Abstract
One of the current standard treatment options for younger patients with stable traumatic vertebral fractures is conservative treatment using braces. Kyphoplasty as a minimally invasive procedure has been shown to be effective in stabilizing vertebral body fractures, resulting in immediate pain relief and improved physical function. The purpose of this prospective study was to clarify whether patients with acute traumatic vertebral fractures benefit more from kyphoplasty or from conservative treatment with a brace. A prospective study was undertaken in two centers. Forty patients with acute painful traumatic vertebral body fractures type A1–A3 (AO-classification) after adequate trauma, without osteoporosis, suitable for kyphoplasty or therapy by brace were included into the study. Follow-up was 12 months. Patients of the kyphoplasty group showed an immediate beneficial and significant effect postoperatively, and better outcomes 1 and 3 months after operation compared to the conservatively treated group in pain feeling, mobility and vertebral body height. After 12 months the difference between both groups was not significant excepting the vertebral body height. Kyphoplasty provides early and lasting reduction of pain and improvement of daily activity. However, there are clinically asymptomatic cement leakages in up to 45% of which we do not know the consequences in long term. Every patient with traumatic vertebral body fracture treated by kyphoplasty has to be informed about that. Long-time results are outstanding and our findings require confirmation by randomized controlled trials.
Keywords: Kyphoplasty, 3-Point-brace, Traumatic vertebral fracture, Comparison, Resorbable cement
Introduction
Various opinions exist regarding the ideal management of thoracolumbar Type A spine fractures without neurologic deficit. Both operative and nonsurgical approaches are advocated. Current standard treatment options for younger patients with traumatic vertebral fractures include conservative treatment with braces, analgetic medication and physiotherapy. Braces keep patients mobile and have little or no side effects apart from being uncomfortable but controlled prospective trials showing effectiveness and patient benefit of braces are rare [9, 13, 14]. Surgical treatment can be performed openly or minimally invasive using balloon-kyphoplasty or vertebroplasty. Balloon-kyphoplasty has been shown to be effective in stabilizing osteoporotic vertebral body fractures, resulting in immediate pain relief and improved physical function [1, 5, 16]. Since 2001 a resorbable calcium phosphate cement has made it possible to use this method in younger patients with osteoporotic vertebral fractures with good results [3]. This study compares the effectiveness of both kyphoplasty and treatment with a brace in younger patients with traumatic non-osteoporotic vertebral fractures. The purpose of this prospective study was to clarify whether patients with acute traumatic vertebral fractures benefit more from kyphoplasty or from conservative treatment with a brace. Outcome was measured using several functional, clinical and morphological tests.
Materials and methods
A clinical prospective non-randomized study was performed in two centers. The study population consisted of 40 consecutive patients without osteoporosis, with painful traumatic vertebral body fractures (AO type A) presenting at the emergency department of the University of Heidelberg (Department of Trauma Surgery and Department of Orthopaedic Surgery) from October 2003 to February 2007.
Inclusion and exclusion criteria
Patients with acute painful traumatic vertebral body fractures type A1–A3 (AO-classification) after adequate trauma were included into the study. Evaluation of suitability for kyphoplasty and conservative treatment was performed in all patients as follows: an interdisciplinary team consisting of trauma surgeons and radiologists analyzed the radiological status of each patient to ensure that kyphoplasty was technically feasible and that treatment with a brace was possible. Patients with osteoporosis (as detected by DXA-scan), allergy against cement components, acute infection, complete burst fractures or neurological deficits due to the fracture were excluded. Patients were informed of the experimental character of the study, risks and benefits of kyphoplasty and conservative management. Based on this informed consent patients were selected into kyphoplasty (Department of Trauma Surgery) or conservative treatment groups (Department of Orthopaedic Surgery).
