Abstract
The objectives of this study were to examine longitudinal patterns of Department of Veterans Affairs (VA)–only use, dual VA and Medicare use, and Medicare-only use by veterans with dementia. Data on VA and Medicare use were obtained from VA administrative datasets and Medicare claims (1998–2001) for 2,137 male veterans who, in 1997, used some VA services, had a formal diagnosis of Alzheimer’s disease or vascular dementia in the VA, and were aged 65 and older. Generalized ordered logit models were used to estimate the effects of patient characteristics on use group over time. In 1998, 41.7% of the sample were VA-only users, 55.4% were dual users, and 2.9% were Medicare-only users. By 2001, 30.4% were VA-only users, 51.5% were dual users, and 18.1% were Medicare-only users. Multivariate results show that greater likelihood of Medicare use was associated with older age, being white, being married, having higher education, having private insurance or Medicaid, having low VA priority level, and living in a nursing home or dying during the year. Higher comorbidities were associated with greater likelihood of dual use as opposed to any single system use. Alternatively, number of functional limitations was associated with greater likelihood of Medicare-only use and less likelihood of VA-only use. These results imply that different aspects of veterans’ needs have differential effects on where they seek care. Efforts to coordinate care between VA and Medicare providers are necessary to ensure that patients receive high-quality care, especially patients with multiple comorbidities.
Keywords: dementia, health services use, Medicare, veterans, longitudinal models
Approximately half (48.4%) of the 5.6 million Department of Veterans Affairs (VA) health system users are aged 65 and older and are eligible for Medicare.1 Because of the substantial health and policy implications, a number of recent studies have examined cross-system use, or dual use, of VA and Medicare.2–5 Most studies on dual use have been cross-sectional or, in a few studies, repeated cross-sectional.3,6 Consequently, it is not known whether and how patterns of dual use change over time.
Dual use may vary for different medical conditions and service types. For example, 28% of veterans who had VA primary care visits also reported non-VA primary care visits, but almost 70% of VA users hospitalized for acute myocardial infarction were initially hospitalized in Medicare hospitals.3,4 Dual users are vulnerable to the lack of coordination of care across systems that may result in underuse of appropriate care or excess use of care in either or both systems. These problems are likely to be greater for veterans with dementia because of the substantial challenges of navigating two healthcare systems while struggling with dementia. The prevalence of dementia in the elderly veteran population is similar to that of the general male population.7 Currently, there are an estimated 558,942 veterans with dementia, of them, 298,144 are VA enrollees, and 175,621 are VA patients. The number of VA patients with dementia is expected to peak at 218,017 in 2017.8 Although high health services use by patients with dementia is well documented, most studies have focused on Medicare use, and few have reported VA use.9–11 A recent study and summary data from the VA Dementia Registry provided a first glimpse of dementia patients’ use of VA health care, reporting an average annual per-patient cost of $19,522 to the VA in 1999.12,13 Although these studies fill the gap in knowledge about use of VA services for veterans with dementia, their lack of Medicare utilization data limited their usefulness. No research has systematically examined use of VA and Medicare services by veterans with dementia.
The research objectives of the current study were therefore to characterize healthcare use of veterans with dementia over a 4-year period and determine predictors of whether a veteran will be a VA-only user, dual user, or Medicare-only user. Data from VA and Medicare administrative files from a sample of elderly veterans clinically diagnosed with Alzheimer’s disease (AD) or vascular dementia (VAD) in the VA were used for the analysis.
METHODS
Study Design and Sample
The sample was drawn from the National Longitudinal Caregiver Study (NLCS), a national investigation of informal caregivers of elderly veterans clinically diagnosed with AD (International Classification of Diseases, Ninth Revision (ICD-9) 331.0) or VAD (ICD-9 290.4) in the VA. The institutional review board at the Durham VA Medical Center (VAMC), where the data were collected, approved the NLCS. The inclusion and exclusion criteria are fully described elsewhere.14,15 The NLCS dementia patient–care-giver dyads were followed annually with up to four mail surveys (1998–2001).
For the purposes of this study, exclusion criteria were (1) aged younger than 65 at the beginning of the study, to ensure Medicare eligibility during the entire study period (n = 132); (2) no VA or Medicare utilization data any time during the study period (n = 8); and (3) use of the VA primarily for pharmacy services, because such users have been shown to be less severely ill than other VA patients (n = 120).16 At baseline, the analysis sample consisted of 2,137 veterans. Because of patient deaths, the sample size for each succeeding year was 1,992 in 1999, 1,633 in 2000, and 1,300 in 2001. The analytical sample therefore contained 7,062 observations, for which the unit of observation is person-year.
