Abstract
Sophisticated and newer imaging capabilities have resulted in increased reporting and treatment options of spinal lumbar synovial cysts (LSS). Most of the patients with lumbar cysts tend to be in their sixth decade of life with a slight female predominance. The incidence of LSS is thought to be less than 0.5% of the general symptomatic population. They may be asymptomatic and found incidentally or the epidural growth of cysts into the spinal canal can cause compression of neural structures and hence associated clinical symptoms. Most of the symptomatic LSS patients present with radicular pain and neurological deficits. Spinal synovial cysts are commonly found at L4-5 level, the site of maximum mobility. They may be unilateral or bilateral and at one or multilevel. MRI is considered the tool of choice for its diagnosis. The etiology of LSS is still unclear, but underlying spinal instability, facet joint arthropathy and degenerative spondylolisthesis has a strong association for worsening symptoms and formation of spinal cysts. Synovial cysts resistant to conservative therapy should be treated surgically. Resection and decompression with or without fusion and instrumentation remains an appropriate option. Synovial cysts may recur following surgery. The optimal approach for patients with juxtafacet LSS remains unclear. The best surgical treatment option for each particular individual should be tailored depending upon the symptoms, radiological findings and other co morbidities.
Keywords: Lumbar synovial cysts, Spondylolisthesis, Conservative treatment, Surgical treatment, Resection and decompression, Spinal fusion
Introduction
In 1885, Baker first described the formation of synovial cysts adjacent joints to a joint [3, 4]. Synovial cyst occur throughout the body, in the spine they may occur anywhere in cervical [23, 25, 37], thoracic [2, 13] and in the lumbar spine [1, 7, 12, 13, 18, 21, 22, 33, 35, 36, 38, 39, 56]. It was in 1950 that it was first described to cause symptoms of spinal nerve compression; Kao et al. later confirmed this in 1968 [27, 28, 55].
In the last decade, improved imaging capabilities such as computed tomography (CT) and magnetic resonance imaging (MRI) have resulted in increase reporting, diagnostic yield and treatment options of spinal synovial cysts. The exact etiology of spinal synovial cyst is still unclear. To date debate continues regarding its origin, cause, pathology and the best treatment.
Incidence, age and sex
Eyster et al. reviewed approx. 1,800 MRIs and CTs over one and half year and found 11 (0.6% of) cases of lumbar synovial cysts of the spine [16]. However Doyle et al. [14] found a prevalence of 2.3% anterior and 7.3% posterior spinal cyst in a review of 303 retrospective analyses of MRIs. Similarly Lemish et al. [33] identified 10 cysts in 2,000 reviews of CT lumbar spines. Synovial cysts in the spine occur predominantly in the lumbar as compared to thoracic and cervical areas [19].
Most of the patients with lumbar cysts tend to be in their sixth decade of life with a range that is varied from as early as 28 years to as late as 94 years [34]. A female bias has been reported often [34], but others refute that [16]. A female to male ratio of 1:1 [34] to 2:1 [22, 39, 54] and 3:1 and 4:1 has been reported [21, 41].
Presenting signs and symptoms
They may be asymptomatic and found incidentally [20, 56]. The epidural growth of cysts into the spinal canal causes compression of neural structures and their associated clinical symptoms. The clinical presentation of a cyst depends on it volume, site and its relationship to the surrounding bony and neural structures.
Most of the symptomatic patients present with radicular pain and neurological deficits. A history of low-back pain invariably precedes the radicular pain (range from 50 to 93%) [21, 54]. Most commonly occurring symptom of synovial cysts of the spine is painful radiculopathy, which may be unilateral or bilateral, reported in 57–100% of cases [21, 54].
Neurogenic claudication is the next most frequently reported symptom ranging from 10 to 44% [34, 41]. This is followed by neurological deficits which includes sensory deficits (range 10–43%), motor deficits (range 20–27%) and reflex abnormalities (up to 57%) [22, 34, 44, 54]. Other sign and symptoms including cauda equina syndrome (range 1–13%) [7, 21, 22, 32, 34, 43, 56]. lateral recess [15] and spinal stenosis syndromes [18, 32] have also been reported.