Interventions
All participants received adequate analgetic medication and physiotherapy. Twenty patients were treated non-operatively with a brace, 20 patients were treated with balloon-kyphoplasty within 7 days after the fracture occurred. Kyphoplasty was performed bitranspedicularly according to standard procedure protocol. A resorbable osteoconductive calcium phosphate cement (Calcibon; Biomet Merck, Darmstadt, Germany) was used. Earlier studies had shown a feasibility of this cement in the use of kyphoplasty, its osseous integration and a very slow rate of resorption [8].
The kyphoplasty patients were discharged within 2–4 days after intervention. In case of non-operative treatment a 3-point-brace (3-point-brace, Teufel, Germany) was fitted on each patient and the patient was then mobilized. These patients were discharged 3–5 days after commencement of therapy.
Follow-up
The follow-up period was 12 months. Patients were examined before and 1, 3, 6 and 12 months after commencement of treatment. Pain was evaluated using the visual analogue scale (VAS). Functional criteria and patient satisfaction were evaluated using the Hannover-VAS-Spine score that has been validated for patients with spinal injuries [7]. Midline vertebral height and kyphosis angle were measured on lateral X-rays of the spine according to standard morphological analysis [12, 15].
Statistical analysis
All data were analyzed using SPSS for Windows 13.0 statistical software (SPSS Inc., Chicago, IL, USA). For the multivariate analysis the ANOVA-modelling with repetitive measurement was used. Categorical data were analyzed with the χ2 test. A p value of <0.05 was considered significant.
Results
Forty patients with 42 traumatic vertebral fractures classified as type A1–A3-fractures (AO) were included in the study. Twenty patients received kyphoplasty, 20 patients were treated with a brace. Twenty patients of each group were available for follow-up. Of all patients 27 were male and 13 female aged 18–63 years (median: 38 years). All fractures were localized in the thoraco-lumbar region between Th 11 and L 5 with a maximum at Th 12 and L 1.
The amount of cement injected into one vertebral body was 3–8 ml (median: 5.3 ml).
Baseline characteristics
There was no statistically significant difference between patient characteristics and morphometric measures between both groups at baseline.
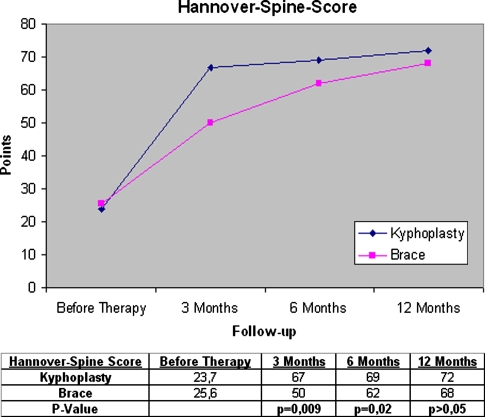
Hannover-VAS-Spine score
In both groups there was a statistically significant improvement of pain and mobility immediately and up to 6 months after commencement of therapy. Patients of the kyphoplasty group showed an immediate beneficial effect postoperatively, and better outcomes 1 month and 3 months after operation compared to the conservatively treated group (p < 0.05, Table 1). After 12 months the difference between both groups was not significant.
Table 1.
Hannover-Spine score
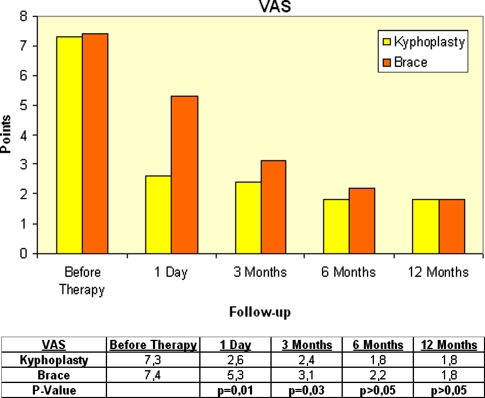
Pain perception (VAS)
Postoperatively, at 3 months and also at 6 months follow-up, the kyphoplasty group showed a significantly better improvement of total VAS compared with the brace group (Table 2).
Table 2.
