Abstract
Background:
Combined injuries to the spinal cord and brachial plexus present challenges in the detection of both injuries as well as to subsequent treatment. The purpose of this study is to describe the epidemiology and clinical factors of concomitant spinal cord injuries in patients with a known brachial plexus injury.
Methods:
A retrospective review was performed on all patients who were evaluated for a brachial plexus injury in a tertiary, multidisciplinary brachial plexus clinic from January 2000 to December 2008. Patients with clinical and/or imaging findings for a coexistent spinal cord injury were identified and underwent further analysis.
Results:
A total of 255 adult patients were evaluated for a traumatic traction injury to the brachial plexus. We identified thirty-one patients with a combined brachial plexus and spinal cord injury, for a prevalence of 12.2%. A preganglionic brachial plexus injury had been sustained in all cases. The combined injury group had a statistically greater likelihood of having a supraclavicular vascular injury (odds ratio [OR] = 22.5; 95% confidence interval [CI] = 1.9, 271.9) and a cervical spine fracture (OR = 3.44; 95% CI = 1.6, 7.5). These patients were also more likely to exhibit a Horner sign (OR = 3.2; 95% CI = 1.5, 7.2) and phrenic nerve dysfunction (OR = 2.5; 95% CI = 1.0, 5.8) compared with the group with only a brachial plexus injury.
Conclusion:
Heightened awareness for a combined spinal cord and brachial plexus injury and the presence of various associated clinical and imaging findings may aid in the early recognition of these relatively uncommon injuries.
Level of Evidence:
Therapeutic Level IV. See Instructions to Authors for a complete description of levels of evidence.
Combined injuries to the spinal cord and brachial plexus have been previously thought to be relatively rare and can be a diagnostic challenge due to the combination of central and peripheral nerve injury. Accurate diagnosis of a brachial plexus injury or spinal cord injury is often delayed and obscured by the neurologic deficits caused by the other injury. In a patient who has sustained polytrauma that includes an overt spinal cord injury, the brachial plexus injury can be overlooked due to the attention mandated for the more acute, life-threatening associated injuries or because the brachial plexus injury is erroneously and presumptively attributed to the spinal cord lesion1-3. Conversely, a spinal cord injury that is associated with subtle neurologic deficits or upper motor neuron signs can go undetected in patients with an obvious brachial plexus lesion and can greatly alter or limit the reconstructive options for treating the brachial plexus injury.
The frequency of brachial plexus injury in patients with spinal cord injury has been reported to be 0.6% to 1.8%1,3-5, but limited data are available on the prevalence of concomitant spinal cord injury in patients with a brachial plexus injury. Root avulsions have been reported to cause Brown-Séquard syndrome, with a prevalence of 2% to 5% in patients with brachial plexus injuries6-8. Direct injury to the spinal cord from the traumatic event or indirect injuries due to nerve root avulsions or intradural nerve root ruptures have been implicated as the cause of these combined injuries1,3,9-11.
Operative treatment of a brachial plexus injury can be influenced and limited by neurologic deficits and dysfunctional upper motor neurons from a coexistent spinal cord injury. Accurate detection of an associated spinal cord injury in a patient with a brachial plexus injury may positively influence the ultimate surgical procedure to achieve successful outcomes. The purpose of this retrospective study was threefold: to describe the prevalence of concomitant spinal cord injury in patients with a known brachial plexus injury, to evaluate the characteristics of patients with combined spinal cord and brachial plexus injury, and to determine the factors associated with the presence of a combined spinal cord and brachial plexus injury.
Materials and Methods
Prevalence of Concomitant Spinal Cord Injury in Patients with Brachial Plexus Injury
Patient Selection
After approval from our institutional review board, the medical records of all patients evaluated for brachial plexus injury in our multidisciplinary brachial plexus clinic from January 2000 to December 2008 were retrospectively reviewed. Patients were excluded if they were less than eighteen years old at the time of evaluation, had sustained a penetrating or iatrogenic injury, had terminal branch injuries without a proximal brachial plexus injury, or had a nontraumatic brachial plexopathy.
Spinal Cord Injury Identification
To identify the presence of a concomitant spinal cord injury, the medical records were reviewed for the presence of clinical symptoms and/or signs as well as imaging evidence (magnetic resonance imaging [MRI] and computed tomography [CT], when available) that was consistent with a coexistent spinal cord injury. All patients had been acutely evaluated and treated in our emergency department or at another facility and were evaluated electively in a delayed fashion by the multidisciplinary team at the brachial plexus clinic. This evaluation initially included a complete assessment by a neurologist followed by a focused evaluation with at least two of the three senior authors: R.J.S. (Department of Neurosurgery), A.T.B. (Department of Orthopedic Surgery/Hand/Microsurgery), and A.Y.S. (Department of Orthopedic Surgery/Hand/Microsurgery).
