Abstract
This randomized controlled clinical trial compares the effectiveness of a biopsychosocial treatment with a solely conventional biomedical therapy in patients with subacute low back pain using parameters for pain intensity, functional status, depressive dysfunction and work performance. Sixty-four patients with a first-time sick leave between 3 and 12 weeks due to low back pain were randomly assigned to either a conventional biomedical therapy (MT; n=33) group, or a biopsychosocial therapy (BT; n=31) group including a psychotherapeutic module; both in accordance with a standardized 3 weeks inpatient treatment. Pain intensity, functional back capacity, clinical parameters and depressive dysfunction revealed significant improvement in both treatment groups at end of 3 weeks therapy (T1). However, at 6 months (T2), analysis revealed significant better results for nearly all parameters in the BT group that showed further improvement from T1 to T2, whereas the values in the MT group deteriorated from T1 back to the baseline values. During the 2-year period after therapy, 10% in MT and 59% in BT required no further sick leave due to low back pain. The results of the study indicate that a psychotherapeutic element in the treatment of low back pain appears to positively influence pain, functional status and work performance when conducted at an early stage of chronification and helps in the achievement of a better outcome.
Keywords: Low back pain, Psychotherapy, Functional status, Sick leave
Introduction
In Germany, 20% of all work-related ailments are attributed to low back pain, with an upward tendency; the total cost of low back pain to society is estimated to be approximately €20 billion per year, although only a small percentage of this amount is used for treatment [19, 20].
Acute back pain seems to respond well to simple treatment measures [1, 3, 6, 17, 31, 35], although there is a lot of variation in the benefit for individual patients. Clinical trials have shown that psychosocial factors have an important influence on the prognosis of low back pain. They display more predictive power in the course of the sickness than biomedical variables [37, 43]. To achieve a reduction in the recurrent symptoms and loss of time from work, these psychosocial risk factors should be taken into consideration in the planning of treatment particularly when the patient is on sick leave [7, 8, 25].
There is strong evidence that return to work becomes unlikely if the time off work exceeds 12 weeks; so clinical interventions should be performed within this time frame [42]. In the few studies conducted so far, there is only moderate evidence that multidisciplinary (biopsychosocial) treatments are superior to biomedical treatment in the improvement of pain, functional status and time to return to work and the long-term effects of psychologic interventions have been discussed controversially [13, 15, 16, 21, 23, 33, 39, 40, 42].
This study was designed to test the hypothesis that a multidisciplinary (biopsychosocial) treatment for patients with subacute low back pain and a first period of sick leave would have benefits in terms of pain, clinical function, depression and time of sick leave compared to a more traditional (biomedical) treatment.
Patients and methods
In 1998 and 1999, a questionnaire was mailed to general practitioners and orthopaedic surgeons in private practice asking for patients who continue to suffer from low back pain despite conventional treatment (medication, injections and chirotherapy by the orthopaedic surgeon, individual physiotherapy on prescription) and seeking intensified treatment in a hospital setting.
Inclusion criteria
Subacute low back pain (corresponding to the level of “temporary pain” according to von Korff [41]) with a first period of sick leave due to low back pain longer than 3 weeks up to a maximum of 12 weeks despite receiving outpatient treatment
Age 18–50 years
Knowledge of domestic language to complete the questionnaires
Exclusion criteria
Request or litigation for early retirement
History or presence of radicular pain in the lower extremity
Anamnestic, clinical and radiological signs as well as laboratory parameters causally connecting low back pain to a specific physical condition such as nucleus pulposus prolapse, tumor, spondylodiscitis, spondylolisthesis, spinal stenosis or cauda equine syndrome. Red flags according to the current guidelines of back pain including history and presence of inflammation, tumor, trauma and neurological deficits had to be ruled out by clinical, radiological or laboratory examination
Systemic diseases like rheumatoid arthritis, Crohn’s disease, diabetes mellitus, cancer or psychiatric disease
Cardiopulmonary or vascular contraindications for physiotherapy.
Patients passing inclusion and exclusion criteria were informed of the study and invited to participate. One physician made the diagnoses before randomization and supervised the treatment programs of both groups.
Randomization
The patients were randomized in blocks of five when entering this study which was based on an inpatient treatment at the authors’ clinic. The physician informed an independent person working elsewhere by phone, who allocated five subsequent patients to one of the two treatment arms by using a lottery system (a piece of paper marked MT or BT, present in equal number, was taken from a black box and returned afterwards to ensure equal binary probability). The patients were informed about their treatment allocation at initiation of therapy.
Further stratification (e.g. by the workplace) was not performed.
