Abstract
Background
The work of care for parents of children with complex special health care needs may be increasing, while excessive work demands may erode the quality of care. We sought to summarize knowledge and develop a general conceptual model of the work of care.
Methods
Systematic review of peer-reviewed journal articles that focused on parents of children with special health care needs and addressed factors related to the physical and emotional work of providing care for these children. From the large pool of eligible articles, we selected articles in a randomized sequence, using qualitative techniques to identify the conceptual components of the work of care and their relationship to the family system.
Results
The work of care for a child with special health care needs occurs within a dynamic system that comprises 5 core components: (1) performance of tasks such as monitoring symptoms or administering treatments, (2) the occurrence of various events and the pursuit of valued outcomes regarding the child's physical health, the parent's mental health, or other attributes of the child or family, (3) operating with available resources and within certain constraints (4) over the passage of time, (5) while mentally representing or depicting the ever-changing situation and detecting possible problems and opportunities. These components interact, some with simple cause-effect relationships and others with more complex interdependencies.
Conclusions
The work of care affecting the health of children with special health care needs and their families can best be understood, studied, and managed as a multilevel complex system.
Background
Medical care advances have dramatically reduced pediatric morbidity and mortality - from formerly premature infants with severe chronic lung disease requiring supplemental oxygen and assisted ventilation, through to adolescents with treatment-refractory epilepsy or myriad other medical conditions - while creating new challenges for children and families [1,2]. In the United States, approximately 13 to 20% of households have an infant, child, or adolescent with a special health care need (CSHCN) [3]. The mounting dependency on medical technology, reliance on multitudes of medications, and intense use of medical services place increased demands on parents. At the same time, parents must also navigate the complicated systems of health insurance and childhood education, while attending to other responsibilities including maintaining their own mental and physical health and that of their families, and wrestling with the larger existential questions posed by their child's illness.
While these dimensions of the experience of illness or disability are often referred to as "caregiving" or the "burden of care", the phrase "work of care" (WOC) specifies the physical and mental efforts of specific tasks in which parents engage, while avoiding the conflation in the term "caregiving" of both a person who is a caregiver and a set of actions that constitute caregiving, and the negative and potentially biased emotive connotations of "burden". While physicians, nurses, and the broad health care system are certainly important to the health and wellbeing of CSHCN, and at various times during a child's life (such as during a hospitalization) may share in performing the tasks involved in caring for the child, the WOC is chiefly performed by the patient and family. Parental WOC is too often an overlooked component when assessing the quality of care structure, processes, and outcomes for CSHCN [4]. In 2003, an Institute of Medicine Report identified 7 key processes of care for CSHCN: care planning, use of preventive services, access to specialists, ancillary services, mental health and dental services, and care coordination [5]. The report failed to address, however, the cumulative and interrelated effects of these processes - which is to say, how the WOC operates within a multi-component dynamic system.
To synthesize and extend our current understanding of the parental WOC for CSHCN, we created a conceptual model via a systematic review of the published literature, aiming to provide a representative synopsis of both empirical findings and perspectives, which can then be used to "clarify, describe, and organize ideas" about how to improve the quality of care for CSHCN [6]. As an initial point of entry into the topic, we located the WOC concept at the intersection of the theoretical frameworks of the sociology of work[7], the psychology of coping [8], and the emerging field of complex systems [9,10]. Taken separately, these frameworks pose interesting and important questions, such as: Why are certain tasks identified as valuable and others are not, and why are specific tasks assigned to specific persons? How do people cope with stressful life events, and how do they use resources in other areas of their lives to do this? How do people's responses to events shape, in ways both predicable and unpredictable, future events? When combined, a conceptual model synthesizing these three frameworks both specifies the tasks inherent to the WOC while sketching an integrated model of how the dynamic WOC system operates as parents attempt to mount an adaptive response to the challenging circumstances of parenting a child with special health care needs.
Methods
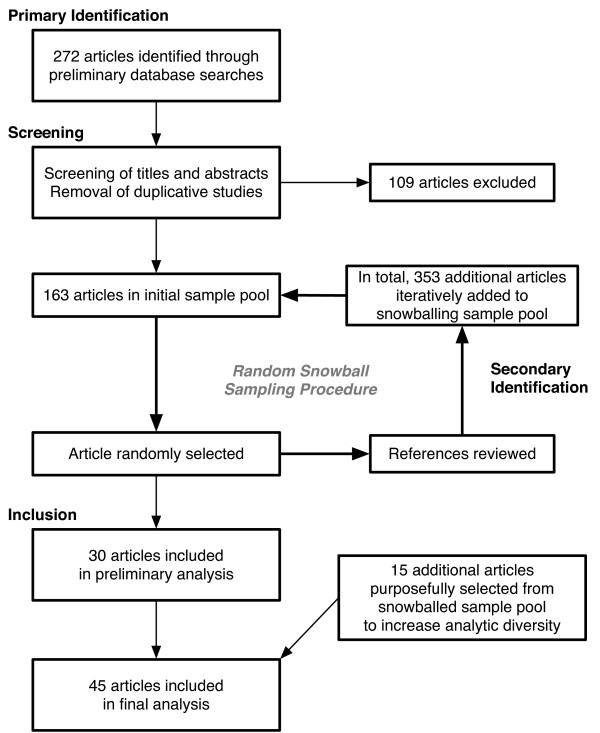
We performed a systematic literature review in multiple databases, and also reviewed the reference sections of articles randomly selected for analysis (Table 1 provides additional information regarding the search [11]). Inclusion criteria were purposefully broad, aiming to capture the range of research questions and methods. We excluded articles focused on non-parental caregivers (such as nurses or home health aids, but including other parental adults such as foster parents or extended family members), caregivers of aging parents, or articles on bereaved parents whose children had previously died. The following databases were reviewed: PubMed, MEDLINE, PsycINFO (Psychological Abstracts), and CINAHL (Cumulative Index to Nursing and Allied Health Literature). Combining randomization with snowball sampling approaches, our strategy, conducted by 2 independent reviewers, proceeded as follows (Figure 1): Using the specified search terms and eligibility criteria, 272 articles were initially retrieved from the databases. We reviewed the titles and abstracts, culling the initial set down to 163 articles. The titles of these pertinent articles were listed in alphabetical order and enumerated from first to last (N1). Using a random number generator (available at http://www.random.org), a number was selected between 1 and N1, corresponding to a unique article. The corresponding article was read, relevant data or concepts were abstracted, and the article's references were reviewed (by reading titles and abstracts), with all newly identified relevant articles added to the list of pertinent articles. The new augmented list was re-enumerated from 1 to N2; a second number was randomly selected between 1 and N2; and the second article was identified, the results analyzed and abstracted, and the references reviewed. This procedure was repeated until the review process had reached a point of thematic saturation, where additional successive articles were no longer adding new information or concepts [12].
