Abstract
Over time, leg prostheses have improved in design, but have been incapable of actively adapting to different walking velocities in a manner comparable to a biological limb. People with a leg amputation using such commercially available passive-elastic prostheses require significantly more metabolic energy to walk at the same velocities, prefer to walk slower and have abnormal biomechanics compared with non-amputees. A bionic prosthesis has been developed that emulates the function of a biological ankle during level-ground walking, specifically providing the net positive work required for a range of walking velocities. We compared metabolic energy costs, preferred velocities and biomechanical patterns of seven people with a unilateral transtibial amputation using the bionic prosthesis and using their own passive-elastic prosthesis to those of seven non-amputees during level-ground walking. Compared with using a passive-elastic prosthesis, using the bionic prosthesis decreased metabolic cost by 8 per cent, increased trailing prosthetic leg mechanical work by 57 per cent and decreased the leading biological leg mechanical work by 10 per cent, on average, across walking velocities of 0.75–1.75 m s−1 and increased preferred walking velocity by 23 per cent. Using the bionic prosthesis resulted in metabolic energy costs, preferred walking velocities and biomechanical patterns that were not significantly different from people without an amputation.
Keywords: walking, metabolic cost, biomechanics, prosthesis, bionic, amputee
1. Introduction
A biological leg must support body weight and accelerate body mass to facilitate normative walking [1–3]. During a single stride, the net mechanical work done on the body's centre of mass is nearly zero, but the leg muscles perform both negative and positive work on the centre of mass [4] to enable forward walking at a steady velocity. The biological calf muscles generate nearly 80 per cent of the mechanical work required to complete each gait cycle [5,6] and typically perform greater positive than negative work during each stance period of level-ground walking [5,7,8]. The magnitude of net positive work per step performed at the ankle joint increases with walking velocity [5,7,8]. By contrast, commercially available passive-elastic prostheses, which comprise carbon fibre springs, can only store and release elastic strain energy while in contact with the walking surface, but cannot generate net positive work. These passive-elastic prostheses release less than one-half of the mechanical energy, and less than one-eighth of the mechanical power normally generated from the soleus and gastrocnemius [9–11]—calf muscles primarily responsible for propulsion and ankle extension during walking.
While using commercially available passive-elastic prostheses, people with a leg amputation (PWA) require 10–30% more metabolic energy to walk at the same velocities as non-amputees [12–14]. This metabolic discrepancy becomes more pronounced at faster walking velocities [12–15]. A greater metabolic energy demand implies that PWA tire more readily, and select slower preferred walking velocities compared with non-amputees [12]. The elevated metabolic demand and slower preferred velocities of PWA are probably explained by the inability of passive-elastic prostheses to provide the net positive work normally done by calf muscles during the push-off phase of walking [9,10]. Previous analytical studies of walking have shown that the application of a push-off force by the trailing leg just prior to the leading leg heel-strike is the most efficient method of replacing the large energy losses that occur during the step-to-step transition [3,16].
A critical objective in the field of prosthetic leg design is to advance an ankle–foot prosthesis capable of emulating the dynamics of the biological ankle. Some recent research has led to the development of quasi-passive ankle–foot prostheses that use active damping or spring-clutch mechanisms to automatically adjust prosthetic ankle angle for distinct ground surfaces [17–20], or to allow improved metabolic walking economy [21]. These quasi-passive devices do not include an actuator that can actively plantar-flex the prosthetic ankle during the terminal stance phase, so no net work is performed during a step, as is not the case with the biological ankle during walking [8,22–24]. The first powered ankle–foot prosthesis capable of performing net positive work was built by Klute et al. [25] in 1998. This device employed pneumatic actuation with off-board power. In 2007, Versluys et al. [26] also designed a powered ankle–foot prosthesis with pneumatic actuation and off-board power. The design and development of energetically autonomous powered systems has been the focus of more recent work [27–34]. In this article, we further develop and clinically analyse the autonomous ankle–foot prosthetic designs described earlier [27–33,35–37].
An autonomous powered prosthesis capable of using elastic energy, performing net positive work and generating a push-off force could greatly improve the walking performance of PWA [8,38]. We hypothesized that if biologically equivalent mechanics were supplied by a prosthetic ankle joint, PWA would achieve metabolic energy costs, preferred walking velocities and biomechanics not significantly different from those of non-amputees.
2. Material and methods
(a). Bionic prosthesis
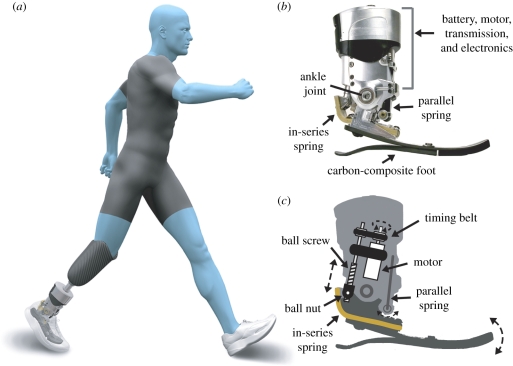
A bionic ankle–foot prosthesis (figure 1a) has been designed with both passive and active components that facilitate the generation of net positive work at the prosthetic ankle joint during the stance phase of walking [32,36,37]. This powered prosthesis performs negative and positive work by employing a series-elastic actuator, comprising a brushless motor and ball-screw transmission in series with a carbon-composite leaf spring (figure 1b,c). The motor's rotary motion is converted into linear motion through the ball-screw transmission. The in-series leaf spring improves motor efficiency by storing and returning some of the energy delivered by the motor. In parallel with the series-elastic actuator is a unidirectional leaf spring that stores energy for prosthetic ankle angles of less than 90° and becomes unattached at angles of greater than 90°. A carbon-composite foot at the base of the prosthesis provides additional compliance in the heel and forefoot. The mass of the prosthesis is 2 kg, designed to emulate the mass of a biological foot and partial shank of an 80 kg person [39]. The overall configuration is autonomous; all the electronics and a Lithium-Polymer battery that provides energy to the motor are housed within the prosthesis. Further details on the hardware and software designs of the powered prosthesis can be found in [32,36,37].
