Abstract
Background:
The treatment of older adults with pain is complex and affected by age-related changes in pharmacokinetics and pharmacodynamics. Chronic pain encompasses a complex array of sensory-discriminatory, motivational-affective, and cognitive-evaluative components. Because of this complexity, both pharmacologic and nonpharmacologic approaches should be considered to treat pain.
Aims:
Given the large number of older persons with pain at the end of life and the few data about this issue, the objective of this article is to review the treatment of pain in this population.
Patients and Methods:
We searched The Cochrane Library, MEDLINE and LILACS from 1990 to 2011 and the references in retrieved manuscripts. The search terms were pain AND elderly AND end of life.
Results:
There are evidences of undertreatment among elderly people. The association of nonpharmacologic resources with the pharmacological treatment can help reduce the use of analgesics minimizing the side effects of long term medication. Pharmacological treatment is escalated in an orderly manner from non-opioid to weak opioid to strong opioid. Adjuvant drugs like anticonvulsants and antidepressants may be necessary.
Conclusions:
The sequential use of analgesics drugs and opioids are considered effective and relatively inexpensive for relieving pain, but no well designed specific studies in the elderly patient are available. There are not specific recommendations about the long-term use of complementary and alternative therapies and although their effectiveness remains unproven they should not be discouraged. Palliative sedation may be a valid palliative care option to relieve suffering in the imminently dying patient.
Keywords: Chronic pain, end of life care, older people, pharmacologic and nonpharmacologic approaches
Introduction
The phenomenon of population aging has been observed throughout the world and Brazil is one of the countries with the fastest rates of aging. In 2025, Brazil will be the 6th country in number of elderly people worldwide. As consequence, the health profile of the population has changed. There was a decrease of acute processes that evolve to cure or death and an increase in chronic degenerative non-communicable diseases (NCDs), which nowadays are primarily responsible for disability and mortality in our population[1,2].
Elderly has the highest prevalence of comorbidity, disability, and frailty of any age group. Because of these characteristics the treatment of older adults with pain is complex and affected by age-related changes in pharmacokinetics and pharmacodynamics. Polypharmacy, defined as either the use of multiple medications or the use of unnecessary medications, is common in older people and increases the risk of adverse drug reactions, nonadherence, and increased cost[3].
Nowadays most elderly people die after a period of deterioration caused by one or more chronic progressive illnesses and the suffering that characterizes the period before death can be related, at least in part, to the experience of unrelieved symptoms. Pain is among the most prevalent of these symptoms and management of chronic nonmalignant and malignant pain prevents disability and improves quality of life in elderly at the end of life. Despite this, pain management is reported to be poor in elderly[4,5].
Chronic pain encompasses a complex array of sensory-discriminatory, motivational-affective, and cognitive-evaluative components. Because of this complexity, both pharmacologic and nonpharmacologic approaches should be considered to treat pain[6].
Given the large number of older persons with pain at the end of life and the few data about this issue, the objective of this article is to review the pharmacologic and nonpharmacologic approaches of the pain treatment in this population.
Methods
We searched The Cochrane Library, MEDLINE and LILACS from 1990 to 2011 and the references in retrieved manuscripts. The search terms were pain AND elderly AND end of life. We included randomized controlled trials (RCTs) and reviews articles.
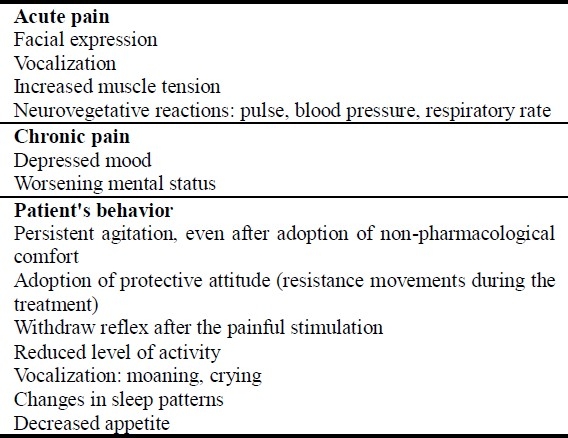
Pain assessment in the elderly
The two most commonly used scales for adults are a verbal descriptor scale (i.e. “Which word best describes your pain; none, mild moderate, severe or excruciating?”) or a numerical scale (i.e. “On a scale from 0 to 10, where 0 indicates no pain and 10 indicates the worst pain you can imagine, how would you rate your pain?”)[7]. However, elderly patients often have significant cognitive, motor, visual, or auditory impairments that must be considered when evaluating the presence and intensity of symptoms, and the assessment method should be modified accordingly. Some signs and symptoms are suggestive of the presence of pain and can be used to assess non-communicative elderly and patients with cognitive impairment or delirium[8,9] (Table 1).