Diagnostic imaging
Plain radiographs have little diagnostic importance in identifying synovial cyst but are useful in excluding other conditions, such as spondylosis, degenerative spondylisthesis and metastatic lesions.
Computed tomography scanning and MRI are the two neuro-diagnostic imaging modalities recommended for characterization of synovial cysts and preoperative planning. MRI will demonstrate not only the nature of the cystic lesion, but also its relationship to the thecal sac. On MR imaging, synovial cysts appear as well circumscribed, smooth, extra-dural in location and adjacent to facet joints. The proteinaceous content of the cyst can demonstrate greater signal intensity than the surrounding CSF on both T1and T2 weighted images [24, 30, 38].
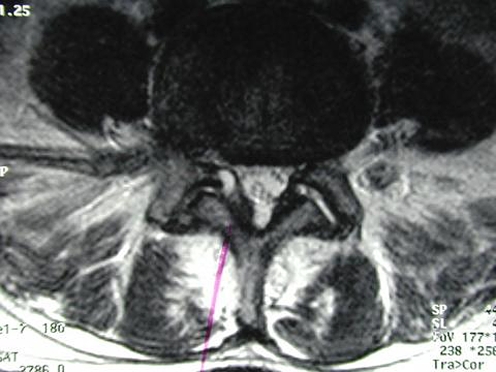
The typical appearance of a cyst on a CT scan can be altered by its content e.g., gas [18, 45, 49], calcification [37], blood [23], inflammation and the osseous structure involvement. Calcification within cyst wall appears low signal intensity on both T1 and T2 weighted images whereas hemorrhagic cysts display increase intensity compared to CSF probably due to T1 shortening caused by methemoglobin. MR imaging is considered to be diagnostic imaging of choice in the workup of suspected synovial cysts [20, 24]. (See Figs. 1 and 2, for sagittal and cross section of MRI, respectively).
Fig. 1.
Cross sectional MRI with the synovial cyst of the spine
Fig. 2.
Sagittal MRI with the synovial cyst of the spine
Level of cysts
The majority of synovial cysts in the lumbar spine occur at the L4–L5 level, the site of maximum mobility. The predilection for cysts to occur adjacent to this facet joint level has been attributed to the amount of degenerative spondylosis and spinal instability [2, 7–11, 17, 21, 22, 25, 26, 29, 31, 40, 46–49, 53, 56]. The range of this finding varies from 51% found by Banning et al. to 80% in the series by Trummer et al. [6, 54].
L5–S1 is considered to be the next most frequent site of developing lumbar cysts; this is followed by L3–4 and then L2–3. Synovial cysts are found equally on both sides of the spine and can be found at two or more levels in one patient [21, 34, 41, 54].
Development and associations
Development of lumbar cysts has been linked with degenerative spondylosis, spinal instability and trauma. Banning et al. [6] noted 90% of his patients with facet arthropathy. Hsu et al. [22] recorded 75% of his patient with degenerative arthropathy on radiological imaging. Trummer et al. [54] noticed a hypermobile facet joint in 60% of his patients. Pirotte recorded 54% of his patients with spondylosis [41].
Perhaps the most interesting finding is its association with spondylolisthesis. Rheust et al. [42] described 38% of patients having an association of it with synovial cysts, gave one of the earliest descriptions of spondylolisthesis in 1980s. The association of spondylolisthesis with cysts varies in other studies; Parlier et al. [39] noted 60% of his patients with spondylolisthesis. Both Lyon et al. [34] and Salmon et al. [45] found 50% of their patients with degenerative spondylolisthesis. Similarly Trummmer et al. found 33% and banning 41% [6,34]. Sabo et al. [44] found 15 of his 56 patients with spondylolisthesis and strongly advocated the use of routine dynamic flexion and extension films for its accurate diagnosis.
Lyon et al. [34] also reported 11% and Howington et al. [21] 18% of their patients with prior surgery and subsequent development of spinal synovial cyst; others have failed to record this observation.