Spinal cord injury was defined as an insult to the spinal cord resulting in a change, either temporary or permanent, in its normal motor, sensory, or autonomic function12. Clinical evidence of spinal cord injury was defined as a temporary or permanent sensory, motor, or sphincter deficit on the basis of the history and/or the clinical examination (major clinical evidence), or by the presence of upper motor neuron signs, such as hyperreflexia, extensor plantar response, the Hoffmann sign, or clonus (minor clinical evidence). Imaging evidence of spinal cord injury was defined as a positive spinal cord abnormality (T2-weighted signal intensity within the cord and/or cord-level subdural or epidural hematoma, or transection) on images or reports of cervical CT scans, CT myelography, or MRI.
Classification of Spinal Cord Injury
In view of the retrospective nature of this study and the nonacute (delayed) evaluation of patients in the brachial plexus clinic, the concomitant spinal cord injury was classified as being “definitive,” “probable,” or “possible” (Table I). A “definitive” spinal cord injury was defined as major clinical evidence and imaging evidence of a spinal cord injury; a “probable” spinal cord injury was defined as minor clinical evidence and imaging evidence of a spinal cord injury or major clinical evidence of a spinal cord injury without imaging available for review; and, lastly, a “possible” spinal cord injury was defined as minor clinical evidence of a spinal cord injury without imaging available for review. There were no patients with major or minor clinical evidence who did not have imaging findings consistent with a spinal cord injury when imaging studies were available. If possible, in patients with marked clinic evidence of spinal cord injury, the level and type of spinal cord injury was determined according to the American Spinal Injury Association (ASIA) classification system12.
TABLE I.
Spinal Cord Injury Classification Scheme
| Clinical Evidence(History and Physical Examination) |
||
| Radiological Evidence (Reports and Images) | Major | Minor |
| Available and positive | Definitive | Probable |
| Unavailable | Probable | Possible |
Characteristics of Patients with Combined Spinal Cord Injury and Brachial Plexus Injury
Clinical information including the age, sex, side of injury, arm dominance, mode of injury, extent of brachial plexus injury, and associated injuries were obtained. Brachial plexus injury was classified as complete when all brachial plexus elements (cervical nerves C5 to T1) were involved (partial or complete motor and/or sensory deficit) and as incomplete when one or more brachial plexus elements were spared. Preganglionic injuries were diagnosed in conjunction with electromyography (EMG)/nerve conduction studies, CT myelogram, and intraoperative findings. The Injury Severity Score (ISS) of patients with a combined injury involving the spinal cord and brachial plexus was calculated by review of the medical records, including the available records from other institutions13.
Factors Associated with the Presence of a Combined Spinal Cord Injury and Brachial Plexus Injury
To assess if certain factors were associated with the presence of a combined spinal cord and brachial plexus injury, several clinical and imaging characteristics were compared between the brachial plexus injured patients who did or did not have a concomitant spinal cord injury during the study period. The assessed clinical factors included the age, mode of injury, extent of brachial plexus injury (complete or incomplete), preoperative score on the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire4, preoperative visual analog scale (VAS), the presence of a Horner sign, and any associated injuries (i.e., supraclavicular or infraclavicular vascular lesions, axial spine fractures, and cervical spine fractures). Subaxial cervical spine injuries were further classified under the Subaxial Injury Classification system (SLIC) and the Allen-Ferguson classification14,15. The assessed imaging factors included the presence and number of pseudomeningoceles on imaging (MRI, CT, and/or CT myelography) and evidence of phrenic nerve dysfunction (determined by the presence of an elevated hemidiaphragm on anteroposterior chest radiographs with or without inspiratory and expiratory views). The ISS was calculated as described by Baker et al.13.