Figure 1.
Bionic ankle–foot prosthesis. (a) The bionic prosthesis attaches to the socket via a pylon and has a mass of 2 kg, equivalent to the biological foot and partial shank of an 80 kg person [39]. (b) The prosthesis includes an actuator in-series with a carbon-fibre leaf spring, in parallel with a unidirectional leaf spring, and heel and forefoot leaf springs that provide elasticity. (c) A series-elastic actuator performs negative and positive work. The actuator comprises a 200 W DC brushless motor (Maxon EC-Powermax 30) and ball-screw transmission (Nook 14 × 3 mm) in series with a carbon-composite leaf spring. A 0.22 kg Lithium-polymer rechargeable battery provides energy to the motor. The prosthesis is 67% efficient; approximately 30 J of electrical energy produce 20 J of net positive work during the stance period of walking, the typical energy requirement for an 80 kg person walking at 1.75 m s−1 [35]. A charged battery produces 4000–5000 steps, sufficient to walk 4–5 km at 1.75 m s−1 and exceeding the 3060 ± 1890 steps per day typically walked by an active PWA [40].
The wireless communication system for the bionic prosthesis allows for ankle stiffness and power delivery to be adjusted in real time while a person with an amputation is walking using the prosthesis. The magnitude and timing of power delivery are measured directly from sensors within the prosthesis and then adjusted to match the performance of a biological ankle. The sensors include motor shaft and ankle joint output encoders, and a 6 d.f. inertial measurement unit comprising three accelerometers and three rate gyroscopes. Similar to biological muscle reflex responses that use afferent feedback to modulate muscle force [41], the bionic prosthesis is capable of positive force feedback (for details of the control scheme, see [36,37]); an increase in the sensed prosthetic ankle joint torque triggers an increase in the torque generated by the actuator during mid- to late-stance phase, resulting in an increase in net positive ankle work production as walking velocity increases.
(b). Subjects
We tested the effects of using the bionic prosthesis by analysing the metabolic energy requirements, preferred walking velocities and biomechanical patterns of seven healthy adult males with a unilateral transtibial amputation and seven age-, height- and weight-matched non-amputees across walking velocities of 0.75–1.75 m s−1. All participants gave informed written consent prior to participation according to the Department of Veterans Affairs Research Service Institutional Review Board. Participants with an amputation were at least 2 years post-amputation, had an amputation owing to trauma, were at or above a K3 level of ambulation and had no known cardiovascular, pulmonary or neurological disease or disorder, and no additional musculoskeletal problems (table 1). A K3 level of ambulation, as defined by Medicare, requires that a person has the ability or potential for ambulation with variable cadence, has the ability to traverse most environmental barriers and may have vocational, therapeutic or exercise activity that demands prosthetic use beyond simple locomotion [42]. Prior to participation, PWA were evaluated by a certified prosthetist who quantified and confirmed the level of amputation and disability. All participants with an amputation used a commercially available passive-elastic prosthesis to walk during their normal daily activities.
Table 1.
Anthropometric characteristics. (Individual and average (s.d.) anthropometric characteristics from PWA with their own commercially available passive-elastic prosthesis, and average (s.d.) anthropometric characteristics from matched non-amputees.)
| participant | age (years) | height (m) | mass (kg) | leg length (m) | years since amputation | prosthesis |
|---|---|---|---|---|---|---|
| 1 | 37 | 1.89 | 90.0 | 1.02 | 17 | Ossur Flex-Foot, VSP |
| 2 | 45 | 1.74 | 92.7 | 0.93 | 19 | College Park, Venture |
| 3 | 50 | 1.74 | 90.7 | 0.92 | 39 | Freedom Innov. Renegade |
| 4 | 50 | 1.80 | 106.7 | 0.98 | 31 | Ossur Flex-Foot, Re-Flex VSP |
| 5 | 60 | 1.84 | 91.0 | 1.04 | 7 | Freedom Innov. Silhouette |
| 6 | 39 | 1.94 | 111.0 | 1.02 | 20 | Ossur Flex-Foot, Vari-Flex EVO |
| 7 | 42 | 1.82 | 112.7 | 1.00 | 20 | Otto Bock, Axtion |
| participant average (s.d.) | 46 (8) | 1.82 (0.07) | 99.5 (10.2) | 0.99 (0.05) | 21.9 (10.3) | |
| non-amputee average (s.d.) | 49 (9) | 1.86 (0.06) | 97.5 (12.1) | 1.01 (0.04) | ||
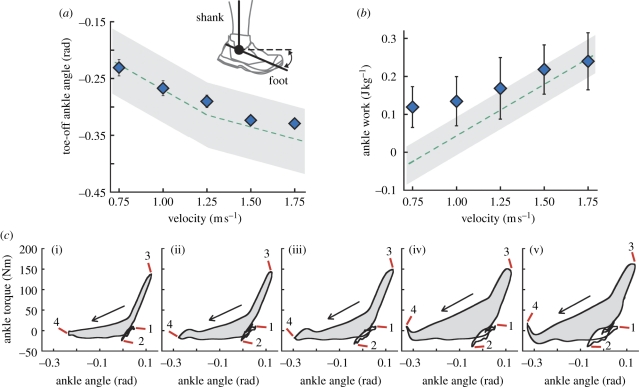
PWA completed two experimental sessions; one using the bionic prosthesis and one using their own passive-elastic prosthesis. Non-amputee participants completed one experimental session. All data were collected at the Gait and Motion Analysis Laboratory of the Providence, RI VA Medical Center, Center for Restorative and Regenerative Medicine. Before experimental sessions with the bionic prosthesis, PWA completed a fitting and acclimation session of at least 2 h. During this session, a certified prosthetist ensured that the bionic prosthesis was properly fitted and aligned. Then, we adjusted the stiffness, damping and power delivery of the bionic prosthesis so that the prosthetic ankle angle at toe-off and the net positive mechanical work matched the average biological ankle data [22,23] within 2 s.d. of the mean (figure 2a,b). Prosthetic ankle torque and angle were measured directly from sensors within the bionic prosthesis during the stance phase of walking, and ankle joint work was calculated from the integral of ankle torque with respect to angle (figure 2c). All values were saved and subsequently implemented during experimental sessions.