Table 1.
Systematic review methodology
| Methods topics | Description | Rationale |
|---|---|---|
| Eligibility Criteria | ||
| Years | All | To assess change in patterns of reporting over time. |
| Language | English only | Study authors were only fluent in English. |
| Publication status | Peer reviewed journals | Peer review set minimum criteria for quality, journals used as primary medium for communication of information. |
| Information sources | ||
| Databases | PUBMED, PSYCINFO, CINAHL, and SOCIOLOGICAL ABSRACTS | Multiple databases were selected to provide access to a breadth of journals. |
| References | Review of reference sections | Provided additional articles not found in database searches. |
| Search | PUBMED example 1: "work+care+burden+pediatric" 2: "caregiving+coping+child+chronic" 3: "caring+children+chronic+disease+parents" 4: "caregivers+role+strain+child" |
Multiple searches using different terms revealed different journal articles to review. |
| Study selection | See figure 1 | |
| Data collection process | Data extracted from 30 journal articles chosen in random order, and 15 additional articles purposefully selected to increase diversity of sample | Used to prevent bias while at the same time sampling from entire population of articles. |
| Data items | See Tables 3 and 4 | Code list generated from qualitative methods based on Grounded Theory (Strauss & Corbin 1987). |
| Summary measures | See Tables 3 and 4 | Categories based on code list. |
| Synthesis of results | Theoretical model used to organize codes/categories | Theoretical model based on data as well as theories of work, coping, and complex systems. |
| Risk of bias across studies | "Medicalization" of work of care in peer review journals, exclusion of lay literature | Journal audience is comprised of medical and research personnel. |
Figure 1.
Procedure for systematic identification and selection of included articles.
With the above procedure, we ultimately identified 516 published articles in English, which were analyzed in random order until thematic saturation was achieved (n = 30). Fifteen additional articles were purposefully sampled from the titles of the remaining 486 references to increase the representation of longitudinal observational studies (n = 5), intervention studies (n = 5), and studies focused on minority populations (n = 5), bringing the total number included in this review to 45 papers.
Using an iterative process, a preliminary list of WOC codes was created and revised following the guidelines of grounded theory [13]. We used this coding strategy to systematically identify and organize the components of the work of care into a conceptual model, based on numerous conversations among the authors, feedback from colleagues who work extensively with CSHCN, and concepts from the frameworks of the sociologies of work, coping, and complex systems.
Results
Articles addressing parental WOC associated with CSCHN were published in 199 different journals devoted to pediatrics and allied disciplines, with 123 journals publishing one article only and 9 journals publishing more than 10 articles (Table 2). Most studies were qualitative research studies (70%) or literature reviews (26%). The majority of research studies were cross-sectional and observational (70%).
Table 2.
Study information for articles retrieved using databases, iterative review of each paper's references, and purposefully
| N | |
|---|---|
| Total sample pool of 516 articles from 199 journals | |
| Mean articles per journal | 2.6 |
| Number of journals with one article only | 123 |
| Number of journals with 10 or more articles | 9 |
| Randomly selected 30 articles from 24 journals | N (%) |
| Retrieved from | |
| PUBMED | 14 (47%) |
| Reference sections of articles | 9 (30%) |
| Other databases | 7 (23%) |
| Study type | |
| Qualitative (Interviews, Focus Groups, Ethnography) | 13 (43%) |
| Literature reviews+ | 8 (26%) |
| Quantitative (Survey, Time diaries) | 7 (20%) |
| Mixed methods | 2 (7%) |
| Randomized Intervention Studies | 0 |
| Study period | |
| Cross-sectional or one visit | 21 (70%) |
| Longitudinal or multiple visits | 1 (3%) |
| N/a (literature review) | 8 (27) |
| Contained visual model | |
| Yes | 5 (17%) |
| No | 25 (83%) |
| Disease type | |
| Unspecified (CSCHN, Chronic Illness, Disability) | 16 (53%) |
| Asthma | 3 (10%) |
| Epilepsy | 2 (7%) |
| Assisted by medical technology | 2 (7%) |
| Type 1 Diabetes | 2 (7%) |
| Other* | 5 (17%) |
| Country of study site | |
| United States | 14 (47%) |
| Australia, Canada, U.K. | 11 (37%) |
| Other** | 5 (17%) |
| Gender of parent-participants | |
| Mothers only | 5 (17%) |
| Mothers and fathers eligible, greater than 55% mothers | 7 (23%) |
| Mothers and fathers eligible, less than or equal to 55% mothers | 3 (10%) |
| Fathers only | 2 (7%) |
| Unspecified | 5 (17%) |
| N/a (literature review) | 8 (27%) |
| Addressed racial or ethnic minorities | |
| Yes | 1 (3%) |
| No | 29 (97%) |
| Purposefully selected 15 additional articles from 10 journals | |
| Longitudinal observational studies | 5 (33%) |
| Intervention studies | 5 (33%) |
| Addressed racial, ethnic, or very poor minorities | 5 (33%) |
+Included only 1 Literature Review with explicit search criteria. * Other disease includes 1 of each of the following: Anorexia, Cancer, Juvenile Rheumatoid Arthritis, Schizophrenia, and Infants At-Risk of SIDS.