Table 1.
Assessment of Pain in the Confused Non-communicative Elderly
Nonpharmacologic therapy of pain
Pain can be alleviated in elderly through the careful use of analgesic drags combined with nonpharmacologic strategies. The nonpharmacological treatment of pain at the end of life has been little explored and yet little used. Lack of a scientific support for the use of these resources has hindered their implementation as effective tools for the treatment of pain. However, these non invasive methods can be of great help to patients suffering from pain. The association of nonpharmacologic resources with the pharmacological treatment can help reduce the use of analgesics minimizing the side effects of long term medication[10].
-
Physical therapies
The role of physiotherapists in palliative care is primarily defined by expert opinion, which is not backed up by good quality evidence. However, an absence of research evidence does not mean that a service or treatment is ineffective, just that we don’t know for certain yet[11]. The maintenance or improvement of the functional component of quality of life and significant improvements in pain are noted in patients who received optimized levels of physiotherapy time and resources[12].
Physical therapy techniques used in pain control:
- Massage: Touch is probably the oldest method of relieving pain and discomfort. Therapeutic massage using stroking and gentle kneading may be used to reduce muscle spasm, relieve pain, aid relaxation, and maintenance of joint range.
- Cold/Heat: Where local skin sensation is normal and tissue is intact, local applications of heat and ice may be used to reduce spasm, for acute inflammatory conditions, and over myofascial trigger points.
- Electrophysical Modalities: Transcutaneous electrical nerve stimulation (TENS) is the only electrical modality currently recommended for use in the presence of active neoplastic disease. Therapeutic ultrasound, interferential or pulsed shortwave diathermy relieves pain and muscle spasm and may be used over normal tissue and for non-cancer patients[11].
- Exercise: Systematic reviews of observational and randomized controlled clinical trials conclude that there is strong evidence that participation in regular physical activity reduces the pain and enhances the functional capacity of older adults with persistent pain. Because persistent pain is commonly associated with prolonged physical inactivity, these effects may be partly due to the reversal of the physiologic consequences of reconditioning[8].
-
Psychological therapies
Formal cognitive-behavioral therapies are helpful for many older adults with persistent pain. Oriented therapy may provide patients and families with the support, knowledge, and skills they need to cope with cancer treatment, pain, and death. Patients and families learn to utilize their preexisting coping abilities and to develop new ones for difficult situations, including uncontrolled pain[13–15]. Delirium and cognitive impairment are obstacles to psychotherapy.
-
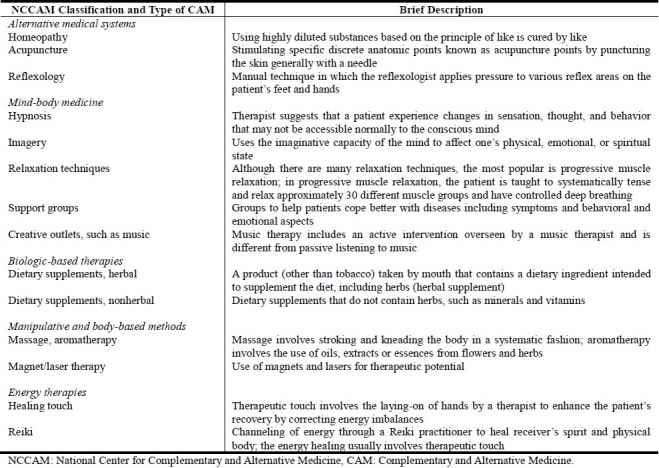
Complementary and alternative therapies
Unrelieved persistent pain commonly causes patients to seek relief with alternative medicine, including homeopathy, acupuncture, healing touch, and music therapy. Although there is little scientific evidence for the efficacy of most of these strategies for controlling persistent pain, it is important that clinicians not leave patients with a sense of hopelessness as a result of their efforts to discourage unapproved but benign therapies or to debunk healthcare quackery and fraud. The effectiveness of homeopathy as a symptomatic treatment for acute and chronic pain remains unproven. Recent neuroscience research suggested that acupuncture induces clinical responses though the modulation of the nervous system[16]. Some trials showed that acupuncture relieves both acute and chronic pain[17–19]. A Cochrane's review concluded that touch therapies may have a modest effect in pain relief and more studies on healing touch and Reiki in relieving pain are needed[20]. Another Cochrane's review showed that listening to music reduces pain intensity levels and opioid requirements, but the magnitude of these benefits is small and, therefore, its clinical importance unclear[21]. Table 2 shows the National Center for Complementary and Alternative Medicine (NCCAM) classification of available complementary and alternative medicine (CAM).