Statistical Analysis
The data were summarized and reported descriptively with use of standard methods: categorical variables were summarized as count over denominator and percentage, while continuous variables were summarized as mean plus standard deviation. To assess if certain factors were associated with the presence of a concomitant spinal cord injury, the clinical and imaging characteristics of patients with brachial plexus injury who did or did not have concomitant spinal cord injury were compared. Continuous variables were evaluated with use of nonparametric Wilcoxon rank-sum tests. Chi-square tests were used to compare categorical variables; when expected cell counts were less than five, Fisher exact tests were performed. Univariate logistic regression was also used to evaluate outcomes comprised of binary variables. The results of the comparisons of the two patient groups are reported in the tables with use of the nominal p values as well as p values adjusted with use of the method of Benjamini and Hochberg, in order to protect against potential type-I error16. All statistical tests were two-sided, and the threshold of significance was set at α = 0.05.
Source of Funding
There was no external source of funding in this study.
Results
Prevalence of Concomitant Spinal Cord Injury in Patients with Brachial Plexus Injury
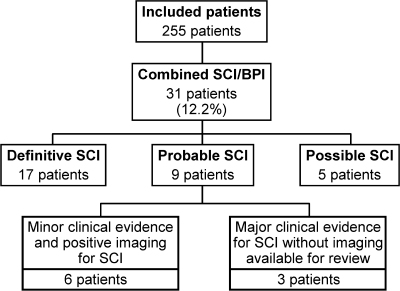
During the study period, 481 patients were evaluated for brachial plexus injury in our brachial plexus clinic. A total of 255 adult patients with closed, traction injuries to the brachial plexus were included in our study (see Appendix). Thirty-one patients had a coexistent spinal cord injury, for a prevalence of 12.2%, including seventeen “definitive,” nine “probable,” and five “possible” cases of spinal cord injury (Fig. 1).
Fig. 1.
Classification of spinal cord injuries (SCI) in patients who have a brachial plexus injury (BPI).
There were twenty patients with major clinical evidence for a spinal cord injury. Identifiable spinal cord injury syndromes and patterns were noted in eight patients. Of these eight patients, two (0.8%) had sustained a complete spinal cord injury (C8 ASIA A [cord transection] and T2 ASIA A), four (1.6%) had Brown-Séquard syndrome, and two (0.8%) had an anterior cord syndrome. In the remaining twelve patients, sensory and/or motor dysfunction was present in the lower extremities in six patients and in the contralateral upper extremity in one patient, and five patients had sole neurologic deficits in the involved upper extremity with imaging findings consistent with concomitant spinal cord injury.
There were twenty-two patients with available imaging confirming a spinal cord abnormality. There was increased T2 intensity within the cervical cord on MRI in nineteen patients, epidural hematoma in one patient, subdural hematoma in one patient, and both epidural and subdural hematomas in one patient.
Characteristics of Patients with Combined Spinal Cord Injury and Brachial Plexus Injury
Of the thirty-one patients with a combined spinal cord injury and brachial plexus injury, there were twenty-two men and nine women (Table II). The mean age at the time of injury was 33.6 ± 11.9 years (range, eighteen to sixty-three years). The dominant extremity sustained the brachial plexus injury in eleven (35.5%) patients. In the four patients with Brown-Séquard syndrome, the primary upper motor neuron lesion occurred on the ipsilateral side as the brachial plexus injury. The mean time from injury to consultation in our brachial plexus clinic was 9.1 months (range, zero to seventy-two months).
TABLE II.
Demographic Data for Patients with Combined Spinal Cord and Brachial Plexus Injuries
| Sex | |
| Male | 22 |
| Female | 9 |
| Age (yr)* | 33.6 ± 11.9 (18 to 63) |
| Injured extremity | |
| Left | 18 |
| Right | 13 |
| Time from injury to consultation (mo)† | 9.1 (0 to 72) |
| Mode of injury | |
| High-speed | 23 |
| Low-speed | 5 |
| Work-related | 2 |
| Skiing | 1 |
| Loss of consciousness | 21 |
Values are given as the mean and the standard deviation, with range in parentheses.
Values are given as the mean, with the range in parentheses.
The mode of injury was due to a “high-speed” (i.e., ≥20 mph) motorized (automobile, motorcycle, or all-terrain vehicle) accident in twenty-three patients (74.2%), a “low-speed” (<20 mph) motorized accident in five patients (16.1%), a work-related accident in two patients (6.5%), and a skiing accident in one patient (3.2%) (Table II). The brachial plexus lesion was complete in twenty-three (74.2%) and incomplete in eight (25.8%) patients (Table III). These incomplete brachial plexus injuries consisted of upper trunk (C5-C6) (n = 4) and upper trunk plus C7 (n = 4) lesions. A preganglionic injury had been sustained in at least one level in all patients with a combined brachial plexus and spinal cord injury.
TABLE III.