Data Sources
To determine where veterans received their healthcare services, several sources of VA and Medicare data were merged. The VA Information Research Center (VIReC), a resource center of the VA Health Services Research and Development (HSR&D) Service, facilitated the merge of VA and Medicare data. VIReC maintains a crosswalk file that includes veterans’ Medicare Health Insurance Claim numbers, Social Security Numbers (SSNs), and scrambled SSNs. Under a data use agreement, VIReC provided Medicare data of the NLCS respondents. After VA and Medicare data were merged and analyses datasets were constructed for this study, data provided from the VIReC were destroyed. Identifiers in the analysis datasets were removed, so individuals can only be identified according to randomly assigned study identification numbers. The James J. Peters VAMC institutional review board approved the study protocol.
The VA Inpatient and Outpatient Medical SAS Data-sets were used to identify information on VA utilization.17 The Medical SAS Datasets contain patient-level records of use and full diagnostic and procedural information for each encounter. Medicare Standard Analytic Files (SAFs) were used to identify Medicare services and costs for all NLCS patients. Medicare SAFs are a set of public access files that contain demographic, utilization, and expenditure data at the individual level. The following SAFs were used in the analyses: inpatient, skilled nursing facility, outpatient, home health agency, carrier (physician or supplier), hospice, durable medical equipment, and Medicare Provider Analysis and Review files. VA data are stored according to federal fiscal year, and Medicare data are stored according to calendar year. VA and Medicare services use and costs were aligned into calendar year summaries using information on dates of service to make the different timeframes compatible.
Dependent Variable
Based on the annualized VA and Medicare inpatient and outpatient utilization data, patients were classified each year, in order of increasing Medicare reliance, into three use groups: VA only, dual use, and Medicare only. The combined VA-only and dual-use groups were considered to have some VA use and the combined dual-use and Medicare-only use groups to have some Medicare use.
Independent Variables
The following independent variables were examined using the conceptual framework developed in Andersen’s Behavioral Model of Health Services Use and from existing literature on health services use among veterans.6,18–24
Predisposing Characteristics
The following predisposing characteristics were examined: age, race (white, black, and other), education (<high school, high school graduate, some college, ≥college graduate), and marital status (married, widowed, other), all of which the caregivers reported in the NLCS. Missing values for patients’ race (~ 8%) were replaced with administrative data from the VA and Medicare following VIReC guidelines.25
Enabling Resources
The following enabling resources were examined: other health insurance (private insurance, Medicaid), geographic access to the VA, and VA priority level. Geographic access to the VA was measured using a straight-line distance between the location of the nearest VAMC and the centroid of the zip code of the veteran’s residence.26 Following previous studies,20,24 VA priority level was defined as a dichotomous variable indicating high (VA priority levels 1–6) or low (VA priority levels 7–8) priority. Veterans with high priority included those who had a service-connected disability or whose income was less than a VA-defined annual income threshold. Veterans with low priority included those whose income was higher than the income threshold and who agreed to pay specified copayments for services.
Need for Services
Comorbidities and functional impairment were examined as measures of patients’ need for services. Patients’ comorbidities were measured using a modified Older Americans Resources and Services comorbidity scale reported by the caregiver.27 Although diagnoses information is available in VA and Medicare data files, these were not used because of the likely presence of coding differences between the two systems. Patients’ functional impairment was measured according to the number of basic and instrumental activity of daily living (ADL) impairments reported by the caregiver,28,29 including difficulty walking several blocks, climbing a flight of stairs, dressing, walking across a room, bathing, eating, getting in and out of bed, using the toilet, managing money, and taking medicine. Dichotomous variables indicating whether the veteran was admitted to a nursing home or died in that year were also included.
Analysis
Following the literature, veterans were categorized into three use groups of increasing Medicare reliance.24,30 Because the proportional odds assumption required by ordered logit models were violated in a number of independent variables, the generalized ordered logit model was chosen for model estimation.31 The fit of the generalized ordered logit model was compared with that of the ordered logit models using log-likelihood ratio tests, and it was confirmed that the former model was a better fit for the data (P<.001).
