Abstract
Objective
We sought to develop a reliable and valid tool for measuring teamwork among Emergency Medical Technician (EMT) partnerships.
Methods
We adapted existing scales and developed new items to measure components of teamwork. After recruiting a convenience sample of 39 agencies, we tested a 122-item draft survey tool. We performed a series of Exploratory Factor Analyses (EFA) and Confirmatory Factor Analysis (CFA) to test reliability and construct validity, describing variation in domain and global scores using descriptive statistics.
Results
We received 687 completed surveys. The EFA analyses identified a 9-factor solution. We labeled these factors [1] Team Orientation, [2] Team Structure & Leadership, [3] Partner Communication, Team Support, & Monitoring, [4] Partner Trust and Shared Mental Models, [5] Partner Adaptability & Back-Up Behavior, [6] Process Conflict, [7] Strong Task Conflict, [8] Mild Task Conflict, and [9] Interpersonal Conflict. We tested a short form (30-item SF) and long form (45-item LF) version. The CFA analyses determined that both the SF and LF versions possess positive psychometric properties of reliability and construct validity. The EMT-TEAMWORK-SF has positive internal consistency properties with a mean Cronbach’s alpha coefficient ≥0.70 across all 9-factors (mean=0.84; min=0.78, max=0.94). The mean Cronbach’s alpha coefficient for the EMT-TEAMWORK-LF version was 0.87 (min=0.79, max=0.94). There was wide variation in weighted scores across all 9 factors and the global score for the SF and LF versions. Mean scores were lowest for the Team Orientation factor (48.1, SD 21.5 SF; 49.3 SD 19.8 LF) and highest (more positive) for the Interpersonal Conflict factor (87.7 SD 18.1 for both SF and LF).
Conclusions
We developed a reliable and valid survey to evaluate teamwork between EMT partners.
INTRODUCTION
Teamwork is important to safe healthcare delivery. Key components of teamwork include mutual trust, shared mental models, and closed loop communication.1 Poor teamwork behaviors are associated with negative patient outcomes.2-4 Teams of EMS providers are most often configured with two EMT-paramedics or one EMT-paramedic and one EMT-Basic,5 though some EMS agencies configure teams with EMT-Intermediates, prehospital nurses, or teams of two EMT-Basics. Research characterizing teamwork in EMS is limited and teamwork measurement tools are lacking.
Teamwork in Emergency Medical Services (EMS) is critical to effective and safe care delivery. EMT partners must work together to establish scene safety, load and move patients, deliver stabilizing care on scene and during transport, and transfer patient care to receiving facilities.6-9 An EMT must anticipate the actions and expectations of his/her partner with minimal disruption. Stress, fatigue, and frequent turnover in partnerships are common characteristics of EMS work that may threaten teamwork between EMT partners.10-14
A tool that can measure teamwork between EMT partners is absent; such a tool may help evaluate training and improve safety by diagnosing poor or positive teamwork and optimize crew pairings. We sought to develop a reliable and valid tool for measuring teamwork among EMTs at the dyadic (2 person) level.
METHODS
Study Design and Sample
We used a cross-sectional study design to develop and test a teamwork instrument on EMTs and paramedics recruited from a convenience sample of EMS agencies. The University of Pittsburgh Institutional Review Board approved this study.
Instrument Development
We followed prescribed steps for survey development by adopting the Salas et al’s “Big Five” framework of teamwork measurement.1,15 This framework operationalizes teamwork into five constructs (Team Leadership, Team Orientation, Mutual Performance Monitoring, Back-Up Behavior, Adaptability) and three coordinating mechanisms (Closed Loop Communication, Shared Mental Models, and Mutual Trust).1 We added an additional construct, the measurement of conflict among teammates. Our focus group work identified conflict as important to EMT teamwork and performance.
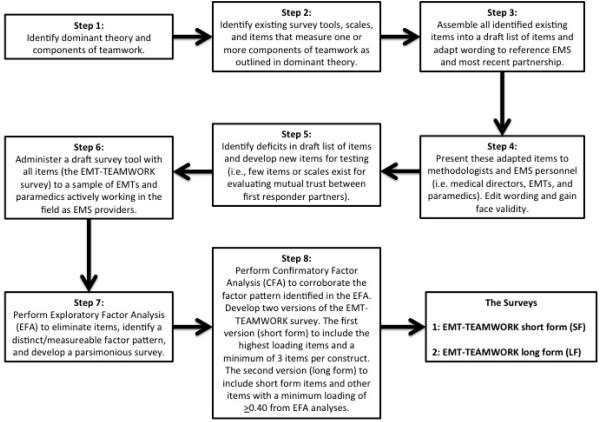
We reviewed the literature to identify established reliable and valid survey scales of teamwork (e.g., the TeamSTEPPS survey and Collective Orientation Scale).16,17 Key search terms included: teamwork, teams, safety, partners, partnerships, and team performance. We also obtained scales under development.18,19 We adapted the wording of all existing scales to reference EMS partnerships at the dyadic level. We then assigned each item in every scale to a construct to designate the component of teamwork or conflict to which it was intended to measure (Figure 1).
Figure 1.
Step-by-step illustration of survey development
We recorded possible item responses on a 7-point Likert scale (Strongly Disagree to Strongly Agree). Forty-five items included the additional response option “Does Not Apply.” We included this response option to: 1) examine the utility of this option for EMS crews as a standard neutral response rather than the standard “Neither Agree nor Disagree”, and 2) to provide EMTs a response option for partnerships where interactions (i.e., patient care episodes) may be limited. In addition, we included 7 questions on EMT demographic characteristics.