Pathology
Cysts are internally lined with cuboid or pseudostratified columnar epithelium and filled with clear or straw colur fluid [22, 30, 44, 51]. The distinction between synovial cysts (with a synovial lining) and ganglion cysts (with out a lining) is a histological one. As other authors have discussed, there is no clinical relevance to differentiating between ganglion and synovial cysts, as their presentations, treatments and prognoses are identical [21, 38, 44]. Others explain synovial and ganglion cysts to be a specific point in a cycle of cyst formation and degeneration [21, 22].
These cysts can on rare occasion hemorrhage and bleed into surrounding soft tissues and or spinal canal causing acute compression of the spinal cord [5, 26, 34, 48, 52]. The incidence of hemorrhagic cyst varies: Lyon et al. [34] reported 18 of his 194 patients to none reported by others.
Conservative management
Conservative treatment modalities include no treatment, bed rest, oral analgesics, physical therapy, orthopedic corsets, chiropractic care, CT-guided needle aspiration and intra-articular injection of corticosteroid drugs and cyst punctures [1, 8–10, 33, 34].
Direct cyst puncture by means of a translaminar CT has been tried but most cyst recur after 6–12 months. Most believe that residual synovium, cyst type and osmotic load of the contrast are contributing factors to poor results [1, 31].
First report of facet joint steroid injection in a symptomatic cyst was reported by Casselman [10] in 1985. Since then steroid and local anesthetics or a combination of both have been injected intra-articularly for therapeutic relief of symptoms with the aid of imaging techniques and with variable results [8–10, 15, 22, 39, 50].
Hsu et al. [22] treated 4 of his 11 cases with epidural steroid injection with short-term relief of symptoms in 3, and 2 of 3 patients had short-term relief with intra-articular injections. Follow-up data was available for 5 months only.
Slipman et al. [50] treated 14 patients with transforaminal epidural steroid injection and physical therapy. Eight of the patients failed non-surgical treatment.
Sauvage et al. [51] treated 13 patients with intra-articular steroid injections. Failure rate were 31 and 58% at 1 and 6 months, respectively. Similarly Parlier et al. [39] treated 28 patients with at least one intra-articular steroid injection. A failure rate of 33 and 64% was reported at 1 and 6 months, respectively.
Few series have found that steroid injections provide acceptable long-term results [1, 8, 39]. However, these treatments often show short-term or no improvement at all [22]. Causes of failures include rarity of cyst involution, inadequate aspiration of fluid, inability to install steroids properly and inability to puncture and cyst recurrence. Aspiration of the cyst fluid is often difficult and increased failure is also attributed to the ball-valve effect as negative pressure is applied [30, 32]. We suggest a conservative trial of all the above modalities for a period of 6 months after which surgical options should be considered [29, 34, 44].
Surgical evaluation and outcome
Surgical treatment is largely recommended in all cases of intractable pain or neurological deficit. The surgical technique will depend on the site, size and associated other factors of the cysts, e.g., duration of symptoms and involvement of surrounding structures etc. in general current therapy for synovial cysts includes excision of the mass (total or partial) and lumbar decompression [34, 36, 44, 53, 56].
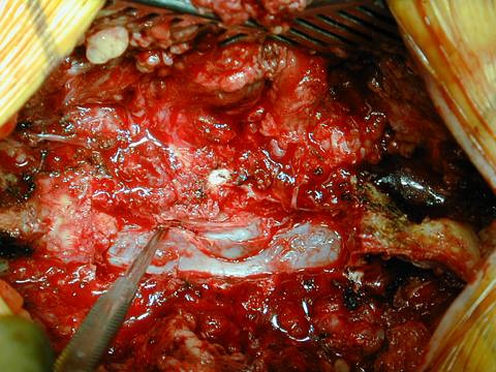
Removal of unilateral cyst in a stenotic spinal canal may involve a partial above or below the level and full (or partial) laminectomy at the level of lesion. The nerve root and thecal dural sac are differentiated from the synovial cyst and its thick viscous fluid to avoid injury to cause cerebrospinal fluid leak and fistula.