Concealment
The patient’s group affiliation was concealed from the physiotherapists who treated patients included in the study along with those from the rehabilitation department. Effective blinding of the physiotherapists was not confirmed. The supervising physician and the psychotherapist were not blinded to the patient’s group assignment. The patients too were aware of their assignment group but were treated in blocks at different times. The observer at 6-month follow-up (T2) was blinded to the assignment group. The observer acquiring sick leave status from health insurance companies at 2 years follow-up (T3) was also blinded.
Break off
Break off of the study was planned if any of the treatments would increase pain at completion.
Clinical interventions
The interventions were based on inpatient rehabilitation programs in both treatment arms with respect to dosage and contents. Each patient received approximately 6 h of daily treatment for 15 days in 3 weeks. The intensity of the treatment was comparable to the multidisciplinary restoration program performed by Bendix et al. [4].
In Germany, usually psychological treatment is not integrated in rehabilitation programs for patients suffering from disabling low back pain, and psychological methods are not part of the professional work of physiotherapists. All physiotherapists involved in this study had studied at a physiotherapy school and had extensive technical experience in the treatment of patients suffering from back pain, but were not trained and did not use cognitive behavioural therapy or any other psychotherapy.
Conventional biomedical therapy (MT group)
The conventional biomedical program included a functional restoration program of individual physiotherapy, group therapy in water, workout, back school and aimed at stretching, strengthening, improving mobility and body control. Passive interventions (massage and physical therapy) were added.
Biopsychosocial treatment (BT group)
In addition to biomedical treatment each patient of the BT group received specifically adapted psychotherapy three times per week and relaxation therapy four times per week. A professional psychotherapist performed this part of the treatment in a group and in an individual setting. Psychotherapy contained analysis of individual psychosocial factors and conflicts contributory to persistent low back pain, enhancement of patient’s understanding of the nature and function of their pain. Psychotherapy sessions also included psychoeducation, that means information given about the physiological relations of pain, stress and the muscular system, behavioural therapy, problem solving, stress relaxation and stress behaviour in specific situations of pain and stress experience. In cases of partner conflict, if the patients agreed, the partner was invited to participate in the therapy sessions as well. To ensure that the timeframes of the therapeutic interventions in both treatment groups were comparable, no group therapy in water was performed in the BT group.
Co-interventions such as medication, injections or chirotherapy were avoided in both groups during inpatient treatment. After completion of treatment programs, the patients were discharged without further interventions by the hospital; they were allowed to contact their general practitioner or orthopaedic surgeon who had referred them for therapy. Further utilization of medical services after completion of the therapy program was not recorded.
Measurements/outcome criteria
Clinical parameters were assessed and psychometric variables obtained by questionnaires at baseline (T0), after completion of the therapy programs at 3 weeks (T1) as well as after 6 months (T2). Sick leave data were recorded at T0 and for the first 2 years after therapy (T3). All measurements used in this study are reliable and valid instruments.
Numeric rating scale (NRS): perceived maximal pain intensity within the last 7 days on a scale ranging from 0 (no pain) to 10 (greatest pain) [10].
Mobility of the thoracic and lumbar spine in centimetres (modified Schober-test, finger-floor-test in forward bending, finger-thigh-test in lateral bending, measured in centimetres [11, 28]).
Torque (isokinetic tests by Cybex™6000 of the torque of flexor and abdominal muscles whilst in a standing position).
Functional capacity of the back (Hannover Functional Status Questionnaire—Back (FFbH-R) [18]). This validated score evaluates functional capacity or level of restriction in clinical function in different activities of daily living. The answers to these 12 questions (e.g. “can you sit on a chair for more than 1 h?”) are combined to give a total score in the form of a percentage of the functional capacity that would be expected in healthy controls (from 0% = no/minimal function to 100% = full function).
Depressive dysfunction (CES-D) [32]. This widely used and accepted, reliable and valid scale consists of 20 items evaluating as a sum score the extent of depression of the patients. With a score of more than 16 points (out of 45) the evaluated person is considered to be at risk for depression.
Sick leave due to low back pain (in days): the responsible health insurance companies were requested to provide sick leave data on the patients for the first 2 years after completion of the therapy (sick leave data is provided in Germany only on request not as a matter of course).
Statistical methods
Data were analysed with the statistical program SAS, Version 6.12. After data verification and validation, student’s t test was applied for univariate analysis testing differences among the groups as well as Chi2-test for differences in frequencies. Further analyses were performed using two-factorial analysis of variance (BT/MT) on the two groups, with contrasts for comparison at T0, T1, T2 and T3. All analyses were performed twice by statistically trained persons.
Pain intensity was the primary endpoint; secondary endpoints were all clinical and functional parameters, and sick leave within 2 years after completion of therapy. For the primary endpoint a confirmatory factor analysis was performed. Tests for significance were conducted mainly to determine interaction effects (group × time).