Recruitment of Agencies
We recruited a convenience sample of EMS administrators affiliated with the National EMS Management Association (NEMSMA). After distributing a letter on the association’s email Listserv describing the study, we recruited administrators with an interest in study participation and contacted each to enroll his/her agency. Eligible agencies provided state licensed prehospital emergency care services and configured crews in dyads. Thirty-nine administrators agreed to participate.
Study Protocol
We administered our EMT-TEAMWORK survey via a secure Internet-based survey system. EMS agency administrators used our survey system to prerecord the following information for each employee: employee email address, employment status (Full-time, Part-time, Volunteer), percent of clinical work (0-100%), years of service at agency (e.g., 5 years) and level of certification (Paramedic, EMT-Basic, Other). The administrators circulated a study flyer and communicated the importance of the study to employees during group meetings and other agency functions. The administrators used our survey system to distribute the EMT-TEAMWORK survey. Individual EMTs received an email from the University of Pittsburgh that included a brief description of our study, a secure link to the survey, and link for opting-out.
We collected data from January to December 2010. We asked administrators to promote participation by letting their employees know they strongly supported the study. Administrators periodically logged into their survey system account to view their agency’s overall response rate. We gave administrators the option of sending the survey links with the opt-out option multiple times. We designed our survey system to keep the respondent / non-respondent status of email addresses confidential. This strategy encouraged administrators to focus on the agency as a whole to promote participation, as they could not follow-up with individual non-respondents. We gave a two-part incentive for the agency with the highest overall response rate. The first part was a $25 dollar gift card to the agency. The second part was a combination of a $5 dollar gift card for all employees in the agency and 30 high-end stethoscopes that the agency administrator could use to restock agency issued first-in bags or distribute to individual employees.
Analysis
At the end of the data collection phase of the study, we received a dataset with coded responses linked to randomly generated agency and survey ID numbers. We calculated percentages, means, and standard deviations to describe the agency and respondent characteristics. Using parametric tests (Pearson correlations and t-tests) and non-parametric tests (chi-square tests), we explored differences in respondents versus non-respondents. We weighted responses from 0 to 100 to improve interpretation of scores by increasing the spread of data (Strongly Disagree=0, Disagree=16.6, Slightly Disagree=33.3, Neither Agree nor Disagree=49.9, Slightly Agree=66.6, Agree=83.3, Strongly Agree=100). We reverse coded negatively worded items.
We performed a series of Exploratory Factor Analyses (EFA) to reduce the total number of items in our draft survey (n=122) and identify distinct/measurable factors of teamwork and conflict.20 We sought to develop two versions of a final survey tool. One version (the Short Form SF) included the minimally recommended number of three items per construct and satisfied the requirements to be low-burden on respondents and most applicable to day-to-day human resource management.15,20 The second version (Long Form LF) included as many items as the CFA analysis would allow and be applicable to investigations of teamwork and have applications in the education and simulation arena.
Our first EFA specified a 10-factor model corresponding to the Salas Big Five framework, TeamSTEPPS survey, and Collective Orientation Scale.1,16,17 Separate EFAs assessed specific 4-factor conflict structure. We used the principal factors approach and oblique rotation method. The principal factors method is a standard approach to extracting a meaningful factor structure and latent variables, and the oblique rotation assumes latent factors are correlated.20 We performed multiple EFAs until we obtained a simple factor structure.20
We retained items with a ≥0.40 factor loading to develop a short form and long form draft of the EMT-TEAMWORK survey.20,21 We excluded items with high loadings on multiple factors.20,21 We used Confirmatory Factor Analysis (CFA) to test if the items selected for the EMT-TEAMWORK-SF and EMT-TEAMWORK-LF surveys exhibited positive model fit characteristics.20,21 We evaluated six standard measures of model fit (construct validity) and three standard measures of internal consistency (reliability): the Goodness of Fit Index (GFI), Bentler’s Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), Bentler & Bonett’s Non-normed Index (NNFI), Bentler & Bonnett’s Normed Fit Index (NFI), Standardized Root Mean Square Residual (SRMR), Cronbach’s alpha coefficients, and item-factor Pearson correlation coefficients, and Pearson factor-to-factor correlation coefficients. An SRMR less than 0.08, RMSEA less than 0.06, and GFI, CFI, NNFI, and NFI ≥0.9 are considered acceptable indices of instrument validity and model fit.20,22-24 Cronbach’s alpha coefficient scores ≥0.70, item-scale Pearson correlations ≥0.40, and factor-to-factor Pearson correlation coefficients that are less than factor Cronbach’s alpha coefficients are evidence that each factor measures unique variance in the data.25-28
We calculated factor summary scores by dividing the sum of item scores by total items retained for the factor. A global teamwork score arose by dividing the sum of factor summary scores by the total number of retained factors. We reverse scored conflict items so that a “Strongly Disagree” was connected to a 100 value – more positive/less conflict score – and a “Strongly Agree” with a 0 – a more negative/more conflict score. For purposes of calculating Pearson correlations, we inverted the scoring to match the valence of all non-conflict items (i.e., Strongly Disagree = 0). Using inverted scores, a negative Pearson correlation coefficient between teamwork constructs and conflict constructs would provide evidence that our survey distinguishes between positive and non-positive teamwork.25 Conversely, a positive correlation would suggest that our specified model is an inaccurate (invalid) fit for the data.