Results from the generalized ordered logit model are similarly interpreted to the ordered logit model. For variables that do not violate the parallel regression assumptions and therefore have coefficient estimates constrained to be the same across equations, the interpretation is the same. For variables that violate the parallel regression assumptions, positive coefficients in each equation indicate that higher values on the independent variable increases the likelihood that the respondent will be in the higher category of the outcome than the current one, whereas negative coefficients indicate that higher values of the independent variable decrease the likelihood that the respondent will be in the higher category of outcome. Examination of the pattern of coefficients, particularly those that violated the parallel regression assumption and therefore differed across equations, may provide insights that would have been obscured or distorted in the ordered logit model.
In this analysis, two equations were estimated. The first equation compared the combined use groups of dual users and Medicare-only users with VA-only users. The second equation compared Medicare-only users with the combined use groups of VA-only users and dual users. In other words, the first equation compared some Medicare users to VA-only users, and the second equation compared Medicare-only users with some-VA users. Dichotomous variables for year were included to estimate changes in use group over time, and interactions between year and need factors were tested (comorbidities and functional limitations). To control for unobserved heterogeneity between Veterans Integrated Service Networks (VISNs), dichotomous variables were included for each of the 22 VISNs in which veterans resided. Odds ratios are reported for all parameter variables. Within-person correlations over time were modeled using Stata’s cluster options (StataCorp., College Station, TX).
RESULTS
Sample Characteristics Over Time
Table 1 reports descriptive characteristics of the sample. At baseline, the average patient was aged 77, white, and married and had 11 years of schooling. In addition to receiving VA care in the prior year and being eligible for Medicare, 21.9% of the patients also had private insurance, and 7.4% had Medicaid. The majority of the patients were in the high VA priority group (91.7%). Almost two-thirds (62.0%) of the patients had ADL limitations, with an average of three of seven ADL limitations. Patients had an average of five comorbidities, with depression, anxiety, or emotional problems (64.3%); arthritis (53.4%); and hypertension (48.3%) being the most prevalent. Patients who survived were younger, more likely to be married, less functionally limited, and less likely to have lived in a nursing home during the year than those who died during the study period (data not shown).
Table 1.
Sample Characteristics Over Time
| Characteristic | 1998 (n = 2,137) | 1999 (n = 1,992) | 2000 (n = 1,633) | 2001 (n = 1,300) |
|---|---|---|---|---|
| Age, mean ± SD | 77.0 ± 5.4 | 77.9 ± 5.4 | 78.7 ± 5.3 | 79.4 ± 5.3 |
| Race, % | ||||
| White | 80.8 | 80.9 | 80.9 | 80.7 |
| Black | 13.7 | 13.6 | 13.2 | 13.6 |
| Other | 5.5 | 5.5 | 5.9 | 5.7 |
| Years of schooling, mean ± SD | 11.0 ± 3.5 | 11.1 ± 3.5 | 11.0 ± 3.5 | 11.0 ± 3.5 |
| Years of schooling, % | ||||
| <12 | 46.9 | 46.5 | 47.0 | 47.6 |
| 12 | 30.3 | 30.3 | 30.2 | 29.4 |
| 13–15 | 10.4 | 10.5 | 10.5 | 10.4 |
| ≥16 | 12.4 | 12.6 | 12.3 | 12.6 |
| Marital status, % | ||||
| Married | 87.8 | 89.8 | 91.0 | 90.0 |
| Widowed | 7.6 | 6.1 | 5.6 | 6.8 |
| Other | 4.6 | 4.1 | 3.4 | 3.2 |
| Health insurance, % | ||||
| Private | 21.9 | 25.9 | 24.5 | 24.1 |
| Medicaid | 7.4 | 8.5 | 6.9 | 6.7 |
| Department of Veterans Affairs priority group, % | ||||
| 1–3 | 39.0 | 39.5 | 39.6 | 41.4 |
| 4–6 | 52.7 | 52.0 | 52.2 | 51.6 |
| 7–8 | 8.4 | 8.4 | 8.2 | 7.1 |
| Miles to nearest Veterans Affairs Medical Center, mean ± SD | 32.7 ± 34.8 | 32.9 ± 34.7 | 32.9 ± 34.8 | 33.3 ± 35.0 |
| Died, % | 6.8 | 16.5 | 20.3 | 18.9 |
| Lived in nursing home, % | 7.2 | 22.4 | 30.0 | 31.6 |
| Number of comorbidities, mean ± SD | 5.3 ± 2.9 | 6.1 ± 3.0 | 6.6 ± 3.2 | 7.0 ± 3.3 |
| Number of activity of daily living limitations, mean ± SD | 2.8 ± 2.6 | 2.9 ± 2.6 | 3.1 ± 2.6 | 3.2 ± 2.7 |
SD = standard deviation.