Assuming large outcome differences between the different time points and—due to literature dealing with biopsychosocial approaches in pain therapy [3, 12, 16]—between the two therapy groups, sample sizes were calculated according to Bortz and Döring [5]. For one-sided testing at a 0.05 significance α-level and with 0.80 power, a sample size of n=20 for each group was required at follow-up. Since 10% were expected to refuse randomization and 25% might be lost to follow-up, n=60 patients had to be included.
Ethics committee
The clinical trial was approved by the ethics committee of the local medical faculty.
Results
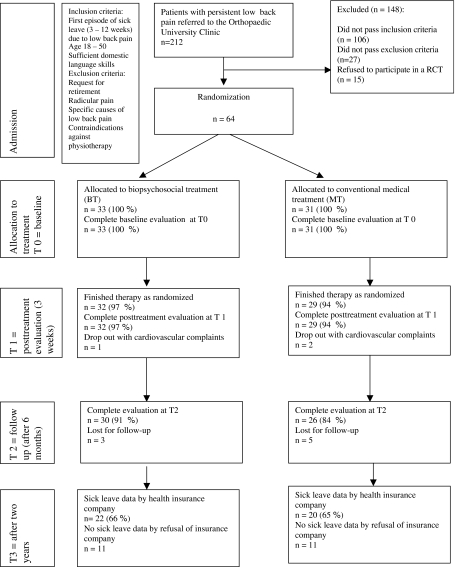
Two hundred and twelve patients had been referred to the outpatients department of the Orthopaedic University Clinic Heidelberg in 1998 and 1999. After fulfilling all criteria, each of the 64 patients was allocated one of the treatment arms (31 MT, 33 BT). Sixty-one patients (95%) completed therapy (29 MT, 32 BT); 56 patients (88%) presented for follow-up after 6 months (26 MT, 30 BT). Sick leave data at T3 were available for 42 patients (66%; 20 MT, 22 BT). The patient flow is portrayed on the patient flow diagram (Fig. 1). At baseline there was no significant difference between those who dropped out and those who were re-examined.
Fig. 1.
Patient flow diagram
At baseline T0, both groups were comparable, i.e. there were no significant differences between patients assigned to the MT or BT groups who were re-examined at T1, T2 and T3 with regard to age, gender, pain intensity, mobility, strength, functional capacity of the back, depressive dysfunction and time of history of low back pain (Table 1).
Table 1.
Baseline data of the patients of biomedical treatment (MT) and biopsychosocial treatment (BT) groups
| Sociodemographic data | MT (n=33) | BT (n=31) |
|---|---|---|
| Age (years; mean, range) | 36.7 (20–48) | 34.9 (19–50) |
| Gender: men (no., %) | 20 (61%) | 16 (52%) |
| Days of sick leave due to low back pain (mean, range) | 53.7 (27–80) | 58.2 (21–84) |
| Parameter | ||
| Maximum pain (last 7 days) on a numeric rating scale (NRS) 0 (no pain) to 10 (worst pain) | 5.28±2.20 | 6.00±1.81 |
| Functional back capacity (Hannover Functional Status Questionnaire—FFbH-R) 0–100% | 57.34±23.7 | 54.36±17.46 |
| Depression | ||
| Depression: general depression scale (CES-D) 0–45 | 9.87±8.51 | 12.40±8.53 |
| Spinal motion | ||
| S1 10+ (modified Schober’s sign in cm) | 14.04±3.64 | 12.02±4.19 |
| Finger-ground spacing (cm) | 18.24±17.04 | 17.17±18.40 |
| Finger-knee spacing left (cm) | 3.64±4.38 | 2.86±3.65 |
| Finger-knee spacing right (cm) | 3.50±4.31 | 3.14±4.16 |
| Strength | ||
| From neutral position to flexion direction Cybex®6000 TEF (Torque in nm) | 87.4±48.08 | 81.55±30.63 |
Thirty-nine of those 56 patients, who were followed up at T2 (31 male and 25 female with a mean age of 34.5±8.26 years), were employed fulltime, 8 part-time and 3 worked at home; 6 patients were unemployed, but on sick leave, at T0 and T2. All patients participating received financial compensations from their health insurance companies.
The changes of all parameters assessed and comparison of the two groups are listed in Table 2.
Table 2.