We performed EFA analyses on a subset of completed surveys, excluding surveys with a “Does Not Apply” response to any item (Dataset A). We created two additional datasets (Dataset B and Dataset M) to: 1) evaluate need (utility) of a “Does Not Apply” response option over a standard neutral response (i.e., Neither Agree nor Disagree), and 2) evaluate impact of imputing mean versus neutral response options. In dataset B we treated surveys with a “Does Not Apply” response as a “Neither Agree nor Disagree” response. We excluded surveys from this imputation if the survey included a “Does Not Apply” response for all items assigned to a factor. This approach was used to identify and exclude potentially erroneous data. Mean item imputation is a widely used survey research technique for recovering items with missing data.29 We used this technique, not to recover missing data, but to create a third dataset (Dataset M) to test the approach of replacing “Does Not Apply” responses with the mean item response from surveys included in dataset A. Discovery of low variation in teamwork scores across datasets A, B, and M would suggest that it is acceptable to impute “Neither Agree nor Disagree” neutral responses where respondents indicated “Does Not Apply.” SAS version 9.2 (Cary, North Carolina) was the designated statistical program.
RESULTS
We received completed surveys from 687 EMS personnel. The overall response rate was 30%, which ranged from 10% to 80% across 39 EMS agencies (mean agency level response rate was 33%). Across the total number of surveys (n= 687), nearly three quarters of respondents were male (72%; Table 1). Among respondents, the most common shift worked was 12-hour (42%) followed by 24-hour shifts (37%). Compared to non-respondents, respondents had greater mean years of agency service (7.2 vs. 5.9, p=0.0001), included a greater proportion of EMT-Paramedics (61% vs. 51%, p=0.0014), and greater proportion of full-time employees (72% vs. 63%, p<0.0001). The mean percentage of clinical work (non-administrative work) among respondents was slightly lower than among non-respondents (66% vs. 70%, p=0.02).
Table 1.
Demographic characteristics of study sample
| Agency demographics | % (freq) | Respondent demographics | Respondents % (freq) mean (SD) |
Non- Respondents % (freq) mean (SD) |
|---|---|---|---|---|
| Total Agencies | N=39 | Total | N=687 | N=1,627 |
| Census Region | Sex | |||
| South | 7.7% (3) | Female | 27.7% (190) | --- |
| Northeast | 35.9% (14) | Male | 72.3% (497) | --- |
| Midwest | 48.7% (19) | Certification * | ||
| West | 7.7% (3) | Paramedic | 61.4% (422) | 50.9% (828) |
| Staffing Mix | EMT-Basic | 28.7% (197) | 36.0% (586) | |
| All paid | 69.2% (27) | Other | 9.9% (68) | 13.1% (213) |
| Mix paid and volunteer | 23.1% (10) | Employment status* | ||
| All volunteer | 5.1% (2) | Full-Time | 71.7% (493) | 63.3% (1,030) |
| Agency Classification | Part-Time | 21.1% (145) | 30.2% (491) | |
| Hospital-Based | 18.0% (7) | Volunteer | 7.2% (49) | 6.6% (106) |
| Fire-Based | 7.7% (3) | |||
| Third Service | 41.0% (16) | Most common shift worked | ||
| Rescue Squad | 5.1% (2) | 24 hour | 36.5% (251) | --- |
| Other | 28.2% (11) | 12 hour | 42.1% (289) | --- |
| Agency Ownership | 8 hour | 17.1% (117) | --- | |
| Private For-Profit | 7.7% (3) | <8 hour | 4.3% (30) | --- |
| Private Non-Profit | 69.2% (27) | |||
| Government Funded | 17.9% (7) | Mean years service at agency* | 7.2 (SD 7.1) | 5.9 (SD 6.6) |
| Member Supported | 2.6% (1) | |||
| Other | 2.6% (1) | Mean % time doing clinical work | 65.8 (SD 37.1) | 69.9 (SD 39.0) |
Table Notes: Indicates a p-value <0.05 for comparisons of proportions between respondents and non-respondents.
Respondents and non-respondents are affiliated with 39 diverse EMS agencies, half of which are located in the Midwest U.S. Census region (Table 1). Sixteen agencies self-classified as a third-service delivery model and 69% operated as a private non-profit.
Datasets A, B, and M were developed for purposes of our EFA and CFA analyses. Dataset A included 318 surveys after excluding any item with a “Does Not Apply” response. Datasets B and M included 548 surveys after using item recovery techniques described in our analysis section. The EFA analyses performed on all datasets independently determined that 14 of the 103 tested teamwork and conflict items failed to reach the ≥0.40 factor loading benchmark or loaded on to multiple factors. The remaining 89 items loaded onto a 9-factor structure that we labeled [1] Team Orientation (TO), [2] Team Structure & Leadership (TSL), [3] Partner Communication, Team Support, & Monitoring (PCTSM), [4] Partner Trust and Shared Mental Models (PTSMM), [5] Partner Adaptability & Back-Up Behavior (PABUB), [6] Process Conflict, [7] Strong Task Conflict, [8] Mild Task Conflict, and [9] Interpersonal Conflict.