Visual analogue scale
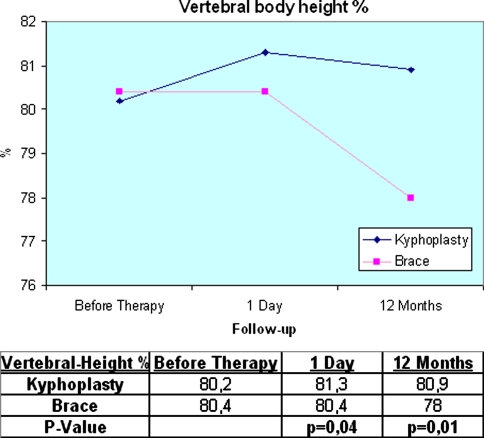
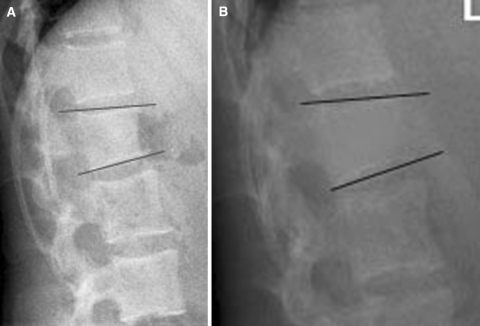
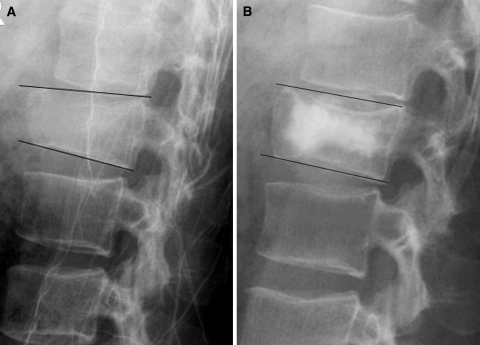
Midline vertebral height and kyphosis angle
Vertebrae treated by kyphoplasty exhibited a postoperative improvement of vertebral height and a relatively constant kyphosis angle during follow-up, while there was a significant increase of the kyphosis angle in the group treated by brace after 12 months (Table 3; Figs. 1, 2) indicating a loss of vertebral height. The loss of midline vertebral height (loss of restoration) was also significantly lower (p < 0.05) in the kyphoplasty group.
Table 3.
Vertebral body height in %
Fig. 1.
A 26-year-old female treated by brace. a Before therapy; b 12 months after therapy
Fig. 2.
A 45-year-old male treated by kyphoplasty. a Before kyphoplasty; b 12 months after kyphoplasty
Complications and adjacent fractures
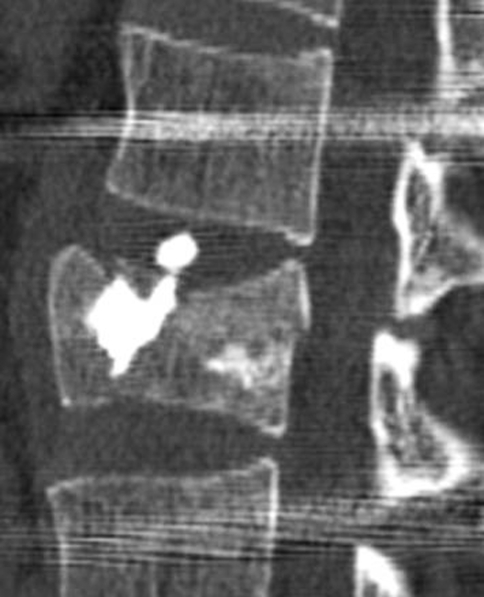
There were no complications in the group treated with braces. Patients with kyphoplasty showed clinically asymptomatic cement leakages in 9 of 20 cases (45%), only diagnosed in routine postoperative CT scans (Fig. 3). There were no neurological, embolic or cardiovascular problems during or after operation. During the time of follow-up no new adjacent or non-adjacent vertebral fractures were detected in either group.
