–2159. doi: 10.1128/AAC.01315-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warfield KL. Jaax NK. Deal EM. Swenson DL. Larsen T. Bavari S. Viral hemorrhagic fevers. In: Swearengen JR, editor. Biodefense—Research Methodology and Animal Models. Boca Raton, FL: CRC Press; 2005. pp. 227–257. [Google Scholar]
- 21.Connolly BM. Steele KE. Davis KJ, et al. Pathogenesis of experimental ebola virus infection in guinea pigs. J Infect Dis. 1999;179(suppl 1):S203–S217. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- 22.Lofts LL. Ibrahim MS. Negley DL. Hevey MC. Schmaljohn AL. Genomic differences between guinea pig lethal and nonlethal Marburg virus variants. J Infect Dis. 2007;196(suppl 2):S305–S312. doi: 10.1086/520585. [DOI] [PubMed] [Google Scholar]
- 23.Lofts LL. Wells JB. Bavari S. Warfield KL. Key genomic changes necessary for in vivo lethal mouse marburgvirus variant selection process. J Virol. 2011;85(8):3905–3917. doi: 10.1128/JVI.02372-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warfield KL. Bradfute SB. Wells J, et al. Development and characterization of a mouse model for Marburg hemorrhagic fever. J Virol. 2009;83(13):6404–6415. doi: 10.1128/JVI.00126-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Warren TK. Warfield KL. Wells J, et al. Advanced antisense therapies for postexposure protection against lethal filovirus infections. Nat Med. 2010;16(9):991–994. doi: 10.1038/nm.2202. [DOI] [PubMed] [Google Scholar]
- 26.Geisbert TW. Lee AC. Robbins M, et al. Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: a proof-of-concept study. Lancet. 2010;375(9729):1896–1905. doi: 10.1016/S0140-6736(10)60357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volchkov VE. Becker S. Volchkova VA, et al. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerase. Virology. 1995;214(2):421–430. doi: 10.1006/viro.1995.0052. [DOI] [PubMed] [Google Scholar]
- 28.Sanchez A. Trappier SG. Mahy BWJ. Peters CJ. Nichol ST. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci U S A. 1996;93(8):3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Volchkov VE. Chepurnov AA. Volchkova VA. Ternovoj VA. Klenk HD. Molecular characterization of guinea pig-adapted variants of Ebola virus. Virology. 2000;277(1):147–155. doi: 10.1006/viro.2000.0572. [DOI] [PubMed] [Google Scholar]
- 30.Volchkova VA. Dolnik O. Martinez MJ. Reynard O. Volchkov VE. Genomic RNA editing and its impact on Ebola virus adaptation during serial passages in cell culture and infection of guinea pigs. J Infect Dis. 2011;204(suppl 3):S941–S946. doi: 10.1093/infdis/jir321. [DOI] [PubMed] [Google Scholar]
- 31.Volchkov VE. Volchkova VA. Mühlberger E, et al. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science. 2001;291(5510):1965–1969. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- 32.Neumann G. Feldmann H. Watanabe S. Lukashevich I. Kawaoka Y. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J Virol. 2002;76(1):406–410. doi: 10.1128/JVI.76.1.406-410.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Towner JS. Paragas J. Dover JE, et al. Generation of eGFP expressing recombinant Zaire ebolavirus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology. 2005;332(1):20–27. doi: 10.1016/j.virol.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 34.Enterlein S. Volchkov V. Weik M, et al. Rescue of recombinant Marburg virus from cDNA is dependent on nucleocapsid protein VP30. J Virol. 2006;80(2):1038–1043. doi: 10.1128/JVI.80.2.1038-1043.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krähling V. Dolnik O. Kolesnikova L, et al. Establishment of fruit bat cells (Rousettus aegyptiacus) as a model system for the investigation of filoviral infection. PLoS Negl Trop Dis. 2010;4(8):e802. doi: 10.1371/journal.pntd.0000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Siegert R. Shu H-L. Slenczka W. Peters D. Müller G. Zur Ätiologie einer unbekannten, von Affen ausgegangenen menschlichen Infektionskrankheit. Dtsch Med Wochenschr. 1967;92(51):2341–2343. doi: 10.1055/s-0028-1106144. [German]. [DOI] [PubMed] [Google Scholar]
- 37.Akinfeeva LA. Aksënova OI. Vasilevič IV, et al. A case of Ebola hemorrhagic fever. Infekcion Bolezni. 2005;3(1):85–88. [Russian]. [Google Scholar]
- 38.Emond RT. Evans B. Bowen ET. Lloyd G. A case of Ebola virus infection. Br Med J. 1977;2(6086):541–544. doi: 10.1136/bmj.2.6086.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Subbotina E. Dadaeva A. Kachko A. Chepurnov A. Genetic factors of Ebola virus virulence in guinea pigs. Virus Res. 2010;153(1):121–133. doi: 10.1016/j.virusres.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 40.Chepurnov AA. Zubavichene NM. Dadaeva AA. Influence of selective passages on the change in Ebola virus properties. Infect Dis Rev. 2001;3(4):183–189. [Google Scholar]
