Abstract
Objectives
To examine whether changes in cardiovascular disease (CVD) risk factors differ by baseline weight status among young adults who maintained or gained weight.
Design
Longitudinal cohort study.
Subjects
White and African Americans who either maintained (±5 pounds; n=488) or gained (>5 pounds; n=2788) weight over 15 years.
Measurements
Anthropometrics and CVD risk factors were measured at baseline (1985–1986) and follow-up. Participants were classified as normal weight (body mass index (BMI) 18.5–24.9 kg/m2) or overweight (BMI ≥25 kg/m2) at baseline. Multivariable models were stratified by ethnicity and weight change category.
Results
Normal weight maintainers tended to have more favorable risk factors at baseline and follow-up than overweight maintainers. Size and direction of 15-year changes in risk factors were similar by weight status, except that in white normal weight maintainers changes in high-density lipoprotein (HDL)-cholesterol (3.3 mg/dl (95% confidence interval (CI): 0.4, 6.3)) and triglycerides (−14.7 mg/dl (−25.8, −3.7)) were more favorable. Weight gain was associated with unfavorable changes in risk factors. Weight gainers normal weight at baseline had less adverse changes in glucose, blood pressure, HDL-cholesterol (whites only) and triglycerides (African Americans only) than overweight gainers. However, normal weight African-American weight gainers had more adverse changes in total (3.1 mg/dl (0.2, 6.1)) and low-density lipoprotein-cholesterol (3.4 mg/dl (0.6, 6.3)).
Conclusions
Baseline weight status does not appear to influence the size or direction of risk factor changes among adults who maintained their weight over 15 years. In contrast, weight gain was associated with changes in some risk factors differentially by baseline weight status.
Keywords: body weight changes, glucose, blood pressure, cholesterol, triglycerides
Introduction
In the United States, an estimated 45% of overweight (body mass index (BMI): ≥25.0 kg/m2) adults self-reported that they were ‘trying to lose weight’.1 Some of them will successfully lose weight; however, the majority of adults will regain the weight within 3–5 years.2,3 Given the difficulty adults experience in losing weight and maintaining the weight loss, a more feasible public health goal for some adults may be maintaining their current weight. In addition, it is important to clarify the potential health benefits of weight maintenance as opposed to weight gain in normal weight (BMI: 18.5–24.9 kg/m2). This is especially important during the transition period from young adulthood to middle age when most Americans gain weight.4,5 Major weight gain (≥5 BMI units) occurs in both normal and overweight women and men.4
The adverse effects of weight gain and the benefits of weight loss have been well documented; however, less is known about the effects of weight maintenance on cardiovascular disease (CVD) risk factors and whether these effects differ by baseline weight status. That is, does maintaining weight have a protective effect for further adverse changes in CVD risk, and is this effect better or worse for those who are overweight at baseline and, therefore, presumably have a more adverse risk factor profile at baseline? The two most relevant studies identified, while not definitive analyses on these issues, give results in opposite directions for maintaining versus gaining weight. St Jeor et al. examined both of these issues in data reflecting 5-year changes in lipids and blood pressure.6 The focus of this analysis was on developing a classification scheme to differentiate weight losers, maintainers and gainers. These authors reported significant differences between the weight change groups for some risk factors (more adverse in gainers than in maintainers or losers). The data presented suggested more adverse low-density lipoprotein (LDL) changes among maintainers who were obese at baseline versus normal weight at baseline, particularly among women. Norman et al. examined 10-year changes in lipids and blood pressure associated with weight gain in the Coronary Artery Risk Development in Young Adults (CARDIA) study cohort, but used data from non-weight gainers and weight losers combined as the comparison group.7 An analysis stratified on weight status suggested that LDL changes associated with weight gain were less adverse in those overweight at baseline. Although both studies found significant differences between weight maintenance and weight gain, neither study examined the impact of baseline weight status and CVD risk factors among weight maintainers or weight gainers separately.
This study specifically addresses the joint issues of weight maintenance versus gain and baseline weight status as potential influences on CVD risk factors, based on 15 years of follow-up in the CARDIA study. The risk factors examined were fasting glucose, systolic and diastolic blood pressure, total, LDL and high-density lipoprotein (HDL)-cholesterol, and triglycerides. We hypothesized that changes in risk factors over 15 years would be more adverse in adults overweight at baseline compared to adults’ normal weight at baseline, in both weight maintainers and weight gainers, and in both African-American and white men and women.