CFA analysis linked 30 high loading items to the 9-factor structure of teamwork and conflict specified in the EFA findings. Values for CFA construct validity measures were positive and include: SRMR=0.016, RMSEA=0.056, GFI=0.93, CFI=0.97, NNFI=0.94, and NFI=0.95. Negative correlations between the five teamwork factors and four conflict factors are further support for construct validity (mean=−0.30, min=0.00, max=−0.69; Table 2). We labeled this 30-item survey model the EMT-TEAMWORK-Short Form (EMT-TEAMWORK-SF).
Table 2.
Construct correlation matrix
| Team Orientation (TC) |
Team Structure & Leadership (TSL) |
Partner Communication, Team Support, & Monitoring (PCTSM) |
Partner Trust and Shared Mental Models (PTSMM) |
Partner Adaptability & Back-Up Behavior (PABUB) |
Process Conflict (PC) |
Strong Task Conflict (STC) |
Mild Task Conflict (MTC) |
Interpersonal Conflict (IC) |
|
|---|---|---|---|---|---|---|---|---|---|
| TSL | |||||||||
| ShortForm | 0.05 | ||||||||
| LongForm | 0.11* | ||||||||
|
| |||||||||
| PCTSM | |||||||||
| ShortForm | 0.23† | 0.45† | |||||||
| LongForm | 0.25† | 0.54† | |||||||
|
| |||||||||
| PTSMM | |||||||||
| ShortForm | 0.17† | 0.41† | 0.50† | ||||||
| LongForm | 0.21† | 0.42† | 0.55† | ||||||
|
| |||||||||
| PABUB | |||||||||
| ShortForm | 0.11* | 0.32† | 0.66† | 0.30† | |||||
| LongForm | 0.18† | 0.45† | 0.73† | 0.45† | |||||
|
| |||||||||
| PC | |||||||||
| ShortForm | −0.18† | −0.35† | −0.41† | −0.69† | −0.33† | ||||
| LongForm | −0.21† | −0.36† | −0.42† | −0.68† | −0.41† | ||||
|
| |||||||||
| STC | |||||||||
| ShortForm | −0.17† | −0.31† | −0.42† | −0.68† | −0.27† | 0.71† | |||
| LongForm | −0.20† | −0.32† | −0.41† | −0.69† | −0.35† | 0.71† | |||
|
| |||||||||
| MTC | |||||||||
| ShortForm | −0.10* | −0.07 | 0.00 | −0.21† | 0.07 | 0.26† | 0.37† | ||
| LongForm | −0.11* | −0.05 | 0.01 | −0.21† | 0.03 | 0.26† | 0.37† | ||
|
| |||||||||
| IC | |||||||||
| ShortForm | −0.14* | −0.36† | −0.41† | −0.61† | −0.34† | 0.69† | 0.63† | 0.20† | |
| LongForm | −0.16† | −0.34† | −0.42† | −0.63† | −0.42† | 0.69† | 0.63† | 0.20† | |
|
| |||||||||
|
Overall
Teamwork Score |
|||||||||
| ShortForm | 0.41† | 0.54† | 0.68† | 0.79† | 0.54† | −0.81† | −0.81† | −0.43† | −0.75† |
| LongForm | 0.43† | 0.56† | 0.69† | 0.80† | 0.63† | −0.81† | −0.81† | −0.43† | −0.76† |
Table Notes:. = p-value <0.05.
= p-value <0.0001.
Correlations based on analysis of Dataset M (n=548).
CFA analyses of the survey that included the additional items linked 45 total items to the 9-factor structure identified in EFA analyses. Tests of model fit and construct validity of this 45 item survey support the 9-factor solution: SRMR=0.025, RMSEA=0.058, GFI=0.85, CFI=0.94, NNFI=0.90 and NFI=0.89. The mean correlation between the five teamwork constructs and four conflict constructs was −0.32 (min=0.03, max=−0.69; Table 2). We labeled this 45-item version of the survey the EMT-TEAMWORK-Long Form (EMT-TEAMWORK-LF).
The EMT-TEAMWORK-SF has positive internal consistency properties. The mean Cronbach’s alpha coefficients for the 9-scales was above the ≥0.70 benchmark (mean=0.84; min=0.78, max=0.94). The mean item-scale Pearson correlation was greater than the ≥0.40 benchmark for high reliability (mean=0.84; min=0.58, max=0.97). The mean factor-to-factor Pearson correlation among the five teamwork constructs was 0.32 (min=0.05, max=0.66), indicating that these factors measure unique variance in the data (Table 2).
The EMT-TEAMWORK-LF also exhibited positive internal consistency and reliability properties. The mean Cronbach’s alpha coefficient was 0.87 (min=0.79, max=0.94). The mean item-scale Pearson correlation was 0.80 (min=0.45, max=0.97). The mean factor-to-factor Pearson correlation among the five teamwork constructs was 0.39 (min=0.11, max=0.73).
There was wide variation in weighted scores across all 9 factors and the global teamwork score of the EMT-TEAMWORK-SF and EMT-TEAMWORK-LF (Table 3). One in every 15 respondents had a global teamwork score ≤50 while 42% scored ≤75.
Table 3.