Proportion of Patients in Each Use Group Over Time
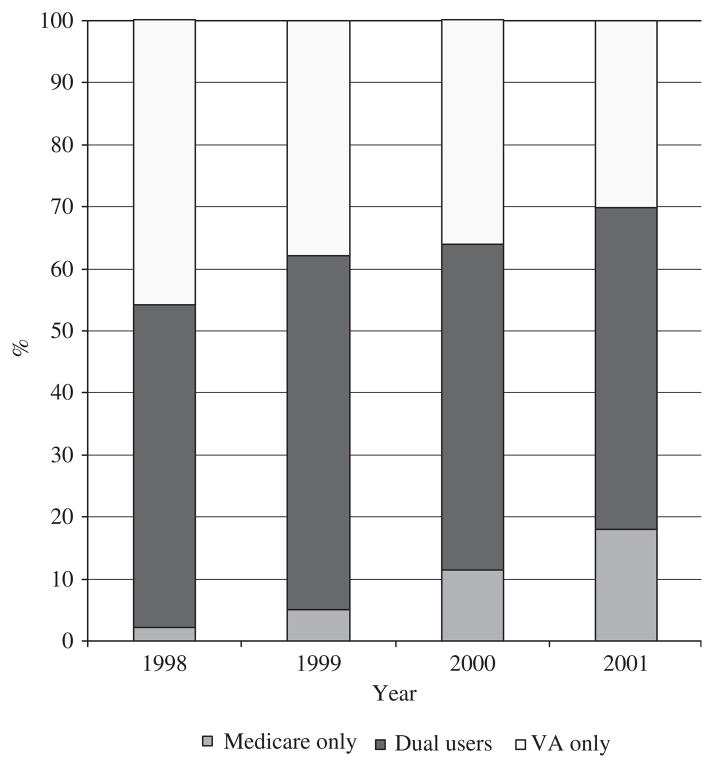
Figure 1 presents trends over time of the proportion of patients in each use group. During the 4-year study period, although the proportion of dual users remained relatively stable, the proportion of Medicare-only users increased, and the proportion of VA-only users declined steadily (P<.001). In 1998 (NLCS baseline), almost all patients were VA users: 41.7% were VA-only users, and 55.4% were dual users, and only 2.9% were Medicare-only users. By the end of the 4-year period, 30.4% were VA-only users, 51.5% were dual users, and 18.1% were Medicare-only users. The distribution of use group did not differ between those who survived the study period and those who died.
Figure 1.
Proportion of veterans with dementia in each user group over time.
Generalized Ordered Logistic Results of the Effects of Patient Characteristics on Use Group Over Time
Table 2 presents generalized ordered logit regression results of the effects of patient characteristics on use group over time.
Table 2.
