Abstract
Intramedullary spinal cord abscess (ISCA) in children is extremely a rare infection of the central nervous system (CNS); and probably a devastating neurological condition. Clinical awareness of patients at risk is crucial for early diagnosis and intervention; as this entity is one of the treatable conditions of paraparesis. Association with congenital neuro-ectodermal abnormality in children is frequent. This pathology highlights the importance of complete neurological checks of infants as a part of their routine physical examination and early management of patients with congenital dermal sinus, prophylactic surgical resection of such a congenital anomaly is recommended by most authors to prevent serious infections of the CNS. However, once the abscess is established; immediate surgical drainage along side adequate antibiotics should be instituted. This may guarantee improving neurological outcome. In this communication, the authors present their experience with four cases of ISCA in children treated successfully with surgical drainage, intravenous antibiotics and neuro rehabilitation between 2001 and 2006 and discuss their results. We concluded that early diagnosis and treatment is essential; before a devastating mechanico-vascular insult of the spinal cord is established from rapid formation of the abscess and a swift expansion of the spinal cord within the limited intraspinal space.
Keywords: Intramedullary spinal cord abscess, Dermal sinus, Myelotomy, Staphylococcus aureus
Introduction
Intramedullary spinal cord abscess (ISCA) is a well recognized and rare entity. It was first described by Hart [13]. Dermal sinus tract, which results from the incomplete partition of epithelial ectoderm and neuroectoderm in the early fetal life, is to be implicated as a source of this pathology in children, it can end anywhere along its tract within the spinal canal compartments and becomes a potential route for spread of infection. Spinal cord abscess may involve any part of the spinal cord but the thoraco-lumbar spine is the most frequent site; however; holocord abscess may occur but it is less common [8, 11, 21]. Clinical suspicion and radiological findings are essential for early diagnosis and treatment; consequently, irreversible spinal cord damage can be avoidable. In children, limited laminectomy with myelotomy focused above the most bulbous segment of the spinal cord for drainage of the abscess and adequate antibiotics is the treatment of choice [1–5, 7].
Case report 1
In August 2006, an 8-month-old girl referred to our services with fever, rapid progressive leg weakness and continuous soiling of the napkins over the past 2 days. Her mother first observed an upper anal cleft opening with occasional discharge at the age of 2 months but no medical care received. On examination, the child was restless, her temperature was at 38.5. There was an upper anal cleft dimple and opening with some crust. The bladder was palpable and her anal tone was weak and had no anal reflex. Upper limbs were normal, whereas the lower extremities were flail and hypotonic with observed no movement. She had no tendon reflexes elicited. There was no response to stimuli till T7/8 level.
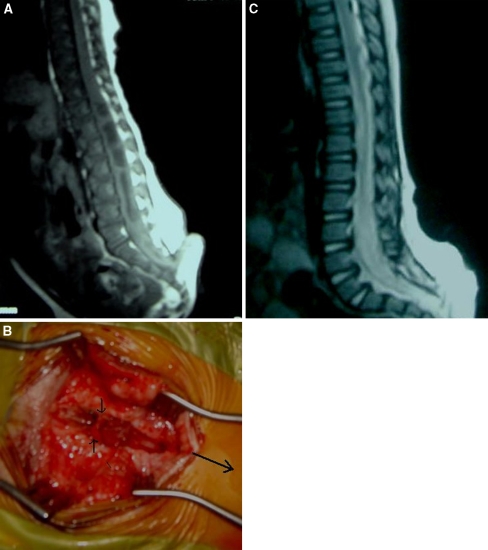
The MR imaging study demonstrated a swollen spinal cord with the intramedullary septated cystic lesion and rim enhancement extending from the low inserted conus medullaris at L5 level to T 11. There was a dermal sinus tract connected the skin to the thecal sac (Fig. 1a).