EMT-TEAMWORK survey Short Form and Long Form summary scores
| Construct | Mean | SD | Median | Min | Max |
|---|---|---|---|---|---|
| Team Orientation (TO) | |||||
| Short Form (n=3 items) | 48.1† | 21.5† | 50.0 | 0 | 100 |
| Long Form (n=6 items) | 49.3† | 19.8† | 50.0 | 0 | 100 |
|
| |||||
| Team Structure & Leadership (TSL) | |||||
| Short Form (n=3 items) | 85.8† | 14.8† | 83.3α | 0 | 100 |
| Long Form (n=6 items) | 81.9† | 14.3† | 83.3† | 0 | 100 |
|
| |||||
| Partner Communication, Team Support, & Monitoring (PCTSM) | |||||
| Short Form (n=6 items) | 78.0† | 16.2† | 80.6 | 8.3 | 100 |
| Long Form (n=10 items) | 79.2† | 15.5† | 81.6α | 5.0 | 100 |
|
| |||||
| Partner Trust and Shared Mental Models (PTSMM) | |||||
| Short Form (n=3 items) | 85.0α | 19.1† | 88.9 | 5.6α | 100 |
| Long Form (n=6 items) | 82.9α | 16.9† | 86.1α | 22.2α | 100 |
|
| |||||
| Partner Adaptability & Back-Up Behavior (PABUB) | |||||
| Short Form (n=3 items) | 74.7α | 18.0† | 77.8α | 11.1 | 100 |
| Long Form (n=5 items) | 76.6† | 16.0† | 80.0α | 23.3 | 100 |
|
| |||||
| Process Conflict (PC) (3-items)*** | |||||
| Short Form (n=3 items) | 83.9α | 18.5† | 83.3 | 0 | 100 |
| Long Form (n=3 items) | 83.9α | 18.5† | 83.3 | 0 | 100 |
|
| |||||
| Strong Task Conflict (STC) (3-items)*** | |||||
| Short Form (n=3 items) | 80.3α | 21.1† | 83.3 | 0∞ | 100 |
| Long Form (n=3 items) | 80.3α | 21.1† | 83.3 | 0∞ | 100 |
|
| |||||
| Mild Task Conflict (MTC) (3-items)*** | |||||
| Short Form (n=3 items) | 54.1α | 24.7† | 50.0 | 0 | 100 |
| Long Form (n=3 items) | 54.1α | 24.7† | 50.0 | 0 | 100 |
|
| |||||
| Interpersonal Conflict (IC) (3-items)*** | |||||
| Short Form (n=3 items) | 87.7† | 18.1† | 94.4α | 0∞ | 100 |
| Long Form (n=3 items) | 87.7† | 18.1† | 94.4α | 0∞ | 100 |
|
| |||||
| Total / Overall Teamwork Score (27-items)*** | |||||
| Short Form (n=30 items) | 75.4† | 12.0† | 77.8† | 20.7 | 99.4 |
| Long Form (n=45 items) | 75.2† | 11.8† | 77.6† | 23.7† | 98.1† |
Table Notes: Scores based on analysis of Dataset M (n=548 surveys).
=Conflict scores are scored in reverse “Strongly Agree = 0 to Strongly Disagree = 100” when calculating the mean, std, median, minimum, and maximum for this table. We used these scores when calculating the Total / Overall Teamwork Score. This allowed the overall score to range from a minimum 0 to maximum 100.
=signifies that the standard deviation of scores across Datasets A, B, and M was greater than 0 and less than 1 percentage points,
= less than 5 percentage points,
= less than 10 percentage points.
The use of mean item imputation, imputation of “Neither Agree nor Disagree” response, or exclusion of observations with a “Does Not Apply” response had no meaningful impact on factor or global teamwork score calculations (Table 3). The mean global teamwork score across all three datasets for the EMT-TEAMWORK-SF was 75.2 (min=74.3, max=75.8). The mean global score for the EMT-TEAMWORK-LF was 75.0 (min=74.2, max=75.6).
DISCUSSION
Recent data show that many EMTs work with 19 different partners annually – and some work with more than 50 partners in one year.14 Frequent turnover in partnerships can disrupt team cohesiveness, influence behavior, and threaten safety.30-35 Improving safety in response to these potential threats to teamwork requires careful diagnosis of deficits in teamwork between partners. We developed the EMT-TEAMWORK survey to be EMT and dyad specific and to identify deficits in teamwork between EMTs. In this study sample, tests confirm both the short form and long form versions of the EMT-TEAMWORK survey have positive psychometric properties of reliability and construct validity. These findings are evidence the EMT-TEAMWORK survey measures multiple components of teamwork that in other settings have been found to impact safety, quality, and performance.3,4
A previous study by Kalisch and colleagues used the Salas “Big Five” framework to develop a similar teamwork measurement tool specific to in-hospital nurses.18 Their approach was similar to ours; they began with 74 candidate items and used EFA techniques to identify a parsimonious factor structure. They then used CFA to develop a reliable and valid survey tool. Their EFA and CFA findings led them to identify five factors and 45 items for use in teamwork tool. The methods and findings of the Kalisch et al study are similar to our own and provide evidence in support of developing survey tools calibrated to the unique interactions of teammates in different occupations.
We are at the earliest stages of teamwork assessment in EMS. We designed the scoring of each domain (construct) and global score to range from 0 to 100 with higher scores indicating more positive perceptions. Table 3 provides an initial illustration of score variation for nine domains of teamwork and across respondents. We recognize that longitudinal study designs are needed to identify change in EMT-TEAMWORK survey scores in response to changes in partnerships over time and to test hypothesized associations between partner familiarity, teamwork, and safety outcomes. These studies may help determine cut points in domain scores where threats to patient and provider safety are elevated.