- 41.Chepurnov AA. Zubavichene NM. Dadaeva AA. Elaboration of laboratory strains of Ebola virus and study of pathophysiological reactions of animals inoculated with these strains. Acta Trop. 2003;87(3):321–329. doi: 10.1016/s0001-706x(03)00122-0. [DOI] [PubMed] [Google Scholar]
- 42.Ebihara H. Theriault S. Neumann G, et al. In vitro and in vivo characterization of recombinant Ebola viruses expressing enhanced green fluorescent protein. J Infect Dis. 2007;196(suppl 2):S313–S322. doi: 10.1086/520590. [DOI] [PubMed] [Google Scholar]
- 43.Smith DH. Johnson BK. Isaacson M, et al. Marburg-virus disease in Kenya. Lancet. 1982;319(8276):816–820. doi: 10.1016/s0140-6736(82)91871-2. [DOI] [PubMed] [Google Scholar]
- 44.Towner JS. Khristova ML. Sealy TK, et al. Marburgvirus genomics and association with a large hemorrhagic fever outbreak in Angola. J Virol. 2006;80(13):6497–6516. doi: 10.1128/JVI.00069-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wauquier N. Becquart P. Padilla C. Baize S. Leroy EM. Human fatal Zaire ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS Negl Trop Dis. 2010;4(10):e837. doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wauquier N. Padilla C. Becquart P. Leroy E. Vieillard V. Association of KIR2DS1 and KIR2DS3 with fatal outcome in Ebola virus infection. Immunogenetics. 2010;62(11–12):767–771. doi: 10.1007/s00251-010-0480-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Muyembe-Tamfum JJ. Kipasa M. Kiyungu C. Colebunders R. Ebola outbreak in Kikwit, Democratic Republic of the Congo: discovery and control measures. J Infect Dis. 1999;179(suppl 1):S259–S262. doi: 10.1086/514302. [DOI] [PubMed] [Google Scholar]
- 48.Fisher-Hoch SP. Lessons from nosocomial viral haemorrhagic fever outbreaks. Brit Med Bull. 2005;73–74(1):123–137. doi: 10.1093/bmb/ldh054. [DOI] [PubMed] [Google Scholar]
- 49.Baron RC. McCormick JB. Zubeir OA. Ebola virus disease in southern Sudan: hospital dissemination and intrafamilial spread. Bull World Health Organ. 1983;61(6):997–1003. [PMC free article] [PubMed] [Google Scholar]
- 50.Geisbert TW. Daddario-DiCaprio KM. Geisbert JB, et al. Marburg virus Angola infection of rhesus macaques: pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J Infect Dis. 2007;196(suppl 2):S372–S381. doi: 10.1086/520608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Daddario-DiCaprio KM. Geisbert TW. Geisbert JB, et al. Cross-protection against Marburg virus strains by using a live, attenuated recombinant vaccine. J Virol. 2006;80(19):9659–9666. doi: 10.1128/JVI.00959-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alves DA. Glynn AR. Steele KE, et al. Aerosol exposure to the Angola strain of Marburg virus causes lethal viral hemorrhagic fever in cynomolgus macaques. Vet Pathol. 2010;47(5):831–851. doi: 10.1177/0300985810378597. [DOI] [PubMed] [Google Scholar]
- 53.Calain P. Monroe MC. Nichol ST. Ebola virus defective interfering particles and persistent infection. Virology. 1999;262(1):114–128. doi: 10.1006/viro.1999.9915. [DOI] [PubMed] [Google Scholar]
- 54.Weidmann M. Sall AA. Manuguerra JC, et al. Quantitative analysis of particles, genomes and infectious particles in supernatants of haemorrhagic fever virus cell cultures. Virol J. 2011;8(1):81. doi: 10.1186/1743-422X-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thompson KA. Yin J. Population dynamics of an RNA virus and its defective interfering particles in passage cultures. Virol J. 2010;7:257. doi: 10.1186/1743-422X-7-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huang AS. Baltimore D. Defective viral particles and viral disease processes. Nature. 1970;226(5243):325–327. doi: 10.1038/226325a0. [DOI] [PubMed] [Google Scholar]
- 57.Roux L. Simon AE. Holland JJ. Effects of defective interfering viruses on virus replication and pathogenesis in vitro and in vivo. Adv Virus Res. 1991;40:181–211. doi: 10.1016/S0065-3527(08)60279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marriott AC. Dimmock NJ. Defective interfering viruses and their potential as antiviral agents. Rev Med Virol. 2010;20(1):51–62. doi: 10.1002/rmv.641. [DOI] [PubMed] [Google Scholar]
- 59.Sekellick MJ. Marcus PI. Interferon induction by viruses. VIII. Vesicular stomatitis virus: [+/−]DI-011 particles induce interferon in the absence of standard virions. Virology. 1982;117(1):280–285. doi: 10.1016/0042-6822(82)90530-x. [DOI] [PubMed] [Google Scholar]
- 60.Yount JS. Gitlin L. Moran TM. Lopez CB. MDA5 participates in the detection of paramyxovirus infection and is essential for the early activation of dendritic cells in response to Sendai Virus defective interfering particles. J Immunol. 2008;180(7):4910–4918. doi: 10.4049/jimmunol.180.7.4910. [DOI] [PubMed] [Google Scholar]