Fig. 1.
a MR sagittal T1 W with gadolinium of the thoraco-lumber spine of showing an enhancing intramedullary a septated cystic cavity with minimal enhancement extends from the low inserted spinal cord to T11. The dermal sinus tract is demonstrated clearly connecting the skin to the spinal cord. b Intraoperative photo of the dermal tract as it is attached to the thecal sac. (2 small arrows is the dermal sinus; long arrow is the direction of head). c Postoperative sagittal MRI scan of the lumber spine showed a total resolution of the abscess; the spinal cord is still low inserted
The child underwent an urgent surgical intervention within a few hours of her presentation. L3–5 laminectomy was then affected. Tracing the dermal tract from skin, it was attached to the thecal sac and extended through it (Fig. 1b). Using the microscope, the tense dura was opened above and below the dermal sinus and reflected. However, the swollen spinal cord herniated through the durotomy. The dermal sinus, which was attached to the lower end of the conus, was dissected gently and then separated from the neural tissue. A 2 cm myelotomy was then made at L3/4 level the site of most intense area; a significant amount of viscous purulent fluid ran out. Then, a no. 6 French, pediatric feeding tube was inserted through the myelotomy; it was gently and slowly advanced rostrally until T11 level to communicate between the septated cavities; the length of advancement of the tube was calculated based on the extension of the lesion on MRI. With gentle aspiration more purulent material was aspirated. Copious irrigation with warm normal saline was then applied. The tension within the spinal cord relieved. The dura was then closed in a watertight fashion, as was the wound.
The patient commenced intravenous vancomycin and tazocin. Evaluation of Gram-stain revealed numerous positively stained cocci. Cultures of blood and the pus aspirate were positive for Staphylococcus aureus. This was sensitive to vancomycin; while tazocin discontinued. Although it was clearly that the infection related to the dermal sinus; the checks for TB and Brucella were negative.
Postoperatively, the patient became afebrile and started to have some movements in her legs from day 4. The leg strength continues to improve steadily. Two weeks later, the child was able to move her legs spontaneously but still had visible residual weakness. Antibiotics ceased after 6 weeks and she was sent for neuro-rehabilitation. The postoperative MRI spine revealed a full resolution of the abscess (Fig. 1c).
The child displayed a significant neurological improvement on the regular assessment as an outpatient for nearly 24 months. Although she still had bilateral foot drop but she was able to control her sphincters and to walk with some aid.
Case report 2
In March 2004, a 2-year-old female patient presented with a 3-day history of retrocollis, staggering and tetraparesis. On examination, she was in agony; her temperature was at 37.7. Her neck was hyper extended; there was a thoraco-cervical pigmented skin and a small dimple with a tiny orifice in the center. The muscle strength was estimated at 3/5 in the upper limbs; while the power in her legs graded as 3–4/5. The muscle tone increased all over and reflexes in the legs were exaggerated. Bladder was extended and palpable; anal tone was increased.
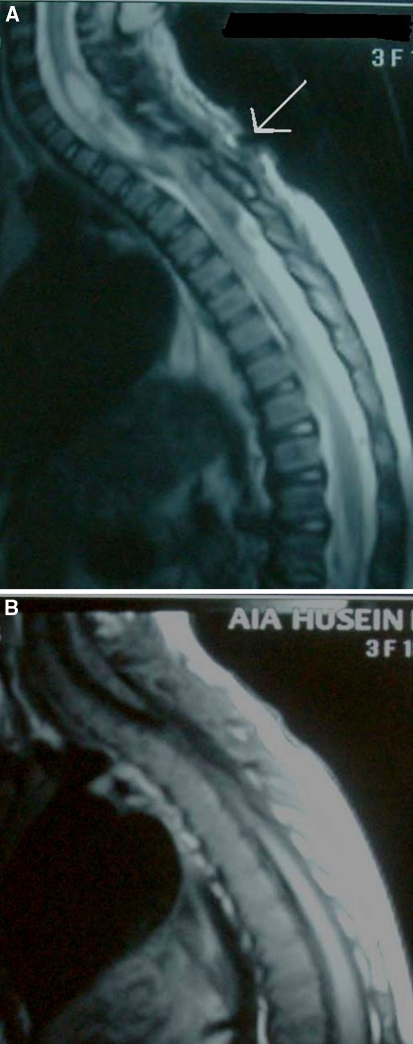
The MRI scan of the cervical spine revealed an intramedullary cystic lesion and central necrosis extended from C5 to TI. The dermal sinus tract and the dimple can also be noticed on the MRI attached to the lower part of the lesion (Fig. 2a). The rest of her investigations, that included thoracic and lumber spine MRI and CT scan of chest and abdomen, were normal.