Type of Combined Brachial Plexus and Spinal Cord Injury
| Type of Injury | Number of Injuries (%) |
| Brachial plexus injury | |
| Complete | 23 (74.2%) |
| Incomplete | 8 (25.8%) |
| Upper trunk (C5-C6) | 4 |
| Upper trunk + C7 | 4 |
| Preganglionic | 31 (100%) |
| Spinal cord injury | |
| Definitive | 17 |
| Probable | 9 |
| Possible | 5 |
| Spinal cord injury | |
| Complete spinal cord injury | 2 (0.78%) |
| Brown-Séquard syndrome | 4 (1.6%) |
| Anterior cord syndrome | 2 (0.78%) |
All patients had associated injuries in addition to their spinal cord injury and brachial plexus injury (see Appendix). The most common associated injury was to the head or face, present in twenty-four patients (77.4%). Loss of consciousness at the time of injury occurred in twenty-one patients (67.7%). Spine fractures had been sustained in twenty patients (64.5%). Cervical spine fractures occurred in fifteen patients (48.4%); these included occipital fractures in three patients, C1 lateral mass fractures in two patients, and a C2 lateral mass fracture in one patient. There were twelve subaxial cervical spine injuries, four of which could be classified under the Allen-Ferguson (A-F) classification and SLIC scoring system (C7 A-F compressive flexion stage 5 and SLIC–6, C5 A-F vertical compression stage 2 and SLIC–3, C6 distractive flexion stage 2 and SLIC–8, and C7 compressive flexion stage 1 and SLIC–2, respectively). Surgical intervention consisting of instrumented arthrodesis was performed in five patients for cervical instability. The remaining subaxial cervical spine fractures were isolated to the spinous and transverse processes. Thoracic and lumbar vertebral fractures were sustained in five and three patients respectively, and none of these patients required surgical intervention for their thoracic or lumbar fractures.
Other associated injuries included thoracic cavity injury (pneumothorax, pulmonary contusions, and rib fractures) in sixteen (51.6%) patients, shoulder girdle injury (clavicle, coracoid, acromion, and scapula) in sixteen (51.6%) patients, upper-extremity injury in eleven (35.5%) patients, lower-extremity injury in twelve (38.7%) patients, upper-extremity vascular injury in four (12.9%) patients, and a visceral injury in three (9.7%) patients. Most associated injuries were ipsilateral to the brachial plexus injury; all of the thoracic (sixteen of sixteen) and upper-extremity injuries (eleven of eleven), 93.8% (fifteen of sixteen) of the shoulder-girdle injuries, and 75% (nine of twelve) of the lower-extremity injuries occurred ipsilaterally. The mean Injury Severity Score for these patients was 26.9 ± 11.8.
Physical examination and/or electrophysiological findings suggestive of a preganglionic injury were present in all of the patients with combined spinal cord and brachial plexus injury (see Appendix). These findings included decreased rhomboid muscle strength in thirteen (41.9%) and rhomboid fibrillations (EMG) in nine (29%) patients, decreased serratus anterior muscle strength in twenty-four (77.4%) patients, a Horner sign in twenty (64.5%) patients, and fibrillations (EMG) in cervical paraspinal muscles in thirteen (41.9%) patients. On inspiration and expiration chest radiographs, phrenic nerve dysfunction was present in nine patients (29%). On CT and MRI imaging, pseudomeningoceles were noted in twenty patients (64.5%) and brachial plexus level (C5-T1) transverse or spinous process fractures were noted in nine patients (29%), seven (77.8%) of those having sustained an ipsilateral preganglionic injury at the same level.
Factors Associated with the Presence of a Combined Spinal Cord Injury and Brachial Plexus Injury
On the basis of the number of patients in this series, no significant differences were found between the mean age at injury, mechanism of injury, extent of brachial plexus injury, preoperative DASH score, or the presence of a vascular injury between the patients with or without an associated spinal cord injury (Table IV). The patients with combined spinal cord and brachial plexus injury had significantly higher occurrence of concomitant spine fracture, especially cervical spine fracture (48.4%, fifteen of thirty-one) compared with brachial plexus injury patients without an associated spinal cord injury (21.4%, forty-eight of 224, p value < 0.001). Among patients with an upper-extremity vascular injury, there was a higher proportion of patients with a supraclavicular vascular injury (three of four) in the group with concomitant spinal cord injury than there was in the group of patients who had brachial plexus injury without associated spinal cord injury (11.8%, four of thirty-four, p value = 0.02).