** Other country includes 1 of each of the following: Germany, New Zealand, Sweden, Switzerland, and 1 study comparing U.S. and Icelandic populations
Work of care components
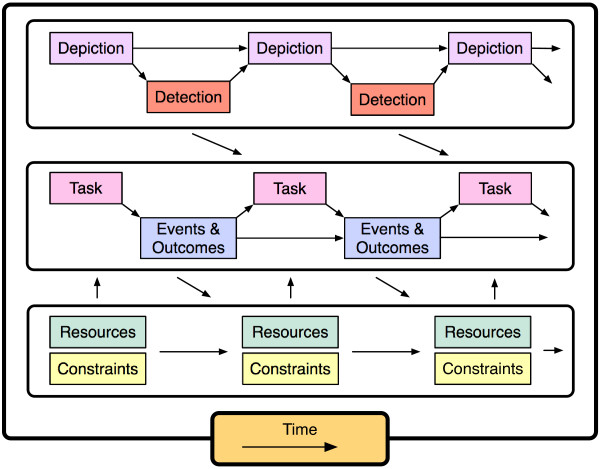
We organized our findings within the framework of a conceptual model developed over the course of performing this review. Figure 2 illustrates the proposed relationships among the following components: (1) performance of tasks, (2) occurrence of events and pursuit of valued outcomes, (3), use of resources and limits of constraints, (4) passage of time, and (5) mentally depicting the situation and detecting problems and opportunities.
Figure 2.
Core components of the dynamic system of parental work of care.
(1) Performance of Tasks
The work of care, on the surface, is all about tasks: the things parents do to achieve the aims of caring for their child, their family, and themselves. These tasks vary greatly, from medication management for a child with asthma [14-16] to completing the extensive paperwork required to receive insurance coverage for a child on a ventilator receiving care at home [17]. Tasks pertaining to the care of the child also include communicating and collaborating with medical professionals [18-20], crisis care, intensive care and emergency room visits [19-23], decision-making about which tasks to take on and who should perform them [15,17,19,24], seeking medical information, and learning new skills [17-20,22,24]. Parents must also continue to perform the regular tasks of parenting, such as providing emotional support to the child and helping him or her with normal developmental needs [19,24-28].
Additionally, parents engage in a variety of WOC tasks pertaining to the family and caregiver including creating daily routines and maintaining a sense of "normal" life [17,21,29,30], caring for siblings [17,29,31-35], managing paid employment [31-34,36] and household chores [17,22,32,33,37], helping and supporting each other [15,19,22,23,29], and communicating skillfully with other family members about the situation [19,38].
The parent must also perform WOC tasks for her- or himself that include both self-care and finding support. Self-care, which in the literature is focused predominantly on emotional management [19,22,23,25,26,30,37-39], should also include attention to diet, exercise and relaxation [22,32,33,40], and may include personal spiritual or religious practices such as prayer or meditation [19,38,40,41]. Finding support includes both maintaining communication with friends and family [19,26,32,33,42,43], and seeking the support of other families in similar situations through formal support groups as well as internet-based groups [17-19,26,33,38,44]. The complete list of WOC tasks is presented in Table 3.
Table 3.
Work of Care Tasks
| Category | Codes | Papers |
|---|---|---|
| CHILD WITH SPECIAL HEALTH CARE NEEDS (CSHCN) CARE WORK | ||
| Medical tasks | Medications and care of technical devices | [15,18,21,24,25,30,37,52,55,56] |
| Management | Overall management | [15,18,19,22,23,26,38,39,56] |
| Collaboration with medical professionals | [18-20] | |
| Bureaucracy/paperwork | [17,19,22,50] | |
| Crisis care and emergency room visits | [19,21-23,57] | |
| Monitoring | Constant awareness of child's health status | [15,18,22,25,38,42,52,58] |
| Decision Making | Deciding which tasks to take on, and which roles. | [15,17,19,24] |
| Education | Seeking medical information/skills training | [17-20,22,24,46] |
| Parenting tasks | Emotional support and developmental needs | [19,20,24-28] |
| FAMILY CARE WORK | ||
| Day-to-day | Daily routines and "normal" life, time management | [17-19,21-23,26,29,30,32,33,46,58] |
| Division of labor | Care of siblings | [17,22,23,29,31,32,35,38,52,58] |
| Employment | [31-34,36] | |
| Household chores | [17,22,32,33,37] | |
| Helping and supporting each other | [15,19,22,23,26,29,30,59] | |
| Communication | Talking with other family members about situation | [19,38,43] |
| PARENTAL SELF CARE WORK | ||
| Self-care | Emotional management | [19,22,23,25,26,30,37-41,43] |
| Diet, exercise, and relaxation | [22,32,33,40] | |
| Personal religious practice (i.e. prayer) | [19,38,40,41] | |
| Finding support | Maintaining communication with friends | [19,26,32,33,42,57] |
| Support of other families in similar situations | [17-19,26,33,38,44,46] | |
| SOCIETAL WORK | ||
| Advocacy | Educating others | [19,26] |
Individual tasks are not performed in a vacuum. A task may be combined synergistically with other tasks, such as when the completion of one task either aids in the performance of another, or reduces the second task's importance. For example, parents taught the task of administering a rectal medication for seizures in their children with epilepsy had fewer ER visits than parents who were not taught the procedure [21]. Since ER visits may also be considered a task, the introduction of the former task had the ability to diminish the latter. Tasks, however, may also combine antagonistically when different tasks require large amounts of time and energy. For example, parents often have difficulty simultaneously caring for their child and maintaining paid employment [36].
