Abstract
The forward bending test according to Adams and rib hump quantification by scoliometer are common clinical examination techniques in idiopathic scoliosis, although precise data about the change of axial surface rotation in forward bending posture are not available. In a pilot study the influence of leg length inequalities on the back shape of five normal subjects was clarified. Then 91 patients with idiopathic scoliosis with Cobb-angles between 20° and 82° were examined by rasterstereography, a 3D back surface analysis system. The axial back surface rotation in standing posture was compared with that in forward bending posture and additionally with a scoliometer measurement in forward bending posture. The changes of back shape in forward bending posture were correlated with the Cobb-angle, the level of the apex of the scoliotic primary curve and the age of the patient. Averaged over all patients, the back surface rotation amplitude increased from 23.1° in standing to 26.3° in forward bending posture. The standard deviation of this difference was high (6.1°). The correlation of back surface rotation amplitude in standing with that in forward bending posture was poor (R2=0.41) as was the correlation of back surface rotation in standing posture with the scoliometer in forward bending posture measured rotation (R2=0.35). No significant correlation could be found between the change of back shape in forward bending and the degree of deformity (R2=0.07), likewise no correlation with the height of the apex of the scoliosis (R2=0.005) and the age of the patient (R2=0.001). Before forward bending test leg length inequalities have to be compensated accurately. Compared to the standing posture, forward bending changes back surface rotation. However, this change varies greatly between patients, and is independent of the type and degree of scoliosis. Furthermore remarkable differences were found between scoliometer measurement of the rib hump and rasterstereographic measurement of the vertebral rotation. Therefore the forward bending test and the identification of idiopathic scoliosis rotation by scoliometer can be markedly different compared to rasterstereographic surface measurement in the standing posture.
Keywords: Rasterstereography, Adams test, Scoliometer, Forward bending test, Idiopathic scoliosis
Introduction
As early as 1865 Adams [1] described the forward bending test to assess the trunk asymmetry and axial rotation of the back surface in scoliosis patients. Later the surface rotation was quantified with the so-called scoliometers which enable measuring an angle between the horizontal plane and a plane across the posterior part of the trunk at the level of maximum deformity [2, 3, 5, 10, 12, 13, 18, 20, 21]. The scoliometer is applied to the back surface laterally to the spinous processes and therefore it measures the rotation of the rib cage and not the vertebral rotation. Several authors postulated the scoliometer measurement as a useful and objective criterion for scoliosis screening and quantification, since it is cheap, easy and reliable, provided the measurement is carried out by a single trained observer [2, 3, 19]. Other authors found high inter-observer errors and do not recommend the scoliometer as a standard examination tool in idiopathic scoliosis [6]. Studying the literature it remains unclear whether the axial rotation can merely be better visualized in forward bending or the surface rotation changes in this body posture. In forward bending the spinal column changes its profile completely into a long kyphosis. It is not clear, how this affects the vertebral rotation and vertebral translation of scoliotic spines. Furthermore, the scapulae affect the thoracic back shape, since their position in forward bending posture is completely different from that in standing posture. So far the change of back shape in forward bending posture is the topic of only one study in the literature [23]. Furthermore, it is unclear how leg length inequality affects axial trunk rotation in forward bending. Axial rotation caused by leg length inequality may be misinterpreted as lumbar or rib hump caused by scoliosis. In the literature only one study reported on this problem [26]. With attention to the worldwide use and high clinical relevance of the forward bending test, the number of studies stating changes of the back shape between the standing and the forward bending posture appears very low and a study with a higher number of patients making use of an objective back shape analysis system appeared necessary. For this purpose we used rasterstereography which is in routine clinical use in our department since 1992 and is well evaluated. The ISIS-Scanner [17, 25] and the Quantec-Imaging-System [11, 22] would have been alternatives, whereas Moirè-topography never could gain acceptance for routine clinical use.
Materials and methods
In previous studies rasterstereography has proved to be a reliable method for precise 3D back shape measurement and for the reconstruction of the spinal shape avoiding any radiation exposure of the patient [8, 9, 14–16]. In order to compare the back shape in standing and forward bending posture, two identical rasterstereographic devices were used.
