Abstract
The aim of the study was to assess the results of treatment of adolescent idiopathic scoliosis (AIS) with the Providence nighttime brace at 1.8 years after discontinuation of bracing. A total of 36 consecutive female patients with an average Cobb angle of 28.4° and an apex below T 10 were studied prospectively. For comparisons, 36 matched patients treated with the Boston full-time brace were studied retrospectively. With the Providence night brace an average of 92% for brace correction of the primary curve was achieved and during follow-up progression of the curve >5° occurred in 27% of the patients. In the control group of the Boston full-time brace patients, brace correction was 50% and the progression of the major curve occurred in 22% of the patients. We conclude that the Providence night brace may be recommended for the treatment of AIS with curves less than 35° in lumbar and thoracolumbar cases.
Keywords: Adolescent idiopathic scoliosis, Brace treatment, The Providence night brace
Introduction
Compliance with the brace regime is a large source of bias in the treatment of idiopathic scoliosis with full-time schedules. Low-profile braces and part-time wearing programs have been developed to lessen negative effects during treatment, but they still exist with conventional braces. The ideal solution to improve compliance might be nighttime-only braces.
Price et al. [13] reported excellent in-brace correction and promising early results with the Charleston nighttime bending brace and stated in their follow-up study [14] that nighttime bracing improves natural history and is justified in the treatment.
d’Amato et al. [2] introduced the Providence nighttime brace and concluded that it is effective in preventing the progression of curves <35° and is more successful in lumbar and thoracolumbar than in thoracic curves. The Providence brace is theoretically not based on overbending of the spine but on direct forces to scoliotic curves. This may decrease the risk of progression of secondary curves, which may theoretically worsen the results for bending braces.
There are no studies which compare results for Providence night bracing with the results of conventional full-time bracing. The aim of this study was to assess the effectiveness of the Providence brace in idiopathic scoliosis with low apexes and compare the results with matched patients treated with the Boston brace.
Materials and methods
The Providence night brace was fabricated as described by d’Amato et al. [2]. It is based on the use of a special acrylic frame to apply direct forces to scoliotic curves. A CAD/CAM model is made based on the measurements of the frame. The brace is fabricated from polypropylene plastic and modified to the patient aiming for maximal correction. The brace is planned to apply controlled lateral and rotational forces on the trunk to move the spine toward the midline or beyond it (Figs. 1, 2).
Fig. 1.
The Providence night brace
Fig. 2.
A patient wearing the Providence night brace and lying on her right side. A view from front
A total of 36 consecutive female patients who were treated with the Providence brace were studied prospectively. None of the patients had been treated before with some other method. All the patients completed the treatment with a minimum follow-up of 1 year after discontinuation of bracing.
A control group, which consisted of 36 patients, who had been treated with the full-time Boston brace, was studied retrospectively. For comparisons, every patient in the Providence group was matched to a patient in the Boston group by age, skeletal age, Risser sign, apex of the curve and the curve magnitude.
The inclusion criteria were adolescent idiopathic scoliosis (AIS) with the apex of the primary curve T 10 or below. Curves >25° were braced immediately and curves between 20 and 25° were braced if progressions >5°occurred during observation. Before the initiation of treatment standing postero-anterior (p-a) and lateral radiographs of the entire spine were taken to find out the profiles of the deformity. No pathologic findings (e.g., spondylolysis, spondylolisthesis, congenital anomalies) were registered.
After fitting the brace, a prone p-a radiograph of the spine with the brace on was taken to detect the correction of the primary and secondary curves. Patients were asked to wear the Providence brace during every night for at least 8 h and they were seen after 6 weeks to check adequate fitting of the brace. In the control group a standing p-a radiograph of the spine with the brace on was taken and the patients were asked to wear the Boston brace 23 h/day.
Every patient was monitored in the outpatient clinic after every 6 months and a new brace was fabricated if there was growth or fitting problems. At every visit, standing p-a radiographs of the spine without the brace were taken. Bracing was continued to growth cessation and a Risser sign of at least 4. Treatment was considered to have failed if progressions >5° occurred or if surgery was performed.
The results were analyzed statistically by using Student’s t -test. Values of P<0.05 were taken to represent statistical significance.
Results
The average age at the initiation of treatment was 13.5 years (range 9.3–15.2) for the Providence night brace group and 13.0 years (10.8–15.3) for the Boston full-time brace group. Skeletal age averaged 13.3 years for both groups.