Results: changes between T0, T1 and T2 (“-”: deterioration)
| Outcome parameter | Group | Changes T1 versus T0 (during treatment) | Changes T2 versus T0 (follow-up) | Changes significance MT versus BT (T2 vs. T0) |
|---|---|---|---|---|
| Mean (±SD) | Mean (±SD) | P value | ||
| Pain (numeric rating scale, 0–10) | MT | 1.46±2.7 | −0.52±3.2 | 0.0001* |
| BT | 1.70±2.1 | 2.96±2.5 | ||
| Spinal motion | ||||
| S1 10+ (modified Schober’s sign in cm) | MT | 0.48±1.2 | 9.22±20.9 | 0.7703 |
| BT | 2.26±7.5 | 7.57±15.6 | ||
| Finger-ground spacing (cm) | MT | 1.61±11.5 | −0.11±16.7 | 0.5779 |
| BT | 1.76±5.3 | 2.68±13.4 | ||
| Finger-knee spacing left (cm) | MT | 0.87±3.3 | −13.39±22.1 | 0.2389 |
| BT | 0.50±2.7 | −6.2±17.8 | ||
| Finger-knee spacing right (cm) | MT | 0.70±3.3 | −12.43±22.3 | 0.2899 |
| BT | 1.00±3.4 | −6.0±17.6 | ||
| Strength | ||||
| From neutral position to flexion direction Cybex® 6000 TEF (torque in nm) | MT | 17.79±34.8 | −0.87±31.5 | 0.9285 |
| BT | 15.59±36.0 | 0.19±33.2 | ||
| Functional capacity | ||||
| Functional capacity (FFbH-R) 0–100 | MT | 6.41±14.9 | 1.19±31.4 | 0.0050* |
| BT | 10.00±17.0 | 25.75±22.4 | ||
| Depression | ||||
| Depression (CES-D) 0–45 | MT | 3.74±4.5 | −0.86±7.8 | 0.0034* |
| BT | 2.40±4.6 | 6.62±7.5 | ||
*Statistically significant
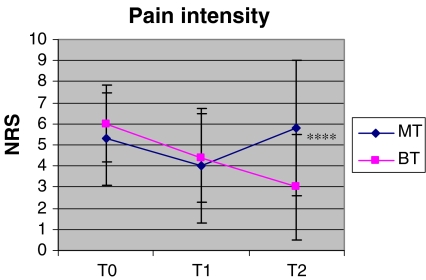
Primary endpoint: pain intensity
Pain intensity decreased significantly in both treatment groups at T1. In the longitudinal analysis, at T2 a further decrease in pain was observed in treatment group BT compared to T1, whereas the intensity of pain in treatment group MT at T2 was statistically not discernable from that at T0; the differences of changes between both treatment arms were significant (Fig. 2).
Fig. 2.
Changes in pain intensity on a numeric rating scale (NRS, scores ranged from 0 no pain to 10 maximum pain severity; at T2 significant difference of change between the treatment groups MT and BT: ****P<0.0001)
Secondary endpoints
Clinical parameters
In both treatment groups lumbar spinal flexion measured by modified Schober’s sign and all other mobility tests did not show significant changes at T1 in contrast to T0 as well as at T2 in contrast to T1.
During and after treatment, muscular strength of trunk flexor muscles did not change significantly either in group MT or in group BT.
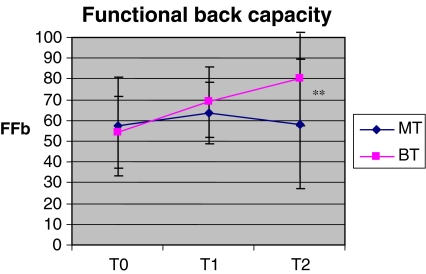
Functional parameters
The functional capacity of the back (scale FFbH-R) increased in both treatment groups from T0 to T1. At T2, further increase was only found in group BT. This difference of change at T2 and difference between the two treatment groups were significant (Fig. 3).
Fig. 3.
Changes in subjective functional capacity of the back (scale FFbH-R: scores in percentage of unrestricted capacity) at T2 significant difference of change to T0 between treatment groups MT and BT; **P=0.005)
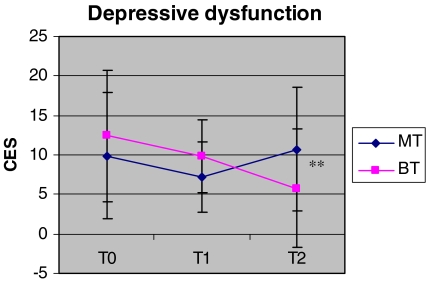
Depression
Depressive dysfunction (scale CES-D) decreased significantly in both treatment groups between T0 and T1, whereas the MT group returned to the same level at T2 as at T0. Further increase of the treatment group BT at T2 evoked significant differences between the groups at this time-point (Fig. 4).
Fig. 4.