Fig. 2.
a Gadolinium-enhanced sagittal MRI T1 W of the cervical spine demonstrating multicystic intramedullary lesion at the level of C5–T1, associated with spinal cord expansion. The dermal sinus tract and the dimple are also illustrated; the tract is attaching the skin to the spinal cord (arrow). b postoperative sagittal MR scanning revealed cervical spinal cord atrophic changes
The child underwent urgent C6–T1 laminectomy and resection of the dermal sinus. A purulent discharge was drained from the pale and tense spinal cord followed by copious irrigation with normal saline. She commenced immediately on vancomycin and tazocin. Cultures of the pus fluid were positive for S. aureus and blood culture was negative. Antibiotics were adjusted to Vancomycin based on the culture sensitivity for 6 weeks. Cultures for acid-fast bacilli (AFB) and Brucella were negative.
She postoperatively demonstrated some improvement and; she was referred to neuro-rehabilitation. On the regular follow-up as an outpatient for 2 years; the patient ended with residual neurological deficit in sort of difficulty walking and spastic tetraparesis with muscle strength almost around 4/5; she also still suffering from urinary urgency and stress incontinence.
Case report 3
In June 2003, a 12-month-old girl, attended with a 3-day history of febrile illness, urinary retention and both leg weakness. On examination, the child was febrile with temperature of 39°C. She had no meningeal signs, there was a mild thoraco-lumber scoliosis and upper anal cleft opening was also noted. The power was graded at 3/5 in hips and knees and at 2/5 in her feet; knee reflexes were preserved while ankle reflexes were absent. She had palpable bladder and weak anal tone.
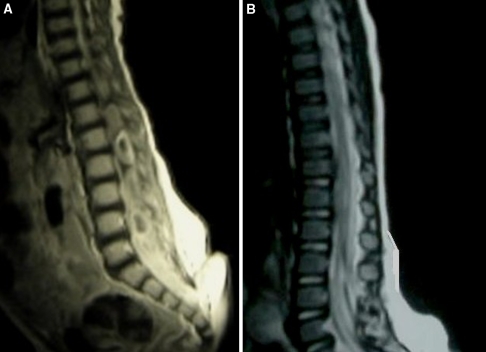
The MRI scan revealed a spinal cord enhancing cystic lesion extended from L1 to S1. The dermal sinus tract was extending from the skin to the lower part of the thecal sac (Fig. 3a).
Fig. 3.
a Sagittal MRI scan T1 W scan with contrast of the thoraco-lumber spine showing intramedullary hypointense multicystic lesion extending from L1 to L5 with marked enhancement and spinal cord enlargement. Note again the dimple and dermal sinus tract as it attached the skin to the thecal sac. b Postoperative MRI scan revealing a significant resolution of the abscess
Laminectomy of L3–5 was then achieved. The edematous spinal cord bulged through the dural opening. The dermal sinus tract was dissected gently and then separated and resected from the neural tissue. A large amount of purulent fluid evacuated from the myelotomy site. Same surgical technique was then applied to aspirate the pus.
Same antibiotic protocol was used. Gram-stain and subsequent cultures of blood and the pus aspirate were positive for S. aureus and negative for AFB and Brucella.
Postoperatively, the patient demonstrated a good recovery; she became afebrile and started to have some movements in her legs within a week. She was sent for neuro-rehabilitation. The postoperative MRI spine revealed a total resolution of the abscess (Fig. 3b).
The child displayed a significant neurological improvement on the regular assessment as an outpatient for nearly 24 months. Although she still had bilateral leg weakness but she was able to control her sphincters and to walk independently.
Case report 4
In January 2001, a 5-year-old boy referred to our service with a 1-day history of rapid progressive lower limb weakness, and both bladder and bowel dysfunction with fever.
On examination, he was sick with the temperature of 39°C and heart rate at 110/minute. He had flail legs and hypotonia, reflexes were absent, bladder was full and palpable; anal tone was weak, meningeal irritation signs were negative. There was no skin abnormality elicited.