Table 2.
NCCAM classification of CAM interventions and their brief description [22]
Pharmacologic therapy of pain
Inferences about the type and mechanisms that may be responsible for the pain are helpful in the evaluation and the management of pain syndromes[23].
-
A)
Nociceptive Pain: may be visceral or somatic and is most often derived from the stimulation of pain receptors. Nociceptive pain may arise from tissue inflammation, mechanical deformation, ongoing injury or destruction. Examples include inflammatory or traumatic arthritis, myofascial pain syndromes, and ischemic disorders. Nociceptive mechanisms usually respond well to traditional approaches to pain management, including common analgesic medications and nonpharmacologic strategies.
-
B)
Neuropathic Pain: results from a pathophysiologic process that involves the peripheral or central nervous system. Examples include diabetic neuropathy, trigeminal neuralgia, post-herpetic neuralgia, poststroke central or thalamic pain, and postamputation phantom limb pain. These pain syndromes do not respond as predictably as do nociceptive pain to conventional analgesic therapy. However, they have been noted to respond to unconventional analgesic drugs, such as tricyclic antidepressants, anticonvulsants, or antiarrhythmic drugs[8].
Nociceptive pain
The use of analgesics for the treatment of acute pain is the same as for non-palliative care patients. The treatment of chronic pain is often poorly managed and requires a different approach. There are evidences of undertreatment especially among elderly people[4].
According to World Health Organization treatment is escalated in an orderly manner from non-opioid to weak opioid to strong opioid - “Analgesic Ladder”(Tables 3 and 4)[24].
Table 3.
World Health Organization (WHO) analgesic ladder [24]
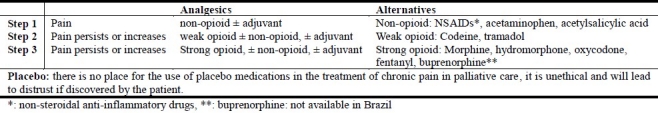
Table 4.
Adjuvant drugs. Adapted from Doyle D, 2008[25]
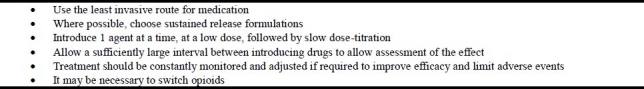
There is a scarcity of published data relating to opioid use in the elderly. The only international guidelines that are available are from the American Geriatric Society, the most recent being from 2002[8] which made a number of important recommendations (Table 5).
Table 5.
Recommendations of the American Geriatric Society for opioid use in the elderly
Elderly's particularities and cautions
The pain management in older individuals follows the same principles as in younger patients. However, the approach may require modification because of comorbidities or physiologic changes associated with aging. Polypharmacy, defined as either the use of multiple medications or the use of unnecessary medications, is common in older people and increases the risk of adverse drug reactions, nonadherence, and increased cost. Several drugs used to treat pain, such as opioids, tricyclic antidepressants, gabapentin, and pregabalin, are among those associated with sedation, dizziness, and falls, particularly in frail or vulnerable elderly patients. Aging is associated with clinically important changes in pharmacokinetics and pharmacodynamics. Drug absorption is generally unchanged, but studies of drug distribution reveal increased plasma concentration of water-soluble drugs and increased half-life of fat-soluble drugs in older adults. For all opioids half-life of the active drug and metabolites is increased in the elderly. It is, therefore, recommended that doses be reduced, a longer time interval be used between doses, and creatinine clearance be monitored[3,8]. Table 6 shows the age-related changes in hepatic metabolism and renal excretion.