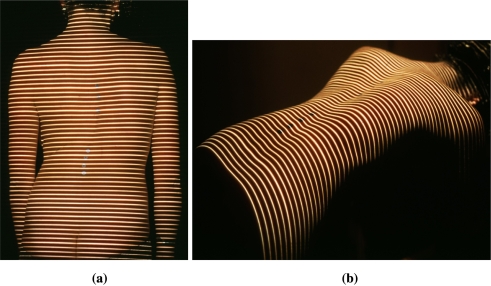
One was positioned behind the patient in the normal upright position, the other one was mounted horizontally above the patient under the ceiling. The distance between the patient’s back surface and the device was equivalent in both positions which enabled precise calibration. The patients were examined in standing posture first. Leg length inequalities were quantified by clinical examination and by rasterstereography and were compensated accurately before the examinations. In correspondence to the Adams test, the patients changed after that into 90° forward bending posture without any other movement and were examined again (Figs. 1a, b; 2a, b).
Fig. 1.
Rasterstereography in standing and forward bending posture
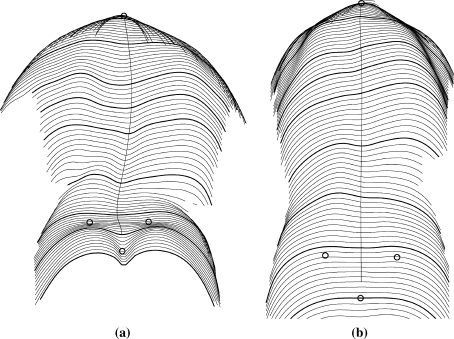
Fig. 2.
Back shape of the same patient in standing (a) and forward bending postures (b)
A pilot study was conducted to analyze the influence of leg length inequality on the axial rotation of the back surface in the area of the lumbar and thoracic spine. Therefore, five healthy men with an average age of 30 years (28–32) were examined with rasterstereography in forward bending posture with artificial leg length inequalities applied to 0.5 cm steps from 3.5 cm on the left down to equality and then up to 3.5 cm on the right (15 measurements/patient). In all measurements of the pilot and the main study, the angle of forward bending was constant and controlled before each examination.
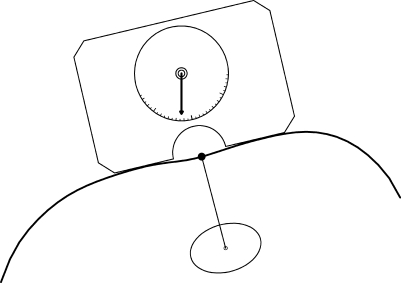
Ninety-one patients with idiopathic scoliosis with Cobb angles of 58° on average (20–82°) were examined comparatively in standing and forward bending posture. Ninety-five comparable record pairs were available. The parameter of interest was the axial back surface rotation in the thoracic and lumbar spine. To be independent of a 3D reference plane, the difference between the maximum right and left axial back surface rotations was calculated (rotation amplitude). Additionally, scoliometer measurement of the rib and lumbar humps was simulated by computer using isolated rasterstereographic transversal profiles of the reconstructed back shape at the levels of maximum deformity (Fig. 3).
Fig. 3.
Computer simulation of scoliometer measurement using isolated rasterstereographic profiles
A computer model similar to the real scoliometer was interactively fitted to the profiles with maximum rotation. Similar to the rasterstereographic rotation measurement, the amplitude between the maximum left and right rotations was calculated instead of the rotation relative to the horizontal plane. This enabled to correlate the scoliometer measurement accurately with the rasterstereographic rotation amplitude.
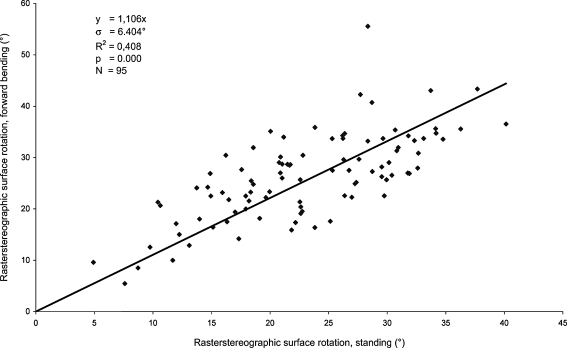
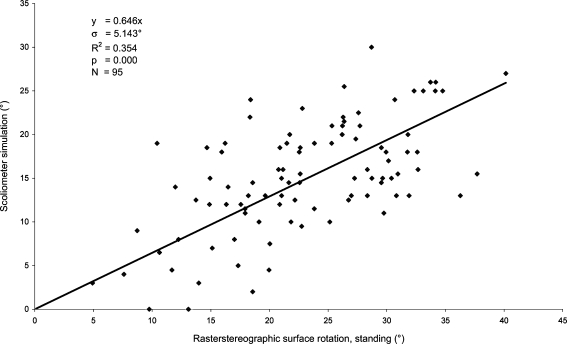
The axial surface rotation amplitude in standing posture was correlated with both that in forward bending posture (Fig. 4) and that calculated by scoliometer simulation (Fig. 5). The differences between the rotation amplitudes in standing and forward bending were correlated with the degree of scoliosis and the level of the apex of the primary curve to clarify whether these parameters had systematical influence on the change of the back shape in forward bending posture. As parameters of the degree of deformity, the amplitudes of rasterstereografic vertebral rotation and lateral vertebral translation in standing posture were considered. The level of the apex of the scoliosis was calculated as the distance between the vertebra prominens and the point of maximum lateral vertebral translation.