TABLE IV.
Comparison of Patient Data Between Patients with Combined Spinal Cord and Brachial Plexus Injuries and Patients with Isolated Brachial Plexus Injuries*
| Patients with BPI and SCI(N = 31) | Patients with BPI Alone (N = 224) | Odds Ratio (95% CI)† | P Value | Adjusted P Value‡ | |
| Years of age (mean and standard deviation) | 33.6 ± 11.9 | 32.7 ± 13.5 | 0.9 (–4.1, 6.0) | 0.43 | 0.67 |
| Mechanism of injury (no. [%]) | |||||
| High-speed | 23 (74.2%) | 154 (69.5%)# | |||
| Low-speed | 5 (16.1%) | 31 (13.9%)# | |||
| Work-related | 2 (6.5%) | 5 (2.2%)# | |||
| Football | 0 (0%) | 5 (2.2%)# | |||
| Skiing | 1 (3.2%) | 3 (1.3%)# | |||
| Other | 0 (0%) | 25 (11.2%)# | |||
| Spinal fractures | 2.60 (1.21, 5.57)† | 0.01 | 0.05 | ||
| Yes | 17 (54.8%) | 71 (31.8%)# | |||
| No | 14 (45.2%) | 152 (68.2%)# | |||
| Level of spinal fracture§(no. [%]) | |||||
| Cervical | 15 (48.4%) | 48 (21.4%) | 3.44 (1.59, 7.45)† | 0.001 | 0.01 |
| Thoracic | 5 (16.1%) | 29 (12.9%) | 1.29 (0.46, 3.63)† | 0.58 | 0.74 |
| Lumbar | 3 (9.7%) | 9 (4%) | 2.56 (0.65, 10.02)† | 0.17 | 0.29 |
| Type of brachial plexus lesion (no. [%]) | 0.83 (0.35, 1.96)† | 0.67 | 0.74 | ||
| Complete | 23 (74.2%) | 70.5% (158) | |||
| Incomplete | 8 (25.8%) | 29.5% (66) | |||
| Vascular Injury (no. [%]) | 0.83 (0.27, 2.52)† | >0.99 | >0.99 | ||
| Yes | 4 (12.9%) | 34 (15.2%) | |||
| No | 27 (87.1%) | 190 (84.8%) | |||
| Level of vascular injury (no. [%]) | 22.5 (1.9, 271.9)† | 0.02 | 0.05 | ||
| Supraclavicular | 3 (75%) | 4 (11.8%) | |||
| Infraclavicular | 1 (25%) | 30 (88.2%) | |||
| Horner sign (no. [%]) | 21 (67.7%) | 88 (39.5%) | 3.22 (1.45, 7.17)† | 0.01 | 0.05 |
| Phrenic nerve dysfunction (no. [%]) | 9 (29%) | 32 (14.3%) | 2.45 (1.04, 5.81)† | 0.04 | 0.09 |
| Number of pseudomeningoceles | 2.3 ± 1.53 | 1.7 ± 1.37 | 0.7 (0.0, 1.3) | 0.04 | 0.09 |
| Preoperative DASH score (mean and standard deviation) | 46.0 ± 18.40 | 45.2 ± 16.87 | 0.8 (–6.9, 8.5) | 0.69 | 0.74 |
| Preoperative VAS (mean and standard deviation) | 5.4 ± 2.68 | 3.7 ± 3.05 | 1.7 (0.2, 3.3) | 0.02 | 0.06 |
BPI = brachial plexus injury; SCI = spinal cord injury; CI = confidence interval; DASH = Disabilities of the Arm, Shoulder and Hand; VAS = visual analog scale.
Dagger indicates the difference in means (95% confidence interval).
The Benjamini-Hochberg procedure was applied to the p values to control the false-discovery rate.
Level of spinal fracture was not mutually exclusive; 20 patients had multiple-level involvement.
Based on denominator of 223 patients, as results were unknown in one patient.
When compared with patients without concomitant spinal cord injury, the patients with combined spinal cord and brachial plexus injury had a higher mean number of pseudomeningoceles (2.3 ± 1.53 versus 1.7 ± 1.37, p value = 0.04), a higher mean pain score on the VAS (5.4 ± 2.68 versus 3.7 ± 3.05, p value = 0.02), were more likely to exhibit a Horner sign (67.7% [twenty-one of thirty-one] versus 39.5% [eighty-eight of 224], p value = 0.01), and were more likely to have a phrenic nerve dysfunction (29% [nine of thirty-one] versus 14.3% [thirty-two of 224], p value = 0.04).