(2) Occurrence of Events and Pursuit of Outcomes
Tasks do not affect other tasks directly. Rather, the performance of each task is followed by events or results in an outcome that then changes the situation, creating a feedback loop that changes or creates subsequent tasks. Events may be expected, such as the progression of issues associated with type 1 diabetes over time [30], or unexpected, such as managing acute emergencies during working hours [36] or being laid off from work, and may or may not be causally related to preceding task performance, and the occurrence of events may be difficult to predict in the immediate future.
In most instances, the primary motivational structure for the WOC is the pursuit of desired outcomes, which may be tied directly to improved health status for the child (such as the pursuit of a lower blood sugar for children with diabetes in order to prevent diabetes-related complications [30,37]), or more generally to improvements in the quality of life for the child [21,31] or parent (which could come about, for example, by a reduction in the stress associated with the WOC [31]), or even to a desire to adhere to medical advice, (for example in the management of adolescent asthma) [15]. Precisely which outcomes are being sought is due in large part to the process of depiction, described below.
(3) Influences of Resources/Constraints
Resources are elements that parents draw on in order to function efficiently, and have a Janus-like quality of enabling some actions while also imposing constraints due to the nature or quantity of the resources (Table 4). Resources/constraints can emanate directly from the child, or the parent, or be aspects of the larger situation. Differences in how groups of people respond to similar situations may be attributable to both current and historical resources/constraints. As with tasks, each potential resource/constraint interacts with other resources/constraints.
Table 4.
Work of Care Resources/Constraints
| Category | Codes | Papers |
|---|---|---|
| CHILD | ||
| Gender | How child's gender affects the situation | [14,17,37] |
| Disease | Diagnosis and prognosis | [24,32,37,41,45,60] |
| Severity, symptoms, and child's quality of life | [14,17,20,31,32,41,45,51,56] | |
| Episodic quality of illness and uncertainty | [41,42,49,57] | |
| Medical care | Type of technology or equipment | [31,42,45,52,58] |
| Frequency of treatments | [32,56]42 | |
| Age | Newborns, children, and adolescents | [14,15,17,33,45] |
| Transitioning to Adult Care | [24,27] | |
| Behavior | Cognitive and emotional function/expression | [14,32,45] |
| Functional ability/activity limitations | [14,32,45,61] | |
| Location | Home, hospital, or elsewhere | [14,17,20,25,31,37,47,51,58] |
| PARENT | ||
| Gender roles | How the roles of mothers and fathers differ | [14,30,31,37,41,49,52,56,59,61] |
| Mental health | Emotions, quality of life, and stress | [14,20,31,32,34,36-38,40,41,43,45,51,52,55,59,61,62] |
| Personality | Hardiness, self-esteem, and coping style | [56,57,59,61,63] |
| Physical health | Sleep, immune function | [33,55,58] |
| Knowledge | Medical and parenting skills and experience | [21,47] |
| Education level | [34,39] | |
| Social support | Availability of friends and family | [17,31,32,57-59,61,63] |
| FAMILY | ||
| Family structure | Family cohesion, including marital dynamics | [35,38,56,58,59,63] |
| Single parents | [14,31,34] | |
| Step parents and foster parents | [45,49] | |
| Siblings | [14,32,35,52,58] | |
| Finances | Employment, income, and expenses | [17,31,32,34,36,37,47,55,56,58,60] |
| Insurance and eligibility for services | [17,45,49,51,60] | |
| SOCIETY | ||
| Minority status | Race, ethnicity, language, culture, and SES | [15,28,47,50,51] |
| Geographic locale | Different regions, countries. Immobility. | [45,47,50,56,61] |
| Attitudes and norms | Disability and disease in childhood | [25,28] |
| Parental responsibility and gender norms | [24,25,28,41,47,49] | |
| Health services | Availability of care facilities and providers | [23,24,31,50] |
| Awareness of available services | [32,45] | |
| Political system | Government policies and funding | [17,31,34,36,45,47,50,56,58] |
To illustrate the category of resources/constraints, consider several examples. First, the age of children alters many of the WOC tasks. Newborn children are small and easier to hold, bathe, and transport, but also present constraints because of uncertain diagnoses, fragility associated with being very young, and the need for medical technologies that are appropriate for children of such a small size [42]. If the child lives until young adulthood, he or she is usually better able to care for himself or herself, both in terms of medication management and emotionally. Another set of problems, however, may emerge, both in terms of increasing behavioral problems [15,27] and limited health services availability [24,45].
Second, across the age spectrum, medical technologies aim to allow families to accomplish the major tasks of improving the child's medical stability and quality of life. From feeding and breathing tubes to wheelchairs, dialysis machines to cardiac monitors, each technology provides specific benefits, and each has its tasks: of complex cleaning and maintenance, and of emotional acceptance [31,46,47]. If the tasks associated with medical technologies are too great, medical technologies may cease to be seen as a valuable resource for families, and instead may become a constraint. In this way, it is possible to see how the tasks associated with certain resources can make those resources less desirable.
Third, both gender and mental health of the parents are important and interrelated resource/constraints. In general, mothers and fathers experience the work of care differently [30,31,37]. Mothers are usually the primary caregivers, and are more likely to feel that, if one parent needs to stay home to care for the sick child, they are responsible. In taking on the primary caregiver role, mothers are less likely to be employed outside the home, and within the home often focus on the tasks central to the child, leaving others to deal with household chores and siblings [31,33,48]. When work of care tasks increase and are more difficult, mothers may become more anxious or depressed [48]. But mothers also report positive mental health states, such as love and appreciation [39]. Fathers' roles and emotional responses may also be gender specific. Fathers report struggling with role strain, in particular the 'provider' role, and role confusion as tasks and responsibilities are divided within the household, and fathers may also experience the same emotional pain and struggles as mothers while receiving less attention and support [41]. Additionally, fathers try to be strong for others, which reduces their support seeking from spouses and others [30]. The presence of stepfathers [49] and foster parents [45], however, warn against overly simple generalizations regarding gender roles and role-related differences.