Fig. 4.
Correlation of surface rotation in forward bending and standing postures
Fig. 5.
Correlation of simulated scoliometer measurement versus surface rotation in standing posture
Results
Considering the most actual a. p. radiographs, the Cobb angle of the included idiopathic scolioses was 58° on average (20–82°).
In forward bending leg length inequality had direct influence on the axial back surface rotation of the lumbar and the thoracic spine. The relationship between leg length inequality and back surface rotation at L4 is linear. Leg length inequality of 2 cm caused lumbar surface rotation of 5°. In the upper spine this surface rotation decreased systematically. At T6 the rotation was 80% and at C7 63% of the surface rotation measured at L4 (always in the same direction).
On average the rotation amplitude in standing posture was 23.1±7.5° (4.9–40.2°) and increased in forward bending to 26.3±8.3° (5.5–55.6°). The inconsistency of rotation changes in forward posture was high (3.2±6.1°). Compared to the rasterstereographic measurement in forward bending of 26.3°, the rotation amplitude measured by simulated scoliometer was low with 15.2±6.4° (0–30.0°).
The correlation of the rotation amplitude in standing posture with that in forward bending posture was poor (R2=0.41, Fig. 4). Likewise, the correlation of the rasterstereographic standing rotation amplitude with the simulated scoliometer was also poor (R2=0.35, 0.41, Fig. 5). The statistically expected rotation in forward bending is 10.6% higher than in standing posture and the scoliometer measured rotation is 35.4% lower than in standing posture (Figs. 4, 5).
The correlation of the change of rotation with the degree of the deformity was poor (R2<0.1). A trend could be observed that in severe deformities the rotation amplitude in the different postures is more similar. No significant correlation was found between the change of rotation and the level of the apex (thoracic or lumbar) of the primary curve (R2=0.002) or the age of the patient (R2=0.001).
Discussion
The clinical relevance of the presented study is high, since the forward bending test is in use worldwide to detect and quantify scoliosis [10, 20, 21]. School screening programs using the forward bending test could reduce the number of surgically treated spinal deformities significantly by early detection and conduction of non-operative treatment [24]. However, the screening is expensive [27] since children were referred to radiography or to orthopedic surgeons, although they have had no clinically relevant spinal deformity [4]. One reason attributing to this problem may be the low sensitivity and specificity of the forward bending test, postulated by other authors earlier [18]. Some authors reject scoliosis screening since there is generally no evidence that the brace treatment is effective [7].
Leg length inequality influences the back shape directly. Before the forward bending test the examiner has to exclude or compensate leg length inequality accurately, otherwise lumbar and thoracic axial surface rotation can feign a lumbar or rib hump and thus scoliotic deformity. This is particularly important in screening programs to avoid unnecessary radiography. Upadhyay et al. [26] found an influence of leg length on the back shape in forward bending only in case of at least 1 cm inequality.
The most important finding of this study is the high dispersion of the differences between the axial back surface rotation amplitude in standing versus forward bending posture. Obviously, the change of the back shape in forward bending is not systematic. On average, the surface rotation increased by 3.2°; however, the standard deviation is nearly twice as much (6.1°). The back surface rotation can be better visualized for an examiner in forward bending posture of the patient, but it changes unsystematically in a clinically relevant amount. The degree of the deformity and the localization of the apex of the scoliotic curve did not correlate with the difference of axial back surface rotation between standing and forward bending postures. Considering the findings of the study, the use of the forward bending test has to be seen in true perspective: The forward bending test does not clearly relate to the deformity in the standing posture.