Fig. 3.
Cement leakage after kyphoplasty in CT-scan
Discussion
Younger patients with traumatic vertebral fractures without neurological deficits are often treated conservatively by using braces or surgically invasive methods using an open procedure. Kyphoplasty as a minimally invasive procedure has been shown to be effective and safe in stabilisation of vertebral fractures, resulting in immediate pain relief and improved physical function [1, 6, 14, 16]. This technique is commonly used for treatment of osteoporotic vertebral fractures. Traumatic vertebral fractures without osteoporosis have not yet been treated with kyphoplasty routinely. Invention of injectable calcium phosphate cements with the potential of being resorbed and replaced by newly formed bone tissue; present a promising alternative for PMMA in younger patients [3, 5]. The calcium phosphate cement used in this study had shown good results in previous clinical trials, particularly no signs of early resorption. The handling presents certain difficulties due to the cement’s immediate hardening so we do not recommend its use without a certain amount of practice. It should be mentioned that the kyphoplasty procedure itself in a patient with normal bone density should be done by a surgeon with extensive experience, as the placement of the cannulas and the balloon pressure needed to achieve a restoration of height in normal bone can differ widely from osteoporotic fractures. Calcium phosphate cement should never be used in more unstable fractures (AO type A3.3 or B and C-fractures) because it is more vulnerable to shear and bending forces as PMMA. Kyphoplasty has in the past been suspected to induce new adjacent vertebral fractures due of the increased strength of the stabilized vertebral body [10, 12–14]. However, during the time of follow-up in these young patients with normal bone density we did not see new vertebral body fractures in either treatment group. Our results indicate a benefit of kyphoplasty over braces particulary in the first 6 months after intervention because of the immediate occurrence of pain reduction and improvement of mobility. Thus allowing the patient an early return to a normal lifestyle. Patient satisfaction was significantly better during the first 6 months after kyphoplasty compared to conservative treatment. In times of high unemployment rates these aspects may not be unimportant.
Several earlier reports show a substantial height restoration of 15–65% of the fractured vertebrae after kyphoplasty in patients with osteoporotic fractures [4, 15, 16]. In our study the average height restoration in the kyphoplasty patients was only 2.2%. This difference is most likely due to the difference in bone structure and strength between normal healthy and osteoporotic bone. Inflation of kyphoplasty balloons inside a traumatically fractured vertebra is remarkably more difficult and higher pressure levels are needed to achieve any effect. However, the internal stabilisation of the fracture seems to have a pain relieving effect by itself. The patients in this study also had significantly less back pain after kyphoplasty even though there was only a slight improvement of vertebral body height. However, 12 months after initiation of treatment both groups displayed no difference in the pain scores, even though the group treated with brace showed a significant loss of the vertebral body height compared to the group treated by kyphoplasty (Table 3). While kyphoplasty may not be able to restore original vertebral body height, it seems to at least be able to conserve an acceptable height and prevent further loss of height. It is yet unclear whether the more anatomical morphometry after kyphoplasty will even prove to be an advantage for the spinal balance when these patients get older. Even though remarkable height restoration was not achieved we do not recommend the use of vertebroplasty in these traumatic fractures. Our study showed a much higher rate of cement leakages compared to other publications. This is due to the nature of these traumatic fractures. The cement leaks through the many fracture cracks. We suspect that this effect would be much more dramatic when using vertebroplasty for these fractures as the cement would be pressed into the vertebra without a preformed cavity using even higher pressure as done in kyphoplasty.
The main limitation of this study was its nonrandomized design. However, we did not observe differences in baseline characteristics between the two groups.
In summary this prospective, nonrandomized study supports the use of kyphoplasty in addition to non-operative analgetic therapy as an effective method to improve and stabilize vertebral deformities due to acute trauma. Kyphoplasty provides early and lasting reduction of pain and improvement of daily activity. However, there are clinically asymptomatic cement leakages in up to 45% of which we do not know the consequences in the long term but which may as well be absorbed. Long-term results and the effects of kyphoplasty in this group of patients are outstanding and our initial findings require further confirmation by larger randomized long-term controlled trials.