Finally, minority populations may (emphasizing the caveat that published studies are relatively limited) assign different meanings to their child's illness [28], have a greater acceptance of the labor required for the WOC [50,51], and simultaneously have greater difficulty establishing relationships with health care providers, elements that may be compounded by language barriers[50].
(4) The Constraints and Passage of Time
Time acts as a constraint to the number of tasks a family can accomplish, while also serving as the ever-changing backdrop to the WOC, leading to predictable and unpredictable, controllable and uncontrollable, outcomes and events [30,33,52]. Time restricts the availability to pursue other activities, either with the family or alone. In addition, over time, children - including ill children - and families grow and develop. These developmental changes continually alter and complicate the WOC in subtle and overt ways [53].
(5) Depicting Situations and Detecting Problems and Opportunities
A parent's interpretation or understanding of a child's medical situation and changes in that situation may or may not be conscious, yet it provides the foundation from which a parent executes particular tasks. Essentially, the meaning that parents give to their child's situation defines the WOC in important ways, and is likely to be related (in critical ways) to their beliefs about the large existential questions their child's illness presents [54]. For example, parents may question and try to understand their situation, and struggle to accept their child's condition [19,22,25,43]. Or parents may question their child's diagnosis and have their own interpretation of the illness's meaning [25,28,38]. Parents may also evaluate their situation on the basis of how 'in control' they feel, and become involved in tasks of care in such a way as to increase their level of control [18,19,41]. Another example of a depiction is when parents stress the positive, and try to stay optimistic about their situation [19,39,41]. The process by which families identify difficulties or problems and how they choose to focus on certain aspects while at the same time ignoring others, depends on the families' overall depiction of the situation.
Framed by their depiction of the situation, families detect problems. Often, detection is accomplished by constant monitoring [18,22,42]. If problems are not detected, care may inadequately meet the needs of the children. For example, in a study of parents of adolescents with asthma, parents perceived their adolescents to be more competent at self-care than the adolescents actually were [15]. How parents depict their situation and detect problems within it will affect the tasks they perform, and may be influenced by resources or lack thereof that aid or hinder these efforts.
Complex causal relationships and emergent phenomena
While relatively simple cause-effect relationships exist in the work of care - such as if a medicine dosage is either missed or overdosed then an untoward event can occur - the interrelationships among elements in each category with the WOC system can create downward or upward spirals of cascading events. Positive feedback loops, for instance, can potentially produce a sequence whereby the WOC results in a parent curtailing and then quitting work, with consequently less income and greater financial constraints, greater stress and reduced task efficiency, and poorer health status [31]. Similar feedback loops can operate in the other direction, for example in the COPE (Creating Opportunities for Parental Empowerment) intervention, wherein a shift in parental knowledge and skills can lead to stronger beliefs in their ability to manage the situation, and therefore less parental stress and fewer subsequent behavioral issues in the child [20]. Through the interaction of these relationships, the WOC acquires characteristics of a multilevel complex adaptive system, wherein the pursuit of specific health outcomes may or may not be aligned with the system's requirement for overall equilibrium [9,10].
Discussion
Across several domains in the published literature, multiple studies delineate the various components of the dynamic parental WOC system for CSHCN. We assert that in conceptually uniting this body of research, work is the most useful underlying construct. Work emphasizes not only the content of the multiple components of care, but also the process of how those core components interact in a dynamic system - a system that affects the health and wellbeing of these children and their families in ways that are critically important, but not yet fully understood. The dynamic WOC system framework established here is intended to sharpen the analytic focus on the complex, systemic interaction of these components of care. Through this framework, we hope to provide a map for more clearly understanding the work of care, and ways in which we can support both families and health care teams as they address the needs of children with special health care needs.
Strengths and limitations of our review
Our sample was based on a systematic review of the medical, nursing, psychological, and sociological literature on topics related to the WOC for children with special health care needs, and evaluated using a thorough randomization approach. Our analysis was organized according to a conceptual model with well-defined categories and directional arrows identifying plausible causal mechanisms. Our study had the major limitation, however, of focusing only on the professional literature to the exclusion of the numerous parent and lay resources that address WOC issues. We chose this strategy in order to better understand how the healthcare community, in particular, has addressed the parental WOC.
WOC and improving the quality of care
If the work of care for parents of CSHCN is, as our review and conceptual model suggests, a complex multilevel adaptive system, then efforts to improve the quality of care received by these children, aiming ultimately to improve their outcomes, must appreciate and grapple with several features of such systems. Chief among these are potential non-linear interdependencies among components of the work of care, which caution us that improvements in certain tasks of the work of care may affect the performance of other tasks, for better or for worse, either in a graded manner (more time performing one task results in an equivalent lessening of time performing another task) or at certain "tipping points" (when the performance of a task goes from barely sufficient to morbidly insufficient)[10]. Observational and interventional studies of parental WOC need to consider measurements from this systems perspective, including not only several process measures for different core components (such as presence of a care plan or a physician checklist), but also aspects of parental self-care (mental health screenings, coping mechanisms) and child outcomes (functional status or quality of life in various domains as well as morbidity and mortality). The system (including the patient and family's socioeconomic status and cultural context) also changes and adapts over time, suggesting both a need for longitudinal studies and for studies to consider potential effect mediators and moderators in both study design and sampling strategies.