Back surface rotation in forward bending posture measured rasterstereographically on the one hand and with simulated scoliometer on the other hand differs considerably by 11.2° on average. This can be explained by the different principles of surface rotation measurement. Rasterstereography measures the surface rotation at the spinous process line. Previous studies showed a high correlation of the surface rotation in this anatomical region with the radiographic vertebral rotation [8, 9, 14]. The scoliometer measures more laterally in the area of the rib cage which does not show the same amount of rotation as the vertebrae. The results demonstrated this impressively. The scoliometer showed only 57% of the rasterstereographically measured rotation amplitude.
Clinical examiners have to be aware of both the variability of back surface rotation in the forward bending test and the underestimation of vertebral rotation with the scoliometer to avoid errors of interpretation. Furthermore the literature reported relevant inter-observer errors [6] of both methods.
Conclusions
Leg length inequality interferes directly with the axial surface rotation of the back and should be compensated accurately before forward bending test.
Axial surface rotation increases in forward bending posture compared to standing by about 3.2° on average; however, the changes showed a high variability. This cannot be explained neither by the degree or type of scoliosis nor by the age of the patient. In the authors’ opinion the standing axial back surface rotation as parameter of the degree of scoliosis cannot be assessed objectively by the forward bending test. This enables better visualization of surface rotation for the clinical examiner, but it is connected with a risk of misinterpretation of spinal deformity.
The scoliometer measures the axial rotation of the rib cage. This is one-third lower the surface rotation measured at the spinous process line.
Rasterstereography provides an objective assessment of back surface rotation in standing posture avoiding the risk of errors due to forward bending and may be an alternative to traditional examination techniques.
References
- 1.Adams W. Lectures on the pathology and treatment of lateral and other forms of curvature of the spine. London: Churchill; 1865. [PMC free article] [PubMed] [Google Scholar]
- 2.Amendt LE, Ause-Ellias KL, Eybers JL, Wadsforth CT, Nielsen DH, Weinstein SL. Validity and reliability testing of the Scoliometer. Phys Ther. 1990;70:108–116. doi: 10.1093/ptj/70.2.108. [DOI] [PubMed] [Google Scholar]
- 3.Bunnel WP. An objective criterion for scoliosis screening. J Bone Joint Surg. 1984;66:1381–1387. [PubMed] [Google Scholar]
- 4.Burwell RG, Webb JK, More EJ. School screening for scoliosis [letter] Lancet. 1981;2:863. doi: 10.1016/S0140-6736(81)91119-3. [DOI] [PubMed] [Google Scholar]
- 5.Burwell RG, Aujla RK, Kirby AS, Moulton A, Webb JK. The early detection of adolescent idiopathic scoliosis in three positions using the Scoliometer and real-time ultrasound: should the prone position also be used? In: Tanguy A, Peuchot B, editors. Research into spinal deformities. Amsterdam/Tokyo: IOS Press/Ohmsha; 2002. pp. 381–385. [PubMed] [Google Scholar]
- 6.Cote P, Kreitz BG, Cassidy JD, Dzus AK, Martel J. A study of the diagnostic accuracy and reliability of the scoliometer and Adam`s foreward bending test. Spine. 1998;23:796–802. doi: 10.1097/00007632-199804010-00011. [DOI] [PubMed] [Google Scholar]
- 7.Dickson RA, Weinstein SL. Bracing (and screening)-yes or no? J Bone Joint Surg (Br) 1999;81-B:193–198. doi: 10.1302/0301-620X.81B2.9630. [DOI] [PubMed] [Google Scholar]
- 8.Drerup B, Hierholzer E. Evaluation of frontal radiographs of scoliotic spines—Part I: Measurement of position and orientation of vertebra and assessment of clinical shape parameters. J Biomech. 1992;25:1357–1362. doi: 10.1016/0021-9290(92)90291-8. [DOI] [PubMed] [Google Scholar]
