Nationwide, approximately 21% of individuals infected with human immunodeficiency virus (HIV) are unaware of their infection.1 HIV partner services (PS), a process of identifying, notifying, and testing HIV-exposed sex and needle-sharing partners, promote early identification of undiagnosed HIV infections—a core objective of all HIV prevention programs.2 Studies have shown that more patients can be reached for PS, and outcomes can improve, when public health workers are integral in the PS process.3–5 However, HIV clinicians and patients have long underutilized the PS system at the New York City (NYC) Department of Health and Mental Hygiene (DOHMH) (Figure 1). NYC outcomes for PS lag when compared with other counties in New York State (NYS).6 Furthermore, a 2004 DOHMH analysis found that disease intervention specialists (DISs) at DOHMH sexually transmitted disease (STD) control clinics elicited four times more partners and were more successful than non-DOHMH providers in notifying and testing partners.4 Therefore, to increase PS for patients diagnosed by non-DOHMH providers, DOHMH formed the HIV Field Services Unit (FSU) in July 2006 to work collaboratively with providers to expand PS access in NYC neighborhoods hardest hit by the HIV epidemic.7 Initially, the FSU partnered with eight hospitals serving neighborhoods with high rates of late HIV diagnosis, high HIV prevalence, and mortality. We report outcomes of the first two full years of implementation and lessons learned.
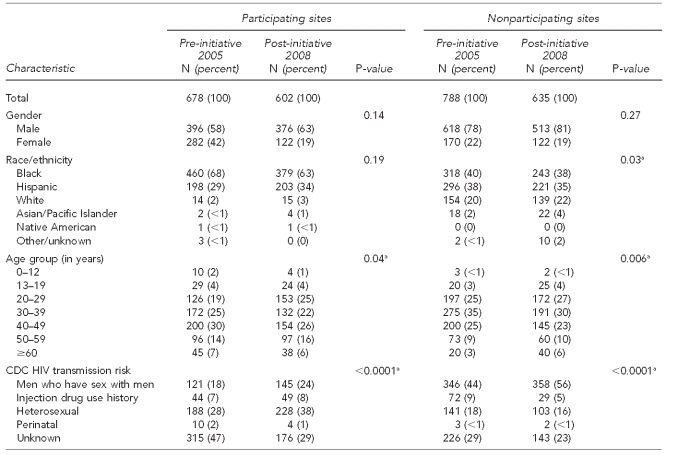
Figure 1.
New York City HIV partner services system before (2005) and after (2008) implementation of the HIV Field Services initiative
HIV = human immunodeficiency virus
NYC = New York City
DOHMH = Department of Health and Mental Hygiene
DIS = disease intervention specialist
PS = partner services
PRF = provider report form
METHODS
Development of DIS field site placements
To introduce the new program, DOHMH program management staff and the DISs designated for each site held in-person meetings with targeted hospitals' HIV care and administrative staff. At the meetings, we reviewed lagging NYC PS outcomes compared with the rest of NYS and the higher yield of PS performed by DOHMH staff at STD clinics compared with the PS outcomes performed by community providers. We also reviewed the NYS laws and regulations pertaining to HIV PS and emphasized the collaborative roles and responsibilities of DOHMH and community providers. A general operational protocol for collaboration was developed and specific steps were tailored to reflect variations in hospital settings. Additional details about this process have been described elsewhere.8
DIS placement in HIV clinics
Eight experienced DISs were assigned on full-time or on-call bases at voluntarily participating hospitals to provide on-site PS assistance to providers and HIV-infected patients. An additional three field-based DISs performed PS at patients' homes and at prearranged field sites in the community throughout all five NYC boroughs.
PS protocol
Provider referrals, HIV surveillance reports, and partner notifications were used to identify patients needing PS. The NYC HIV/AIDS reporting system (HARS), a population-based surveillance registry of all New Yorkers diagnosed with acquired immunodeficiency syndrome (AIDS) since 1981 and HIV since 2000, was used to prioritize and plan PS. Patients chose a partner notification option: patient-delivered, provider-delivered, or DIS-assisted. Notification of named partners not in HARS was prioritized above already reported partners (Figure 2). DISs or providers screened for domestic violence risk associated with planned notifications; partner notifications proceeded if risk seemed low. We requested that partners authorize access to their HIV-negative test results, which are not reportable in NYS.
Figure 2.