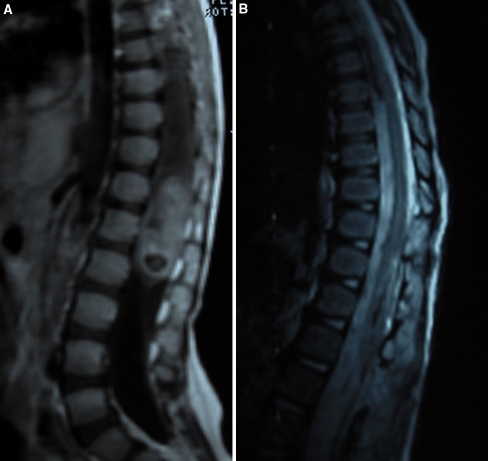
There was a localized conus medullaris septated cystic lesion with some enhancement on the lumber MRI scan (Fig. 4a), the rest of his investigations was normal.
Fig. 4.
MR sagittal T1 W with contrast of the thoraco-lumber spine demonstrating a localized conus medullaris cystic lesion with irregular enhancement with swollen spinal cord mimicking neoplastic lesions. b Postoperative MRI sagittal scan revealed a total resolution of the abscess and the spinal cord swelling
The child underwent immediate T12–L1 laminectomy for drainage of the ISCA; the uptight spinal cord relieved after the drainage of the purulent fluid and irrigation. No congenital abnormality detected intraoperatively.
The pus cultures were positive for S. aureus and sensitive to vancomycin.
Because of his febrile illness, he had a stormy postoperative course. He started to improve after 3 days and became stable after a weak. Antibiotics discontinued after 6 weeks and he was sent to neuro-rehabilitation. The postoperative MRI revealed a total resolution of the abscess (Fig. 4b). On the 24 month assessment the patient was ambulatory alone with power ranging between 4–4 + /5, although his bladder and bowel function improved on training but he still had dysuria and constipation.
Analytical review and results
The study group consisted of four children, three females and one male (3:1), treated for ISCA between 2001 and 2006. The diagnosis was based on the clinical presentation; an MRI scan is positive for intramedullary spinal cord lesion, intraoperative pus collection and positive culture for bacterial growth. (Table 1).
Table 1.
Demographic distribution
| No. | % | |
|---|---|---|
| Sex M:F | 1:3 | 25:75 |
| Age (median) | 2.2 years | |
| Symptoms duration to treatment | 1–3 days | |
| Location | ||
| Thoraco-lumber | 2 | 50 |
| Cervical | 1 | 25 |
| Conus medullaris | 1 | 25 |
Neural tube defect abnormality presented in three patients. Dermal sinus was found on the three cases (75%) and supposed to be the direct source of bacterial implant to the spinal cord. Although the origin of infection could not be identified on the fourth case; hematogenous route or spread from adjacent focus of infection was believed to be the cause of infection in one case. S. aureus was the offensive organism in all cases.
Fever and rapid progressive weakness with double sphincteric problems were the cardinal presenting symptoms in common. Preoperative work up includes; full clinical assessment, complete blood count, erythrocyte sedimentation rate, C-reactive protein, blood cultures and MRI of the spine with gadolinium contrast. All patients treated surgically with limited laminectomy and myelotomy for draining of the abscess along with the normal saline irrigation and concomitant with a 6-week course of intravenous antibiotics based on the sensitivity.
Intraoperatively, the spinal cord was swollen and appeared whitish with no visible thrombosed blood vessels in all cases. The relatively local avascularity of the spinal cord and high mechanical pressure locally from the abscess formation within a non-expansible space is believed to be the cause of the devastating spinal cord damage, which could be irreversible, if left untreated for a longer time.
However, intensive neuro-rehabilitation was organized for all cases. On the regular assessment for 24 months; one patient demonstrated a significant neurological improvement; while the other three patients displayed a satisfactory recovery (Table 2).
Table 2.