In the Providence group 17/36 (47%) patients were Risser 0–1 and 19/36 (53%) Risser 2–3. In the Boston group the Risser signs were 0–1 18/36 (50%) and 2–3 (50%) 18/36, respectively.
The average major curve magnitude at brace prescription was 28.4° (20–42) in the study group and 28.8° (20–42) in the control group. The corresponding Cobb angles of the secondary curves were 17.7 and 18.8°.
The apex of the major curve was T 10 in 2, T 11 in 1, T 12 in 10, L 1 in 18 and L 2 in 5 in both groups.
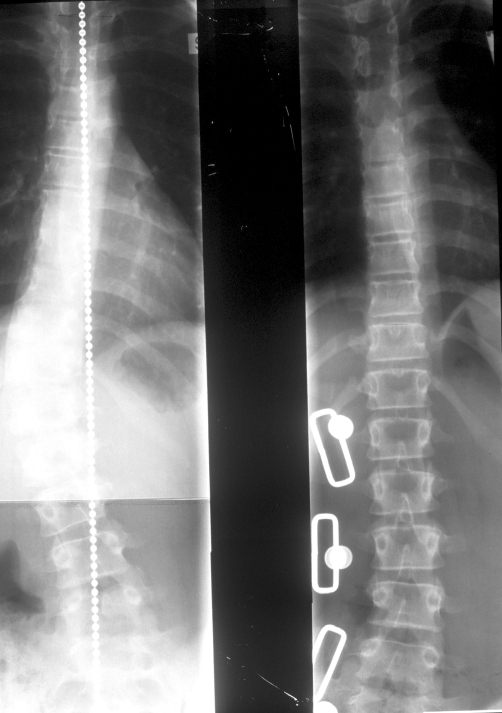
The average correction for the braces as seen on the prone radiographs was 92% for the Providence nighttime brace and in standing radiographs 50% for the Boston group. Corrections >100% were achieved in 31% of the Providence brace patients (Fig. 3).
Fig. 3.
A 12-year-old girl. On the left standing postero-anterior radiograph before bracing. On the right prone radiograph in the Providence brace
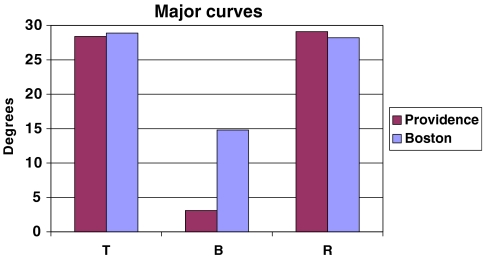
The average length of brace wear was 1.8 years in both groups. Follow-up after discontinuation of bracing averaged 1.8 years in the Providence group and 2.3 years in the Boston group. At the latest follow-up the mean magnitude of the major curve was 29.1° for the Providence patients and 28.2° for the Boston patients. Corresponding figures for secondary minor curves were 21.3 and 20.3°. An increase of Cobb angle >5° of the major curve occurred in 10/36 (27%) in the Providence group and in 8/36 (22%) in the Boston group. There was no statistical difference in the results of treatment between the groups (Table 1).
Table 1.
Comparison of Cobb angles between the Providence night brace and the Boston brace. T Before treatment, B in brace, R result of treatment
The average increase of the secondary minor curve was 2.5° for the Providence brace patients and 1.5° for the Boston patients with no statistical significance between the groups.
One patient who had been treated with the Providence progressed to surgical level and was operated on using anterior instrumentation. In the Boston group none of the patients needed operative treatment.
There was no statistical significance for the results between Risser 0–1 and 2–3 in the Providence patients.
Discussion
Association between brace correction and risk of curve progression has been demonstrated in several studies of full-time braces [3, 11] and also for part-time wear [4, 15]. The results of treatment with braces seem to correlate with dose response wear.
The fundamental idea of nighttime-only bracing is to decrease the negative effects of brace wear to the quality of life without worsening the final results of treatment. This is theoretically possible with better brace correction and better compliance with wear. These are probably the only factors which we can influence during brace treatment of scoliosis.