HIV field services unit workflow for provider report, partner elicitation, partner notification, and HIV testing after implementation of the HIV Field Services program in New York City, 2006
aImplemented January 2008
bImplemented February 2009
HIV = human immunodeficiency virus
FSU = field services unit
DIS = disease intervention specialist
HARS = HIV/AIDS surveillance registry
NYC = New York City
PS = partner services
In February 2008, DOHMH implemented field-testing using the OraSure® HIV-1 Oral Specimen Collection Device (Orasure Technologies Inc., Bethlehem, Pennsylvania) following partner notification to remove barriers to testing and negative test documentation. PS outcomes were entered into DOHMH's partner notification database. During the partner elicitation interview, DISs assessed patients' understanding of the follow-up care plan made by providers. If DISs identified a lack of understanding on the part of the patient, or reluctance to adhere to the follow-up plan, they attempted to address potential barriers by facilitating appointment scheduling; providing transportation to appointments; and offering a patient brochure explaining HIV transmission, pathogenesis, management, and PS. Exposed partners testing HIV-positive following notification and testing were also linked to medical care.
PS outcomes
At the participating sites pre-intervention, and at nonparticipating sites post-intervention, provider reports of PS outcomes (partner elicited, notified, and tested) were accepted by DOHMH as the final outcome. Providers could report patient-delivered partner notification to DOHMH without having verified the notification by speaking with the named partner. At the participating sites during the post-intervention period, DISs and provider-delivered or provider-verified notifications were accepted as the final outcomes. Only patient-delivered notifications verified by DISs with the notified partner were acceptable as successful notification. Patient-delivered notifications without DIS verification were recorded as non-notifications.
Data analysis
We assessed the FSU's impact by comparing PS outcomes before (2005) and after (2008) FSU implementation, as well as by comparing outcomes in participating sites and eight nonparticipating sites. Both participating and nonparticipating sites are major HIV diagnostic and treatment centers serving diverse, populous neighborhoods throughout NYC. The nonparticipating sites were selected for this comparison based on their similarity to participating sites in volume of new HIV diagnoses reported each year. PS data for 2005 were obtained from the provider report form (PRF) database, which consists of names of known sex and needle-sharing partners of HIV-infected people (living or deceased) and any PS outcomes performed by the providers or their patients or provider request for DIS-assisted notification through the health department's longstanding contact notification assistance program.
PS data for 2008 for participating providers were extracted from the FSU partner and PRF databases. The partner names in both databases were matched and duplicate reports were identified and merged into one record. PS data for nonparticipating sites in 2005 and 2008 were extracted from the PRF database. We restricted our comparison to newly diagnosed patients because this group's PS need is universal. We used Chi-square tests to compare differences between groups and Fisher's exact test for expected cell values <5. Statistical significance was set at p≤0.05.
RESULTS
Demographics of HIV-positive patients
Of 3,809 patients diagnosed in NYC in 2008,9 602 (15%) and 635 (16%) were from participating and selected nonparticipating sites, respectively. Significantly (p≤0.0001) more patients at participating sites than at nonparticipating sites were black (63% vs. 38%) or reported heterosexual transmission risk (38% vs. 16%). Nonparticipating site patients were more likely than participating site patients to be white (22% vs. 3%), aged 30–39 years (30% vs. 22%), and men who have sex with men (MSM) (56% vs. 24%). The demographic composition of patients at participating and nonparticipating sites did not change significantly between 2005 and 2008 (Table). A significant change in age distribution was observed only for people ≥ 60 years of age at nonparticipating sites from 2005 to 2008 (3% vs. 6%). At both participating and nonparticipating sites, the proportions of MSM increased significantly from 2005 to 2008. We observed improved ascertainment of Centers for Disease Control and Prevention-defined heterosexual HIV transmission risk behavior at participating sites from 2005 to 2008.
Table.