Discussion
In our study, the prevalence of concomitant spinal cord injury in adult patients with a closed-traction brachial plexus injury was 12.2%, which is significantly higher than what has been previously reported1,3,5-8,17,18. Concomitant spinal cord injury in patients with brachial plexus injury is theorized to occur directly from the traumatic event. Direct spinal cord injury may occur from the initial traumatic force transmitted to the spinal cord. The cervical and midthoracic portions of the spine are believed to be susceptible to damage with excessive lateral flexion3, a mechanism inherent to most traction-type brachial plexus injuries involving forcible separation of the head and/or neck from the shoulder1,2,5. Both excessive lateral flexion and hyperextension have been postulated as a cause of combined spinal cord and brachial plexus injury3,9. In patients with Brown-Séquard or central cord syndrome, rotation with hyperextension19 or hyperextension alone20 has been speculated to be the mechanism of spinal cord injury.
Indirect (secondary) injuries to the spinal cord, as a result of a preganglionic brachial plexus injury, have also been hypothesized to result in combined spinal cord and brachial plexus injury. Intradural ruptures (rootlet rupture proximal to the dorsal root ganglion) or central avulsions (rootlet and central nervous tissue avulsed from the spinal cord)8,21,22 can result in anterior horn cell death6. Central avulsions intrinsically cause spinal cord damage; this is evidenced by signal intensity changes within the spinal cord on MRI in up to 20% of patients with brachial plexus injury23 and by MRI findings of spinal cord hemorrhage, scarring, edema, and/or posttraumatic syrinx in preganglionic injuries24,25. Another mechanism by which preganglionic injuries may cause spinal cord injury is by acute spinal cord compression and/or displacement due to scar tissue26 or epidural, subarachnoid, or subdural hematoma10,11. In our series, all patients with a combined brachial plexus and spinal cord injury had sustained a preganglionic injury of at least one level. However, it is not possible to determine if spinal cord injury occurred directly from the trauma or indirectly from the preganglionic injury in these patients.
Patients with a combined spinal cord and brachial plexus injury are subjected to a higher level of trauma along with major associated injuries. The mechanism responsible for concomitant spinal cord and brachial plexus injury in our patients was of sufficient magnitude to cause other associated injuries in all patients with combined spinal cord and brachial plexus injury. The prevalence of ipsilateral associated injuries, both in the patients in our study as well as in the patients reported in the literature3, reflects the force of the initial trauma. Moreover, the ISS in our patients with combined spinal cord and brachial plexus injury (Injury Severity Score, 26.9 ± 11.8) was higher when compared with the reported17 Injury Severity Score of multitrauma patients with brachial plexus injury (Injury Severity Score, 24), likely reflecting the severity of initial trauma in patients with a combined injury involving the spinal cord and the brachial plexus.
On the basis of our findings of factors associated with the presence of a combined spinal cord and brachial plexus injury, these concomitant lesions appear to be related to both the severity of the initial traumatic injury to the cervical region and to the preganglionic nature of the brachial plexus injury. Reflective of the severity of the initial traumatic injury to the proximal brachial plexus and/or cervical area, patients with a concomitant spinal cord injury were significantly more likely to have an associated fracture of the spine (especially of the cervical region [p < 0.001]) and supraclavicular vascular injury (p = 0.02) than were patients with brachial plexus injury but no concomitant spinal cord injury. Patients with combined spinal cord and brachial plexus injury were also more likely to have factors associated with a preganglionic injury, such as higher preoperative pain (p value = 0.02), Horner syndrome (p = 0.01), phrenic nerve dysfunction (p = 0.04), and increased number of pseudomeningoceles (p = 0.04). The presence of these clinical and/or imaging factors in patients with brachial plexus injury should raise suspicion for possible coexistent subtle spinal cord injury. Similarly, initial evaluation of the brachial plexus injured patient should include a thorough neurologic examination of the lower extremities for any signs of myelopathy and a review of imaging studies of the spinal cord.