Table 6.
Age-related Changes in Hepatic Metabolism and Renal Excretion (Adapted from Schmader et al) [3]
![]()
-
A)
Non-Opwids: the non-opioid analgesics include acetylsalicylic acid (ASA), other NSAIDs, and acetaminophen.
-
1)NSAIDs: The gastrointestinal harm induced by NSAIDs may be the most prevalent adverse event associated with this drug. Gastrointestinal adverse events are more likely to occur with long-term use and with higher doses of the NSAID. Advanced age is a risk factor for gastrointestinal complications and a proton pump inhibitor or misoprostol should be used during the treatment with the NSAIDs. The use of COX-2 inhibitors may reduce the risk for gastrointestinal events; however, this benefit is negated if the patient is using aspirin, even at low doses. The cardiotoxicity of the NSAIDs in the elderly is of particular concern. The patient populations most likely to be prescribed NSAIDs for pain relief are often the same populations with cardiovascular risk factors and it does not appear that the toxic effects can be avoided by restricting their use to short durations. Selection of therapy must weigh cardiovascular risk as well as benefit, other risks of therapy, and costs. The cardiovascular risks first appeared to be a class effect of the COX-2 (cycloxygenase-2) inhibitors. Naproxen and ibuprofen appear to be the safest with respect to cardiovascular risk, when specifically measuring cardiovascular events and mortality. Naproxen appears to convey a statistically significant protective outcome in terms of cardiovascular events however for those with cardiovascular disease or risk factors for ischemic heart disease the American Heart Association recommends acetaminophen, aspirin, tramadol, and opioid analgesics as firstline therapy. Although the rate of NSAID-induced nephrotoxicity has been estimated to be low (1-5%) the NSAIDs, including COX-2 inhibitors, must be used cautiously or not at all in patients with predisposing renal conditions. It is important to monitor blood pressure, weight, and serum creatinine and potassium concentrations when appropriate, use the lowest dose possible, and consider limiting dietary salt intake[6,24].
-
2)Acetaminophen: The adverse effects are liver and renal toxicity and caution is necessary in patients with liver damage. The total dose per day should not exceed 4000 mg of acetaminophen[26].
-
1)
-
B)
Weak Opioids: the weak opioid analgesics include tramadol and codeine. Tramadol has a ceiling effect for analgesia and can lower the seizure threshold. Anorexia, nausea and vomiting, constipation and dizziness are frequent side effects. The most common adverse reactions with codeine are constipation and drowsiness. Codeine can depress central nervous system. Both tramadol and codeine require dose adjustment for renal impairment.
-
C)
Strong Opioids: all opioids are considered effective in cancer and non-cancer pain management, but no well designed specific studies in the elderly patient are available. Higher opioid doses are often needed for neuropathic pain than for nociceptive pain. With all opioids, the adverse reactions and events can be limited by using lower starting doses, longer dose intervals, and slow titration; however, constipation, nausea, and vomiting often require prophylaxis or therapy. Patients never become tolerant to the constipating effects of opioids. Always start stimulant laxative/softener combination with opioids. Other common adverse reactions with opioids use include sedation, impaired judgment, impaired psychomotor function and respiratory depression[8,27,28].
-
D)
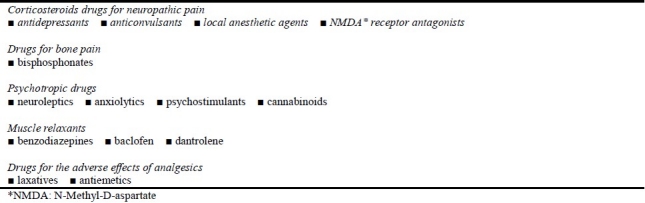
Adjuvant Drugs: The adjuvant drugs (Table 4) may be necessary for one of three reasons[24]:
- to treat the adverse effects of analgesics (e.g. antiemetics and laxatives);
- to enhance pain relief (e.g. a corticosteroid in nerve compression pain and a anticonvulsant in neuropathic pain);
- to treat concomitant psychological disturbances such as insomnia, anxiety and depression (e.g. night sedatives, anxiolytics, antidepressants).
