Abstract
For anterior correction and instrumentation of thoracic curves single rod techniques are widely used. Disadvantages of this technique include screw pullouts, rod fractures and limited control of kyphosis. This is a prospective study of 23 consecutive patients with idiopathic thoracic scoliosis treated with a new anterior dual rod system. Aim of the study was to evaluate the safety and efficacy of this new technique in the surgical treatment of idiopathic thoracic scoliosis. To the best knowledge of the authors, this is the largest series on dual rod dual screw instrumentation over the entire fusion length in thoracic scoliosis. Twenty-three patients with an average age of 15 years were surgically treated with a new anterior dual rod system through a standard open double thoracotomy approach. Average clinical and radiological follow-up was 28 months (24–46 months). Fusion was carried out mostly from end-to-end vertebra. The primary curve was corrected from 66.6° to 28.3° (57.5% correction) with an average loss of correction of 2.0° at Cobb levels and of 1.3° at fusion levels. Spontaneous correction of the secondary lumbar curve averaged 43.2% (preoperative Cobb angle 41.2°). The apical vertebral rotation was corrected by 41.1% with a consecutive correction of the rib hump of clinically 66.7%. The thoracic kyphosis measured 29.2° preoperatively and 33.6° at follow-up. In seven patients with a preoperative hyperkyphosis of on average 47.3° thoracic kyphosis was corrected to 41.0°. This new instrumentation enables an entire dual rod instrumentation over the whole thoracic fusion length. It offers primary stability without the need of postoperative bracing. Dual screw dual rod instrumentation offers the advantages of a high screw pullout resistance, an increased overall stability and satisfactory sagittal plane control.
Keywords: Idiopathic scoliosis, Thoracic scoliosis, Anterior fusion, Selective fusion, Dual rod instrumentation
Introduction
Dwyer was the first author reporting in 1969 on anterior correction and instrumentation of a thoracic scoliosis [6]. However, with the Harrington- and later the Cotrel–Dubousset Instrumentation posterior fusion became the gold standard in the surgical treatment of thoracic scoliosis [5, 15]. The indications for anterior procedures i.e. the Zielke Instrumentation were mainly limited to thoracolumbar and lumbar curves [9, 11, 17, 33].
Some 30 years later, first reports on anterior correction and instrumentation of thoracic curves emerged. The advantages of the anterior technique included a shorter fusion length, a better derotation and a better correction of both primary and the non-instrumented secondary lumbar curves compared to the posterior procedures. The disadvantages, however, were a higher pseudarthrosis rate due to the lack in stability with frequent rod fractures, screw pullouts and the need for postoperative bracing or even casting [1, 3, 14, 22, 25, 30].
To overcome the disadvantages of anterior single rod techniques, several dual rod systems were developed by different authors [12, 16, 18]. However, due to the size of the plates, its application was mainly limited to thoracolumbar and lumbar curves. Kaneda was the first author to report on anterior dual rod instrumentation in thoracic scoliosis; however, the dual rod instrumentation was rarely carried out higher than T8 [19].
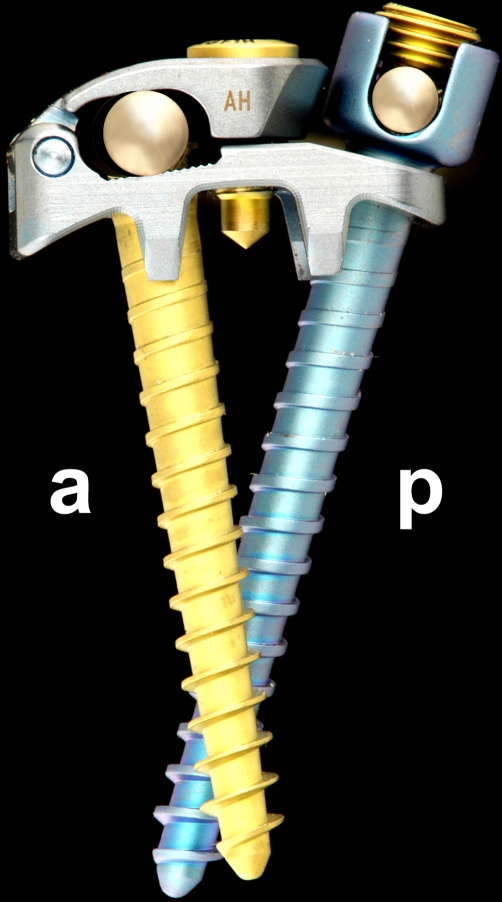
The Halm–Zielke Instrumentation (HZI) is a dual rod system consisting of a flexible 4 mm smooth or threaded rod and a solid fluted 5 mm rod fixed by a lid-plate with a more anteriorly placed sunk screw and a more posteriorly placed either Zielke screw (for the threaded rod) or top loading screw (for the 4 mm smooth rod) (Fig. 1). The reported results on thoracolumbar and lumbar curves have demonstrated good correction results with an implant failure rate below 5% [4, 12, 13]. For its use in thoracic curves, the plate and screws were downsized, still being fully compatible with the original system. After extensive biomechanical testing at the University of Esslingen/Germany (Head: Prof. Dr. L. Issler) and after its CE marking, it was introduced for clinical use in 2000.