The detection of a concomitant spinal cord injury in the patients with brachial plexus injury may be important for the choice of surgical intervention required to achieve successful outcomes. Poor surgical outcomes have been reported in patients with spinal cord injury and a concomitant brachial plexus injury1,27 and have been attributed to the delayed identification of the brachial plexus injury1,28. However, in the patient with a brachial plexus injury and a concomitant spinal cord injury, the lesion to the spinal cord may contribute to poor surgical results, depending on the surgical strategy. For example, the results of intercostal nerve transfers are extremely poor in patients with Brown-Séquard syndrome6. We postulate that the spasticity associated with the upper motor-neuron lesion could result in compromised target sensorimotor function. Although complete spinal cord lesions are easily identified, cases of partial, incomplete, and subtle spinal cord lesions or syndromes (Brown-Séquard, anterior cord syndrome) may be missed and could negatively affect surgical reconstruction that relies on normal spinal cord function. Vigilance for even minor clinical evidence for a spinal cord injury (upper motor-neuron signs) must be upheld, as these may be indicative of preganglionic, central nerve root avulsions (indirect spinal cord injury) or serve as a harbinger of an abnormal cervical spinal cord with brachial plexus roots that are inadequate for utilization.
The limitations of this retrospective study from a tertiary medical center include the possibility of recall bias (from delayed evaluation), loss of pertinent clinical information (from outside institutions), and/or resolution of physical findings associated with spinal cord injury (from delayed evaluation). These factors would lead to underestimation of the prevalence of spinal cord injury. Conversely, by considering upper motor-neuron signs as minor clinical evidence of a spinal cord injury, the prevalence of spinal cord injury could have been overestimated and the lack of outcome data could limit any discussion regarding the clinical significance. However, even if only the patients with “definitive” and “probable” spinal cord injury were considered to have combined injuries, the prevalence would be 10.2%, much higher than the currently reported prevalence. It is likely that in previous reports, only patients with overt spinal cord injury had been detected and that subtle spinal cord injury may have been missed. Our study suggests that combined brachial plexus injury and spinal cord injury is not infrequent and may be reflective of improved survivability due to airbags and the increased energy associated with these injuries.
We believe that concomitant spinal cord injury in patients with brachial plexus injury has been underreported and underrecognized, as subtle spinal cord injury can easily go undetected if a detailed history and/or complete neurologic examination are not performed. The presence of associated injuries (such as cervical fractures and/or supraclavicular vascular injuries) and preganglionic injury signs and symptoms (Horner syndrome, preoperative pain as reported on a visual analog scale, phrenic nerve dysfunction, and pseudomeningoceles) should increase the suspicion for an associated spinal cord injury. The high prevalence of combined spinal cord injury and brachial plexus injury in this report will hopefully increase the awareness of these combined injuries and improve their identification. The identification of a concomitant spinal cord injury is important because it could impact the surgical strategy to treat these injuries and potentially influence the outcome of brachial plexus surgical reconstruction.
Supplementary Material
A chart showing the breakdown of brachial plexus injuries for all causes and tables showing associated injuries as well as imaging and clinical findings suggestive of a preganglionic injury in patients with a combined spinal cord and brachial plexus injury
Acknowledgments
Note: The authors thank Dirk R. Larson, MS, and Matthew R. Jensen, BS, (Mayo Clinic, Department of Biostatistics) for their assistance with statistical analysis.
Footnotes
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Akita S, Wada E, Kawai H. Combined injuries of the brachial plexus and spinal cord. J Bone Joint Surg Br. 2006;88:637-41 [DOI] [PubMed] [Google Scholar]
- 2.Grundy DJ, Silver JR. Problems in the management of combined brachial plexus and spinal cord injuries. Int Rehabil Med. 1981;3:57-70 [DOI] [PubMed] [Google Scholar]
- 3.Grundy DJ, Silver JR. Combined brachial plexus and spinal cord trauma. Injury. 1983;15:57-61 [DOI] [PubMed] [Google Scholar]