Additional spinal fusion procedures (with or without instrumentation) are performed if the spine is deemed unstable/listhesis or significant spondylosis is noted. Onforio et al. [38] reported 8 of 12 patients while Kurtz et al. [32] reported three of four with spondylolisthesis, none underwent spinal fusion. Of the 15 patients with spondylolisthesis in the series by Sabo et al. [44] series, six had spinal fusion. No difference in outcome was found in patients having fusion from those who did not. Forty-six patients had excellent outcomes while 12 had occasional pain and 1 had a poor outcome [44].
Approximately half of patients had grade 1 spondylolisthesis in the series reported by Lyons et al. only 18 patients with spinal instability had fusion. Ninty-one percent of patients had good pain relief with 82% of patients had motor relief. Forty-seven patients were lost in the follow-up [34]. Howington et al. [21] reported a similar finding, one patient deemed to have spinal instability underwent spinal fusion, no separate outcome of spinal fusion results were mentioned in either of the above series. Khan et al. [29] noted a better outcome with patients undergoing fusion surgery for their group of patients with spondylolisthesis and synovial spinal cysts than those without fusion.
Pirotte et al. reported 100% postoperative relief immediately after surgery. Five patients developed symptoms of sciatica within the first year. No spondylolisthesis or fusion was reported in his series. Others have mentioned an association between spinal cysts and spondylolisthesis/instability and better surgical outcomes without any mention of the results of its different type of procedures. However as there are no randomized clinical control trials to prove or disapprove optimum treatment for patients with cysts and spondylolisthesis, it is our view that the treatment of cysts in these situations should be tailored according to individual situation with aim to remove symptomatic cysts and aim to achieve optimum stabilization of the spine. Results of other surgical and non-surgical outcomes are summarized in Table 1. (See Figs. 3 and 4, showing intraoperative dissection of lumbar synovial cyst, of the spine and a dissected synovial cyst respectively).
Table 1.
Showing different studies of synovial cyst of the spine with their outcomes
| Study | No. of pts | Gender | Side of cyst | Primary procedure | Primary fusions | Follow-up duration | Delayed fusion | Outcomes | Other |
|---|---|---|---|---|---|---|---|---|---|
| Lyon et al. | 194 | 94F 100M | Rt=Lt | Lam/res | 18 | 6 m min | 4 | 134(91%) good, 82% motor relief | 47 lost f/u |
| Howington et al. | 28 | 21F 7M | 15Rt 13Lt | Lam/res | 1 | 40 m avg | 1 | 88% and 21% relief of rad. & back pain resp. | |
| Pirotte et al. | 46 | 38F 8M | / | Lam/res | / | 12 m min. | / | 100% imm. Postop pain relief | 5 rec. cysts |
| Trummer et al. | 19 | 7F 12M | 6Rt 12Lt | Lam/res | / | 3 m min. | / | 17 pts exc. 2 good | 1 rec. cyst |
| Sabo et al. | 56 | 32F 24M | 30Rt 25Lt | Lam/res | 7 | 12 m avg | 2 | 46 pts exc. 12 occ. Pain 1 poor | 4 rec. cysts |
| Banning et al. | 31 | 19F 11M | 22Rt 11Lt | Lam/res | 2 | 24 m avg | / | 20 exc/good, 11 fair | 3 rec. cysts |
| Hsu et al. | 19 | 13F 6M | 8 bilobed | Lam/res | / | 14 pts 1.5 years | / | 3 exc. 4 good | 6 cons.3/4 epi. steroid inj |
| Salmon et al. | 28 | 22F 6M | 1 bilateral | Lam/res | range 3–10 years | / | 26 exc/good, 2 fair/poor | ||
| Parlier et al. | 30 | 21F 9M | / | Epi. steroid inj | / | 12 m min | / | 50% exc/good, 18 fair/poor | 2 lost f/u |
| Bureau et al. | 12 | 8F 4M | / | Epi. steroid inj | / | 23 m avg | / | 74% exc, 1 fair, 2 poor | 6 cyst regress |
| Khan et al. | 39 | 11F 28M | 20Rt 22 Lf | Lam/res | 26 | 26 m | 4 | Fusion= 80% exc/good, 8%poor | Nonfusion=699%exc/good, 15%poor |
Pts Patients, Rt right, Lt left, Lam/res Laminectomy and resection, Epi epidural, Inj injection, m months, f/u followup, rad radicular, Exc excellent, Imm immediate, postop postoperative, rec recurrent
Fig. 3.