Conclusions
The work of care warrants greater attention and investigation. Three topics in particular merit rigorous study. First, we need to improve our epidemiologic and sociological understanding of the WOC system. Is the volume of parental WOC truly increasing for the population of parents of CSHCN? What are the most prevalent or influential tasks, and how do key resources or constraints affect task performance? What are the most informative ways to gather and analyze dynamic WOC system data (such as prospective cohort studies and structural equation or non-parametric dynamic system modeling)? Second, we should examine how increases in the parental WOC load relate to changes in work efficiency, and potentially diminishing returns or errors of commission or omission, and develop methods to feasibly monitor and optimize workload. Third, we need to study the occupational health and safety of parents, and the role and impact of broader societal support (through programs such as family medical leave, health insurance benefits that include nursing and respite, and social security income supplementation). These are some of the tasks we need to perform to create new resources to better manage the work of care and improve the outcomes for children with CSHCN and their families.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
KRH participated in the design of the study, performed the data retrieval, analyzed and interpreted the data, drafted sections of the manuscript, revised the manuscript for key intellectual content, read and approved the final manuscript. AMB participated in the design of the study, performed the data retrieval, analyzed and interpreted the data, revised the manuscript for key intellectual content, read and approved the final manuscript. CF participated in the design of the study, analyzed and interpreted the data, drafted sections of the manuscript, revised the manuscript for key intellectual content, read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Kari R Hexem, Email: hexem@email.chop.edu.
Abigail M Bosk, Email: abbe.bosk@gmail.com.
Chris Feudtner, Email: feudtner@email.chop.edu.
Acknowledgements
We thank Mary Rourke, PhD, and Jane Kavanagh for their comments on this manuscript. Chris Feudtner had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was supported in part by The Pew Charitable Trusts. This funding body had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
References
- Bronzino JD, Smith VK, Wade ML. Medical Technology and Society: An Interdisciplinary Perspective. Cambridge: MIT Press; 1990. [Google Scholar]
- Tennant PW, Pearce MS, Bythell M, Rankin J. 20-year survival of children born with congenital anomalies: a population-based study. Lancet. 2010;375(9715):649–656. doi: 10.1016/S0140-6736(09)61922-X. [DOI] [PubMed] [Google Scholar]
- Bethell CD, Read D, Blumberg SJ, Newacheck PW. What is the prevalence of children with special health care needs? Toward an understanding of variations in findings and methods across three national surveys. Matern Child Health J. 2008;12(1):1–14. doi: 10.1007/s10995-007-0220-5. [DOI] [PubMed] [Google Scholar]
- Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- Adams K, Corrigan JM, (eds) Priority Areas for National Action: Transforming Health Care Quality. Washington D.C.: National Academies Press; 2003. [PubMed] [Google Scholar]
- Shojania K, McDonald KM, Wachter R, Owens D. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies, Vol 1: Series Overview and Methodology. Vol. 1. Stanford, CA; 2004. [PubMed] [Google Scholar]
- Grint K. The Sociology of Work: An Introduction. Malden, MA: Blackwell Publishers Inc; 1998. [Google Scholar]
- Snyder CR, (ed) Coping: The Psychology of What Works. New York: Oxford University Press; 1999. [Google Scholar]
- Meadows D. Thinking in Systems. White River Junction, VT: Chelsea Green Publishing; 2008. [Google Scholar]
- Miller JH, Page SE. Complex Adaptive Systems: An Introduction to Computational Models of Social Life. Princeton, NJ: Princeton University Press; 2007. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green B, Hall J. Qualitative Methods for Literature Reviews. Ann Rev Psychol. 1984;35:37–53. doi: 10.1146/annurev.ps.35.020184.000345. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of Qualitative Research: Second Edition. Thousand Oaks, CA: Sage Publications, Inc; 1998. [Google Scholar]
- Rydström I, Dalheim-Englund AC, Holritz-Rasmussen B, Möller C, Sandman PO. Asthma--quality of life for Swedish children. J Clin Nurs. 2005;14(6):739–749. doi: 10.1111/j.1365-2702.2005.01135.x. [DOI] [PubMed] [Google Scholar]
- Walders N, Drotar D, Kercsmar C. The allocation of family responsibility for asthma management tasks in African-American adolescents. J Asthma. 2000;37(1):89–99. doi: 10.3109/02770900009055432. [DOI] [PubMed] [Google Scholar]
- Georgiou A, Buchner DA, Ershoff DH, Blasko KM, Goodman LV, Feigin J. The impact of a large-scale population-based asthma management program on pediatric asthma patients and their caregivers. Ann Allergy Asthma Immunol. 2003;90(3):308–315. doi: 10.1016/S1081-1206(10)61799-1. [DOI] [PubMed] [Google Scholar]
- Aday LA, Wegener DH. Home care for ventilator-assisted children: implications for the children, their families, and health policy. Child Health Care. 1988;17(2):112–120. doi: 10.1207/s15326888chc1702_9. [DOI] [PubMed] [Google Scholar]