Analysis of the cases with intramedullary spinal cord abscess
| Case I | Case II | Case III | Case IV | |
|---|---|---|---|---|
| Age/sex | 8 m/F | 2/F | 1/F | 5/M |
| Presence of congenital anomaly/risk factor | Sacral dermal sinus, tethered cord | Cervical dimple and dermal sinus | Sacral dermal sinus | Negative |
| Status | Fever, paraplegia | Fever, tetraparesis | Fever and paraplegia | Febrile illness, paraplegia |
| Site of abscess | Thoraco-lumber | Cervical | Thoraco-lumber | Conus medullaris |
| Probable route of spread | Direct | Direct | Direct | Blood |
| Treatment | Drainage and antibiotics | Drainage and antibiotics | Drainage and antibiotics | Drainage and antibiotics |
| Intraoperative appearance of the spinal cord | Swollen, pale and scanty blood vessels | Swollen, pale and scanty blood vessels | Swollen, pale and scanty blood vessels | Swollen, pale and scanty blood vessels |
| Inflammatory markers | Elevated | Slight elevation | Missed | Elevated |
| WBCs, ESR and CRP | ||||
| Abscess culture | S. aureus | S. aureus | S. aureus | S. aureus |
| Blood culture | S. aureus | Negative | S. aureus | Negative |
| Outcome | Good | Fair | Good | Excellent |
Excellent: Significant improvement, the patient is completely independent
Good: some improvement, the patient is independent but she needs some aid
Fair: minimal improvement, although there was some neurological improvement but the patient still with disability and needs help
Discussion
Intramedullary spinal cord abscess is a rare neurosurgical condition and may resemble spinal cord neoplasms. The origin of this pathology is variable; although it could be cryptic but metastatic blood infection and extension from adjacent structures are the major source of this type of infection. The common hemopoietic sources include congenital defects, urogenital or lung infection and infective endocarditis [17]. In adults, blood route is the main source of ISCA. Congenital dermal sinus is implicated as the leading cause of ISCA in children. It was found to be the origin of infection in approximately half of affected children compared with a quarter in all age groups. The congenital neural tube defect is just recently considered as the most important source of ISCA in the antibiotic era, it is high likely, because other sources of infection are more effectively treated with antibiotics before they end with a serious central nervous infection [6, 8, 12, 21].
The dermal sinus is due to imperfect separation between cutaneous and neural ectoderm in the early fetal life and results in an epithelialized tract. It may end anywhere along its way superficially within the skin or deeply in the intraspinal spaces and may be associated with other congenital anomalies such as dermoid cyst and tethered cord. As a result, this tract could be a potential route of bacterial dissemination to the central nervous system (CNS). It can cause meningitis or infect the spaces around the spinal cord or even infect the spinal cord itself; basically when the latter becomes in direct contact with the sinus. Thoraco-lumbar region of spinal cord is a frequent site of involvement. This infection has a potentiality to spread vertically along the fiber tracts of the cord itself to involve the entire spine [9, 10, 16, 17, 20].
Intramedullary spinal cord abscess may present at any age but children under the age of five are more likely affected. S. aureus is usually the most common cultured organism in this group; other pathogens may also be implicated but less frequently [1, 6, 21]. Specific infections, such as B.melitensis and AFB, are to be considered mainly in endemic areas [22, 26]. In Simon et al. [21] review of children with ISCA the mean age of presentation was around 15.5 months ranging between 6 months and 5 years and S. aureus was the significant offensive organism of ISCA; occasionally cultures can be negative.
Even with a marked reduction in the mortality and morbidity rate in the post antimicrobial era, this infection may result in a considerable damage to the spinal cord and the neurological outcome may remain disappointing. Still, early diagnosis and appropriate surgical intervention with administration of wide spectrum antibiotics is the main stay to prevent neurological disability and to improve the functional outcome [1, 21].
Magnetic resonance imaging with gadolinium contrast is the gold-standard of investigation before surgical planning. Whole spine should be scanned to show the location and extension of the abscess. It usually illustrates a cystic cavitation with septation within the spinal cord matrix and peripheral enhancing rim. Localized abscess with variable enhancement may resemble neoplasms. MRI is also helpful in demonstrating the co-existence of congenital anomalies [20].