In-brace correction with full-time braces has ranged in previous studies from about 40 to 60% [3, 5, 10, 18] and it has been suggested that to be effective correction in brace should be >50%. Theoretically, in-brace correction with nighttime braces should be much higher because of the much reduced wear time per day. Price et al. [13] reported that 73% in-brace correction on supine radiographs with the Charleston bending brace. d’Amato et al. [2] in their study of 102 female patients achieved an average of 96% initial in-brace correction for all curves with the Providence nighttime brace. The average percentage of Cobb angle correction for thoracolumbar curves was 111% and for lumbar curves 103%. In this study the apex of all major curves was T 10 or below and the average initial in-brace correction was 92% and a correction >100% was achieved in 11/36 (31%) of cases. These figures were much better than the 50% in-brace correction in the Boston group. The real difference in the correction percentage is probably not as high, because radiographs were taken prone after night bracing and it has been shown that Cobb angles may differ between supine (or prone) and standing radiographs 10–35% [17]. However, the Providence night brace produced significantly better initial in-brace correction than the Boston brace.
Compliance with the brace is a problem especially with full-time braces because it is impossible to monitor compliance accurately. It is evident that true brace compliance is less than estimated clinically and by the patient questionnaire. Studies of compliance monitoring by a data logger and a temperature sensor have shown that the patients overreport their hours of brace wear. This also applies to part-time wearers [16]. It has been usually assumed that nighttime-only bracing improves compliance. However, actual compliance is difficult to assess, because many patients occasionally undress the brace during sleep. In this study we did not use any monitoring but we asked during follow-up visits, if the patients had any difficulties with wearing the brace. None of 36 patients with the Providence brace were totally noncompliant, but it is evident that true compliance is less than estimated with night braces too.
Any orthotic treatment of idiopathic scoliosis should improve the natural history of the disease and it has been generally accepted that treatment has failed if there is progression >5° in the Cobb angle. Natural history studies have suggested that the risk of progression increases with the magnitude of the curve and in young patients [1, 9]. Lonstein and Carlson [6] reported that patients with Rissers 0 or 1 and curves of 20–29° had a 68% rate of progression. Nachemson et al. [8] reported in their prospective study of scoliotic female patients with curves between 25 and 35° the progression of 66% of curves of untreated patients. The natural history of larger curves with Cobb angles between 35 and 45° has remained obscure but the literature is almost uniform in its conclusion that an increase in curve magnitude also increases the risk of progression in the growing spine. Several studies of full-time bracing have confirmed that brace treatment in AIS improves the natural history of the disease [7, 12, 15].
Price et al. [14] reported failures of treatment with the Charleston bending brace in 34% of patients and suggested that nighttime bracing in AIS is justified. d’Amato et al. [2] concluded that the results of treatment with the Providence night brace system were successful in >90% of cases for thoracolumbar and lumbar curves <35°. In this study the results of treatment were somehow inferior and progression of major curve >5° occurred in 27% of patients. However, the data in this study supports d’Amatos conclusion that the Providence night brace improves the natural history of idiopathic scoliosis with curves <35°, at least for thoracolumbar and lumbar curves.
The efficacy of bracing in idiopathic scoliosis has been widely studied with conventional full-time braces. Most of them report that up to 20–35% of the curves progress >5° for different reasons [3, 8]. Nighttime bracing may be regarded as justified if the results of treatment with night braces in preventing progression are comparable with the results of full-time bracing. It is difficult to draw conclusions from the available reports and comparative studies are needed. Katz et al. [5] examined 319 patients with AIS treated with either the Boston brace or the Charleston bending brace. They concluded that the Boston brace is more effective in preventing curve progression but night bracing should be considered in the treatment of thoracolumbar and lumbar curves <35°, for which both orthoses were comparably effective. Our results are in accordance with Katz’s results and we did not find statistical differences between the results of the Providence nighttime bracing and the Boston full-time bracing. This confirms the concept that nighttime bracing may be justified at least with thoracolumbar and lumbar curves in adolescent idiopathic scoliosis.
Price et al. [14] discussed the difficulties of unbending two opposite curves and the increased risk of progression of the compensatory curves with the Charleston bending brace. In this study we did not find differences in this sense between the full-time conventional and nighttime bracing. This result suggests that Providence nighttime bracing probably does not increase the risk of the progression of secondary curves.
The aim of this study was not to widely analyze the factors which have an influence on the risk of curve progression with nighttime bracing. The number of Risser 2–3 was quite high (53%) but we included these patients in the study because this represents the usual situation when the indication of bracing has been detected a little late. In this series of night bracing, we did not find any statistical significance between Risser 0–1 and 2–3 in the progression of the curves. However, this finding requires more data to be ascertained one way or another.