References
- 1.Atalay B, Caner H, Gokce C, Altinors N. Kyphoplasty: 2 years of experience in a neurosurgery department. Surg Neurol. 2005;64(2):72–76. doi: 10.1016/j.surneu.2005.07.039. [DOI] [PubMed] [Google Scholar]
- 2.Braun W, Markmiller M, Ruter A. Conservative therapy of fractures of the thoracic and lumbar spine Indications, treatment regimen, results. Chirurg. 1991;62:404408. [PubMed] [Google Scholar]
- 3.DaFonseca K, Baier M, Grafe I, Libicher M, Noeldge G, Kasperk C, et al. Balloon kyphoplasty in the therapy of vertebral fractures. Orthopade. 2006;35(10):1101–1109. doi: 10.1007/s00132-006-1005-z. [DOI] [PubMed] [Google Scholar]
- 4.Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, et al. Contribution of vertebral deformities to chronic back pain and disability The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1992;7:449456. doi: 10.1002/jbmr.5650070413. [DOI] [PubMed] [Google Scholar]
- 5.Jarvik JG, Kallmes DF, Deyo RA. Point of view: Kyphoplasty: more answers more questions? Spine 1. 2006;31(1):65–66. doi: 10.1097/01.brs.0000192686.23902.06. [DOI] [PubMed] [Google Scholar]
- 6.Kasperk C, Hillmeier J, Nöldge G, Grafe IA, Da Fonseca K, Raupp D, et al. Treatment of painful vertebral fractures by Kyphoplasty with primary osteoporosis: a prospective nonrandomized controlled study. JBMR. 2005;20:604–613. doi: 10.1359/JBMR.041203. [DOI] [PubMed] [Google Scholar]
- 7.Knop C, Oeser M, Bastian L, Zdichavsky M, Blauth M. Development and validation of the VAS spine score. Unfallchirurg. 2001;104:48–497. doi: 10.1007/s001130170111. [DOI] [PubMed] [Google Scholar]
- 8.Libicher M, Hillmeier J, Liegibel U, Sommer U, Pyerin W, Vetter M, et al. (2006) Osseous integration of calcium phosphate in osteoporotic vertebral fractures after kyphoplasty: initial results from a clinical and experimental pilot study. Osteoporos Int [DOI] [PubMed]
- 9.Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:16311638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 10.Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285:320323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 11.Lin JT, Lane JM. Nonmedical management of osteoporosis. Curr Opin Rheumatol. 2002;14:441446. doi: 10.1097/00002281-200207000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, et al. Quality of life in patients with vertebral fractures: Validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporos Int. 1999;10:15016. doi: 10.1007/s001980050210. [DOI] [PubMed] [Google Scholar]
- 13.Patwardhan AG, Li SP, Gavin T, Lorenz M, Meade KP, Zindrick M. Orthotic stabilization of thoracolumbar injuries. A biomechanical analysis of the Jewett hyperextension orthosis. Spine. 1990;15:654661. doi: 10.1097/00007632-199007000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Pfeifer M, Begerow B, Minne H. Effects of a new spinal orthosis on posture, trunk strength, and quality of women with postmenopausal osteoporosis: A randomized trial. Am J Phys Med Rehabil. 2004;83:177186. doi: 10.1097/01.PHM.0000113403.16617.93. [DOI] [PubMed] [Google Scholar]
- 15.Taylor RS, Fritzell P, Taylor RJ (2007) Ballon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J 16(8):1085–1100 [DOI] [PMC free article] [PubMed]
- 16.Voggenreiter G. Baloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30(24):2806–2812. doi: 10.1097/01.brs.0000190885.85675.a0. [DOI] [PubMed] [Google Scholar]