Intraoperative dissection of lumbar synovial cyst of the spine
Fig. 4.
A dissected lumbar synovial cyst of the spine
One of the detail records of postoperative complication comes from Lyon et al. [34]. His series noted (three patients with) cerebrospinal fluid fistula, (one patient each with) discitis, epidural hematoma, seroma, deep vein thrombosis and death. Banning et al. [6] recorded three of his patients (9%) while Salmon et al. 45 reported five patients with postoperative cerebrospinal fluid leaks. Trummer et al. [54] noted no postoperative complications in his series of patients.
Pirotte et al. noted five of his 46 patients had developed recurrent cysts within the first year of follow-up. Trummer et al. noted one recurrent cyst. Similarly Banning et al. [6] found 3% and Sabo et al. [44] noticed 4 of his patients with recurrent cysts. Khan et al. [29] found only one recurrent cyst in their follow-up of patients. We conclude that removal of synovial cysts with subsequent adequate fixation (with or without instrumentation) should be strongly considered to prevent recurrent symptoms and cysts at the site of removal especially if the spine is deemed unstable.
Conclusion
Improved imaging capabilities have resulted in increase reporting, diagnostic yield and treatment options of spinal synovial cysts. A majority of patients with lumbar cysts tend to be in their sixth decade of life. There is a slight female predominance. A variable incidence has been described in the literature; it is thought that it may be less than 0.5% of the general symptomatic population. They may be asymptomatic and found incidentally. The epidural growth of cysts into the spinal canal causes compression of neural structures and their associated clinical symptoms. Most of the symptomatic patients present with radicular pain and neurological deficits.
Spinal cysts are commonly found at L4–5 level, the site of maximum instability. They may be unilateral or bilateral and at one or multilevel. MRI is the tool of choice for diagnosis. The etiology is still unclear but underlying spinal instability, facet joint arthropathy and degenerative spondylolisthesis has a strong association for worsening symptoms and formation of spinal cysts.
Synovial cysts resistant to conservative therapy should be treated surgically. Resection and decompression with or without fusion and instrumentation remains an appropriate option. Synovial cysts may reoccur following surgery. It appears that the optimal approach for patients with juxtafacet cysts remains unclear. The best surgical treatment approach for each particular individual should be tailored depending upon the symptoms, radiological findings and other co morbidities.
References
- 1.Abrahams JJ, et al. CT-guided needle aspiration biopsy of an intraspinal synovial cyst (ganglion): case report and review of the literature. AJNR Am J Neuroradiol. 1988;9.2:398–400. [PMC free article] [PubMed] [Google Scholar]
- 2.Awward EE, et al. Synovial cyst of the midthoracic spine. AJNR Am J Neuroradiol. 1991;12.3:562–563. [PMC free article] [PubMed] [Google Scholar]
- 3.Baker WM. Formation of synovial cysts in connection with joints. St. Bartholomews Hospital Reports. 1885;21:177–190. [Google Scholar]
- 4.Baker WM. On the formation of synovial cysts in the leg in connection with disease of the knee-joint 1877. Clin Orthop. 1994;299:2–10. [PubMed] [Google Scholar]