Elderly is a population at risk for developing side effects of drugs acting on central nervous system. Dizziness, somnolence or sedation, and peripheral edema are reported common side effects of anticonvulsants. Dry mouth and somnolence or sedation are reported side effects of tricyclic antidepressants and benzodiazepines[29].
Neuropathic pain
The exclusion of older adults with comorbidities and the underrepresentation of the “old old” (people >80 years) are phenomena seen in clinical trials of medications for neuropathic pain[3,30].
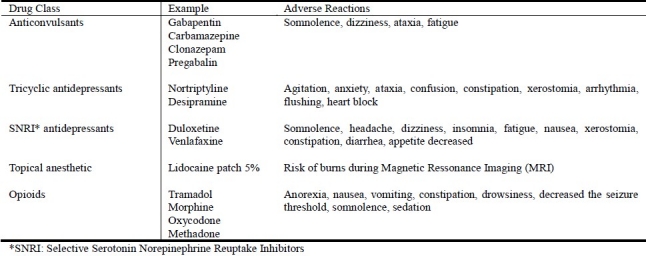
Neurophatic pain can require higher doses of opioids. Table 7 shows drug classes, examples and adverse reactions of the pharmacological treatment of the neuropathic pain.
Table 7.
Palliative sedation
Palliative sedation therapy (PST) is a controversial issue. When other treatments fail to relieve suffering in the imminently dying patient, PST may be a valid palliative care option. PST is defined as the use of specific sedative medications to relieve intolerable suffering from refractory symptoms by a reduction in patient consciousness, using appropriate drugs carefully titrated to the cessation of symptoms. The initial dose of sedatives should usually be small enough to maintain the patients’ ability to communicate periodically. In the case of continuous and deep PST, the disease should be irreversible and advanced, with death expected within hours to days. Midazolam should be considered first-line choice[31].
Conclusions
Both pharmacologic and nonpharmacologic approaches should be considered to treat pain in elderly at the end of life. It is difficult to make specific recommendations about the long-term use of complementary and alternative therapies but it is important that clinicians not leave patients with a sense of hopelessness as a result of their efforts to discourage unapproved but benign therapies. The sequential use of analgesics drugs according the WHO ladder is a relatively inexpensive yet effective method for relieving pain. All opioids are considered effective and are used in cancer and non-cancer pain management, but no well designed specific studies in the elderly patient are available. To relieve suffering in the imminently dying patient palliative sedation may be a valid palliative care option.
References
- 1.Instituto Brasileiro de Geografia e Estatística. [Accessed May 11, 2011]. at http://www.ibge.br/
- 2.World Health Organization (WHO) World Health Statistics. 2009. [Accessed May 15, 2011]. at http://www.who.int/whosis/whostat/EN_WHS09_Full.pdf .
- 3.Schmader KE, Baron R, Haanpaa ML, et al. Treatment considerations for elderly and frail patients with neuropathic pain. Mayo Clin Proc. 2010;85(3 Suppl):S26–32. doi: 10.4065/mcp.2009.0646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group. Systematic Assessment of Geriatric Drug Use via Epidemiology. JAMA. 1998;279(23):1877–1882. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 5.Fineberg IC, Wenger NS, Brown-Saltzman K. Unrestricted opiate administration for pain and suffering at the end of life: knowledge and attitudes as barriers to care. J Palliat Med. 2006;9(4):873–883. doi: 10.1089/jpm.2006.9.873. [DOI] [PubMed] [Google Scholar]
- 6.Herndon CM, Hutchison RW, Berdine HJ, et al. Management of chronic nonmalignant pain with nonsteroidal antiinflammatory drugs.Joint opinion statement of the Ambulatory Care, Cardiology, and Pain and Palliative Care Practice and Research Networks of the American College of Clinical Pharmacy. Pharmacotherapy. 2008;28(6):788–805. doi: 10.1592/phco.28.6.788. [DOI] [PubMed] [Google Scholar]
- 7.Management of cancer pain: adults. Cancer Pain Guideline Panel. Agency for Health Care Policy and Research. Am Fam Physician. 1994;49(8):1853–1868. [PubMed] [Google Scholar]
- 8.The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205–224. doi: 10.1046/j.1532-5415.50.6s.1.x. [DOI] [PubMed] [Google Scholar]
- 9.Pautex S, Michon A, Guedira M, et al. Pain in severe dementia: self-assessment or observational scales? J Am Geriatr Soc. 2006;54(7):1040–1045. doi: 10.1111/j.1532-5415.2006.00766.x. [DOI] [PubMed] [Google Scholar]
- 10.Sampaio L, Moura C, Resende M. Recursos fisioterapêuticos no controle da dor oncológica: revisão da literatura. Rev Bras Cancerol. 2005;51(4):339–334. [Google Scholar]
- 11.Jolliffe J, Bury T. The effectiveness of physiotherapy in the palliative care of older people. The Chartered Society of Physiotherapy. 2002. [Accessed May 23, 2011]. at: www.csp.org.uk .