Changes of depressive dysfunction (scale CES-D; at T2 significant difference of change to T0 between the treatment groups MT and BT; **P=0.0034)
Sick leave
Data from 42 patients revealed that during the first 2 years after therapy, 2 out of 20 in group MT (10 %) and 13 out of 22 in group BT (59 %) required no further sick leave due to lower back pain. Patients in group BT were significantly more capable to go to work (912 days of leave) compared to group MT (2,228 days of leave). Additionally, the number of sick leave periods in group BT (85 periods) was significantly less than in treatment group MT (228 periods) (Table 3).
Table 3.
Sick leave data for the first 2 years after therapy (n=42; MT=20; BT=22)
| Sick leave data | T3 during first 2 years after therapy | P MT versus BT | |
|---|---|---|---|
| MT | BT | ||
| Percentage of patients without sick leave following therapy | 10% | 59% | |
| Percentage of patients with sick leave more than 6 months following therapy | 35% | 18% | |
| Sick leave periods per patient | 11.4 | 3.86 | 0.004* |
| Sick leave days per patient | 111.40 | 41.45 | 0.001* |
*Statistically significant
Discussion
In this randomized trial, two high dose, multimodal treatments (one biomedical, the other biopsychosocial) for subacute low back pain with a first episode of sick leave were conducted. Changes were assessed in pain level, functional capacity and disability for both treatment groups. Both groups improved during 3 weeks inpatient therapy, but further improvement of all parameters after 6 months follow-up could only be found for the patients of the biopsychosocial treatment. During the first 2 years after therapy, significantly fewer sick leave days were accumulated by the biopsychosocial treatment group.
Although this clinical trial provides statistically and clinically significant evidence that patients suffering from subacute low back pain who do not resume work should be treated using a biopsychosocial approach, some questions remain open.
Potential limitations of the study
Nearly 90% of the patients could be followed in terms of clinical and functional parameters at 6 months after initial therapy. However, analysis of sick leave after 2 years with a loss of follow-up of 34% may be a relevant threat to validity. Unfortunately, some insurance companies provided data of sick leave of their patients in this study although they initially had agreed to participate. However, baseline data were comparable to those patients who were followed up and whose sick leave data were available. Moreover, a bias regarding outcome is very unlikely, because the missing data were from several insurance companies and there were no confounding effects with specific occupations or other individually linked associations. In order to assess the costs incurred by low-back-pain-induced sick leave above the expense of treatment, the cooperation with health insurance companies should be improved.
The patients, of course, were not blind to their group assignment. They and their physicians were informed of the intention to offer a biopsychosocial treatment approach. It can be assumed that patients not interested in psychological treatment might have resisted taking part in such a clinical trial, and patients interested in psychological treatment might have benefited particularly if treated this way or taken a disappointing course if assigned to the biomedical group. Furthermore, the patients may have informed the physiotherapists during therapy of the groups they were allocated to and might have earned additional therapeutical support as a member of the biopsychosocial group. However, the biomedical therapy improved in pain and other clinical parameters as well and there were no dropouts from therapy because of complaints. However, the treatment groups took divergent courses after completion of therapy. Since further treatment after the inpatient period was not monitored, the different developments of both groups concerning the clinical outcome may be caused by co-interventions in the follow-up period. However, both groups had the same opportunity to make use of further therapeutic support after initial therapy. Thus, the superiority of the results in the BT group can be explained either by (a) the better treatment effects in this group or by (b) the better post-treatment ability of the patients in the BT group to use more helpful post-treatment therapy.
Moreover, block randomization was performed in this study in order to decrease the extensive costs because the therapy groups were treated at different times which might have a threat to validity compared to a “true” randomization. However, there was no increased risk of contamination or bias between the groups due to the performed randomization procedure, because the different groups were strictly separated from each other. Furthermore, the corresponding clinical development of both groups during the inpatient treatment makes it unlikely that there was a bias of the treating physicians or therapists.
Physical exercise programs are considered effective and evidential in the treatment of chronic back pain, however, these are controversial with respect to their long-term effectiveness [44]. Taimela et al. [36] and Ljunggren et al. [23] emphasize the importance of further monitoring of (home) exercise. Assuring training compliance appears more important than measurable gains in mobility and strength [9, 21, 26, 27]. Comparing the two treatment groups, it appears reasonable that the psychotherapeutic model was responsible for the improved values of the group BT at 6 months follow-up after completion of therapy; a better training compliance might have been achieved, e.g. by a better understanding of pain, pain causes and pain-related behaviour.