Fig. 1.
Lateral view of the Halm–Liljenqvist instrumentation, with posterior 4 mm smooth rod and top loading screw (p) and closed lid-plate with anterior sunk screw and anterior solid fluted 5 mm rod (a)
Aim of this prospective study was to present the preliminary results of 23 consecutive patients with idiopathic thoracic scoliosis having been surgically treated with this new anterior dual rod system and to compare these results with the published reports on anterior correction and fusion in thoracic curves.
Materials and methods
Between May 2000 and January 2003, 24 patients with idiopathic right-sided thoracic scoliosis were surgically treated at our institution using the new anterior dual rod system (Halm–Liljenqvist Instrumentation, DePuy Spine, Kirkel-Limbach, Germany). One patient left the country and was thus lost to follow-up. The average age at surgery was 15.0 years (12–19 years). In Table 1, the clinical data including curve type and fusion length are summarized. The clinical and radiometric data were collected prospectively by an independent observer. All patients were operated by one surgeon (U. L.). Average follow-up was 28.3 months (24–46 months). Rib hump, lumbar hump and trunk decompensation were measured clinically. Perioperative parameters including operating time, intraoperative blood loss, transfusion of autologous and homologous blood as well as intra- and postoperative complications were documented. The SRS-24 questionnaire in German translation was sent to 23 patients with a 100% return rate at follow-up. This questionnaire consists of 24 questions divided into following seven domains: pain, general self-image, postoperative self-image, general function, overall level of activity, postoperative function, and satisfaction. Each item is scored on a five-point scale with a score of 5 representing a good outcome and a score of 1 being a poor outcome [10].
Table 1.
Data on 23 patients and the Cobb angle of the main thoracic curve (MTC) and the secondary lumbar curve (LC)
| Patient No. | Age (years) | Curve type | Curve length | Fusion length | Preop MTC | Bending MTC | Postop MTC | Follow-up MTC | Preop LC | Bending LC | Postop LC | Follow-up LC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 14 | 1C+ | T6-T11 | T6-T12 | 50 | 22 | 28 | 30 | 43 | 12 | 40 | 34 |
| 2 | 19 | 1A− | T5-T12 | T6-T12 | 56 | 12 | 18 | 18 | 30 | 0 | 15 | 12 |
| 3 | 14 | 1CN | T6-T11 | T6-T11 | 60 | 33 | 30 | 34 | 45 | 17 | 30 | 30 |
| 4 | 17 | 2BN | T6-T12 | T5-T11 | 76 | 63 | 33 | 39 | 45 | 20 | 25 | 34 |
| 5 | 13 | 1CN | T6-T12 | T6-T12 | 70 | 44 | 28 | 32 | 50 | 24 | 29 | 32 |
| 6 | 17 | 1BN | T6-T11 | T6-T11 | 54 | 45 | 27 | 29 | 40 | 15 | 28 | 28 |
| 7 | 13 | 1B+ | T5-T12 | T5-T12 | 77 | 46 | 34 | 37 | 48 | 7 | 32 | 28 |
| 8 | 12 | 1C+ | T7-T12 | T7-L1 | 79 | 42 | 29 | 28 | 55 | 18 | 35 | 28 |
| 9 | 16 | 1B+PT | T6-T12 | T6-T12 | 76 | 45 | 36 | 39 | 46 | 16 | 26 | 27 |
| 10 | 15 | 1BN | T6-T12 | T6-T12 | 60 | 34 | 32 | 32 | 36 | 5 | 23 | 24 |
| 11 | 17 | 2A− | T5-T11 | T5-T11 | 63 | 54 | 33 | 33 | 13 | -20 | 2 | 8 |
| 12 | 15 | 1BN | T7-T12 | T5-T12 | 50 | 20 | 21 | 25 | 42 | 7 | 29 | 26 |
| 13 | 12 | 3BN | T6-T12 | T6-L2 | 85 | 60 | 30 | 30 | 53 | 34 | 35 | 35 |
| 14 | 12 | 1A− | T6-T12 | T6-T12 | 74 | 24 | 24 | 28 | 35 | 5 | 32 | 20 |
| 15 | 16 | 2A+ | T5-T12 | T6-L1 | 70 | 35 | 19 | 18 | 30 | 8 | 5 | 2 |
| 16 | 18 | 1C− | T7-T12 | T7-L3 | 66 | 43 | 30 | 30 | 58 | 10 | 15 | 18 |
| 17 | 17 | 1CN | T6-T12 | T6-T12 | 58 | 35 | 22 | 25 | 48 | 20 | 25 | 27 |
| 18 | 14 | 1B+ | T6-T12 | T6-T12 | 57 | 25 | 35 | 35 | 35 | 0 | 28 | 18 |
| 19 | 15 | 2BN | T5-T11 | T5-T11 | 65 | 46 | 28 | 28 | 40 | 14 | 20 | 16 |