Generalized Ordered Logistic Regression Results of the Effects of Patient Characteristics on Use Group Over Time
| Characteristic | Odds Ratio (95% Confidence Interval) P-Value | |
|---|---|---|
| Combined Medicare-Only and Dual-Use Group versus VA-Only Group | Medicare-Only Group vs. Combined Dual-Use and VA-Only Group | |
| Predisposing factors | ||
| Age (reference 65–74) | ||
| 75–84 | 1.28 (1.07–1.53) .006 | 1.28 (1.07–1.53) .006 |
| ≥85 | 1.35 (1.01–1.87) .06 | 1.35 (1.01–1.87) .06 |
| White = 1 | 1.31 (1.05–1.64) .02 | 1.31 (1.05–1.64) .02 |
| Married = 1 | 1.28 (1.00–1.68) .07 | 1.28 (1.00–1.68) .07 |
| Years of schooling | 1.04 (1.02–1.07) .001 | 1.04 (1.02–1.07) .001 |
| Enabling factors | ||
| Private insurance = 1 | 2.93 (2.43–3.53) <.001 | 2.93 (2.43–3.53) <.001 |
| Medicaid coverage = 1 | 1.32 (1.00–1.73) .046 | 1.32 (1.00–1.73) .046 |
| Department of VA priority level = low | 1.81 (1.30–2.53) <.001 | 5.04 (2.97–8.56) <.001 |
| Distance to nearest VA Medical Center, miles (reference <10) | ||
| 10–29 | 1.33 (1.07–1.66) .01 | 1.02 (0.98–1.03) .27 |
| 30–49 | 2.66 (2.07–3.42) <.001 | 0.92 (0.47–1.82) .82 |
| ≥50 | 3.19 (2.52–4.05) <.001 | 1.26 (0.71–2.22) .43 |
| Need factors | ||
| Number of comorbidities | 1.03 (1.01–1.05) .10 | 0.87 (0.81–0.94) <.001 |
| Living in a nursing home = 1 | 1.94 (1.47–2.54) <.001 | 1.94 (1.47–2.54) <.001 |
| Died = 1 | 2.37 (1.76–3.18) <.001 | 2.37 (1.76–3.18) <.001 |
| Number of ADL limitations | 1.17 (1.13–1.22) <.001 | 1.04 (0.94–1.14) .48 |
| ADL limitation × year | 0.97 (0.95–0.99) .01 | 1.05 (1.01–1.09) .02 |
| Year (reference 1998) | ||
| 1999 | 1.07 (0.93–1.22) .36 | 1.07 (0.93–1.22) .36 |
| 2000 | 1.04 (0.85–1.28) .70 | 1.04 (0.85–1.28) .70 |
| 2001 | 1.23 (0.93–1.63) .16 | 1.23 (0.93–1.63) .16 |
VA = Department of Veterans Affairs; ADL = activity of daily living.
Predicting Combined Medicare Only and Dual Use (Some Medicare Use)
In terms of predisposing factors, the likelihood of using some Medicare services (being in the combined Medicare-only and dual-use group) compared with using VA only was higher for veterans who were older (75–84: odds ratio (OR) = 1.28, 95% confidence interval (CI) = 1.07–1.53; ≥85: OR = 1.35, CI = 1.01–1.87, than for those aged 65 to 74), white (OR = 1.31, 95% CI = 1.05–1.64), married (OR = 1.28, 95% CI = 1.01–1.68), and had more years of schooling (OR = 1.04, 95% CI = 1.02–1.07). In terms of enabling factors, veterans with private insurance (OR = 2.93, 95% CI = 2.43–3.53), Medicaid (OR = 1.32, 95% CI = 1.00–1.73), and low VA priority level (OR = 1.81, 95% CI = 1.30, 2.53) were more likely to use some Medicare services. Veterans who lived further away from a VAMC were also more likely to use some Medicare services. Those who lived 10 to 29, 30 to 49, and 50 miles or more away were increasingly more likely than those who lived within 10 miles of a VAMC to use some Medicare services (OR = 1.33, 95% CI = 1.07–1.66; OR = 2.66, 95% CI = 2.07–3.42; and OR = 3.19, 95% CI = 2.52–4.05, respectively). In terms of need factors, the likelihood of using some Medicare services was higher for veterans with higher comorbidities (OR = 1.03, 95% CI = 1.01–1.06), those who lived in a nursing home during the year (OR = 1.94, 95% CI = 1.47–2.54), and those who died (OR = 2.37, 95% CI = 1.76–3.18). The likelihood of using some Medicare services at baseline was higher for those with more functional limitations (OR = 1.17, 95% CI = 1.13–1.22), although over time, the rate of increase in some Medicare use slowed, indicated by the OR of interaction between functional limitations and year (OR = 0.97, 95% CI = 0.95–0.99).
Predicting Medicare-Only Use
None of the predisposing factors violated the proportional odds assumption, indicating that these variables have the same effect on the likelihood of using Medicare-only and using some VA services (being in the combined dual-use and VA-only group) as their effects on the likelihood of using some Medicare services (being in the combined Medicare-only and dual-use group) and using VA only. That is, the likelihood of using Medicare only was higher than the likelihood of using some VA services for veterans who were older and white and had more years of schooling. In terms of enabling factors, the insurance variables did not violate the proportional odds assumption between the equations either. That is, veterans with private insurance and Medicaid were more likely to use Medicare only. The estimated ORs on variables related to access to the VA were in the same direction but with substantially different magnitudes. Specifically, veterans with low VA priority level were approximately five times as likely to use Medicare only as those with high VA priority levels (OR = 5.04, 95% CI = 2.97–8.56), but distance from the veteran’s residence to the nearest VAMC were not statistically significant. In terms of need factors, all of the variables violated the proportional odds assumption except for living in a nursing home or dying. Specifically, the likelihood of using Medicare only was lower for veterans with higher comorbidities (OR = 0.87, 95% CI = 0.81–0.94). At baseline, functional limitations did not affect the likelihood of using Medicare only, although over time, the likelihood of using Medicare only increased as veterans became more functionally limited (OR = 1.05, 95% CI = 1.01–1.09).