- 9.Drerup B, Hierholzer E. Evaluation of frontal radiographs of scoliotic spines—Part II: Relations between lateral deviation, lateral tilt and axial rotation of vertebrea. J Biomech. 1992;25:1443–1450. doi: 10.1016/0021-9290(92)90057-8. [DOI] [PubMed] [Google Scholar]
- 10.Dunn BH, Hakala MW, McGee ME. Scoliosis screening. Pediatrics. 1978;61:794–797. [PubMed] [Google Scholar]
- 11.Goldberg CJ, Kaliszer M, Moore DP, Fogarty EE, Dowling FE. Surface topography, Cobb angles, and cosmetic change in scoliosis. Spine. 2001;15:E55–E63. doi: 10.1097/00007632-200102150-00005. [DOI] [PubMed] [Google Scholar]
- 12.Götze HG. Der Rotationsindex bei idiopathischen Thorakalskoliosen. Z Orthop. 1973;111:737–743. [PubMed] [Google Scholar]
- 13.Grossmann TW, Mazur JM, Cummings RJ. An evolution of the Adams foreward bend test and the scoliometer in a scoliosis school screening setting. J Ped Orthop. 1995;15:535–538. doi: 10.1097/01241398-199507000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Hierholzer E. Objektive Analyse der Rückenform von Skoliosepatienten. Stuttgart, New York: Gustav Fischer; 1993. [Google Scholar]
- 15.Hackenberg L, Hierholzer E, Pötzl W, Götze C, Liljenqvist U. Rasterstereographic back shape analysis in idiopathic scoliosis after anterior correction and fusion. Clin Biomech. 2003;18:1–8. doi: 10.1016/S0268-0033(02)00165-1. [DOI] [PubMed] [Google Scholar]
- 16.Hackenberg L, Hierholzer E, Pötzl W, Götze C, Liljenqvist U. Rasterstereographic back shape analysis in idiopathic scoliosis after posterior correction and fusion. Clin Biomech. 2003;18:883–889. doi: 10.1016/S0268-0033(03)00169-4. [DOI] [PubMed] [Google Scholar]
- 17.Johnson MR, Upadhyay SS, Burwell RG, Webb JK. Integrated shape imaging system (ISIS) an evaluation of its capacity to measure lateral spine curves and appraise hump dynamics on forward flexion. J Bone Joint Surg. 1987;69-B:851–852. [Google Scholar]
- 18.Karachalios T, Sofianos J, Roidis N, Sapkas G, Korres D, Nikolopoulos K. Ten-year follow-up evaluation of a scool screening program for scoliosis. Is the forward-bending test an accurate diagnostic criterion for the screening of scoliosis? Spine. 1999;24(22):2318–2324. doi: 10.1097/00007632-199911150-00006. [DOI] [PubMed] [Google Scholar]
- 19.Lonstein JE. Screening for spinal deformities in Minnesota schools. Clin Orthop. 1977;126:33–42. [PubMed] [Google Scholar]
- 20.Murell GAC, Coonrad RW, Moorman CT, Fitch RD. An assesment of the reliability of the scoliometer. Spine. 1993;18:709–712. doi: 10.1097/00007632-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Pearsall DJ, Reid GJ, Hedden DM. Comparison of three non-invasive methods for measuring scoliosis. Phys Ther. 1992;72:648–657. doi: 10.1093/ptj/72.9.648. [DOI] [PubMed] [Google Scholar]
- 22.Sakka SA, Wojcik A, Macindoe S, Metha MH. Reproducibility and reliabilityof the quantec surface imaging system in the assessment of spinal deformity. In: D´Amico M, Merolli A, Santambrogio GC, editors. Three-dimensional analysis of spinal deformities. Amsterdam/Tokyo: IOS Press/Omsha; 1995. pp. 441–445. [Google Scholar]
- 23.Stokes IA, Moreland MS. Measurement of the shape of the surface of the back in patients with idiopathic scoliosis. The standing and foreward-bending position. J Bone Joint Surg. 1987;69:203–211. [PubMed] [Google Scholar]
- 24.Torell G, Nordwall A, Nachemson A. The changing pattern of scoliosis treatment due to effective screening. J Bone Joint Surg. 1981;63-A:337–341. [PubMed] [Google Scholar]
- 25.Turner-Smith AR, Harris JD, Houghton GR, Jefferson RJ. A method for analysis of back shape in scoliosis. J Biomech. 1988;21:497–509. doi: 10.1016/0021-9290(88)90242-4. [DOI] [PubMed] [Google Scholar]
- 26.Upadhyay SS, Burwell RG, Webb JK. The use of the Scoliometer to valuate hump dynamics in relation to leg length in equality and pelvic tilt. J Bone Joint Surg. 1987;69B:851. [Google Scholar]
- 27.Yawn BP, Yawn RA. The estimated cost of school scoliosis screening. Spine. 2000;25:2387–2391. doi: 10.1097/00007632-200009150-00019. [DOI] [PubMed] [Google Scholar]