| 20 | 15 | 2CN | T6-T12 | T6-T12 | 74 | 42 | 28 | 32 | 52 | 16 | 38 | 31 |
| 21 | 19 | 1BN | T7-T12 | T7-T12 | 50 | 32 | 20 | 23 | 33 | 4 | 23 | 26 |
| 22 | 14 | 1A− | T6-T12 | T6-T12 | 80 | 43 | 32 | 35 | 31 | 18 | 15 | 16 |
| 23 | 12 | 1A+ | T6-T12 | T6-T12 | 83 | 32 | 35 | 38 | 40 | 13 | 28 | 19 |
| Average | 15.0 | 66.6±11.2 | 38.1±12.5 | 28.3±5.4 | 30.3±5.9 | 41.2±10.2 | 11.4±10,5 | 25.1±9,6 | 23.4±8.7 |
Radiographic analysis included Cobb angle measurements of the primary and secondary curves and of their flexibility on bending films. All curves were classified according to the Lenke's classification [23]. The vertebral rotation of the thoracic and lumbar apex vertebra was measured according to Perdriolle [27]. Furthermore, the tilt angle of the lowest instrumented vertebra (LIV) was documented. Translation of the apical vertebra of the thoracic curve was measured as the distance of the center of the apical vertebra from the central sacral vertical line (CSVL) in centimetres. Shoulder balance was measured comparing the points of intersection of the clavicles with the first or second rib. Trunk decompensation was determined as the deviation of the CSVL from the spinous process of C7 in centimetres. Sagittal plane analysis included measurement of thoracic kyphosis (T4 – T12), thoracolumbar junction (T10 – L2) and lumbar lordosis (L1 – L5). Sagittal trunk decompensation was measured as the deviation of the plumb-line from C7 from the center of the disc L5/S1 in centimetres. Long cassette anterior–posterior and lateral standing radiographs were obtained preoperatively, postoperatively and at follow-up.
Surgical technique
After administration of general anaesthesia and placement of a double lumen tube, the patient is prepared in a left lateral position. The skin is usually incised over the 7th rib and the latissimus dorsi muscle is cut. The lower thoracotomy is performed between the 8th and 9th rib after incising a few centimetres of the external oblique abdominal muscle. Via this lower thoracotomy the lower three to four discs can be excised. To get access to the upper and midthoracic spine, the anterior serratus muscle is detached from its origin at the chest wall and usually the 5th rib is removed. The upper discs are excised. Disc excision should be complete and the posterior longitudinal ligament should be visualized. This approach enables an instrumentation between T5 and L1. The selection of fusion levels mostly corresponds to the Cobb levels (end-to-end vertebra). For a more distal fusion level the diaphragm needs to be detached and the psoas muscle is mobilized. The technique of instrumenting and correcting the spine has extensively been reported by Halm et al. [4, 12, 13]. The lid-plates are placed on the lateral aspect of the vertebral body. At the beginning of the series, every level was instrumented with a lid-plate; later we changed to every second level with a single screw and a washer in-between. At the upper levels, parts of the ribheads need to be excised to enable an appropriate lid-plate placement. For screw insertion the holes are prepared with an awl and explored with a sounder to exclude any posterior vertebral cortex violation. The more posteriorly placed Zielke or top loading screws should be directed parallel to the posterior longitudinal ligament. Routinely, a bicortical screw purchase is aimed for, however, excessive contralateral penetration must be prevented in order not to risk any impingement of the aorta [29]. Proper screw length is ensured by manually palpating the contralateral screw tips with the finger. To enable an accurate screw length the different screw lengths are available in 2.5 mm increments.