- 5.Bandiera S, et al. Hemorrhagic synovial lumbar cyst: a case report and review of the literature. Chir Organi Mov. 1999;84.2:197–203. [PubMed] [Google Scholar]
- 6.Banning CS, Thorell WE, Leibrock LG. Patient outcome after resection of lumbar juxtafacet cysts. Spine. 2001;26(8):969–972. doi: 10.1097/00007632-200104150-00024. [DOI] [PubMed] [Google Scholar]
- 7.Baum JA, Hanley EN., Jr Intraspinal synovial cyst simulating spinal stenosis. A case report. Spine. 1986;11.5:487–489. doi: 10.1097/00007632-198606000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Bjorkengren AG, et al. Symptomatic intraspinal synovial cysts: opacification and treatment by percutaneous injection. AJR Am J Roentgenol. 1987;149.1:105–107. doi: 10.2214/ajr.149.1.105. [DOI] [PubMed] [Google Scholar]
- 9.Bureau NJ, et al. Lumbar facet joint synovial cyst: percutaneous treatment with steroid injections and distention. Radiology. 2001;221(1):179–185. doi: 10.1148/radiol.2211010213. [DOI] [PubMed] [Google Scholar]
- 10.Casselman ES. Radiologic recognition of symptomatic spinal synovial cysts. AJNR Am J Neuroradiol. 1985;6.6:971–973. [PMC free article] [PubMed] [Google Scholar]
- 11.Conrad MR, Pitkethly DT. Bilateral synovial cysts creating spinal stenosis: CT diagnosis. J Comput Assist Tomogr. 1987;11.1:196–197. doi: 10.1097/00004728-198701000-00049. [DOI] [PubMed] [Google Scholar]
- 12.Deshmukh NV, Kanse P (2003) Lumbar facet synovial cyst. Postgrad Med J 79.933:419, 423–419, 424 [DOI] [PMC free article] [PubMed]
- 13.Doherty PF, et al. Bilateral synovial cysts of the thoracic spine a case report. Surg Neurol. 1993;39.4:279–281. doi: 10.1016/0090-3019(93)90005-L. [DOI] [PubMed] [Google Scholar]
- 14.Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: prevalence on magnetic resonance imaging. Spine. 2004;29(8):874–878. doi: 10.1097/00007632-200404150-00010. [DOI] [PubMed] [Google Scholar]
- 15.Duplay J, Grellier P, Roche JL. Non discal surgical sciatic neuralgia (author’s transl) Sem Hop. 1981;57.25–28:1242–1245. [PubMed] [Google Scholar]
- 16.Eyster EF, Scott WR. Lumbar synovial cysts: report of eleven cases. Neurosurgery. 1989;24(1):112–115. doi: 10.1097/00006123-198901000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Eustacchio S, et al. Intraspinal synovial cyst at the craniocervical junction. Zentralbl Neurochir. 2003;64.2:86–89. doi: 10.1055/s-2003-40378. [DOI] [PubMed] [Google Scholar]
- 18.Fardon DF, Simmons JD. Gas-filled intraspinal synovial cyst. A case report. Spine. 1989;14.1:127–129. doi: 10.1097/00007632-198901000-00029. [DOI] [PubMed] [Google Scholar]
- 19.Freidberg SR, Fellows T, Thomas CB, Mancall AC (1994) Experience with symptomatic spinal epidural cysts. Neurosurgery 34(6):989–993; discussion 993 [DOI] [PubMed]
- 20.Hemminghytt S, et al. Intraspinal synovial cysts: natural history and diagnosis by CT. Radiology. 1982;145.2:375–376. doi: 10.1148/radiology.145.2.7134440. [DOI] [PubMed] [Google Scholar]
- 21.Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg. 1999;91.2(Suppl):193–199. doi: 10.3171/spi.1999.91.2.0193. [DOI] [PubMed] [Google Scholar]
- 22.Hsu KY, et al. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine. 1995;20.1:80–89. doi: 10.1097/00007632-199501000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Jabre A, Shahbabian S, Keller JT. Synovial cyst of the cervical spine. Neurosurgery. 1987;20.2:316–318. doi: 10.1227/00006123-198702000-00020. [DOI] [PubMed] [Google Scholar]