DISCUSSION
This study examined longitudinal patterns of use of VA and Medicare services for a sample of veterans with dementia who were prior VA users. By following the veterans for up to 4 years, results from this study permit patterns of where veterans obtain health care to be more accurately described. Comparable with rates reported in recent studies, this study found that more than half of the veterans in the sample also used Medicare.24 Because the sample was selected from veterans who were VA users in 1997, fewer than 3% relied on Medicare only at the beginning of the study period. During the 4-year study period, Medicare-only use increased substantially, and VA-only use decreased substantially. By the end of the 4-year study period, almost one-fifth of patients in the sample had become Medicare-only users.
The reason for increasing reliance on Medicare in this sample of veterans with dementia is unclear. If there is a constant proportion of veterans switching use groups each year, a year-by-year increase in the Medicare-only group would be expected for a number of years before a steady state is reached, because the study sample was drawn from veterans who used VA services during the year before study enrollment and therefore would only include dual users or VA-only users at baseline. However, an analysis of whether there is a steady state of proportions of veterans in each use group and the proportion of veterans that may switch from one group to another was beyond the scope of this analysis.
If the choice of where to obtain care depends on veterans’ and system-wide characteristics, then the analysis sheds light on which variables these might be and how they affect veterans’ choices. Several results from this analysis are of note. First, the coefficients on the number of comorbidities had opposite effects across equations; that is, number of comorbidities was associated with greater likelihood of belonging to the combined Medicare-only and dual-use group than to the VA-only group but was associated with lower likelihood of belonging to the Medicare-only group than to the combined dual-use and VA-only group. This suggests that a greater number of comorbidities was associated with greater likelihood of dual use as opposed to single-system use. Nevertheless, although the number of functional limitations was associated with greater likelihood of belonging to the combined Medicare-only and dual-use group than to the VA-only group, suggesting less VA-only use, the opposite effect across equations for the interaction term of the number of functional limitations and year suggests that the decreases in VA-only use were associated with increases in Medicare-only use. These results together imply an unmet need for services among these veterans. The strong relationship between comorbidities and the higher likelihood of dual use suggests that efforts to coordinate care between VA and Medicare providers are necessary to ensure that patients receive high-quality care, especially patients with multiple comorbidities. The differences in the effects of comorbidities and functional limitations on use group suggest that different aspects of veterans’ needs have differential effect on where veterans seek care.
Second, results from this analysis show that enabling resources (e.g., private insurance, VA priority level) strongly predict which system veterans seek care in. In particular, one of the strongest predictors of Medicare-only use was veterans’ VA priority level. This demonstrates that changes in one system may affect demand for care in the other system. Although other factors may influence where veterans seek care, the analyses were restricted to variables available in administrative data sets. Studies on other diseases show that the VA provided less specialty care, such as angioplasty, because of limited on-site availability of cardiac procedures in the VA healthcare system.32 Studies also have shown that Medicare-eligible VA users were increasingly hospitalized in Medicare hospitals for acute myocardial infarction.3 Although distance from the nearest VAMC was controlled for, access to VA services because of geographic and logistic difficulties remain. Perhaps, as dementia worsens, patients experiencing a lack of specialty care in the VA (e.g., access to neurologists or specific rehabilitation services) increase their use of healthcare services outside the VA. Future studies will examine whether differences in the availability of specialty care exist for dementia care.