Figure 2.
Ankle angle, work and torque versus angle across walking velocities. (a) Average ankle angle at toe-off and (b) ankle work per step during the stance phase of walking for PWA using the powered prosthesis (blue diamonds) were within 2 s.d. of the mean data for non-amputees (green dashed lines). Non-amputee toe-off data are extrapolated from Winter [22] and ankle work data are from Palmer [23]. The foot segment is perpendicular to the shank segment at an ankle angle of zero (inset in (a)). Error bars indicate s.e.m. Grey shaded areas represent ±1 s.d. of the non-amputee average. (c) The prosthetic ankle joint torque versus angle for a representative participant with an amputation using the bionic prosthesis illustrates the positive work (grey shaded areas within the traces) provided by the prosthesis. 1, heel strike; 2, foot flat; 3, maximum dorsiflexion; 4, toe-off. (i) 0.75 m s−1; (ii) 1.00 m s−1; (iii) 1.25 m s−1; (iv) 1.50 m s−1; (v) 1.75 m s−1.
(c). Metabolic cost of transport and preferred velocity
We measured and compared gross rates of oxygen consumption and carbon dioxide production using a portable metabolic analysis system (Cosmed K4b2, IT) while participants walked at five constant velocities (0.75, 1.00, 1.25, 1.50 and 1.75 m s−1) on a level treadmill (Sole Fitness F85). The velocity trial order was randomized and participants had at least 2 min rest between trials. We calculated average steady-state metabolic power in Watts (W) from 4–6 min of each trial using a standard equation [43]. Then, we divided the metabolic power by each participant's weight and velocity to calculate the metabolic cost of transport (J Nm−1). Following metabolic measurements, we determined preferred walking velocity by incrementally increasing and decreasing the treadmill velocity until each participant ascertained the velocity that they felt most comfortable.
(d). Step-to-step transition work
We calculated step-to-step transition work, the work done by each individual leg on the centre of mass during transitions, using the individual limbs method described by Donelan et al. [44]. To estimate the time when the step-to-step transition occurred, we used the double support phase of walking, when both feet are in contact with the ground. We calculated step-to-step transition work from the time-integral of external mechanical power during double support. We determined external mechanical power from the dot product of each leg's resultant ground reaction force and the instantaneous centre of mass velocity. We calculated each leg's resultant ground reaction force from the vector sum of the vertical (Fz), horizontal (Fy) and lateral (Fx) ground reaction forces acting on each leg. Individual leg ground reaction forces were measured at 1000 Hz as participants walked at 0.75, 1.00, 1.25, 1.50 and 1.75 m s−1 across two separate force platforms (Advanced Medical Technology Incorporated, Watertown, MA, USA) embedded in a 10 m level walkway. We measured forward velocity from a reflective marker placed over the 7th cervical vertebrae using a motion analysis system (Qualysis, Gothenburg, Sweden) sampled at 200 Hz. Only trials that were within 0.05 m s−1 of the given velocity were analysed. Ground reaction force data were filtered with a fourth-order zero lag Butterworth 60 Hz low-pass digital filter (MATLAB, Mathworks, Natick, MA, USA). Centre of mass velocities (vcom) were obtained by calculating the time-integral of the centre of mass accelerations using the following equations [45]:
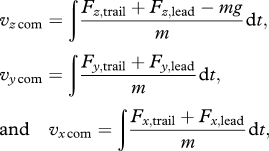 |
where ‘trail' indicates the trailing leg, ‘lead' indicates the leading leg, m the body mass and g the acceleration due to gravity (−9.81 m s−2). Integration constants for vertical (vz) and lateral (vx) velocities were determined by assuming that the average vcom over a stride equalled zero. The integration constant for horizontal velocity (vy) was determined by assuming that the average vcom over a stride equalled forward walking velocity. To isolate the period of double support, we determined the time period when the vertical ground reaction force for both legs exceeded 5 N. We calculated step-to-step transition work during double support, divided by each participant's mass in kilograms and averaged three steps per subject at each velocity. We were primarily interested in understanding how net positive ankle work from the bionic prosthesis, specifically the power delivered during late stance phase, affected the overall mechanical work done on the centre of mass, so we have analysed and presented data where the trailing leg is always the leg using a prosthesis and the leading leg is always the biological leg for PWA.