- 4.Germann G, Wind G, Harth A. [The DASH (Disability of Arm-Shoulder-Hand) Questionnaire—a new instrument for evaluating upper extremity treatment outcome]. Handchir Mikrochir Plast Chir. 1999;31:149-52 German [DOI] [PubMed] [Google Scholar]
- 5.Narakas AO. [Injuries of the brachial plexus and neighboring peripheral nerves in vertebral fractures and other trauma of the cervical spine]. Orthopade. 1987;16:81-6 German [PubMed] [Google Scholar]
- 6.Nordin L, Sinisi M. Brachial plexus-avulsion causing Brown-Sequard syndrome: a report of three cases. J Bone Joint Surg Br. 2009;91:88-90 [DOI] [PubMed] [Google Scholar]
- 7.Stephen AB, Stevens K, Craigen MA, Kerslake RW. Brown-Séquard syndrome due to traumatic brachial plexus root avulsion. Injury. 1997;28:557-8 [DOI] [PubMed] [Google Scholar]
- 8.Birch R. Traumatic lesions of the brachial plexus. : Birch R, Bonney G, Wynn Parry C. Surgical disorders of the peripheral nerves. Edinburgh: C Livingstone; 1998. p 157-207 [Google Scholar]
- 9.Roaf R. Lateral flexion injuries of the cervical spine. J Bone Joint Surg Br. 1963;45:36-8 [Google Scholar]
- 10.Russell NA, Mangan MA. Acute spinal cord compression by subarachnoid and subdural hematoma occurring in association with brachial plexus avulsion. Case report. J Neurosurg. 1980;52:410-3 [DOI] [PubMed] [Google Scholar]
- 11.Flannery MC, Birch R. Acute compression of the cervical spinal cord: a complication of preganglionic injury to the brachial plexus. Injury. 1990;21:247-8 [DOI] [PubMed] [Google Scholar]
- 12.American Spinal Injury Association Reference manual of the international standards for neurological classification of spinal cord injury. Chicago: American Spinal Injury Association; 2003 [Google Scholar]
- 13.Baker SP, O'Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187-96 [PubMed] [Google Scholar]
- 14.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Zeiller SC, Anderson DG, Bono CM, Stock GH, Brown AK, Kuklo T, Oner FC. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30:2325-33 [DOI] [PubMed] [Google Scholar]
- 15.Allen BL, Jr, Ferguson RL, Lehmann TR, O'Brien RP. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7:1-27 [DOI] [PubMed] [Google Scholar]
- 16.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57:289-300 [Google Scholar]
- 17.Midha R. Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery. 1997;40:1182-9 [DOI] [PubMed] [Google Scholar]
- 18.Webb JC, Munshi P, Saifuddin A, Birch R. The prevalence of spinal trauma associated with brachial plexus injuries. Injury. 2002;33:587-90 [DOI] [PubMed] [Google Scholar]
- 19.Chechick A, Amit Y, Shaked I, Rappaport ZH, Tadmor R. Brown-Séquard syndrome associated with brachial plexus injury in neck trauma. J Trauma. 1982;22:430-1 [DOI] [PubMed] [Google Scholar]
- 20.Schneider RC, Cherry G, Pantek H. The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg. 1954;11:546-77 [DOI] [PubMed] [Google Scholar]
- 21.Schenker M, Birch R. Diagnosis of the level of intradural rupture of the rootlets in transaction lesions of the brachial plexus. J Bone Joint Surg Br. 2001;83:916-20 [DOI] [PubMed] [Google Scholar]
- 22.Tavakkolizadeh A, Saifuddin A, Birch R. Imaging of adult brachial plexus traction injuries. J Hand Surg Br. 2001;26:183-91 [DOI] [PubMed] [Google Scholar]
- 23.Yoshikawa T, Hayashi N, Yamamoto S, Tajiri Y, Yoshioka N, Masumoto T, Mori H, Abe O, Aoki S, Ohtomo K. Brachial plexus injury: clinical manifestations, conventional imaging findings, and the latest imaging techniques. Radiographics. 2006;26 Suppl 1:S133-43 [DOI] [PubMed] [Google Scholar]
- 24.Volle E, Assheuer J, Hedde JP, Gustorf-Aeckerle R. Radicular avulsion resulting from spinal injury: assessment of diagnostic modalities. Neuroradiology. 1992;34:235-40 [DOI] [PubMed] [Google Scholar]
- 25.Hems TE, Birch R, Carlstedt T. The role of magnetic resonance imaging in the management of traction injuries to the adult brachial plexus. J Hand Surg Br. 1999;24:550-5 [DOI] [PubMed] [Google Scholar]
- 26.Penfield W. Late spinal paralysis after avulsion of the brachial plexus. J Bone Joint Surg Am. 1949;31:40. [PubMed] [Google Scholar]
- 27.Sedel L. The results of surgical repair of brachial plexus injuries. J Bone Joint Surg Br. 1982;64:54-66 [DOI] [PubMed] [Google Scholar]
- 28.Bentolila V, Nizard R, Bizot P, Sedel L. Complete traumatic brachial plexus palsy. Treatment and outcome after repair. J Bone Joint Surg Am. 1999;81:20-8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A chart showing the breakdown of brachial plexus injuries for all causes and tables showing associated injuries as well as imaging and clinical findings suggestive of a preganglionic injury in patients with a combined spinal cord and brachial plexus injury