There are several limitations of the study. First, as mentioned before, because the study sample was drawn from elderly U.S. veterans with dementia who had used VA services during the year before study enrollment, the sample may not be representative of all veterans with dementia who were eligible for Medicare and VA services. A study that compared the characteristics of VA users and veterans who did not use VA services showed that VA users were older, less educated, and in poorer health.33 The sample of previous VA users therefore provides insights into patterns of healthcare use in a more-vulnerable segment of veterans with dementia. Starting from a sample of VA users also is relevant to VA administrators as they consider budget and resources plans. Second, in this study overall patterns of VA and Medicare services use were examined. Use of specific types of VA and Medicare services may be different from overall patterns. Future work will examine how patients use specific types of services over time in more detail. Third, there have been important secular changes in VA eligibility criteria and Medicare reimbursement policies since this study. For example, Medicare Part D may have changed the context for dual VA–Medicare use in recent years. Future studies that examine VA–Medicare use will take these policies changes into account.
This is the first study to examine longitudinal patterns of use of VA and Medicare services for veterans with dementia. For planning purposes, it is important for health-care systems to know prospectively where their patients will probably be seeking care. There also may be quality-of-care implications for knowing where patients seek health care if misallocation of resources leads to reductions in or elimination of services. More importantly, for patients with dementia and other chronic conditions, coordinated efforts between the VA and Medicare are necessary to ensure that patients receive high-quality care.
Acknowledgments
This project was supported by VA HSR&D IIR 05-114 (PI Zhu). Drs. Zhu, Penrod, and Ross also are supported by VA HSR&D TRP-02-149. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Sponsor’s Role: The sponsor had no role in the study or writing of the manuscript.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Study concept and design: Zhu, Penrod, Ross, Sano. Acquisition of data: Zhu, Dellenbaugh. Analysis and interpretation of data: Zhu, Dellenbaugh, Penrod, Ross. Drafting of the manuscript: Zhu. Critical revision of the manuscript for important intellectual content: Penrod, Ross, Sano. Statistical analysis: Zhu, Dellenbaugh. Administrative, technical, or material support: Zhu. Study supervision: Zhu.
References
- 1.Department of Veterans Affairs Strategic Plan FY2006–2011. Washington, DC: Office of the Secretary; 2006. [Google Scholar]
- 2.Wright SM, Daley J, Fisher ES, et al. Where do elderly veterans obtain care for acute myocardial infarction: Department of Veterans Affairs or Medicare? Health Serv Res. 1997;31:739–754. [PMC free article] [PubMed] [Google Scholar]
- 3.Wright SM, Petersen LA, Lamkin RP, et al. Increasing use of Medicare services by veterans with acute myocardial infarction. Med Care. 1999;37:529–537. doi: 10.1097/00005650-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Borowsky SJ, Cowper DC. Dual use of VA and non-VA primary care. J Gen Intern Med. 1999;14:274–280. doi: 10.1046/j.1525-1497.1999.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hynes DM, Stroupe KT, Greer JW, et al. Potential cost savings of erythropoietin administration in end-stage renal disease. Am J Med. 2002;112:169–175. doi: 10.1016/s0002-9343(01)01103-2. [DOI] [PubMed] [Google Scholar]
- 6.Weeks WB, Bott DM, Lamkin RP, et al. Veterans Health Administration and Medicare outpatient health care utilization by older rural and urban New England veterans. J Rural Health. 2005;21:167–171. doi: 10.1111/j.1748-0361.2005.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 7.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29:125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. [Accessed February 10, 2009];VHA Office of the Assistant Deputy Under Secretary for Health for Policy and Planning VA Dementia Projections 2002–2022 [on-line] Available at http://www1.va.gov/vhareorg/reports.htm.
- 9.Gutterman EM, Markowitz JS, Lewis B, et al. Cost of Alzheimer’s disease and related dementia in managed-Medicare. J Am Geriatr Soc. 1999;47:1065–1071. doi: 10.1111/j.1532-5415.1999.tb05228.x. [DOI] [PubMed] [Google Scholar]
- 10.Taylor DH, Jr, Sloan FA. How much do persons with Alzheimer’s disease cost Medicare? J Am Geriatr Soc. 2000;48:639–646. doi: 10.1111/j.1532-5415.2000.tb04721.x. [DOI] [PubMed] [Google Scholar]
- 11.Bynum JP, Rabins PV, Weller W, et al. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52:187–194. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- 12.Yu W, Ravelo A, Wagner TH, et al. Prevalence and costs of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(3 Suppl):146S–167S. doi: 10.1177/1077558703257000. [DOI] [PubMed] [Google Scholar]
- 13.Office of Geriatrics and Extended Care and VA Central Office. [Accessed October 10, 2007.];VA Dementia Registry. 2004 [on-line]. Available at http://www.va.gov/geriatricsshg/docs/DementiaCodesRegistry4-2-04.xls.