The results of other studies have provided some evidence that integrated psychotherapy in a functional restoration program increases the effectiveness of treatment [16, 33, 42]. The randomized trial conducted by Moffett et al. [29] revealed the superiority of a combined exercise and behavioural treatment in primary care management, and concluded that rather than the intensity of pain, the ability to cope was improved. Lindström et al. [21, 22] and Loisel et al. [24] took a behavioural therapy approach in an occupational setting by teaching the patients that it is safe to move and found an earlier return to work than in the control group. Turner et al. [38, 39] in a randomized trial compared behavioural treatment, exercise and a combination of both in an outpatient and in a group setting for back patients mostly not in sick leave; whilst short-term effects were superior after the combination therapy, all significant differences disappeared after 6 months due to small sample sizes. Nicholas et al. [30] reported superior improvements for patients with chronic low back pain after a combined psychological and physiotherapeutical treatment over those treated by exercise and discussion sessions. Bendix et al. [3, 4] found similar results at follow-up, but approximately 30% of their patients were actually working when starting the restoration program. A systematic review by Guzman et al. [12] emphasized that a high dose, biopsychosocial therapy improves function and pain considerably compared to biomedical therapy; in terms of sick leave, their conclusions were contradictory. Other randomized studies, however, found no superiority of a multidisciplinary treatment program in psychological changes and sick leave days at 6 months follow-up [2] or 1 year [1] after therapy. Finally, the results of this randomized study suggest that improvements in pain and psychological parameters during therapy will continue only under the condition of integrated psychotherapy, which moreover can reduce the sick leave days in the further follow-up period. Physical parameters like spinal motion and muscle strength did not show any difference at the different time-points, and also did not correlate with pain or function, and therefore seem to be of little relevance in the outcome measurements of patients with low back pain.
Comparability of the quoted studies is limited by differences in the disability levels of the patients and intensity, contents and settings of the therapies applied. Although Bendix et al. [4] and Guzman et al. [12] recommend high-intensive programs (and the present study did so), knowledge remains limited on which dose of treatment should be applied and where it should be performed. Biopsychosocial therapy is a cost- and time-consuming treatment although fewer sick leaves will compensate for the therapy expenses. To the authors’ knowledge, there is no study in the literature demonstrating the quality or quantity of behavioural therapy that should be applied or shows a benefit in therapy outcome. Some studies demonstrate that also programs with less extensive psychotherapeutic involvement [13] or even simple advice [14] may have an adequate benefit for patients with low back pain and correlated sick leave. Moreover, a greater educational or researcher input may enhance the “psychotherapeutic” effect when evaluating therapy outcome of this and other studies. This is a threat to the generalizability of the results. However, this study is aimed primarily at the question of whether the midterm results of a biopsychosocial therapy are superior to conventional biomedical therapy.
The differences in treatment intensity and modality appear to be more dependent upon specific expectations and facilities driven by the different standards of national health systems than on rational measurements of how much therapy a patient deserves. Further, no knowledge was gained by the present study as to which biomedical models, which technique of psychotherapy should be applied and which health care provider should perform it (physiotherapist with skills in behavioural treatment or psychotherapy specialist). The usage of the term “psychotherapy” ranges, in the quoted studies, from giving advice that activity does not harm to specialized and high dose individual psychotherapy such as that in the present study. Therefore, we assume that patients’ pre-study experiences are decisive in the choice of which dose of psychotherapy should be applied in a randomized study to achieve optimum results.
The probability of the resumption of work will be low if the work place is unsatisfactory and benefit of sick leave high. If unemployment is high and benefit of sick leave is better than unemployment benefit, no therapy will cure low back pain with sick leave. There is no doubt that therapy should be initiated before sick leave has resulted in unemployment. This might be the reason why a high dose therapy performed early in the first sick leave period resulted in less sick leave days during the following 2 years. Treatment costs of low back pain in Germany are small compared to the secondary social costs caused by sick leave litigation, unemployment benefits and early retirement; calculations of treatment costs remain secondary as long as treatment effects an improvement in the likelihood of return to work [34].
This study supports the moderate evidence that a biopsychosocial rehabilitation program is superior in the treatment of low back pain if performed in a still subacute state; however, further high quality studies remain a necessity as concluded by Karjalainen et al. [16] in their systematic review. It should be noted that sick leave data has been found to be extremely useful in order to prove the efficacy of a biopsychosocial approach as a cost effective and beneficial treatment for lower back pain.
Conclusions
This randomized controlled clinical trial indicates that a biopsychosocial treatment option in patients with subacute low back pain and a first episode of sick leave appears to positively influence pain, functional status and work performance after completion of therapy compared to a treatment with conventional biomedical therapy. The results of this study show that a psychotherapeutic element in the treatment of low back pain is beneficial when conducted at an early stage of chronification and helps in the achievement of a better prognosis.