(e). Statistics
We used one-way ANOVAs to compare between PWA and non-amputee participants, and used repeated-measures ANOVAs to compare results between prosthetic feet. Significant differences were further analysed with a Tukey HSD follow-up procedure, where significant differences were detected as p < 0.05. We performed follow-up statistical power analyses on our data with n = 7 for metabolic cost of transport and step-to-step transition work [46]. At the velocities measured, we calculated an average statistical power of 0.96 to detect a 15 per cent difference and of 0.74 to detect a 10 per cent difference in the metabolic cost of transport. We also calculated an average statistical power of 0.84 to detect a 15 per cent difference and of 0.58 to detect a 10 per cent difference in the trailing leg step-to-step transition work. Thus, we believe we had adequate statistical power to conclude that PWA using the bionic prosthesis had equivalent metabolic demands and trailing leg step-to-step transition work compared with non-amputees.
3. Results
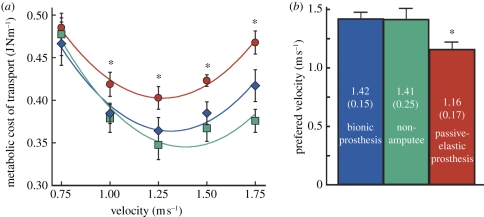
PWA using the bionic prosthesis during walking normalized metabolic energy costs compared with non-amputees. At 0.75, 1.0, 1.25, 1.5 and 1.75 m s−1, the metabolic costs of transport were 0.47, 0.39, 0.36, 0.39 and 0.42 J Nm−1, respectively, for PWA using the bionic prosthesis, and 0.48, 0.38, 0.35, 0.37 and 0.38 J Nm−1, respectively, for non-amputees. Compared with using the bionic prosthesis, the metabolic costs of transport for PWA using a passive-elastic prosthesis were not significantly different at 0.75 m s−1, but were 8.9, 10.6, 9.9 and 12.1 per cent greater (p < 0.01) at 1.0, 1.25, 1.5 and 1.75 m s−1, respectively (figure 3a). When PWA walked at a freely chosen velocity while using the bionic prosthesis they preferred to walk 1.4 m s−1, equivalent to the preferred velocity of non-amputees (figure 3b). Compared with using their own passive-elastic prosthesis, PWA using the bionic prosthesis preferred to walk at a 23 per cent faster velocity.
Figure 3.
Gross metabolic cost of transport and preferred walking velocity. (a) PWA using the bionic prosthesis (blue diamonds) had nearly the same average metabolic cost of transport (COT) as non-amputees (green squares) (p > 0.50 for 0.75–1.50 m s−1; p = 0.17 for 1.75 m s−1). Cost of transport is the metabolic energy needed to transport unit weight a unit distance, equal to (metabolic demand)/(body weight × distance travelled). PWA using a passive-elastic prosthesis (red circles) had 11–25% greater cost of transport (p < 0.05) at 1.00–1.75 m s−1 compared with non-amputees. (b) Average preferred walking velocities of PWA using the bionic prosthesis (blue bar) and non-amputees (green bar) were equivalent (p = 0.97). PWA using a passive-elastic prosthesis (red bar) preferred to walk significantly slower (p = 0.008). Values within bars indicate averages (s.e.m.). Asterisks (*) indicate significant differences between PWA using the bionic prosthesis compared with using a passive-elastic prosthesis. Error bars indicate s.e.m. Second-order polynomial curve equations in (a) are, non-amputee: COT = 0.303v2 – 0.846v + 0.934, r2 = 0.49; bionic prothesis: COT = 0.308v2 – 0.808v + 0.895, r2 = 0.39; and passive-elastic prosthesis: COT = 0.295v2 – 0.750v + 0.295, r2 = 0.52. COT is calculated in Joules per Newton body weight per metre. v is velocity in metres per second.