As a part of routine clinical examination; all newborns should be checked for the presence of dermal sinus or other congenital defects. Once it is discovered; prophylactic surgical resection is highly advocated by many authors, regardless of age, to avoid serious neurosurgical complications [16–18]. Should the abscess occurred, suitable intravenous antimicrobial agents and prompt surgical evacuation through a limited laminectomy and myelotomy with copious irrigation with normal saline is considered the treatment of choice simultaneously, any concomitant abnormalities should also be treated during the surgery. On the other hand, in cases of extensive abscess; gentle advancing of inside catheter rostrally through the limited myelotomy, to communicate the septated cavities and to drain the abscess, can be achieved effectively with remarkable results [9, 15, 18, 23–25]. In this way we may protect the child from unnecessary extensive laminectomy and its subsequent orthopedic complications [14, 19].
Outcome of spinal cord abscesses was dismal in the pre antibiotic era, with high mortality and morbidity rate. However, once the preliminary diagnosis is made, early and adequate surgical treatment alongside antibiotics can only offer favorable outcome [5, 6, 10, 21].
Conclusions
Suspicion of spinal cord abscess should be raised in patients with dermal sinus and rapid progressive weakness in particular those who develop febrile illness. Entire spine MRI is essential in assessing all patients and for planned surgery. Before irreversible spinal cord damage can occur from vascular compromise and local mechanical pressure within a restricted and non-expansible space; timely surgical drainage through limited laminectomy and myelotomy with adequate antibiotics is advocated and considered as an effective model of treatment with satisfactory results. It is still highly recommended to eradicate the dermal sinus once it is found; serious CNS infection and its potential disabling condition will be eliminated.
References
- 1.Bartels RH, Gonera EG, Spek JA, Thijssen HO, Mullaart RA, Gabreels FJ. Intramedullary spinal cord abscess. A case report. Spine. 1995;20:1199–1204. doi: 10.1097/00007632-199505150-00017. [DOI] [PubMed] [Google Scholar]
- 2.Bavdekar SB, Rao N, Kamat JR. Intramedullary spinal cord abscess. Indian J Pediatr. 1997;64:428–431. doi: 10.1007/BF02845220. [DOI] [PubMed] [Google Scholar]
- 3.Benzil DL, Epstein MH, Knuckey NW. Intramedullary epidermoid associated with an intramedullary spinal abscess secondary to a dermal sinus. Neurosurgery. 1992;30:118–121. doi: 10.1227/00006123-199201000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Bruff P, Sgouros S. Lumbar dermoid cyst causing pyomyelia in a child. Pediatr Neurosurg. 2002;36:162–163. doi: 10.1159/000048374. [DOI] [PubMed] [Google Scholar]
- 5.Byrne RW, Roenn KA, Whisler WW. Intramedullary abscess: a report of two cases and a review of the literature. Neurosurgery. 1994;35:321–326. doi: 10.1097/00006123-199408000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Chan CT, Gold WL. Intramedullary abscess of the spinal cord in the antibiotic era: clinical features, microbial etiologies, trends in pathogenesis, and outcomes. Clin Infect Dis. 1998;27:619–626. doi: 10.1086/514699. [DOI] [PubMed] [Google Scholar]
- 7.Chidambaram B, Balasubramaniam V. Intramedullary abscess of the spinal cord. Pediatr Neurosurg. 2001;34:43–44. doi: 10.1159/000055991. [DOI] [PubMed] [Google Scholar]
- 8.David C, Brasme L, Peruzzi P, Bertault R, Vinsonneau M, Ingrand D. Intramedullary abscess of the spinal cord in a patient with a right-to-left shunt: case report. Clin Infect Dis. 1997;24:89–90. doi: 10.1093/clinids/24.1.89. [DOI] [PubMed] [Google Scholar]
- 9.Desai KI, Muzumdar DP, Goel A. Holocord intramedullary abscess: an unusual case with review of literature. Spinal Cord. 1999;37:866–870. doi: 10.1038/sj.sc.3100930. [DOI] [PubMed] [Google Scholar]