- Jerrett MD, Costello EA. Gaining control: parents' experiences of accommodating children's asthma. Clin Nurs Res. 1996;5(3):294–308. doi: 10.1177/105477389600500305. [DOI] [PubMed] [Google Scholar]
- Canam C. Common adaptive tasks facing parents of children with chronic conditions. J Adv Nurs. 1993;18(1):46–53. doi: 10.1046/j.1365-2648.1993.18010046.x. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Alpert-Gillis L, Feinstein NF, Crean HF, Johnson J, Fairbanks E, Small L, Rubenstein J, Slota M, Corbo-Richert B. Creating opportunities for parent empowerment: program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics. 2004;113(6):e597–607. doi: 10.1542/peds.113.6.e597. [DOI] [PubMed] [Google Scholar]
- Kriel RL, Cloyd JC, Hadsall RS, Carlson AM, Floren KL, Jones-Saete CM. Home use of rectal diazepam for cluster and prolonged seizures: efficacy, adverse reactions, quality of life, and cost analysis. Pediatr Neurol. 1991;7(1):13–17. doi: 10.1016/0887-8994(91)90099-7. [DOI] [PubMed] [Google Scholar]
- Sullivan-Bolyai S, Sadler L, Knafl KA, Gilliss CL. Great expectations: a position description for parents as caregivers: Part I. Pediatr Nurs. 2003;29(6):457–461. [PubMed] [Google Scholar]
- Whyte DA. A family nursing approach to the care of a child with a chronic illness. J Adv Nurs. 1992;17(3):317–327. doi: 10.1111/j.1365-2648.1992.tb01910.x. [DOI] [PubMed] [Google Scholar]
- Milliken PJ, Rodney PA. Parents as caregivers for children with schizophrenia: moral dilemmas and moral agency. Issues Ment Health Nurs. 2003;24(8):757–773. [PubMed] [Google Scholar]
- Young B, Dixon-Woods M, Findlay M, Heney D. Parenting in a crisis: conceptualising mothers of children with cancer. Soc Sci Med. 2002;55(10):1835–1847. doi: 10.1016/S0277-9536(01)00318-5. [DOI] [PubMed] [Google Scholar]
- Clawson JA. A child with chronic illness and the process of family adaptation. J Pediatr Nurs. 1996;11(1):52–61. doi: 10.1016/S0882-5963(96)80038-8. [DOI] [PubMed] [Google Scholar]
- Luther B. Age-specific activities that support successful transition to adulthood for children with disabilities. Orthop Nurs. 2001;20(1):23–29. doi: 10.1097/00006416-200101000-00006. [DOI] [PubMed] [Google Scholar]
- Holroyd EE. Chinese cultural influences on parental caregiving obligations toward children with disabilities. Qual Health Res. 2003;13(1):4–19. doi: 10.1177/1049732302239408. [DOI] [PubMed] [Google Scholar]
- Honey A, Halse C. The specifics of coping: parents of daughters with anorexia nervosa. Qual Health Res. 2006;16(5):611–629. doi: 10.1177/1049732305285511. [DOI] [PubMed] [Google Scholar]
- Sullivan-Bolyai S, Rosenberg R, Bayard M. Fathers' reflections on parenting young children with type 1 diabetes. MCN Am J Matern Child Nurs. 2006;31(1):24–31. doi: 10.1097/00005721-200601000-00007. [DOI] [PubMed] [Google Scholar]
- Thyen U, Kuhlthau K, Perrin JM. Employment, child care, and mental health of mothers caring for children assisted by technology. Pediatrics. 1999;103(6 Pt 1):1235–1242. doi: 10.1542/peds.103.6.1235. [DOI] [PubMed] [Google Scholar]
- O'Dell C, Wheless JW, Cloyd J. The personal and financial impact of repetitive or prolonged seizures on the patient and family. J Child Neurol. 2007;22(5 Suppl):61S–70S. doi: 10.1177/0883073807303070. [DOI] [PubMed] [Google Scholar]
- Crowe TK, Florez SI. Time use of mothers with school-age children: a continuing impact of a child's disability. Am J Occup Ther. 2006;60(2):194–203. doi: 10.5014/ajot.60.2.194. [DOI] [PubMed] [Google Scholar]
- Schuster MA, Chung PJ, Elliott MN, Garfield CF, Vestal KD, Klein DJ. Perceived effects of leave from work and the role of paid leave among parents of children with special health care needs. Am J Public Health. 2009;99(4):698–705. doi: 10.2105/AJPH.2008.138313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PD, Williams AR, Graff JC, Hanson S, Stanton A, Hafeman C, Liebergen A, Leuenberg K, Setter RK, Ridder L. et al. A community-based intervention for siblings and parents of children with chronic illness or disability: the ISEE study. J Pediatr. 2003;143(3):386–393. doi: 10.1067/S0022-3476(03)00391-3. [DOI] [PubMed] [Google Scholar]
- George A, Vickers MH, Wilkes L, Barton B. Working and Caring for a Child with Chronic Illness: Challenges in Maintaining Employment. Employ Respons Rights J. 2008;20:165–176. doi: 10.1007/s10672-008-9065-3. [DOI] [Google Scholar]
- Landolt MA, Ribi K, Laimbacher J, Vollrath M, Gnehm HE, Sennhauser FH. Posttraumatic stress disorder in parents of children with newly diagnosed type 1 diabetes. J Pediatr Psychol. 2002;27(7):647–652. doi: 10.1093/jpepsy/27.7.647. [DOI] [PubMed] [Google Scholar]
- Coffey JS. Parenting a child with chronic illness: a metasynthesis. Pediatr Nurs. 2006;32(1):51–59. [PubMed] [Google Scholar]
- Chernoff RG, List DG, DeVet KA, Ireys HT. Maternal reports of raising children with chronic illnesses:the prevalence of positive thinking. Ambul Pediatr. 2001;1(2):104–107. doi: 10.1367/1539-4409(2001)001<0104:MRORCW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Minor HG, Carlson LE, Mackenzie MJ, Zernicke K, Jones L. Evaluation of a Mindfulness-Based Stress Reduction (MBSR) program for caregivers of children with chronic conditions. Soc Work Health Care. 2006;43(1):91–109. doi: 10.1300/J010v43n01_06. [DOI] [PubMed] [Google Scholar]