References
- 1.Alaranta H, Rytokoski U, Rissanen A, et al. Intensive physical and psychosocial training program for patients with chronic low back pain. A controlled clinical trial. Spine. 1994;19:1339–1349. doi: 10.1097/00007632-199406000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Altmaier EM, Lehmann TR, Russell DW, Weinstein JN, Feng Kao C. The effectiveness of psychological interventions for the rehabilitation of low back pain: a randomized controlled trial evaluation. Pain. 1992;49:329–35. doi: 10.1016/0304-3959(92)90240-C. [DOI] [PubMed] [Google Scholar]
- 3.Bendix Af, Bendix T, Labriola M. Functional restoration for chronic low back pain: two-year follow-up of two randomized trials. Spine. 1998;23:717–725. doi: 10.1097/00007632-199803150-00013. [DOI] [PubMed] [Google Scholar]
- 4.Bendix AF, Bendix T, Lund C, et al. Comparison of three intensive programs for chronic low back pain patients: a prospective, randomized, observer-blinded study with one year follow-up. Scand J Rehab Med. 1997;29:81–89. [PubMed] [Google Scholar]
- 5.Bortz J, Döring N. Forschungsmethoden und Evaluation. Berlin Heidelberg New York: Springer; 2002. [Google Scholar]
- 6.Burton AK, Waddell G, et al. Information and advice to patients with back pain can have a positive effect. Spine. 1999;24:2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 7.Burton AK. Back injury and work loss. Spine. 1997;22:2575–2580. doi: 10.1097/00007632-199711010-00021. [DOI] [PubMed] [Google Scholar]
- 8.Cherkin DC. Primary care research on low back pain. The state of the science. Spine. 1998;23:1997–2002. doi: 10.1097/00007632-199809150-00017. [DOI] [PubMed] [Google Scholar]
- 9.Clauw DJ, Williams D, Lauerman W, et al. Pain sensitivity as a correlate of clinical status in individuals with chronic low back pain. Spine. 1999;24:2035–2041. doi: 10.1097/00007632-199910010-00013. [DOI] [PubMed] [Google Scholar]
- 10.Downie WW, Leatham PA, Rhind VM. Studies with pain rating scales. Ann Rheum Dis. 1978;37:378–381. doi: 10.1136/ard.37.4.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frost M, Stuckey S, Smalley LA, et al. Reliability of measuring trunk motions in centimeters. Phys Ther. 1982;62:1431–1437. doi: 10.1093/ptj/62.10.1431. [DOI] [PubMed] [Google Scholar]
- 12.Guzman J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: systematic review. B Med J. 2001;322:1511–1516. doi: 10.1136/bmj.322.7301.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haldorsen EM, Grasdal AL, Skouen JS, Risa AE, Kronholm K, Ursin H. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long-term sick-listed employees with musculoskeletal pain. Pain. 2002;95:49–63. doi: 10.1016/S0304-3959(01)00374-8. [DOI] [PubMed] [Google Scholar]
- 14.Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine. 1995;20:473–477. doi: 10.1097/00007632-199502001-00011. [DOI] [PubMed] [Google Scholar]
- 15.Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, Roquelaure Y, Penneau-Fontbonne D, Richard I. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine. 2004;29:487–493. doi: 10.1097/01.BRS.0000102320.35490.43. [DOI] [PubMed] [Google Scholar]
- 16.Karjalainen K, Malmivaara A, Tulder M, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain in working-age adults. Spine. 2001;26:262–269. doi: 10.1097/00007632-200102010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Koes BW, Bouter LM, Mameren H. The effectiveness of manual therapy, physiotherapy, and treatment by the general practitioner for nonspecific back and neck complaints: a randomized clinical trial. Spine. 1992;17:28–35. doi: 10.1097/00007632-199201000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Kohlmann T, Raspe HH. Der Funktionsfragebogen Hannover zur alltagsnahen Diagnostik der Funktionsbeeinträchtigung durch Rückenschmerzen (FFbH-R) Rehabilitation. 1996;35:1–8. [PubMed] [Google Scholar]
- 19.Kössler F. Arbeitsbedingte Muskel-Skelett-Erkrankungen (MSE)—eine interdisziplinäre Herausforderung. ErgoMed. 1998;5:220–236. [Google Scholar]
- 20.Lenhardt U, Elkeles T, Rosenbrock R. Rückenschmerzen—Befunde epidemiologischer Forschung. Z Allg Med. 1994;70:561–565. [Google Scholar]
- 21.Lindström I, Ohlund C, Eek C, et al. Mobility, strength, and fitness after a graded activity program for patients with subacute low back pain. A randomized prospective clinical study with a behavioral therapy approach. Spine. 1992;17:641–652. doi: 10.1097/00007632-199206000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Lindström I, Ohlund C, Eek C, et al. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with a operant-conditioning behavioral approach. Phys Ther. 1992;72:279–290. doi: 10.1093/ptj/72.4.279. [DOI] [PubMed] [Google Scholar]