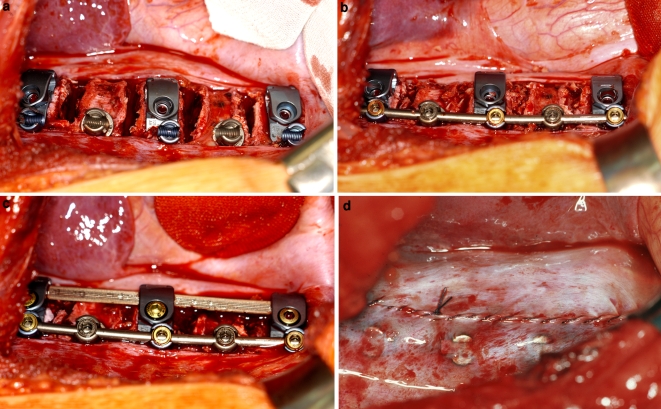
Curve correction is achieved by intersegmental compression routinely using the more posteriorly placed smooth 4 mm rod or in more rigid curves the 4 mm threaded Zielke rod. The segmental derotation is achieved by bringing the individually and according to the vertebral rotation displaced screw heads into one line by inserting the posterior rod. Prior to curve correction the endplates are prepared and the disc spaces are filled with morselized bone chips from the resected rib. Finally, the solid rod is bent according to the residual frontal curve and to the aimed thoracic kyphosis and is inserted into the lid-plates. Additionally either slight segmental compression (to increase kyphosis) or distraction (to decrease kyphosis) can be administered. Due to the low profile of the implant (8.5 mm), the parietal pleura can be completely closed with a running stitch (Fig. 2).
Fig. 2.
a Intraoperative situation after disc resection and placement of the lid-plates and the screws. Note that the lid-plates are placed on every other vertebra with single top-loading screws and washers in-between. b The disc spaces are filled with morselized rib grafts and correction with the more posterior smooth rod has been obtained by segmental compression. c Second rod has been inserted and the lid plates are closed. d Due to the low implant height (8.5 mm) a complete closure of the parietal pleura with a running stitch is possible
The patients are mobilized without any external support on the first postoperative day. The chest drain was removed on average on the 5th postoperative day. In five patients with a residual lumbar curve greater than 25° a brace treatment was initiated to control the lumbar curve until skeletal maturity. In one patient (no. 11) with a rigid thoracic lordoscoliosis, the anterior procedure was preceeded by a posterior release in one stage. Costoplasties were not performed in any case.
Results
Average operative time was 218 min (120–330 min) with an average intraoperative blood loss of 660 ml (200–1,500 ml). Predonated autologous blood was retransfused in ten patients; in two patients, additional homologous blood transfusion was necessary. In nine cases the amount of the intraoperatively salvaged blood loss was sufficient to retransfuse an average amount of 352 ml.
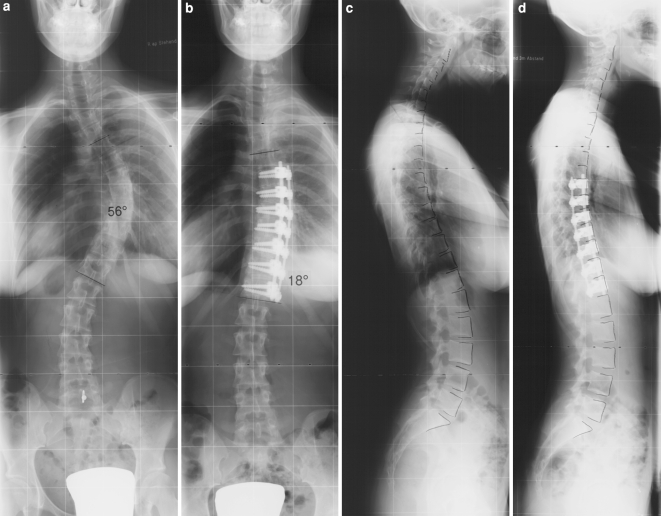
The data on the Cobb angles of the main thoracic and the secondary curves have been compiled in Table 1. Within the instrumented levels of the thoracic curve the Cobb angle was reduced from 66.2±10.6° to 27.4±5.8° (58.6% correction) with an average loss of correction of 1.3°. The proximal thoracic curve measured 33.0±6.7° (20–46°) preoperatively with a flexibility of 39.4% on reverse bending films. Spontaneous curve correction averaged 37.6% with a final Cobb angle of 20.6±6.3° (9–30°) (Figs. 3, 4).
Fig. 3.
A 19-year-old female patient with Lenke type 1A- curve (patient no. 2). a Preoperative Cobb angle of 56°. b Halm–Liljenqvist instrumentation from T6 to T12 with a Cobb angle of 18° and a balanced spine at follow-up. c Preoperative thoracic kyphosis of 12°. d At follow-up, normal thoracic kyphosis of 28°
Fig. 4.
A 15-year-old female patient with Lenke type 2CN curve (patient no. 20). a Preoperative Cobb angle of 74° for the thoracic and 52° for the lumbar curve. b Halm–Liljenqvist instrumentation from T6 to T12 and 1 year of postoperative brace treatment to control the lumbar curve. At follow-up, thoracic Cobb angle of 32° and lumbar Cobb angle of 31° with a balanced spine. c Preoperative thoracic kyphosis of 26°. d Lateral view at follow-up demonstrates normal thoracic kyphosis of 25°
The radiographic data on rotation, translation and tilt of the LIV as well as shoulder and trunk balance are compiled in Table 2. The average correction of the apical vertebral rotation was 41.1% and that of the apical vertebral translation was 80.0%. The tilt of the LIV was corrected by an average of 65.6%. Shoulder imbalance was corrected from 0.8 cm preoperatively to 0.3 cm at follow-up. Trunk imbalance remained unchanged with 1.3 cm (0–3 cm) preoperatively and 1.4 cm at follow-up (0–3 cm). Radiographically, there was no spontaneous derotation of the lumbar spine with an apical vertebral lumbar rotation of 11.5° (0–30°) preoperatively and 11.7° (0–30°) at follow-up.