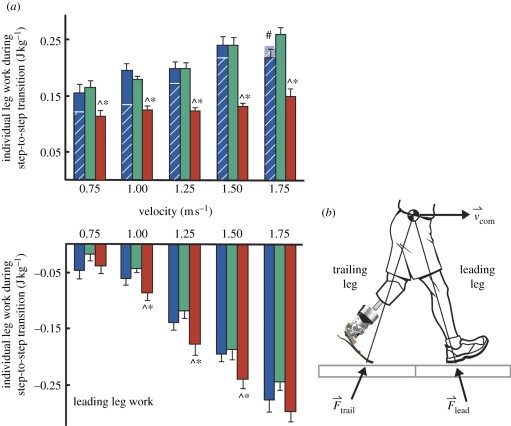
Appropriate delivery of positive prosthetic ankle work prior to and during step-to-step transitions was presumably the reason underlying improvements in the metabolic costs and preferred walking velocities of PWA using the bionic prosthesis. The bionic prosthesis provided high peak ankle power at the end of the single support phase to facilitate forward propulsion, and the redirection and acceleration of the body's centre of mass [3,44]. We quantified the effects of positive prosthetic ankle power on the overall biomechanics of the body by calculating step-to-step transition work [44] during double-support. Previous studies have established that step-to-step transition work exacts a proportional metabolic cost [3,44] and is a major determinant of the metabolic cost of walking [1,2]. We found that the positive work done by the trailing leg, the push-off work, was not different between the legs of PWA using the bionic prosthesis and the legs of non-amputees across velocities of 0.75–1.5 m s−1 (figure 4). At 0.75, 1.0, 1.25, 1.5 and 1.75 m s−1, trailing leg work was 0.16, 0.19, 0.20, 0.24 and 0.22 J kg−1, respectively, for PWA using the bionic prosthesis and was 0.17, 0.18, 0.20, 0.24 and 0.26 J kg−1, respectively, for non-amputees. PWA using the bionic prosthesis generated significantly greater push-off work in their prosthetic trailing leg compared with that when using a passive-elastic prosthetic foot (figure 4a). Compared with using the bionic prosthesis, trailing leg work for PWA using a passive-elastic prosthesis was 26.7, 35.9, 38.2, 45.3 and 31.6 per cent less (p < 0.006) at 0.75, 1.0, 1.25, 1.5 and 1.75 m s−1, respectively (figure 4a). We also found that the negative work done by the leading leg, the collision work, was not different between PWA using the bionic prosthesis and non-amputees (figure 4). At 0.75, 1.0, 1.25, 1.5 and 1.75 m s−1, the leading leg work was −0.05, −0.06, −0.14, −0.20 and −0.28 J kg−1, respectively, for PWA using the bionic prosthesis and was −0.02, −0.04, −0.12, −0.19 and −0.24 J kg−1, respectively, for non-amputees. By contrast, the collision work done by the leading biological leg of PWA using a passive-elastic prosthesis was significantly greater compared with that using the bionic prosthesis and to non-amputees at walking velocities of 1.0–1.5 m s−1. Compared with using the bionic prosthesis, leading leg work for PWA using a passive-elastic prosthesis was 41.1, 26.8 and 22.6 per cent greater (p < 0.05) at 1.0, 1.25 and 1.5 m s−1, respectively.
Figure 4.
Step-to-step transition work. (a) Average individual leg mechanical step-to-step transition work from PWA using the bionic prosthesis (blue bars) was not different from non-amputees (green bars) except for trailing leg work at 1.75 m s−1. The leg using a prosthesis is always the trailing leg and the biological leg is always the leading leg in PWA. Average ankle work per step attributed to the bionic prosthesis (white stripes overlaid on trailing leg blue bars) comprised approximately 87% of the overall trailing leg work done on the centre of mass across all velocities. At 1.75 m s−1, the ankle work performed by the bionic prosthesis was greater than the trailing leg step-to-step transition work, implying that ankle work was dissipated at the knee and/or hip joints. PWA using a passive-elastic prosthesis (red bars) generated significantly less trailing leg work and experienced greater leading leg collision work compared with using the bionic prosthesis and to non-amputees. The hash sign (#) indicates a significant difference between PWA using the bionic prosthesis and non-amputees, asterisks (*) indicate significant differences between PWA using the bionic prosthesis compared with using a passive-elastic prosthesis, and carets (^) indicate significant differences between non-amputees and PWA using a passive-elastic prosthesis (p < 0.05). Error bars indicate s.e.m. (b) Step-to-step transition work equals the time-integral of mechanical power (Watts with respect seconds). Mechanical power is the dot product of each leg's ground reaction force (Ftrail and Flead) and the instantaneous centre of mass velocity (vcom) [44].
4. Discussion
Commercially available passive-elastic prostheses store and return elastic strain energy while in contact with the ground during walking, but they cannot provide net positive ankle work, work that is necessary for efficient transition from step-to-step during walking. The bionic ankle generates net positive work by using a battery rather than metabolic energy. Thus, PWA using the bionic prosthesis experienced normative ankle mechanics and push-off work in their trailing leg (figure 4), yet did not incur the full metabolic penalty associated with producing that work. Also, PWA using the bionic prosthesis preferred to walk at the same velocity as non-amputees, suggesting that use of the bionic prosthesis improved functional ability [12,47].
Although use of the battery powered prosthesis normalized metabolic cost in PWA compared with non-amputees, it did not augment metabolic cost below normative levels (figure 3a). We estimated the metabolic contribution made by the motor assuming that the mechanical work done by the motor could replace the mechanical work done by the muscles. For example, the bionic prosthesis performs an average of 23.86 J of net positive work during the stance period of level walking at 1.75 m s−1. Assuming muscle has 25 per cent efficiency to perform positive work [4], 23.86 J of positive mechanical work would account for an estimated 95.44 J of metabolic energy, roughly equivalent to a metabolic cost of transport of 0.056 (normalized to average body weight of participants with an amputation and while walking 1.75 m s−1). PWA using a passive-elastic prosthesis had a metabolic cost of transport of 0.468 and decreased metabolic cost of transport by 0.051 when using the bionic prosthesis, only 0.005 less than the cost estimated from the work done by the motor.