Characteristics of index cases diagnosed at HIV medical care sites that participated or did not participate in the HIV Field Services program in New York City, 2005 and 2008
aSignificant at p≤ 0.05
HIV = human immunodeficiency virus
CDC = Centers for Disease Control and Prevention
Comparison of PS outcomes pre- and post-intervention
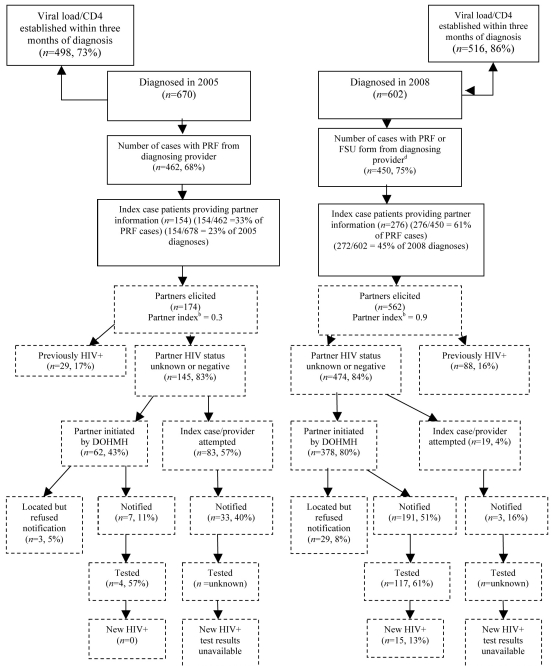
As shown in Figure 3, at participating sites, we observed significant improvements (p≤0.0001) in the partner-index ratio (partners elicited/patients interviewed) (0.3 in 2005 vs. 0.9 in 2008), as well as proportions of patients naming partners (33% in 2005 vs. 61% in 2008) and of named partners notified (51% in 2005 vs. 67% in 2008). DIS-assisted partner notifications increased markedly from 2005 to 2008 (43% vs. 80% attempted; 11% vs. 51% delivered). In 2008, 61% of notified partners at participating sites were tested; 15 out of 117 (13%) tested were newly diagnosed with HIV infection.
Figure 3.
Partner elicitation and notification results comparing the yields of partner elicitation, notification, and testing of participating HIV Field Testing program sites in New York City, 2005 and 2008a,b,c
aFor 2005, partner information is from the PRF only. For 2008, partner information is from the PRF and FSU.
bPartner index: partners elicited/HIV cases diagnosed. Index cases were from data collected as of March 30, 2009.
cCases that had both PRF and FSU forms were counted as one record, and all partners received on either form were included in the analysis.
dUnless otherwise indicated, proportions were calculated using the number inside the box as the numerator, and the number in the nearest “upstream” box as the denominator.
PRF = provider report form
FSU = field services unit
HIV = human immunodeficiency virus
DOHMH = Department of Health and Mental Hygiene
PS outcomes were similar at participating and nonparticipating sites in 2005. Comparison of key PS outcome indicators in 2008 demonstrated significant differences between participating and nonparticipating sites in the post-intervention period. In participating sites, 75% of newly diagnosed patients had a PRF submitted (indicating submission of partner elicitation information from the clinical provider) compared with 44% at nonparticipating sites (p=0.0001). Comparison of PRFs from nonparticipating providers to PRFs and FSU reports from participating sites indicated that more partners at participating sites were elicited (474 vs. 13; p=0.0001) and notified (194 vs. 1; p=0.0001). The number of partners tested could not be compared due to incomplete HIV testing information on partners notified by non-DOHMH providers (data not shown).
DISCUSSION
In 2006, DOHMH expanded HIV PS access through a unique public-private collaboration that markedly improved outcomes at participating sites. The largest expansion of PS access was to black and Hispanic people—two groups disproportionately affected by the HIV epidemic in NYC.9 Participating providers and clients expressed satisfaction with the collaboration.8 Key factors in the initiative's success were stationing DISs at HIV clinical sites, integrating DISs into clinical teams, delivering PS and testing at locations chosen by clients, and using surveillance data to plan and prioritize PS. Compared with nonparticipating sites during the same time period, participating sites experienced a substantial improvement in PS outcomes after the introduction of FSU, despite serving a smaller proportion of MSM clients, whose participation in PS has been observed to result in PS outcomes that are greater than or equal to the magnitude of non-MSM PS clients.10
We observed an HIV seropositivity rate among tested partners (13%) that was lower than previously published rates by PS programs.11,12 One potential reason for this difference is that STD program DISs typically lack access to HIV surveillance data to verify clients' self-reported HIV serostatus,13,14 resulting in the inclusion of people previously diagnosed with HIV among those reported newly diagnosed through PS. A crucial component of HIV PS is accurate documentation of index and partner characteristics and notification outcomes. Our practice of verifying notifications not performed by health department staff with the exposed partner or provider was very successful. Among our cohort, 88% of patient-delivered notifications were verified, although the fact that clients knew we would be confirming notification with their partner may have prompted them to be more vigilant in their own notification efforts than they might otherwise have been.