Table 2.
Radiographic data on transverse and coronal plane measurements
| Preoperative | Latest follow-up | |
|---|---|---|
| Apical thoracic vertebral rotation | 27.0° (12–40°) | 15.9° (10–25°) |
| Apical thoracic vertebral translation | 5.0 cm (1.1–8.5 cm) | 1.0 cm (−1.0 to 3.3 cm) |
| Tilt LIVa | 30.5° (20–40°) | 10.5° (0–20°) |
| Shoulder height | 0.8 cm (0–2.0 cm) | 0.3 cm (0–1.5 cm) |
| Coronal balance | 1.3 cm (0–3.0 cm) | 1.4 cm (0–3.0 cm) |
aLowest instrumented vertebra
Concerning the different lumbar modifier five of the six preoperative A modifier remained A modifier and one changed to B modifier. Of the ten preoperative B modifier three remained B modifier, one changed to A and six to C and of the seven C modifier six remained C and one changed to B modifier at the latest follow-up. The preoperative lumbar Cobb angle averaged 31.8° (modifier A), 42.9° (modifier B) and 45.9° (modifier C), respectively, and corrected spontaneously by 56, 34 and 43%, respectively, at latest follow-up. However, the modifier A curves were more flexible (85% correction on bending films) compared to the B (69% correction) and C modifier (71% correction). Whereas the translation of the lumbar apex vertebra remained unchanged in the A and C modifier, it increased by 29% from 1.7 cm preoperatively to 2.2 cm at the latest follow-up in the B modifier group. There were no cases of trunk decompensation in any groups.
Overall, thoracic kyphosis was increased from 29.2° preoperatively to 33.6° at follow-up. The average sagittal Cobb angle at the instrumented levels remained unchanged during follow-up (22.5° preoperatively, 21.3° postoperatively, 21.9° at follow-up). In seven patients with a preoperative hypokyphosis of on average 9.6° (−5 to 18°) thoracic kyphosis was corrected to 28.9° (17 – 44°). Six of these cases, had a normal thoracic kyphosis of more than 20° at follow-up. In seven patients with a preoperative hyperkyphosis of on average 47.3° (41–62°) thoracic kyphosis was corrected to 41.0° (22–60°). In five of these cases normal thoracic kyphosis was restored (<40°).
On scoliometer measurement correction of the rib hump averaged 66.7% with 17.4° preoperatively and 5.8° at follow-up. The lumbar hump corrected spontaneously from 5.5° preoperatively to 1.7° at follow-up (69.1% correction). Trunk imbalance measured 0.6 cm preoperatively and 0.3 cm at follow-up (Fig. 5). In the SRS-24 questionnaire, a mean overall score of 3.8±0.4 was achieved. The preoperative scores for pain, self-image and function were 3.5±0.6, 3.0±1.2 and 3.8±0.7, respectively. At follow-up, these scores changed to 3.8±0.7 (P=0.29), 4.0±0.8 (P=0.02) and 3.3±1.1 (P=0.18), respectively. The satisfaction with surgery rated 4.0±1.0.
Fig. 5.
Clinical pictures of patient no. 20 (Fig. 4). a Preoperatively, right shoulder elevation of 1.5 cm and asymmetric waist lines. b At follow-up, balanced spine with leveled shoulders and symmetric waist lines. c Preoperative situation in forward bending with a rib hump of 15°. d At follow-up, satisfactory correction of the rib hump deformity
Complications
Postoperatively, two patients developed an atelectasis of the left lung requiring a bronchoscopic lavage on the first postoperative day with an uneventful further course. Two patients (patients number 1 and 11) had a fractured threaded rod at the 12 months follow-up. At latest follow-up of these two patients (both 36 months follow-up) both patients were free from any symptoms, there were no evidences of pseudarthrosis or any significant loss of correction. There were no neurological complications or deep infections.
Discussion
Posterior instrumentation and fusion represent the gold standard in the treatment of idiopathic thoracic scoliosis. However, there are reports in the literature indicating favourable results of anterior instrumentation and fusion in terms of a better three-dimensional curve correction and a shorter fusion length [1, 3, 14, 22, 25, 30]. In this prospective study, 23 consecutive patients were treated with an anterior dual rod instrumentation and fusion. The average fusion length was 6.1 segments with an average frontal curve correction of 58% and a loss of correction of 1.3° within fusion levels.