In conclusion, with the Providence night brace, very good in-brace correction (mean 92%) on supine radiographs was achieved. A total of 27% of the curves progressed >5° during follow-up but these results were comparable with the results of full-time Boston bracing. The results of this study suggest that the Providence night brace may be recommended in the treatment of AIS with curves <35° in lumbar and thoracolumbar cases.
References
- 1.Bunnell WP. the natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986;11:773–776. doi: 10.1097/00007632-198610000-00003. [DOI] [PubMed] [Google Scholar]
- 2.d’Amato CR, Griggs S, McCoy Nighttime bracing with the Providence brace in adolescent girls with idiopathic scoliosis. Spine. 2001;26:2006–2012. doi: 10.1097/00007632-200109150-00014. [DOI] [PubMed] [Google Scholar]
- 3.Emans JB, Kaelin A, Bancel P, Hall Miller JE; ME. The Boston bracing system for idiopathic scoliosis. Follow-up results of 295 patients. Spine. 1986;11:792–801. doi: 10.1097/00007632-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Green NE. Part-time bracing of adolescent idiopathic scoliosis. J Bone Joint Surg (Am) 1986;68:738–742. [PubMed] [Google Scholar]
- 5.Katz DE, Richards BS, Browne RH, Herring JA. A comparison between the Boston brace and the Cherleston bending brace in adolescent idiopathic scoliosis. Spine. 1997;22:1302–1312. doi: 10.1097/00007632-199706150-00005. [DOI] [PubMed] [Google Scholar]
- 6.Lonstein JE, Carlson JM. The prediction of curve progression in untreated scoliosis during growth. J Bone Joint Surg (Am) 1984;66:1061–1071. [PubMed] [Google Scholar]
- 7.Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis: a review of one thousand and twenty patients. J Bone Joint Surg (Am) 1994;76:1207–1221. doi: 10.2106/00004623-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis: a prospective, controlled study based on data from the Brace study of the Scoliosis Research Society. J Bone Joint Surg (AM) 1995;77:815–821. doi: 10.2106/00004623-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Nachemson A, Lonstein JE, Weinstein SL (1982) Prevalence and natural history committee report. Read at the annual meeting of the scoliosis research society. Denver, Colorado
- 10.Olaffsson Y, Saraste H, Söderlund V, Hoffsten M. Boston brace in the treatment of idiopathic scoliosis. J Ped Orthop. 1995;15:524–527. doi: 10.1097/01241398-199507000-00023. [DOI] [PubMed] [Google Scholar]
- 11.Peltonen J, Poussa M, Ylikoski M. Three-year results of bracing in scoliosis. Acta Orthop Scand. 1988;59:487–490. doi: 10.3109/17453678809148769. [DOI] [PubMed] [Google Scholar]
- 12.Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity; logistic regression analysis based on the data from the Brace study of the Scoliosis Research Society. J Bone Joint Surg (Am) 1995;77:823–827. doi: 10.2106/00004623-199506000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Price CT, Scott DS, Reed FE, Jr, Riddick MF. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace: preliminary report. Spine. 1990;15:1294–1299. doi: 10.1097/00007632-199012000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Price CT, Scott DS, Reed FE, Jr, Sproul JT, Riddick MF. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace: long-term follow-up. J Ped Orthop. 1997;17:703–707. doi: 10.1097/00004694-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatment for idiopathic scoliosis. J Bone Joint Surg Am. 1997;79:664–674. doi: 10.2106/00004623-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Takemisu M, Bowen R, Rahman T, Glutting J, Scott C. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine. 2004;29:2070–2074. doi: 10.1097/01.brs.0000138280.43663.7b. [DOI] [PubMed] [Google Scholar]
- 17.Torell G, Nachemson A, Haderspeck-Grip K, Schultz A. Standing and supine Cobb measures in girls with idiopathic scoliosis. Spine. 1985;10:425–427. doi: 10.1097/00007632-198506000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Willner S. Effect of the Boston thoracic brace on the frontal and sagittal curves of the spine. Acta Orthop Scand. 1984;55:457–460. doi: 10.3109/17453678408992394. [DOI] [PubMed] [Google Scholar]