We used the opportunity to collaborate with participating sites as a means to improve providers' awareness of their legal obligation in NYS to report HIV-diagnosed patients and their named partners to the health department using the PRF. We distributed our own brochures for providers, which include instructions on reporting cases and partners at initial diagnosis.15–17 We also reminded providers of an often overlooked portion of the PRF designed to accommodate reporting of additional, previously unreported partners who might be elicited at follow-up visits after diagnosis and the initial PRF submission. Our encouragement of the use of this form was part of an overall message that HIV-infected patients' need for PS endures for years following diagnosis, and clinic visits are opportunities to address this ongoing need. Providing HIV PS is a complex task that requires time, expertise, and resources to achieve; this initiative provides a consistent and effective alternative to accomplish what is otherwise a time-consuming and difficult process for most NYC providers.
Aside from improving case surveillance, there are other program benefits not captured by the outcome measures reported in this article. We believe that counseling HIV-negative partners after their HIV exposure had a far greater positive impact on clients' HIV risk behaviors than it would have were it delivered under routine HIV testing circumstances. We also used our front-line experience to develop tailored educational materials about PS and HIV prevention for NYC providers and patients, likely further enhancing the impact of our prevention counseling.15–19 Furthermore, the FSU's linkage-to-care efforts likely reduced HIV transmission by influencing patients' antiretroviral medication initiation and adherence, leading to lower HIV viral-load levels and transmission risk.20,21
Limitations
Our findings were subject to several limitations. First, participating facilities served mostly black or Hispanic HIV-positive index cases and, thus, our findings may not be generalizable to other facilities. We may have underestimated the number of notified HIV-exposed partners who were tested for HIV because of the barriers to documenting HIV-negative test results. Because such results are not reportable in NYS, DISs must have partners complete and sign a release of HIV-related information form to verify HIV-negative test results with clinical providers. Many partners refuse to sign this form at notification, and providers may not always report partners' test results to us. We also may have underreported the number of HIV-exposed partners newly diagnosed with HIV infection following partner notification by HIV index patients or community providers. Providers only submit PRFs on 44% of all newly diagnosed HIV patients at nonparticipating facilities; known partners may not have been reported on the forms submitted as required by law, thereby contributing to an undercounting of HIV case findings from provider- or patient-delivered partner notifications.
CONCLUSION
This program's implementation demonstrates that DISs can be integrated into HIV clinical settings to achieve large-scale improvements in community-wide PS outcomes. The favorable response to this program by providers and clients has led to the expansion to 35 facilities in NYC from 2009 through 2011. Preliminary 2009 program data show more improvements in PS outcomes, despite doubling the number of participating sites with no increases in personnel, illustrating efficiency gains achieved as the program matures.
Footnotes
The Human Immunodeficiency Virus (HIV) Field Services program is funded by the Centers for Disease Control and Prevention under HIV prevention grant #U62/CCU223460-06-1. The authors are grateful to the HIV Field Services Unit staff for their skillful implementation of the program and their ongoing dedication to curb HIV transmission in New York City. The authors are indebted to the medical providers at the participating hospitals and to the patients and partners whose cooperation made this program possible. The authors thank Tamar Renaud, Steve Rubin, Judith Sackoff, and Chris Larkin for their contributions in conceptualizing the program. This study was determined to be exempt from Institutional Review Board approval.
REFERENCES
- 1.Campsmith ML, Rhodes PH, Hall HI, Green TA. Undiagnosed HIV prevalence among adults and adolescents in the United States at the end of 2006 [published erratum appears in J Acquir Immune Defic Syndr 2010;54:112] J Acquir Immune Defic Syndr. 2010;53:619–24. doi: 10.1097/QAI.0b013e3181bf1c45. [DOI] [PubMed] [Google Scholar]
- 2.Hogben M, McNally T, McPheeters M, Hutchinson AB. The effectiveness of HIV partner counseling and referral services in increasing identification of HIV-positive individuals: a systematic review. Am J Prev Med. 2007;33(2 Suppl):S89–100. doi: 10.1016/j.amepre.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 3.Taylor MM, Mickey T, Winscott M, James H, Kenney K, England B. Improving partner services by embedding disease intervention specialists in HIV-clinics. Sex Transm Dis. 2010;37:767–70. doi: 10.1097/OLQ.0b013e3181e65e8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malave MC, Shah D, Sackoff JE, Rubin S, Begier EM. Human immunodeficiency virus partner elicitation and notification in New York City: public health does it better. Sex Transm Dis. 2008;35:869–76. doi: 10.1097/OLQ.0b013e31817d2f82. [DOI] [PubMed] [Google Scholar]
- 5.Landis SE, Schoenbach VJ, Weber DJ, Mittal M, Krishan B, Lewis K, et al. Results of a randomized trial of partner notification in cases of HIV infection in North Carolina. N Engl J Med. 1992;326:101–6. doi: 10.1056/NEJM199201093260205. [DOI] [PubMed] [Google Scholar]
- 6.New York State Department of Health. HIV/AIDS statistics in New York State: report on partner notification activities 2002–2003 and 2004. [cited 2011 Jul 15]. Available from: URL: http://www.health.state.ny.us/diseases/aids/statistics.