- 24.Jackson DE, Jr, et al. Intraspinal synovial cysts: MR imaging. Radiology. 1989;170.2:527–530. doi: 10.1148/radiology.170.2.2911681. [DOI] [PubMed] [Google Scholar]
- 25.Jost SC, Hsien Tu P, Wright NM. Symptomatic intraosseous synovial cyst in the cervical spine: a case report. Spine. 2003;28.17:E344–E346. doi: 10.1097/01.BRS.0000090501.42188.2A. [DOI] [PubMed] [Google Scholar]
- 26.Kaneko K, Inoue Y. Haemorrhagic lumbar synovial cyst. A cause of acute radiculopathy. J Bone Joint Surg Br. 2000;82.4:583–584. doi: 10.1302/0301-620X.82B4.10444. [DOI] [PubMed] [Google Scholar]
- 27.Kao CC, et al. Lumbar intraspinal extradural ganglion cyst. J Neurosurg. 1968;29.2:168–172. doi: 10.3171/jns.1968.29.2.0168. [DOI] [PubMed] [Google Scholar]
- 28.Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg. 1974;41.3:372–376. doi: 10.3171/jns.1974.41.3.0372. [DOI] [PubMed] [Google Scholar]
- 29.Khan AM, Synnot K, Camissa FP, Girardi FP. Lumbar synovial cysts of the spine: an evaluation of surgical outcome. J Spinal Disord Tech. 2005;18(2):127–131. doi: 10.1097/01.bsd.0000156830.68431.70. [DOI] [PubMed] [Google Scholar]
- 30.Knox AM, Fon GT. The appearances of lumbar intraspinal synovial cysts. Clin Radiol. 1991;44.6:397–401. doi: 10.1016/S0009-9260(05)80658-0. [DOI] [PubMed] [Google Scholar]
- 31.Koenigsberg RA. Percutaneous aspiration of lumbar synovial cyst: CT and MRI considerations. Neuroradiology. 1998;40(4):272–273. doi: 10.1007/s002340050584. [DOI] [PubMed] [Google Scholar]
- 32.Kurz LT, et al. Intraspinal synovial cyst causing sciatica. J Bone Joint Surg Am. 1985;67.6:865–871. [PubMed] [Google Scholar]
- 33.Lemish W, Apsimon T, Chakera T. Lumbar intraspinal synovial cysts. Recognition and CT diagnosis. Spine. 1989;14.12:1378–1383. doi: 10.1097/00007632-198912000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Lyons MK, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg. 2000;93.1(Suppl):53–57. doi: 10.3171/spi.2000.93.1.0053. [DOI] [PubMed] [Google Scholar]
- 35.Mercader J, Munoz GJ, Cardenal C. Intraspinal synovial cyst: diagnosis by CT. Follow-up and spontaneous remission. Neuroradiology. 1985;27.4:346–348. doi: 10.1007/BF00339570. [DOI] [PubMed] [Google Scholar]
- 36.Metellus P, et al. A retrospective study of 32 lumbar synovial cysts. Clinical aspect and surgical management. Neurochirurgie. 2003;49.2–3(Pt 1):73–82. [PubMed] [Google Scholar]
- 37.Nijensohn E, et al. Calcified synovial cyst of the cervical spine: CT and MR evaluation. J Comput Assist Tomogr. 1990;14.3:473–476. doi: 10.1097/00004728-199005000-00031. [DOI] [PubMed] [Google Scholar]
- 38.Onofrio BM, Mih AD. Synovial cysts of the spine. Neurosurgery. 1988;22.4:642–647. doi: 10.1227/00006123-198804000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Parlier-Cuau C, et al. Symptomatic lumbar facet joint synovial cysts: clinical assessment of facet joint steroid injection after 1 and 6 months and long-term follow-up in 30 patients. Radiology. 1999;210.2:509–513. doi: 10.1148/radiology.210.2.r99fe60509. [DOI] [PubMed] [Google Scholar]
- 40.Pendleton B, Carl B, Pollay M. Spinal extradural benign synovial or ganglion cyst: case report and review of the literature. Neurosurgery. 1983;13.3:322–326. doi: 10.1227/00006123-198309000-00021. [DOI] [PubMed] [Google Scholar]