We have the following recommendations for those that wish to employ the EMT-TEAMWORK survey before the completion of additional research. First, we recommend that EMS managers administer the survey to EMTs for each unique partnership and document scores over time at the individual and team level. Second, memory of occupational experiences decays at a rapid pace.36,37 We recommend managers administer the survey no more than two months post shift/partnership to obtain accurate responses to EMT-TEAMWORK items.36 Third, the EMT-TEAMWORK LF and SF were developed for two different purposes. The EMT-TEAMWORK-LF includes additional items that make it better suited for research purposes. For example, investigators may use the EMT-TEAMWORK-LF to evaluate the impact of experimental team training programs in the formative or continuing education settings. On the other hand, because of its brevity (roughly 5 minutes), the SF form seems more appropriate for day-to-day human resource purposes. Fourth, confidentiality of responses may be an issue that affects participation and validity of responses from EMTs. We recommend managers offer assurances to EMTs that their scores will be held confidential and will not be shared with their partners. See Appendix A for copies of both the SF and LF EMT-TEAMWORK surveys.
LIMITATIONS
At the individual respondent level, our study sample is analogous to samples of EMS workers in other studies in age, sex, employment status, and level of certification (Table 4). However, our results cannot be generalized to determine the level of teamwork in EMS agencies across the United States. However, generalizability of these scores was not an aim of this study. Our primary aim was to develop a valid and reliable survey tool for evaluating teamwork between EMS provider partnerships at the dyadic level – not agency level. The dyadic configuration of EMS partnerships is the most common structure of EMS workers and is not limited to one type of delivery model. Tables 1 and 4 highlight the diversity of our study sample at the agency level, which we believe strengthens application of the EMT-TEAMWORK survey to most EMS delivery models. Modifications in item wording would be necessary for EMS agencies that configure teams of three or four.
Table 4.
Characteristics of study sample compared to other research studies of EMS workers
| Characteristic | Study Sample |
LEADS Sample38 |
High Response EMS Sample39 |
NHTSA Workforce Report40 ** |
Resuscitation Outcomes Consortium Agencies41 |
Longitudinal Study of EMS Turnover42 |
National Survey of EMS Safety Culture12 |
|
|---|---|---|---|---|---|---|---|---|
| Respondents (n=687) |
Non- Respondents (n=1,627) |
|||||||
|
Individual
Characteristics |
||||||||
|
| ||||||||
| Sex | ||||||||
| Male | 72.3% | --- | 72.9% | 71.8% | 71-77% | --- | --- | 73.2% |
| Female | 27.7% | --- | 27.1% | 28.2% | 23-29% | --- | --- | 26.8% |
|
| ||||||||
| Certification | ||||||||
| EMT-Basic | 28.7% | 36.0% | 58.1% | 50.7% | #72% | 58.2% | --- | 19.4% |
| Paramedic | 61.4% | 50.9% | 34.6% | 49.3% | #22% | 34.2% | --- | 62.1% |
|
| ||||||||
| Mean Age in Years | 36.9 | --- | --- | --- | 35 | --- | --- | --- |
|
| ||||||||
| Employment Status | ||||||||
| Full-Time | 71.7% | 63.3% | --- | --- | $89% | --- | --- | 77.6% |
| Part-Time | 21.1% | 30.2% | --- | --- | $11% | --- | --- | 20.6% |
| Volunteer | 7.2% | 6.6% | --- | --- | --- | --- | 1.8% | |
|
| ||||||||
| Agency Affiliation (EMT unit of measurement) |
Fire includes Rescue squads |
+Includes | ||||||
| Fire-Based | 11.8% | 7.9% | 34.1% | --- | county/3rd | --- | --- | --- |
| County/3rd Service | 60.0% | 50.6% | 12.1% | --- | +30%^^ | --- | --- | --- |
| Hospital | 16.2% | 20.1% | 9.9% | --- | 20%^^ | --- | --- | --- |
| Other | 12.0% | 21.5% | 43.8% | --- | 50%^^ | --- | --- | --- |
|
| ||||||||
| Mean Years of Service at Agency |
7.2 (SD 7.1) | 5.9 (SD 6.6) | --- | --- | --- | --- | --- | --- |
|
| ||||||||
| Mean Percentage of Work devoted to Clinical Field Work (not administrative) |
65.8 (SD 37.1) | 69.9 (SD 39.0) | --- | --- | --- | --- | --- | --- |
|
| ||||||||
|
Agency
Characteristics (Agency Unit of Measurement) |
||||||||
|
| ||||||||
| Agency Affiliation | ||||||||
| Fire-Based | (+ Rescue Squad) 10.5% | --- | --- | --- | 62.5% | 10.0% | 11.5% | |
| County/3rd Service | 39.5% | --- | --- | --- | 25.7% | 22.5% | 19.7% | |
| Hospital | 18.4% | --- | --- | --- | N/A | 27.5% | 29.5% | |
| Other (i.e. private) | 29.0% | --- | --- | --- | 11.8% | 40.0% | 39.3% | |
The NHTSA Workforce report includes statistics based on data from the 2003 and 2005 Current Population Survey (CPS), the 2007 National Registry of EMTs (NREMT) registration database, the 2004-05 Edition of the Bureau of Labor Statistics Occupational Outlook Handbook.