Factors that could contribute to metabolic normalization but not augmentation in PWA using the bionic prosthesis may include limited energy transfer between the bionic prosthesis and the proximal leg owing to the lack of a rigid interface connecting the residual limb to the socket, the lack of a working gastrocnemius muscle in the residual limb of PWA, and compromised walking stability. The residual limb is connected to the socket using friction and suction from a sleeve surrounding the skin's surface, but there can be considerable movement between the limb and the socket, which would decrease the energy transferred from the bionic prosthesis to the proximal leg. The bi-articular gastrocnemius spans the ankle and knee joints in the biological leg, allows energy to be transferred between the ankle and knee [48,49], and contributes to whole-body angular momentum [50]. Without effective energy transfer between the prosthetic ankle and biological knee joint, additional proximal muscles are probably recruited to compensate, which would incur metabolic penalties for PWA. Finally, PWA may have compromised stability compared with non-amputees when walking on a treadmill, which may increase metabolic demands. Future bionic devices that solve issues of attachment, effective energy transfer and stability could further improve metabolic costs, potentially allowing PWA to walk with less metabolic energy than people with biological limbs.
We found that with adequate power provided by a bionic prosthetic ankle, high-functioning PWA achieved normative metabolic energy costs, preferred walking velocities and mechanical work compared with non-amputees. Never before has a lower limb prosthetic device been able to emulate biological function in this manner.
Acknowledgements
All participants gave informed written consent prior to participation according to the Department of Veterans Affairs Research Service Institutional Review Board.
This research is sponsored by a Career Development Award given to A.M.G. from the Rehabilitation, Research and Development Service, Department of the Veterans Affairs and the Center for Restorative and Regenerative Medicine Providence VA Medical Center (VA RR&D A3962R). The authors thank Susan D'Andrea and Natalie Wilhelm for their assistance in data collection. The authors also thank iWalk, Inc. for providing the bionic prostheses and technical assistance.
The authors declare a competing financial interest: Author Hugh Herr is Chief Scientific Officer, consultant, and stock owner in iWalk, Inc., a company in Cambridge, MA commercializing the Bionic Ankle–Foot Prosthesis.
References
- 1.Donelan J. M., Kram R., Kuo A. D. 2002. Mechanical work for step-to-step transitions is a major determinant of the metabolic cost of human walking. J. Exp. Biol. 205, 3717–3727 [DOI] [PubMed] [Google Scholar]
- 2.Grabowski A., Farley C. T., Kram R. 2005. Independent metabolic costs of supporting body weight and accelerating body mass during walking. J. Appl. Physiol. 98, 579–583 10.1152/japplphysiol.00734 (doi:10.1152/japplphysiol.00734) [DOI] [PubMed] [Google Scholar]
- 3.Kuo A. D., Donelan J. M., Ruina A. 2005. Energetic consequences of walking like an inverted pendulum: Step-to-step transitions. Exerc. Sport Sci. Rev. 33, 88–97 10.1097/00003677-200504000-00006 (doi:10.1097/00003677-200504000-00006) [DOI] [PubMed] [Google Scholar]
- 4.Margaria R. 1968. Positive and negative work performances and their efficiencies in human locomotion. Int. Z. Angew. Physiol. 25, 339–351 10.1007/BF00699624 (doi:10.1007/BF00699624) [DOI] [PubMed] [Google Scholar]
- 5.Winter D. A. 1983. Energy generation and absorption at the ankle and knee during fast, natural, and slow cadences. Clin. Ortho. Rel. Res. 175, 147–154 [PubMed] [Google Scholar]
- 6.Soo C. H., Donelan J. M. 2010. Mechanics and energetics of step-to-step transitions isolated from human walking. J. Exp. Biol. 213, 4265–4271 10.1242/jeb.044214 (doi:10.1242/jeb.044214) [DOI] [PubMed] [Google Scholar]
- 7.DeVita P., Helseth J., Hortobagyi T. 2007. Muscles do more positive than negative work in human locomotion. J. Exp. Biol. 210, 3361–3373 10.1242/jeb.003970 (doi:10.1242/jeb.003970) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen A. H., Childress D. S., Miff S. C., Gard S. A., Mesplay K. P. 2004. The human ankle during walking: implications for design of biomimetic ankle prostheses. J. Biomech. 37, 1467–1474 10.1016/j.jbiomech.2004.01.017 (doi:10.1016/j.jbiomech.2004.01.017) [DOI] [PubMed] [Google Scholar]
- 9.Bateni H., Olney S. J. 2002. Kinematic and kinetic variations of below-knee amputee gait. Prosth. Orthot. Sci. 14, 2–10 10.1097/00008526-200203000-00003 (doi:10.1097/00008526-200203000-00003) [DOI] [Google Scholar]