In publications on standard open single rod instrumentation in thoracic scoliosis the reported primary curve correction ranges from 43 to 58% with a loss of correction of 1 to 5° and a pseudarthrosis rate of up to 6% [3, 7, 20, 22, 30]. Betz et al. [1] reported on a loss of correction of more than 10° in 23% of their patients. With endoscopic techniques correction rates between 51 and 84% have been published [21, 29, 32]. Kaneda et al. [19] published a paper on 20 patients with thoracic scoliosis treated with the Kaneda dual rod system. Average curve correction was 71% with a loss of correction of 1° and a pseudarthrosis rate of 5%. However, a full-length dual rod instrumentation including the upper fusion levels could only be carried out in eight patients (Table 3). In his surgical technique, Kaneda points out that a dual rod instrumentation proximal to T8 is rarely possible due to the small size of the vertebral bodies. In the present series, a full-length dual rod instrumentation was possible in all patients.
Table 3.
Compiled data on correction results of anterior spinal instrumentation and fusion in thoracic curves
| Authors | N | Surgical technique | Instrumentation | Preop MTC (°) | Flexibilitya | Postop MTC | Correction (%) |
|---|---|---|---|---|---|---|---|
| Kaneda et al. (1997) | 20 | Open | (Dual rod)b | 65 | Not provided | 19° | 71 |
| Lenke et al. (1999) | 70 | Open | Single rod | 57 | 42% | 24° | 58 |
| Sweet et al. (2001) | 43 | Open | Single rod | 55 | Not provided | 29° | 47 |
| Kuklo et al. (2001) | 41 | Open | Single rod | 58 | 47% | 28° | 52 |
| Bullmann et al. (2003) | 64 | Open | Single rod | 63 | 59% | 27° | 58 |
| Lenke (2003) | 11 | Endoscopic | Single rod | 53 | Not provided | 26° | 51 |
| Sucato et al. (2004) | 14 | Endoscopic | Single rod | 56 | 53% | 9° | 84 |
| Edwards et al. (2004) | 15 | Open | Single rod (n=10) Dual rod (n=5) |
56 | 55% | 32° | 43 |
| Wong et al. (2004) | 12 | Endoscopic | Single rod | 52 | 37% | 20° | 62 |
| Present study | 23 | Open | Dual rod | 67 | 43% | 28° | 58 |
aCurve correction on preoperative bending
bFull length dual rod instrumentation in only eight patients
The major disadvantages of anterior single rod instrumentations are especially proximal screw pullouts of up to 20% and rod fractures of up to 31% as well as a pseudarthrosis rate of up to 6% [1, 2, 14, 30]. There were no cases of pseudarthrosis or intraoperative screw pullout in the present series. However, we observed two cases with fractures of the threaded rod within the first postoperative year without any relevant loss of correction. This phenomenon of Zielke rod fractures despite bony union has been reported by several other authors [1, 3, 12, 13, 14]. To prevent this and to eliminate the “fiddling factor” of the Zielke rod, we now routinely use the 4 mm smooth rod. However, in cases of very rigid curves we still prefer the threaded rod due to its high flexibility and its gradual correcting abilities. Techniques to increase the fixation strength of the screws include a bicortical screw fixation and a dual screw fixation. Ogon et al. [26] demonstrated an increase of the fixation strength of a dual screw construct by 80% compared to a single screw instrumentation.
Despite selective thoracic fusion in all but one patient (patient number 16), there were no cases of lumbar curve decompensation or marked trunk imbalance. The preoperative Cobb angles of the secondary lumbar curves ranged from 13 to 55° and corrected down to less than 25° on side bending in all but one patient. Numerous studies have shown, that in primary thoracic curves even with secondary lumbar curves up to 50° a selective fusion can be performed safely [3, 7, 14, 19, 22, 23, 24, 30]. An interesting finding was that in six out of ten cases with a preoperative lumbar modifier B, the apical vertebral translation progressed and the modifier changed to C despite an average spontaneous lumbar curve correction of 34%. In the lumbar modifier A and C, the apical vertebral translation remained overall unchanged, a finding which is confirmed by other authors [7].
A hyperkyphotic thoracic spine has been found to be a contraindication for an anterior single rod instrumentation due to limited abilities to correct the sagittal plane deformity with this technique [1, 3, 30]. The dual rod system enables a correction of both hypo- and hyperkyphotic thoracic curves. In seven patients with a preoperative hyperkyphosis of on average 47.3° (41–62°) thoracic kyphosis was corrected to 41.0° (22–60°). In five of these cases normal thoracic kyphosis was restored (<40°). These data correspond to other authors reporting on satisfactory results with dual rod instrumentation in Scheuermann's kyphosis [8].