- 7.Frieden TR, Das-Douglas M, Kellerman SE, Henning KJ. Applying public health principles to the HIV epidemic. N Engl J Med. 2005;353:2397–402. doi: 10.1056/NEJMsb053133. [DOI] [PubMed] [Google Scholar]
- 8.Udeagu CC, Bocour A, Gale I, Begier EM. Provider and client acceptance of a health department enhanced approach to improve HIV partner notification in New York City. Sex Transm Dis. 2010;37:266–71. doi: 10.1097/OLQ.0b013e3181d013e0. [DOI] [PubMed] [Google Scholar]
- 9.New York City Department of Health and Mental Hygiene. New York City HIV/AIDS annual surveillance statistics 2008: list of annual tables. [cited 2010 May 5]. Available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/ah/surveillance2008_tables_all.pdf.
- 10.Brewer DD. Case-finding effectiveness of partner notification and cluster investigation of sexually transmitted diseases/HIV. Sex Transm Dis. 2005;32:78–83. doi: 10.1097/01.olq.0000153574.38764.0e. [DOI] [PubMed] [Google Scholar]
- 11.Golden MR, Hogben M, Potterat JJ, Hansfield HH. HIV partner notification in the United States: a national survey of program coverage and outcomes. Sex Transm Dis. 2004;31:709–12. doi: 10.1097/01.olq.0000145847.65523.43. [DOI] [PubMed] [Google Scholar]
- 12.Marcus JL, Bernstein KT, Klausner JD. Updated outcomes of partner notification for human immunodeficiency virus, San Francisco, 2004–2008. AIDS. 2009;23:1024–6. doi: 10.1097/QAD.0b013e32832921a7. [DOI] [PubMed] [Google Scholar]
- 13.Renaud TC, Woog V, Ramaswamy CK, Tsoi BW, Sabharwal CJ, Pickett L, et al. Overstating social networks' ability to diagnose new cases of HIV. Am J Public Health. 2010;100(Suppl1):S5–6. doi: 10.2105/AJPH.2009.182998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Potterat JJ. The end of laissez-faire HIV partner notification? Trust but verify. Sex Transm Dis. 2009;36:463–4. doi: 10.1097/OLQ.0b013e3181aaf163. [DOI] [PubMed] [Google Scholar]
- 15.New York City Department of Health and Mental Hygiene. Help your patients tell their partners: encourage HIV partner notification with the NYC Health Department. [cited 2009 Jun 24]. Available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/hiv-fsu-provider-brochure.pdf.
- 16.New York City Department of Health and Mental Hygiene. Diagnosed with HIV? The New York City Health Department can help you and your partner. [cited 2009 Jun 24]. Available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/hiv-fsu-patient-brochure.pdf.
- 17.New York City Department of Health and Mental Hygiene. Need help notifying the partners of your HIV positive patients? [cited 2009 Jun 24]. Available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/cnap_provider_brochure.pdf.
- 18.New York City Department of Health and Mental Hygiene. Need help telling your partners they should get tested for HIV? [cited 2009 Jun 24]. Available from: URL: http://www.nyc.gov/html/doh/downloads/pdf/dires/cnap_patient_card.pd.
- 19.Sabharwal CJ. HIV partner services and the field services unit. 2010. [cited 2009 Jun 24]. Available from: URL: http://www.nyc.gov/html/doh/downloads/ppt/dires/provider_outreach_pres_2010_jpg.ppt.
- 20.Cohen MS, Gay C, Kashuba AD, Blower S, Paxton L. Narrative review: antiretroviral therapy to prevent the sexual transmission of HIV-1. Ann Intern Med. 2007;146:591–601. doi: 10.7326/0003-4819-146-8-200704170-00010. [DOI] [PubMed] [Google Scholar]
- 21.Hutchinson AB, Farnham PG, Dean HD, Ekwueme DU, del Rio C, Kamimoto L, et al. The economic burden of HIV in the United States in the era of highly active antiretroviral therapy: evidence of continuing racial and ethnic differences. J Acquir Immune Defic Syndr. 2006;43:451–7. doi: 10.1097/01.qai.0000243090.32866.4e. [DOI] [PubMed] [Google Scholar]