- 14.Moore MJ, Zhu CW, Clipp EC. Informal costs of dementia care: Estimates from the National Longitudinal Caregiver Study. J Gerontol B Psychol Sci Soc Sci. 2001;56B:S219–S228. doi: 10.1093/geronb/56.4.s219. [DOI] [PubMed] [Google Scholar]
- 15.Zhu C, Moore M, Clipp E. Dementia problem behavior and the production of informal caregiving services. J Econ Household. 2003;1:59–76. [Google Scholar]
- 16.Zhu S, Gardner J, Hendricks A. Health Care Financing and Economics Data Brief #2004-10. VA Boston Health Care System Research and Development; Boston: 2004. How many enrollees come to VA just for pharmacy? [Google Scholar]
- 17.Hynes DM, Joseph G, Pfeil C. Using Vista data for research. VIReC Insights. 2002;3:1–8. [Google Scholar]
- 18.Burgess JF, Jr, DeFiore DA. The effect of distance to VA facilities on the choice and level of utilization of VA outpatient services. Soc Sci Med. 1994;39:95–104. doi: 10.1016/0277-9536(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 19.General Accounting Office Veterans Health Care: Use of VA Services by Medicare Eligible Veterans. Washington, DC: Government Printing Office; 1994. [Google Scholar]
- 20.General Accounting Office Progress and Challenges in Providing Care to Veterans. Washington, DC: Government Printing Office; 1999. [Google Scholar]
- 21.Mooney C, Zwanziger J, Phibbs CS, et al. Is travel distance a barrier to veterans’ use of VA hospitals for medical surgical care? Soc Sci Med. 2000;50:1743–1755. doi: 10.1016/s0277-9536(99)00414-1. [DOI] [PubMed] [Google Scholar]
- 22.Shen Y, Hendricks AM, Zhang S, et al. VHA enrollees’ health care coverage and use of care. Med Care Res Rev. 2003;60:253–267. doi: 10.1177/1077558703060002007. [DOI] [PubMed] [Google Scholar]
- 23.Hynes DM, Cowper D, Manheim L, et al. Report to the Undersecretary of Health Department of Veterans Affairs. VA Information Resource Center; 2003. [Accessed February 10, 2009.]. Research Findings from the VA Medicare Data Merge Initiative: Veterans Enrollment, Access and Use of Medicare and VA healthcare. [on-line]. Available at http://www.virec.research.va.gov/DataSourcesName/VA-MedicareData/USHreport.pdf. [Google Scholar]
- 24.Hynes DM, Koelling K, Stroupe K, et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care. 2007;45:214–223. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- 25.VA Information Resource Center (VIReC) [Accessed February 10, 2009.];Researchers’ Guide to VA Data: Data Issues Brief. 2004 March; [on-line]. Available at http://www.virec.research.va.gov.
- 26.FY2002 Geographic Access to Veterans Health Administration Services. Washington, DC: Veterans Health Administration Office, Department of Veterans Affairs; 2002. [Google Scholar]
- 27.Fillenbaum G. Multidimensional Functional Assessment of Older Adults. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 28.Katz S, Ford A, Moskowitz R, et al. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. AMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 29.Nagi S. An epidemiology of disability among adults in the United States. Millbank Memorial Fund Q. 1976;54:439–467. [PubMed] [Google Scholar]
- 30.Williams R. Generalized ordered logit/partial proportional odds models for ordinal dependent variables. Stata J. 2006;6:58–82. [Google Scholar]
- 31.Long J, Freese J. Regression Models for Categorical Dependent Variables Using Stata. 2. College Station, TX: Stata Press; 2006. [Google Scholar]
- 32.Petersen LA, Normand SL, Leape LL, et al. Regionalization and the underuse of angiography in the Veterans Affairs Health Care System as compared with a fee-for-service system. N Engl J Med. 2003;348:2209–2217. doi: 10.1056/NEJMsa021725. [DOI] [PubMed] [Google Scholar]
- 33.Liu CF, Maciejewski ML, Sales AE. Changes in characteristics of veterans using the VHA health care system between 1996 and 1999. Health Res Policy Syst. 2005;3:5. doi: 10.1186/1478-4505-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]