- 41.Pirotte B, et al. Synovial cysts of the lumbar spine: surgery-related results and outcome. J Neurosurg. 2003;99.1(Suppl):14–19. doi: 10.3171/spi.2003.99.1.0014. [DOI] [PubMed] [Google Scholar]
- 42.Reust P, et al. Degenerative spondylolisthesis, synovial cyst of the zygapophyseal joints, and sciatic syndrome: report of two cases and review of the literature. Arthritis Rheum. 1988;31(2):288–294. doi: 10.1002/art.1780310220. [DOI] [PubMed] [Google Scholar]
- 43.Rousseaux P, et al. Synovial cysts and synovialomas of the lumbar spine. Histo-pathologic and neuro-surgical aspects apropos of 8 cases. Neurochirurgie. 1989;35.1:31–39. [PubMed] [Google Scholar]
- 44.Sabo RA, Tracey PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg. 1996;85:560–565. doi: 10.3171/jns.1996.85.4.0560. [DOI] [PubMed] [Google Scholar]
- 45.Salmon B, et al. A Juxtafacet cyst of the lumbar spine Clinical, radiological and therapeutic aspects in 28 cases. Acta Neurochir (Wien) 2001;143(2):129–134. doi: 10.1007/s007010170117. [DOI] [PubMed] [Google Scholar]
- 46.Schmid G, et al. Lumbar intraspinal juxtafacet cysts: MR imaging and CT-arthrography. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr. 2002;174.10:1247–1252. doi: 10.1055/s-2002-34561. [DOI] [PubMed] [Google Scholar]
- 47.Schollner D. Ganglion on a vertabral joint. Z Orthop Ihre Grenzgeb. 1967;102.4:619–620. [PubMed] [Google Scholar]
- 48.Soon CK, Razak M. Haemorrhagic lumbar synovial cyst. Med J Malaysia. 2001;56(Suppl D):57–60. [PubMed] [Google Scholar]
- 49.Spencer RR, Jahnke RW, Hardy TL. Dissection of gas into an intraspinal synovial cyst from contiguous vacuum facet. J Comput Assist Tomogr. 1983;7.5:886–888. doi: 10.1097/00004728-198310000-00025. [DOI] [PubMed] [Google Scholar]
- 50.Slipman CW, et al. Nonsurgical treatment for radicular of pain of zygoapophyseal joint cyst origin: therapeutic selective nerve root block. Arch Phys Med Rehabil. 2000;81(8):1119–1122. [PubMed] [Google Scholar]
- 51.Sauvage P, et al. Lumbar intraspinal synovial cysts: imaging and treatment by percutaneous injection. Report of thirteen cases. J Radiol. 2000;81(1):33–38. [PubMed] [Google Scholar]
- 52.Tatter SB, Cosgrove GR. Hemorrhage into a lumbar synovial cyst causing an acute cauda equina syndrome Case report. J Neurosurg. 1994;81.3:449–452. doi: 10.3171/jns.1994.81.3.0449. [DOI] [PubMed] [Google Scholar]
- 53.Tillich M, et al. Symptomatic intraspinal synovial cysts of the lumbar spine: correlation of MR and surgical findings. Neuroradiology. 2001;43.12:1070–1075. doi: 10.1007/s002340100682. [DOI] [PubMed] [Google Scholar]
- 54.Trummer M, et al. Diagnosis and surgical management of intraspinal synovial cysts: report of 19 cases. J Neurol Neurosurg Psychiatry. 2001;70(1):74–77. doi: 10.1136/jnnp.70.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vosschulte K, Borger G. Anatomische and funktinonelle Untersuchugen iiber den Bandsheibenprolaps. Langenbecks Arch klin Chir. 1950;265:329–355. doi: 10.1007/BF01399563. [DOI] [PubMed] [Google Scholar]
- 56.Yarde WL, et al. Synovial cysts of the lumbar spine: diagnosis, surgical management, and pathogenesis. Report of eight cases. Surg Neurol. 1995;43.5:459–464. doi: 10.1016/0090-3019(95)80090-4. [DOI] [PubMed] [Google Scholar]