- 10.Zmitrewicz R. J., Neptune R. R., Walden J. G., Rogers W. E., Bosker G. W. 2006. The effect of foot and ankle prosthetic components on braking and propulsive impulses during transtibial amputee gait. Arch. Phys. Med. Rehabil. 87, 1334–1339 10.1016/j.apmr.2006.06.013 (doi:10.1016/j.apmr.2006.06.013) [DOI] [PubMed] [Google Scholar]
- 11.Zmitrewicz R. J., Neptune R. R., Sasaki K. 2007. Mechanical energetic contributions from individual muscles and elastic prosthetic feet during symmetric unilateral transtibial amputee walking: a theoretical study. J. Biomech. 40, 1824–1831 10.1016/j.jbiomech.2006.07.009 (doi:10.1016/j.jbiomech.2006.07.009) [DOI] [PubMed] [Google Scholar]
- 12.Hsu M. J., Nielsen D. H., Lin-Chan S. J., Shurr D. 2006. The effects of prosthetic foot design on physiologic measurements, self-selected walking velocity, and physical activity in people with transtibial amputation. Arch. Phys. Med. Rehabil. 87, 123–129 10.1016/j.apmr.2005.07.310 (doi:10.1016/j.apmr.2005.07.310) [DOI] [PubMed] [Google Scholar]
- 13.Torburn L., Powers C. M., Guiterrez R., Perry J. 1995. Energy-expenditure during ambulation in dysvascular and traumatic below-knee amputees: a comparison of 5 prosthetic feet. J. Rehabil. Res. Dev. 32, 111–119 [PubMed] [Google Scholar]
- 14.Waters R. L., Mulroy S. 1999. The energy expenditure of normal and pathologic gait. Gait Posture 9, 207–231 10.1016/S0966-6362(99)00009-0 (doi:10.1016/S0966-6362(99)00009-0) [DOI] [PubMed] [Google Scholar]
- 15.Genin J. J., Bastien G. J., Franck B., Detrembleur C., Willems P. A. 2008. Effect of speed on the energy cost of walking in unilateral traumatic lower limb amputees. Eur. J. Appl. Physiol. 103, 655–663 10.1007/s00421-008-0764-0 (doi:10.1007/s00421-008-0764-0) [DOI] [PubMed] [Google Scholar]
- 16.Kuo A. D., Donelan J. M. 2010. Dynamic principles of gait and their clinical implications. Phys. Therapy 90, 157–174 10.2522/ptj.20090125 (doi:10.2522/ptj.20090125) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koniuk W. 2002. Self-adjusting prosthetic ankle apparatus. US Patent no. 6 443993
- 18.Li C., Tokuda M., Furusho J., Koyanagi K., Morimoto S., Hashimoto Y., Nakagawa A., Akazawa Y. 2006. Research and development of the intelligently-controlled prosthetic ankle joint. In Proc. IEEE Int. Conf. Mechatronics Autom., Luoyang, Henan, 25–28 June 2006, pp. 1114–1119. IEEE 10.1109/ICMA.2006.257781 (doi:10.1109/ICMA.2006.257781) [DOI] [Google Scholar]
- 19.Ossur Inc. 2008. PROPRIO FOOT with EVO design. See www.ossur.com .
- 20.Williams R. J., Hansen A. H., Gard S. A. 2009. Prosthetic ankle–foot mechanism capable of automatic adaptation to the walking surface. J. Biomech. Eng. Trans. ASME 131, 035002. 10.1115/1.3005335 (doi:10.1115/1.3005335) [DOI] [PubMed] [Google Scholar]
- 21.Collins S. H., Kuo A. D. 2010. Recycling energy to restore impaired ankle function during human walking. PLoS ONE 5, e9307. 10.1371/journal.pone.0009307 (doi:10.1371/journal.pone.0009307) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winter D. A. 1983. Biomechanical motor patterns in normal walking. J. Motor Behav. 15, 302–330 [DOI] [PubMed] [Google Scholar]
- 23.Palmer M. L. 2002. Sagittal plane characterization of normal human ankle function across a range of walking speeds. Masters thesis, Massachusetts Institute of Technology, MA, USA [Google Scholar]
- 24.Hof A. L., Geelen B. A., Vandenberg J. 1983. Calf muscle moment, work and efficiency in level walking: role of series elasticity. J. Biomech. 16, 523–537 10.1016/0021-9290(83)90067-2 (doi:10.1016/0021-9290(83)90067-2) [DOI] [PubMed] [Google Scholar]
- 25.Klute G. K., Czernieki J., Hannaford B. 1998. Development of powered prosthetic lower limb. Presented at the 1st Natl Meeting, Veterans Affairs Rehabil. R&D Service, 1–3 October 1998, Washington, DC. Department of Veterans Affairs Rehabilitation, Research and Development Service [Google Scholar]
- 26.Versluys R., Peeraer L., Van der Perre G., Van Gheluwe B., Lefeber D. 2007. Design of a powered below-knee prosthesis. Presented at the 12th World Congr. Int. Soc. Prosthet. Orthot. 29 July–3 August 2007. Vancouver, BC, Canada [Google Scholar]
- 27.Au S. K., Bonato P., Herr H. 2005. An EMG-position controlled system for an active ankle-foot prosthesis: an initial experimental study. In Proc. IEEE Int. Conf. Rehabil. Robot, 28 June-1 July 2005, Chicago, IL, USA, pp. 375–379 10.1109/ICORR.2005.1501123 (doi:10.1109/ICORR.2005.1501123) [DOI] [Google Scholar]
- 28.Au S. K., Herr H. 2006. Initial experimental study on dynamic interaction between an amputee and a powered ankle-foot prosthesis. Presented at Dyn. Walking: Mech. Control Hum. Robot. Locomotion, 6–8 May 2006, Ann Arbor, MI, USA [Google Scholar]
- 29.Au S. K., Weber J., Herr H. 2007. Biomechanical design of a powered ankle-foot prosthesis. In IEEE 10th Int. Conf. on Rehab. Robotics, Noordwijk, The Netherlands pp. 298–303 IEEE [Google Scholar]