- 12.Laakso EL, McAuliffe A, Cantlay A. The impact of physiotherapy intervention on functional independence and quality of life in palliative patients. Cancer Forum. 2003;27(1):15–20. [Google Scholar]
- 13.Breitbart W. Psychiatric management of cancer pain. Cancer. 1989;63(11 Suppl):2336–2342. doi: 10.1002/1097-0142(19890601)63:11<2336::aid-cncr2820631144>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 14.Keefe FJ, Affleck G, Lefebvre JC, Starr K, Caldwell DS, Tennen H. Pain coping strategies and coping efficacy in rheumatoid arthritis: a daily process analysis. Pain. 1997;69(1-2):35–42. doi: 10.1016/s0304-3959(96)03246-0. [DOI] [PubMed] [Google Scholar]
- 15.Keefe FJ, Blumenthal J, Baucom D, et al. Effects of spouse-assisted coping skills training and exercise training in patients with osteoarthritic knee pain: a randomized controlled study. Pain. 2004;110(3):539–549. doi: 10.1016/j.pain.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 16.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136(5):374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 17.NIH Consensus Conference. Acupuncture. JAMA. 1998;280(17):1518–1524. [PubMed] [Google Scholar]
- 18.Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005;366(9480):136–143. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 19.Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141(12):901–910. doi: 10.7326/0003-4819-141-12-200412210-00006. [DOI] [PubMed] [Google Scholar]
- 20.So PS, Jiang Y, Qin Y. Touch therapies for pain relief in adults. Cochrane Database Syst Rev. 2008;(4):CD006535. doi: 10.1002/14651858.CD006535.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database Syst Rev. 2006;(2):CD004843. doi: 10.1002/14651858.CD004843.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Bardia A, Barton DL, Prokop LJ, Bauer BA, Moynihan TJ. Efficacy of complementary and alternative medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol. 2006;24(34):5457–5464. doi: 10.1200/JCO.2006.08.3725. [DOI] [PubMed] [Google Scholar]
- 23.Cherny N. Pain assessment and cancer pain syndromes. In: Hanks G, Cherny N, Christakis N, Fallon M, Kaasa S, Portenoy R, editors. Oxford Textbook of Palliative Medicine. Fourth Ed. New York: Oxford University Press; 2010. pp. 599–626. [Google Scholar]
- 24.Cancer pain relief. Second Edition. Geneva: World Health Organization; 1996. World Health Organization. [Google Scholar]
- 25.Doyle D, Woodruff R. The IAHPC Manual of Palliative Care. IAHPC Press. 2008. [Accessed May 23, 2011]. at http://www.hospicecare.com/iahpc-manual/iahpc-manual-08.pdf .
- 26.Ferrell B, Levy MH, Paice J. Managing pain from advanced cancer in the palliative care setting. Clin J Oncol Nurs. 2008;12(4):575–581. doi: 10.1188/08.CJON.575-581. [DOI] [PubMed] [Google Scholar]
- 27.Pergolizzi J, Boger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an International Expert Panel with focus on the six clinically most often used World Health Organization Step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone) Pain Pract. 2008;8(4):287–313. doi: 10.1111/j.1533-2500.2008.00204.x. [DOI] [PubMed] [Google Scholar]
- 28.Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;112(4):810–833. doi: 10.1097/ALN.0b013e3181c43103. [DOI] [PubMed] [Google Scholar]
- 30.Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85(3 Suppl):S3–14. doi: 10.4065/mcp.2009.0649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Graeff A, Dean M. Palliative sedation therapy in the last weeks of life: a literature review and recommendations for standards. J Palliat Med. 2007;10(1):67–85. doi: 10.1089/jpm.2006.0139. [DOI] [PubMed] [Google Scholar]