- 23.Ljunggren AE, Weber H, Kogstad O, et al. Effect of exercise on sick leave due to low back pain. Spine. 1997;22:1610–1617. doi: 10.1097/00007632-199707150-00017. [DOI] [PubMed] [Google Scholar]
- 24.Loisel P, Abenhaim L, Durand P, et al. A population-based, randomized clinical trial on back pain management. Spine. 1997;22:2911–2918. doi: 10.1097/00007632-199712150-00014. [DOI] [PubMed] [Google Scholar]
- 25.Main CJ, Waddell G. Behavioral responses of examination. Spine. 1998;23:2367–2371. doi: 10.1097/00007632-199811010-00025. [DOI] [PubMed] [Google Scholar]
- 26.Mannion AF, Müntener M, Taimela S, et al. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24:2435–2448. doi: 10.1097/00007632-199912010-00004. [DOI] [PubMed] [Google Scholar]
- 27.Martin PR, Rose MJ, Nichols PJR, et al. Physiotherapy exercises for low back pain: process and clinical outcome. Int Rehabil Med. 1980;8:34–38. doi: 10.3109/03790798609166509. [DOI] [PubMed] [Google Scholar]
- 28.Mellin G. Physical therapy for chronic low back pain: correlation between spinal mobility and treatment outcome. Scand J Rehab Med. 1985;17:163–166. [PubMed] [Google Scholar]
- 29.Moffett J, Torgerson D, Bell-Syer S, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. Br Med J. 1999;319:279–283. doi: 10.1136/bmj.319.7205.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nickolas MK, Wilson PH, Goyen J. Comparison of cognitive behavioral group treatment and an alternative nonpsychological treatment for chronic low back pain. Pain. 1992;48:339–347. doi: 10.1016/0304-3959(92)90082-M. [DOI] [PubMed] [Google Scholar]
- 31.Patijn J, Durinck JR. Effects of manual medicine on absenteeism. J Man Med. 1991;6:49–53. [Google Scholar]
- 32.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;3:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 33.Schonstein E, Kenny D, Keating J, Koes B, Herbert RD. Physical conditioning programs for workers with back and neck pain; a cochrane systematic review. Spine. 2003;28:E391–E395. doi: 10.1097/01.BRS.0000092482.76386.97. [DOI] [PubMed] [Google Scholar]
- 34.Schwartz FW, Bitzer EM, Döring H et al (1999) Gesundheitsausgaben für chronische Krankheit in Deutschland. Lengerich, Berlin, Düsseldorf, Leipzig, Riga, Scottsdale, Wien, Zagreb: Papst
- 35.Szpalski M, Hayez JP. Objective functional assessment of the efficacy of tenoxicam in the treatment of acute back pain. A double-blind placebo-controlled study. Br J Rheumatol. 1994;33:74–78. doi: 10.1093/rheumatology/33.1.74. [DOI] [PubMed] [Google Scholar]
- 36.Taimela S, Takala EP, Asklöf T, et al. Active treatment of chronic neck pain. Spine. 2000;25:1021–1027. doi: 10.1097/00007632-200004150-00018. [DOI] [PubMed] [Google Scholar]
- 37.Thomas E, Silman AJ, Croft PR, et al. Predicting who develops chronic low back pain in primary care. A prospective study. Brit Med J. 1999;318:1662–1667. doi: 10.1136/bmj.318.7199.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turner JA, Clancy SC, Mc Quade KJ, et al. Effectiveness of behavioral therapy for chronic low back pain: a component analysis. J Consult Clin Psychol. 1990;58:573–579. doi: 10.1037/0022-006X.58.5.573. [DOI] [PubMed] [Google Scholar]
- 39.Turner JA, Jensen MP. Efficacy of cognitive therapy for chronic low back pain. Pain. 1993;52:169–177. doi: 10.1016/0304-3959(93)90128-C. [DOI] [PubMed] [Google Scholar]
- 40.Tulder MW, Koes BW. Low back pain and sciatica: chronic. Clin Evid. 2002;8:1171–87. [PubMed] [Google Scholar]
- 41.Korff M. Studying the natural history of back pain. Spine. 1994;19:2041S–2046S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- 42.Waddell G, Burton AK. Occupational health guidelines for the management of low back pain at work: evidence review. Occup Med. 2001;51:124–135. doi: 10.1093/occmed/51.2.124. [DOI] [PubMed] [Google Scholar]
- 43.Waddell G, McCulloch JA, Kummel E, et al. Nonorganic physical signs in low-back pain. Spine. 1980;5:117–125. doi: 10.1097/00007632-198003000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Waddell G. A new clinical model for the treatment of low-back pain. Spine. 1987;12:632–644. doi: 10.1097/00007632-198709000-00002. [DOI] [PubMed] [Google Scholar]