- 30.Au S. K., Herr H., Weber J., Martinez-Villalpando E. C. 2007. Powered ankle-foot prosthesis for the improvement of amputee ambulation. In Proc. Annual Int. Conf. of the IEEE Engineering in Medicine and Biology Society, New York, pp. 3020–3026 IEEE; [DOI] [PubMed] [Google Scholar]
- 31.Herr H., Weber J., Au S. K. 2007. Powered ankle-foot prosthesis. In Proc. Biomech. Lower Limb Health, Dis. Rehabil., 3–5 September 2007, Manchester, UK, pp. 72–74 [Google Scholar]
- 32.Au S. K., Herr H. M. 2008. Powered ankle-foot prosthesis: the importance of series and parallel motor elasticity. IEEE Robot. Autom. Mag. 15, 52–59 10.1109/MRA.2008.927697 (doi:10.1109/MRA.2008.927697) [DOI] [Google Scholar]
- 33.Au S. K. 2009. A powered ankle-foot prosthesis that improves transtibital amputee ambulation. PhD thesis, Massachusetts Institute of Technology, Cambridge, MA [Google Scholar]
- 34.Hitt J., Bellman R., Holgate M., Sugar T., Hollander K. 2007. The sparky (spring ankle with regenerative kinetics) projects: design and analysis of a robotic transtibial prosthesis with regenerative kinetics. In Proc. ASME Int. Des. Eng. Tech. Conf., Las Vegas, NV, USA, pp. 1587–1598 [Google Scholar]
- 35.Au S. K., Weber J., Herr H. 2009. Powered ankle-foot prosthesis improves walking metabolic economy. IEEE Trans. Robot. 25, 51–66 10.1109/TRO.2008.2008747 (doi:10.1109/TRO.2008.2008747) [DOI] [Google Scholar]
- 36.Eilenberg M. F., Geyer H., Herr H. 2010. Control of a powered ankle-foot prosthesis based on a neuromuscular model. IEEE Trans. Neural Syst. Rehab. Eng. 18, 164–173 10.1109/TNSRE.2009.2039620 (doi:10.1109/TNSRE.2009.2039620) [DOI] [PubMed] [Google Scholar]
- 37.Markowitz J., Krishnaswamy P., Eilenberg M. F., Endo K., Barnhart C., Herr H. 2011. Speed adaptation in a powered transtibial prosthesis controlled with a neuromuscular model. Phil. Trans. R. Soc. B 366, 1621–1631 10.1089/rstb.2010.0347 (doi:10.1089/rstb.2010.0347) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanderson D. J., Martin P. E. 1997. Lower extremity kinematic and kinetic adaptations in unilateral below-knee amputees during walking. Gait Posture 6, 126–136 10.1016/S0966-6362(97)01112-0 (doi:10.1016/S0966-6362(97)01112-0) [DOI] [Google Scholar]
- 39.Dempster W. T. 1955. Space requirements of the seated operator. WADC Technical Report (TR-55-159) Wright-Patterson Air Force Base, OH [Google Scholar]
- 40.Stepien J. M., Cavenett S., Taylor L., Crotty M. 2007. Activity levels among lower-limb amputees: self-report versus step activity monitor. Arch. Phys. Med. Rehabil. 88, 896–900 10.1016/j.apmr.2007.03.016 (doi:10.1016/j.apmr.2007.03.016) [DOI] [PubMed] [Google Scholar]
- 41.Kandel E. R., Schwartz J. H., Jessell T. M. 2000. Principles of neural science, 4th edn. Columbus, OH: McGraw-Hill [Google Scholar]
- 42.Centers for Medicare and Medicaid Services 2001. US Department of Health and Human Services. HCFA Common Procedure Coding System (HCPCS). Springfield, VA: US Department of Commerce, National Technical Information Service; Chapter 5.3 [Google Scholar]
- 43.Brockway J. M. 1987. Derivation of formulae used to calculate energy expenditure in man. Hum. Nutr. Clin. Nutr. 41, 463–471 [PubMed] [Google Scholar]
- 44.Donelan J. M., Kram R., Kuo A. D. 2002. Simultaneous positive and negative external mechanical work in human walking. J. Biomech. 35, 117–124 10.1016/S0021-9290(01)00169-5 (doi:10.1016/S0021-9290(01)00169-5) [DOI] [PubMed] [Google Scholar]
- 45.Cavagna G. A. 1975. Force platforms as ergometers. J. Appl. Physiol. 39, 174–179 [DOI] [PubMed] [Google Scholar]
- 46.Lenth R. V. 2010. Java applets for power and sample size (Computer software). Retrieved 18 November 2010 from http://www.stat.uiowa.edu/~rlenth/power
- 47.Archer K. R., Castillo R. C., MacKenzie E. J., Bosse M. J. 2006. Gait symmetry and walking speed analysis following lower-extremity trauma. Phys. Therapy 86, 1630–1640 10.2522/ptj.20060035 (doi:10.2522/ptj.20060035) [DOI] [PubMed] [Google Scholar]
- 48.Zajac F. E., Neptune R. R., Kautz S. A. 2003. Biomechanics and muscle coordination of human walking. II. Lessons from dynamical simulations and clinical implications. Gait Posture 17, 1–17 10.1016/S0966-6362(02)00069-3 (doi:10.1016/S0966-6362(02)00069-3) [DOI] [PubMed] [Google Scholar]
- 49.Neptune R. R., Zajac F. E., Kautz S. A. 2004. Muscle force redistributes segmental power for body progression during walking. Gait Posture 19, 194–205 10.1016/S0966-6362(03)00062-6 (doi:10.1016/S0966-6362(03)00062-6) [DOI] [PubMed] [Google Scholar]
- 50.Neptune R. R., McGowan C. P. 2011. Muscle contributions to whole-body sagittal plane angular momentum during walking. J. Biomech. 44, 6–12 10.1016/j.jbiomech.2010.08.015 (doi:10.1016/j.jbiomech.2010.08.015) [DOI] [PMC free article] [PubMed] [Google Scholar]