=indicates source was the 2007 NREMT database statistics cited within the NHTSA Workforce report and excludes statistics from EMT-Intermediates.
=is used to indicate data from this source does not stratify EMTs by volunteer status and automatically labels an EMT as Full-Time based on the EMT working greater than or equal to 35 hours per week.
Categories reported in the NHTSA Workforce report are not completely analogous to the stratums defined in this study. We collapsed several categories in the NHTSA Workforce report deemed similar to stratums in this study (e.g. 50% Other includes “private ambulance services and ‘other’ in the Workforce Report; and 30% County/3rd service includes all types of local government types).
=The mean of medians reported in Table 2 of the Davis et al, 2007 publication.
For the ROC agency affiliation, the categories are Fire-Based, Non-fire government (county/3rd service), and Private (other).
We identified differences in respondents and non-respondents that may have an impact on scores calculated for the 9 factors and global score of the EMT-TEAMWORK survey. Part-time and volunteer EMTs were more common among non-respondents. In some paid agencies, part-timers may be used to fill empty or unfilled shifts or called upon on an as needed basis. Their perceptions of one or more components of teamwork may be lower and contribute to a drop in the mean weighted scores for one or more component scores of the EMT-TEAMWORK survey. This concern extends to agencies with all-volunteer personnel who represent a small proportion of respondents. Again, these differences in respondents and non-respondents do not impact the development of the tool or findings from psychometric tests. These differences may impact scores across the 9 factors and global score measured by the EMT-TEAMWORK survey.
CONCLUSIONS
We developed a reliable and valid survey that can evaluate nine components of teamwork between EMT partners. The EMT-TEAMWORK survey scores can be used to diagnose deficits in teamwork between newly formed to well-established partnerships.
Supplementary Material
REFERENCES
- 1.Salas E, Sims DE, Burke CS. Is there a “Big Five” in teamwork? Small Group Research. 2005;36(5):555–599. [Google Scholar]
- 2.Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13(5):330–334. doi: 10.1136/qshc.2003.008425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabol LI, Andersen ML, Osterbaard D, Bjorn B, Lilja B, Mogensen T. Descriptions of verbal communication errors between staff. An analysis of 84 root cause analysis-reports from Danish hospitals. Qual Saf Health Care. 2011 doi: 10.1136/bmjqs.2010.040238. [DOI] [PubMed] [Google Scholar]
- 4.Mazzocco K, Petitti DB, Fong KT, et al. Surgical team behaviors and patient outcomes. Am J Surg. 2008 doi: 10.1016/j.amjsurg.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Williams DM. JEMS 2008 200 city survey: the future is your choice. JEMS. 2009;34(2):36–51. doi: 10.1016/S0197-2510(09)70044-0. [DOI] [PubMed] [Google Scholar]
- 6.Wang HE, Weaver MD, Abo BN, Kaliappan R, Fairbanks RJ. Ambulance stretcher adverse events. Qual Saf Health Care. 2009;18(3):213–216. doi: 10.1136/qshc.2007.024562. [DOI] [PubMed] [Google Scholar]
- 7.Ray AM, Kupas DF. Comparison of rural and urban ambulance crashes in pennsylvania. Prehosp Emerg Care. 2007;11(4):416–420. doi: 10.1080/10903120701536966. [DOI] [PubMed] [Google Scholar]
- 8.Vilke GM, Tornabene SV, Stepanski B, et al. Paramedic self-reported medication errors. Prehosp Emerg Care. 2007;11(1):80–84. doi: 10.1080/10903120601021358. [DOI] [PubMed] [Google Scholar]
- 9.Rittenberger JC, Beck PW, Paris PM. Errors of omission in the treatment of prehospital chest pain patients. Prehosp Emerg Care. 2005;9(1):2–7. doi: 10.1080/10903120590891688. [DOI] [PubMed] [Google Scholar]
- 10.Cydulka RK, Emerman CL, Shade B, Kubincanek J. Stress levels in EMS personnel: a national survey. Prehospital Disaster Med. 1997;12(2):136–140. [PubMed] [Google Scholar]
- 11.Revicki DA, Gershon RR. Work-related stress and psychological distress in emergency medical technicians. J Occup Health Psychol. 1996;1(4):391–396. doi: 10.1037//1076-8998.1.4.391. [DOI] [PubMed] [Google Scholar]
- 12.Patterson PD, Huang DT, Fairbanks RJ, Simeone SJ, Weaver MD, Wang HE. Variation in emergency medical services workplace safety culture. Prehosp Emerg Care. 2010;14(4):448–460. doi: 10.3109/10903127.2010.497900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patterson PD, Suffoletto BP, Kupas DF, Weaver MD, Hostler D. Sleep quality and fatigue among prehospital providers. Prehosp Emerg Care. 2010;14(2):187–193. doi: 10.3109/10903120903524971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patterson PD, Arnold RM, Abebe K, et al. Variation in Emergency Medical Technician partner familiarity. Health Serv Res. 2011 doi: 10.1111/j.1475-6773.2011.01241.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeVellis RF. Scale Development: Theory and Applications. Vol 26. SAGE Publications, Inc.; Newberry Park, CA: 1991. [Google Scholar]