Anterior instrumentation enables a true segmental derotation of 42–48% [3, 19]. In this series the instrumented derotation averaged 41% resulting in a correction of the rib hump deformity of 67%. Radiologically, there was literally no spontaneous derotation of the lumbar spine, however, clinically the lumbar hump was reduced by 69%. The latter has been confirmed by three-dimensional surface analysis in a study on the rotational behaviour of secondary curves after selective anterior instrumentation and fusion [28]. In the anteriorly instrumented thoracic curves, a 14% derotation of the lumbar spine using digitized radiographs, a 49% derotation using threedimensional surface analysis and a 70% improvement of the lumbar hump using the scoliometer was found. One of the explanations might be a straightening of the lumbar spine due to the spontaneous frontal curve correction resulting in a decrease of the surface asymmetry and thus to a reduction of the lumbar hump [28]. The scores in the SRS-24 questionnaire are comparable with the data given by White et al. after posterior instrumentation and fusion in idiopathic scoliosis [31]. The reported scores for self-image after surgery, function after surgery and satisfaction with surgery were 3.3, 2.8 and 4.4, respectively, with an overall score of 4.0.
Conclusion
Anterior dual rod instrumentation in idiopathic thoracic scoliosis enables a true threedimensional curve correction with a fusion length comparable to the curve length. The advantages over single rod techniques include the reduced risk of intra- and postoperative screw pullout, a better control of thoracic kyphosis and a higher fusion rate. Due to the high stability of the system, there is no need for postoperative bracing. However, thoracic dual rod instrumentation is technically demanding and requires a double thoracotomy approach. A larger prospective series with a longer follow-up is neccesary to confirm these preliminary results.
References
- 1.Betz R, Harms J, Clements D, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999;24:225–239. doi: 10.1097/00007632-199902010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Betz RR, Lenke LG, Lowe TG et al (2000) Proximal screw pull-out during anterior instrumentatuion for thoracic scoliosis: preventive techniques. In: 35th Annual Meeting Scoliosis Research Society, Cairns, Australia, 18–21 October 2000
- 3.Bullmann V, Halm H, Lepsien U, et al. Selective ventral derotation spondylodesis in idiopathic thoracic scoliosis. Z Orthop. 2003;141:65–72. doi: 10.1055/s-2003-37307. [DOI] [PubMed] [Google Scholar]
- 4.Bullmann V, Halm H, Niemeyer Th, et al. Dual-rod correction and instrumentation of idiopathic scoliosis with the Halm–Zielke Instrumentation. Spine. 2003;28:1306–1313. doi: 10.1097/00007632-200306150-00016. [DOI] [PubMed] [Google Scholar]
- 5.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 6.Dwyer AF, Newton NC, Sherwood AA. An anterior approach to scoliosis: a preliminary report. Clin Orthop. 1969;62:192–202. [PubMed] [Google Scholar]
- 7.Edwards CC, Lenke LG, Peelle M, et al. Selective thoracic fusion for adolescent idiopathic scoliosis with C modifier lumbar curves: 2- to 16-year radiographic and clinical results. Spine. 2004;29:536–546. doi: 10.1097/01.BRS.0000109992.22248.77. [DOI] [PubMed] [Google Scholar]
- 8.Gaines RW, Moller H, Min K et al (2003) Short segment anterior apical instrumentation for Scheuermann's kyphosis. In: Poster presented at the 38th annual meeting of the Scoliosis Research Society, 10–13 September 2003, Quebec City
- 9.Giehl JP, Zielke K, Hack H-P. Zielke ventral derotation spondylodesis. Orthopäde. 1989;18:101–117. [PubMed] [Google Scholar]
- 10.Haher T, Gorup J, Shin T, et al. Results of the scoliosis research society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. Spine. 1999;24:1435–1440. doi: 10.1097/00007632-199907150-00008. [DOI] [PubMed] [Google Scholar]
- 11.Halm H, Liljenqvist U, Castro WHM, et al. Surgical treatment of idiopathic thoracolumbar scoliosis. Cotrel–Dubousset Instrumentation versus ventral derotation spondylodesis. Z Orthop. 1995;133:282–288. doi: 10.1055/s-2008-1039449. [DOI] [PubMed] [Google Scholar]
- 12.Halm H, Liljenqvist U, Niemeyer Th, et al. Halm–Zielke Instrumentation as improvement over Zielke-VDS. Z Orthop. 1997;135:403–411. doi: 10.1055/s-2008-1039408. [DOI] [PubMed] [Google Scholar]