- McNeill T. Fathers' experience of parenting a child with juvenile rheumatoid arthritis. Qual Health Res. 2004;14(4):526–545. doi: 10.1177/1049732303262374. [DOI] [PubMed] [Google Scholar]
- Maclean BL. Parenting of at-risk infants in the face of uncertainty: home apnea monitoring of subsibs. J Pediatr Nurs. 1999;14(3):201–209. doi: 10.1016/S0882-5963(99)80013-X. [DOI] [PubMed] [Google Scholar]
- Vickers MH Bounded Grief at Work: Working and Caring for Children with Chronic Illness Illness, Crisis & Loss 2005133201–218.21977727 [Google Scholar]
- Ireys HT, Sills EM, Kolodner KB, Walsh BB. A social support intervention for parents of children with juvenile rheumatoid arthritis: results of a randomized trial. J Pediatr Psychol. 1996;21(5):633–641. doi: 10.1093/jpepsy/21.5.633. [DOI] [PubMed] [Google Scholar]
- Ray LD. Categorical service allocation and barriers to care for children with chronic conditions. Can J Nurs Res. 2005;37(3):86–102. [PubMed] [Google Scholar]
- Nicholas DB, Keilty K. An evaluation of dyadic peer support for caregiving parents of children with chronic lung disease requiring technology assistance. Soc Work Health Care. 2007;44(3):245–259. doi: 10.1300/J010v44n03_08. [DOI] [PubMed] [Google Scholar]
- Cohen MH. The technology-dependent child and the socially marginalized family: a provisional framework. Qual Health Res. 1999;9(5):654–668. doi: 10.1177/104973299129122144. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Butensky E, Harmatz P, Vichinsky E, Heyman MB, Acree M, Wrubel J, Wilson L, Folkman S. Caregiving time in sickle cell disease: psychological effects in maternal caregivers. Pediatr Blood Cancer. 2007;48(1):64–71. doi: 10.1002/pbc.20792. [DOI] [PubMed] [Google Scholar]
- Zarelli DA. Role-governed behaviors of stepfathers in families with a child with chronic illness. J Pediatr Nurs. 2009;24(2):90–100. doi: 10.1016/j.pedn.2008.02.029. [DOI] [PubMed] [Google Scholar]
- Rehm RS. Legal, financial, and ethical ambiguities for Mexican American families: caring for children with chronic conditions. Qual Health Res. 2003;13(5):689–702. doi: 10.1177/1049732303013005007. [DOI] [PubMed] [Google Scholar]
- Shin SH, Brown TA. Racial and ethnic disparities in caregiver strain and the use of child mental health services: a structural equation model. Psychiatr Serv. 2009;60(8):1039–1045. doi: 10.1176/appi.ps.60.8.1039. [DOI] [PubMed] [Google Scholar]
- Wasserman AL. A prospective study of the impact of home monitoring on the family. Pediatrics. 1984;74(3):323–329. [PubMed] [Google Scholar]
- Kazak AE, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer MA, Rourke M. An integrative model of pediatric medical traumatic stress. J Pediatr Psychol. 2006;31(4):343–355. doi: 10.1093/jpepsy/jsj054. [DOI] [PubMed] [Google Scholar]
- Kazak AE, McClure KS, Alderfer MA, Hwang WT, Crump TA, Le LT, Deatrick J, Simms S, Rourke MT. Cancer-related parental beliefs: the Family Illness Beliefs Inventory (FIBI) J Pediatr Psychol. 2004;29(7):531–542. doi: 10.1093/jpepsy/jsh055. [DOI] [PubMed] [Google Scholar]
- Kuster PA, Merkle CJ. Caregiving stress, immune function, and health: implications for research with parents of medically fragile children. Issues Compr Pediatr Nurs. 2004;27(4):257–276. doi: 10.1080/01460860490884165. [DOI] [PubMed] [Google Scholar]
- Svavarsdottir EK, Rayens MK, McCubbin M. Predictors of adaptation in Icelandic and American families of young children with chronic asthma. Fam Community Health. 2005;28(4):338–350. doi: 10.1097/00003727-200510000-00006. [DOI] [PubMed] [Google Scholar]
- Hirose T, Ueda R. Long-term follow-up study of cerebral palsy children and coping behaviour of parents. J Adv Nurs. 1990;15(7):762–770. doi: 10.1111/j.1365-2648.1990.tb01904.x. [DOI] [PubMed] [Google Scholar]
- Hewitt-Taylor J. Caring for children with complex needs: staff education and training. J Child Health Care. 2005;9(1):72–86. doi: 10.1177/1367493505050506. [DOI] [PubMed] [Google Scholar]
- Dahlquist LM, Czyzewski DI, Jones CL. Parents of children with cancer: a longitudinal study of emotional distress, coping style, and marital adjustment two and twenty months after diagnosis. J Pediatr Psychol. 1996;21(4):541–554. doi: 10.1093/jpepsy/21.4.541. [DOI] [PubMed] [Google Scholar]
- Lukemeyer A, Meyers M, Smeeding T. Expensive Children in Poor Families: Out of Pocket Expenditures for the Care of Disabled and Chronically Ill Children in Welfare Families. Journal of Marriage and the Family. 2000;62:399–415. doi: 10.1111/j.1741-3737.2000.00399.x. [DOI] [Google Scholar]
- Silver EJ, Westbrook LE, Stein RE. Relationship of parental psychological distress to consequences of chronic health conditions in children. J Pediatr Psychol. 1998;23(1):5–15. doi: 10.1093/jpepsy/23.1.5. [DOI] [PubMed] [Google Scholar]
- Blader JC. Which family factors predict children's externalizing behaviors following discharge from psychiatric inpatient treatment? J Child Psychol Psychiatry. 2006;47(11):1133–1142. doi: 10.1111/j.1469-7610.2006.01651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tak YR, McCubbin M. Family stress, perceived social support and coping following the diagnosis of a child's congenital heart disease. J Adv Nurs. 2002;39(2):190–198. doi: 10.1046/j.1365-2648.2002.02259.x. [DOI] [PubMed] [Google Scholar]