- 10.DiTullio MV., Jr Intramedullary spinal abscess: a case report with a review of 53 previously described cases. Surg Neurol. 1977;7:351–354. [PubMed] [Google Scholar]
- 11.Erlich JH. Acute intramedullary spinal cord abscess: case report. Surg Neurol. 1992;38:287–290. doi: 10.1016/0090-3019(92)90043-M. [DOI] [PubMed] [Google Scholar]
- 12.Guzel N, Eras M, Guzel DK. A child with spinal intramedullary abscess. Childs Nerv Syst. 2003;19:773–776. doi: 10.1007/s00381-003-0802-5. [DOI] [PubMed] [Google Scholar]
- 13.Hart J. A case of encysted abscess in the center of the spinal cord. Dublin Hosp Rep. 1830;5:522–524. [Google Scholar]
- 14.Katsumi Y, Honma T, Nakamura T. Analysis of cervical instability resulting from laminectomies for removal of spinal cord tumor. Spine. 1989;14:1171–1176. doi: 10.1097/00007632-198911000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Koppel BS, Daras M, Duffy KR. Intramedullary spinal cord abscess. Neurosurgery. 1990;26:145–146. doi: 10.1097/00006123-199001000-00023. [DOI] [PubMed] [Google Scholar]
- 16.Krishnapundh B, Tayard D, Wiroje P. Holocord intramedullary abscess due to dermal sinus in a 2 month old child successfully treated with limited myelotomy and aspiration. Case report. J Neurosurg (4 Suppl Pediatrics) 2006;104:269–274. doi: 10.3171/ped.2006.104.4.269. [DOI] [PubMed] [Google Scholar]
- 17.Morandi X, Mercier P, Fournier HD, Brassier G. Dermal sinus and intramedullary spinal cord abscess. Report of two cases and review of the literature. Childs Nerv Syst. 1999;15:202–208. doi: 10.1007/s003810050370. [DOI] [PubMed] [Google Scholar]
- 18.Morimoto K, Takemoto O, Nakamura H, Takeuchi M. Spinal dermal sinus associated with intramedullary abscess and dermoid. Pediatr Neurosurg. 2003;39:225–226. doi: 10.1159/000072478. [DOI] [PubMed] [Google Scholar]
- 19.Papagelopoulos PJ, Peterson HA, Ebersold MJ, Emmanuel PR, Choudhury SN, Quast LM. Spinal column deformity and instability after lumbar or thoracolumbar laminectomy for intraspinal tumors in children and young adults. Spine. 1997;22:442–451. doi: 10.1097/00007632-199702150-00019. [DOI] [PubMed] [Google Scholar]
- 20.Rogg JM, Benzil DL, Haas RL, Knuckey NW. Intramedullary abscess, an unusual manifestation of a dermal sinus. AJNR Am J Neuroradiol. 1993;14:1393–1395. [PMC free article] [PubMed] [Google Scholar]
- 21.Simon JK, Lazareff JA, Diament MJ, Kennedy WA. Intramedullary abscess of the spinal cord in children: a case report and review of the literature. Pediatr Infect Dis. 2003;22:186–192. doi: 10.1097/01.inf.0000048910.19136.49. [DOI] [PubMed] [Google Scholar]
- 22.Suzer T, Coskun E, Tahta K, Bayramoglu H, Duzcan E. Intramedullary spinal tuberculoma presenting as a conus tumor: a case report and review of the literature. Eur Spine J. 1998;7:168–171. doi: 10.1007/s005860050050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tacconi L, Arulampalam T, Johnston FG, Thomas DG. Intramedullary spinal cord abscess: case report. Neurosurgery. 1995;37:817–819. doi: 10.1097/00006123-199510000-00028. [DOI] [PubMed] [Google Scholar]
- 24.Thome C, Krauss JK, Zevgaridis D, Schmiedek P. Pyogenic abscess of the filum terminale. Case report. J Neurosurg. 2001;95((1)(Suppl)):100–104. doi: 10.3171/spi.2001.95.1.0100. [DOI] [PubMed] [Google Scholar]
- 25.Tsurubuchi T, Matsumura A, Nakai K, Fujita K, Enomoto T, Iwasaki N, et al. Reversible holocord edema associated with intramedullary spinal abscess secondary to an infected dermoid cyst. Pediatr Neurosurg. 2002;37:282–286. doi: 10.1159/000066306. [DOI] [PubMed] [Google Scholar]
- 26.Vajramani GV, Nagmoti MB, Patil CS. Neurobrucellosis presenting as an intramedullary spinal cord abscess. Ann Clin Microbiol Antimicrob. 2005;16(4):14. doi: 10.1186/1476-0711-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]