- 13.Halm H, Liljenqvist U, Niemeyer Th, et al. Halm–Zielke-Instrumentation for primary stable anterior scoliosis surgery. Eur Spine J. 1998;7:429–434. doi: 10.1007/s005860050103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harms J, Jeszenszky D, Beele B (1997) Ventral correction of thoracic scoliosis. In Bridwell K, DeWald R (eds) The textbook of spinal surgery, vol 40. Lippincott-Raven, Philadelphia, pp 611–626
- 15.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg. 1962;44A:591–610. [PubMed] [Google Scholar]
- 16.Hopf C, Eysel P, Dubousset J. Operative treatment of scoliosis with Cotrel–Dubousset–Hopf Instrumentation. New anterior spinal device. Spine. 1997;22:618–627. doi: 10.1097/00007632-199703150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Kaneda K, Fujiya N, Satoh S. Results with Zielke instrumentation for idiopathic thoracolumbar and lumbar scoliosis. Clin Orthop. 1986;205:195–203. [PubMed] [Google Scholar]
- 18.Kaneda K, Shono Y, Satoh S, et al. New anterior instrumentation for management of thoracolumbar and lumbar scoliosis. Spine. 1996;21:1250–1262. doi: 10.1097/00007632-199605150-00021. [DOI] [PubMed] [Google Scholar]
- 19.Kaneda K, Shono Y, Satoh S, et al. Anterior correction of thoracic scoliosis with Kaneda anterior spinal system. Spine. 1997;22:1358–1368. doi: 10.1097/00007632-199706150-00015. [DOI] [PubMed] [Google Scholar]
- 20.Kuklo T, Lenke L, Won D, et al. Spontaneous proximal thoracic curve correction after isolated fusion of the main thoracic curve in adolescent idiopathic scoliosis. Spine. 2001;26:1966–1975. doi: 10.1097/00007632-200109150-00006. [DOI] [PubMed] [Google Scholar]
- 21.Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine. 2003;28:S36–S43. doi: 10.1097/00007632-200308011-00007. [DOI] [PubMed] [Google Scholar]
- 22.Lenke L, Betz R, Bridwell K, et al. Spontaneous lumbar curve coronal correction after selective anterior or posterior thoracic fusion in adolescent idiopathic scoliosis. Spine. 1999;24:1663–1671. doi: 10.1097/00007632-199908150-00007. [DOI] [PubMed] [Google Scholar]
- 23.Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of arthrodesis. J Bone Joint Surg. 2001;83A:1169–1181. [PubMed] [Google Scholar]
- 24.Lenke LG, Edwards CC, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine. 2003;28:S199–S207. doi: 10.1097/01.BRS.0000092216.16155.33. [DOI] [PubMed] [Google Scholar]
- 25.Liljenqvist U, Halm H. Augmentation of ventral derotation spondylodesis by double rod instrumentation. Z Orthop. 1998;136:50–56. doi: 10.1055/s-2008-1044651. [DOI] [PubMed] [Google Scholar]
- 26.Ogon M, Haid C, Krismer M, et al. Comparison between single-screw and triangulated, double-screw fixation in anterior spine surgery. A biomechanical test. Spine. 1996;21:2728–2734. doi: 10.1097/00007632-199612010-00005. [DOI] [PubMed] [Google Scholar]
- 27.Perdriolle R, Vidal J. Etude de la courbure scoliotique: importance de l’extension et de la rotation vertebral. Rev Chir Orthop. 1981;67:25–34. [PubMed] [Google Scholar]
- 28.Schulte TL, Hackenberg L, Bullmann V et al (2004) A prospective analysis of spontaneous changes of the vertebral rotation of secondary curves after selective anterior fusion of idiopathic scoliosis. In: Paper read at the 39th annual meeting of the Scoliosis Research Society, 6–9 September 2004 Buenos Aires, Argentina
- 29.Sucato DJ, Kassab F, Dempsey M. Analysis of screw placement relative to the aorta and spinal canal following anterior instrumentation for thoracic idiopathic scoliosis. Spine. 2004;29:554–559. doi: 10.1097/01.BRS.0000106495.91477.92. [DOI] [PubMed] [Google Scholar]
- 30.Sweet F, Lenke L, Bridwell K, et al. Prospective radiographic and clinical outcomes and complications of single rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine. 2001;26:1956–1965. doi: 10.1097/00007632-200109150-00005. [DOI] [PubMed] [Google Scholar]
- 31.White S, Asher M, Lai S, et al. Patients' perceptions of overall function, pain, and appearance after primary posterior instrumentation and fusion for idiopathic scoliosis. Spine. 1999;16:1693–1700. doi: 10.1097/00007632-199908150-00011. [DOI] [PubMed] [Google Scholar]
- 32.Wong H, Hee H, Yu Z, et al. Results of thoracoscopic instrumented fusion versus conventional posterior instrumented fusion in adolescent idiopathic scoliosis undergoing selective thoracic fusion. Spine. 2004;29:2031–2038. doi: 10.1097/01.brs.0000138304.77946.ea. [DOI] [PubMed] [Google Scholar]
- 33.Zielke K. Ventral derotation spondylodesis. Results of treatment of idiopathic lumbar scoliosis. Z Orthop. 1982;120:320–329. doi: 10.1055/s-2008-1051620. [DOI] [PubMed] [Google Scholar]