- 16.Clancy CM, Tornberg DN. TeamSTEPPS: assuring optimal teamwork in clinical settings. Am J Med Qual. 2007;22(3):214–217. doi: 10.1177/1062860607300616. [DOI] [PubMed] [Google Scholar]
- 17.Driskell JE, Salas E, Hughes S. Collective orientation and team performance: development of an individual difference measure. Hum Factors. 2010;52(2):316–328. doi: 10.1177/0018720809359522. [DOI] [PubMed] [Google Scholar]
- 18.Kalisch BJ, Lee H, Salas E. The development and testing of the nursing teamwork survey. Nurs Res. 2010;59(1):42–50. doi: 10.1097/NNR.0b013e3181c3bd42. [DOI] [PubMed] [Google Scholar]
- 19.Bendersky C, Behfar K, Weingart LR, Jehn KA, Todorova G, Bear J. Revisiting the dimensions of intra-group conflict: theoretical and psychometric construct refinement. Paper presented at: Annual Meeting of the International Association for Conflict Management2010; Boston, MA. [Google Scholar]
- 20.Hatcher L. A Step-by-Step Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling. SAS Institute Inc.; Cary, North Carolina: 1994. [Google Scholar]
- 21.Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess. 1995;7(3):286–299. [Google Scholar]
- 22.Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1988;103(3):411–423. [Google Scholar]
- 23.Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: the effect of sample size. Psychol Bull. 1988;103(3):411–423. [Google Scholar]
- 24.Lance CE, Butts MM, Michels LC. The sources of four commonly reported cutoff criteria - What did they really say? Organizational Research Methods. 2006;9(2):202–220. [Google Scholar]
- 25.Ware JE, Gandek B. Methods for Testing Data Quality, Scaling Assumptions, and Reliability: The IQOLA Project Approach. J Clin Epidemiol. 1998;51(11):945–952. doi: 10.1016/s0895-4356(98)00085-7. [DOI] [PubMed] [Google Scholar]
- 26.Guilford JP. Psychometric Methods. McGraw-Hill; New York, NY: 1954. [Google Scholar]
- 27.Peterson RA. A meta-analysis of cronbach’s coefficient alpha. J Consum Res. 1994;21(2):381–391. [Google Scholar]
- 28.Nunnally J. Psychometric theory. McGraw-Hill; New York, New York: 1978. [Google Scholar]
- 29.Huisman M. Imputation of missing item responses: some simple techniques. Qual Quant. 2000;34:22. [Google Scholar]
- 30.Harrison DA, Mohammed S, McGrath JE, Florey AT, Vanderstoep SW. Time matters in team performance: effects of member familiarity, entrainment, and task discontinuity on speed and quality. Personnel Psychology. 2003;56(3):633–669. [Google Scholar]
- 31.Gruenfeld DH, Mannix EA, Williams KY, Neale MA. Group composition and decision making: how member familiarity and information distribution affect process and performance. Organ Behav Hum Decis. 1996;67(1):1–15. [Google Scholar]
- 32.Bradley JH, Hebert FJ. The effect of personality type on team performance. Journal of Management Development. 1997;16(5):337–353. [Google Scholar]
- 33.Board NTS. A Review of Flightcrew-Involved Major Accidents of U.S. Air Carriers, 1978 through 1990. National Transportation Safety Board; Washington, D.C.: 1994. pp. PB94–917001. [Google Scholar]
- 34.Piquette D, Reeves S, LeBlanc VR. Stressful intensive care unit medical crises: How individual responses impact on team performance. Crit Care Med. 2009;37(4):1251–1255. doi: 10.1097/CCM.0b013e31819c1496. [DOI] [PubMed] [Google Scholar]
- 35.Smith-Jentsch KA, Kraiger K, Cannon-Bowers JA, Salas E. Do familiar teammates request and accept more backup? Transactive memory in air traffic control. Hum Factors. 2009;51(2):181–192. doi: 10.1177/0018720809335367. [DOI] [PubMed] [Google Scholar]
- 36.Jenkins P, Earle-Richardson G, Slingerland DT, May J. Time dependent memory decay. Am J Ind Med. 2002;41(2):98–101. doi: 10.1002/ajim.10035. [DOI] [PubMed] [Google Scholar]
- 37.Landren DD, Hendricks S. Effect of recall on reporting of at-work injuries. Public Health Rep. 1995;110(3):350–354. [PMC free article] [PubMed] [Google Scholar]
- 38.Studnek JR, Bentley M, Crawford JM, Fernandez AR. An assessment of key health indicators among emergency medical services professionals. Prehosp Emerg Care. 2010;14(1):14–20. doi: 10.3109/10903120903144957. [DOI] [PubMed] [Google Scholar]
- 39.Patterson PD, Huang DT, Fairbanks RJ, Wang HE. The emergency medical services safety attitudes questionnaire. Am J Med Qual. 2010;25(2):109–115. doi: 10.1177/1062860609352106. [DOI] [PubMed] [Google Scholar]
- 40.Chapman SA, Lindler V, Kaiser JA, Nielsen CS, Bates T, Hailer-O’Keefe L. Emergency Medical Services Workforce for the 21st Century Project. National Highway Traffic Safety Administration; Washington, D.C.: 2008. [Google Scholar]
- 41.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11(4):369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 42.Patterson PD, Jones CB, Hubble MW, et al. The longitudinal study of turnover and the cost of turnover in emergency medical services. Prehosp Emerg Care. 2010;14(2):209–221. doi: 10.3109/10903120903564514. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.