Materials and methods
Study population
The CARDIA study is a prospective observational study designed to examine the evolution of cardiovascular risk factors among 5115 young adults aged 18–30 at baseline (1985–1986). Participants were recruited from four clinical sites in Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA. Sampling was designed to achieve approximately equal distributions across gender, ethnicity (African American, white), age (18–24, 25–30 years) and education (high school or less, greater than high school) groups. The details of the study design and recruitment protocol have been described previously.8 Participants were re-examined at years 2, 5, 7, 10 and 15 with retention rates of 90, 86, 81, 79 and 74% of surviving participants, respectively. Approximately 2.5% of the study cohort died during the 15 years of follow-up. This study was approved by the Institutional Review Boards (IRB) at each field center and this analysis was approved by the University of North Carolina at Chapel Hill Public Health IRB.
Measures and covariates
Body weight was measured at all clinic examinations in light clothing to the nearest 0.2 pound using a balance beam scale. Height was measured to the nearest 0.5cm without shoes using a vertical ruler. Body mass index was calculated as weight in kilograms divided by height in meters squared. We excluded body weights if the participant was currently pregnant at any examination or had been pregnant (>13 gestational weeks) within the 180 days before clinic examination (n=724). Among participants who attended the 15-year examination, 90% had a valid measured weight for at least five of the six clinic examinations. Baseline weight status was categorized as normal weight or overweight.
Body weights measured over 15 years of follow-up were examined to identify participants who met our criteria for weight maintenance or weight gain. Participants were classified as weight maintainers if they met one of the two following conditions: (1) follow-up (year 15) weight was within 5 pounds of baseline (year 0) weight; or (2) baseline and follow-up weights were within 5 pounds of average weight calculated for each participant over all visits during the 15-year interval. Participants were classified as weight gainers if they did not meet either weight maintainer definition and gained greater than 5 pounds between baseline and the 15-year follow-up.
As a measure of weight fluctuation, we calculated the root mean square error deviation (RMSE) around the regression line of weight in relation to age for each subject, using all available measured weights. A low RMSE indicates less weight fluctuation and a large RMSE large weight fluctuation, independent of the overall trend (gain, loss, maintain). Root mean square error deviation was correlated with baseline BMI (r=0.47) and with 15-year weight change (r=0.21), indicating that participants who were heavier and who gained more weight had greater fluctuations in weight.
Study participants were asked to fast for 12 h before their clinic examination. Fasting blood samples were sent to the Northwest Lipid Research Laboratories, University of Washington (Seattle, WA, USA) for lipid determination. The laboratory participates in the Center for Disease Control and Prevention (CDC) lipids standardization program, and the samples were analyzed continuously. Total cholesterol and triglycerides were measured enzymatically within 6 weeks of collection.9 High-density lipoprotein-cholesterol was determined after dextran sulfate–magnesium chloride precipitation. 10 Low-density lipoprotein-cholesterol was calculated using the Friedewald equation.11 Low-density lipoprotein-cholesterol was not calculated for participants with triglyceride levels ≥400 mg/dl. Extensive quality control measures were taken to insure that changes in lipids were not the result of laboratory changes.12 Serum glucose levels were measured by a hexokinase method at Linco Research Inc. (St Charles, MO, USA). Blood pressure was measured three times after a 5-min rest using a Hawksley random zero sphygmomanometer (WA Baum Company, Copaige, NY, USA) on the right arm of the seated participant. The average of the last two measures was used for the analysis. Blood pressure was measured according to the same protocol at each exam. The 15-year changes in the risk factors were calculated as the difference between the baseline and 15-year follow-up measurements.
Age (date of birth), race/ethnicity and gender were self-reported during the recruitment phase and confirmed during the clinic visit. Educational attainment was based on self-reported number of years of schooling and the highest degree earned at the 15-year follow-up examination. Based on the participants’ responses, we created six education levels (less than high school education, high school graduate, associate degree, some college, bachelors degree and advanced degree). For some analyses, we combined the less than high school and high school groups and the associate degree and some college groups. Elapsed time between examinations was calculated using the baseline and follow-up examination dates. Based on the participants’ self-reported responses to questionnaires on cigarette smoking, alcoholic beverage consumption and physical activity at baseline and follow-up examinations, we created variables that reflected status at the beginning and end of the 15-year interval. Responses from the intermediate examinations were ignored. For cigarette smoking status, participants were classified as never-smokers (never-smoker at baseline and follow-up); former smokers (previous smoking history at baseline or follow-up) or current smokers (smoker at followup). The self-reported number of servings of alcoholic beverages (beer, wine and liquor) consumed per day was used to calculate average grams of alcohol consumed per day.13 The four categories created for alcoholic beverage consumption were none or rare (0 g/day at baseline and follow-up), current light to moderate (1–20 g/day at followup), current heavy (≥21 g/day) and former (≥1 g/day at baseline and 0 g/day at follow-up). Physical activity level was measured using the CARDIA physical activity history questionnaire, an interviewer-based self-report of duration and intensity of participation in 13 categories of exercise over the previous 12 months14,15 and expressed in ‘exercise units’. Cut points for the participation levels for total physical activity (low, medium and high) were based on the distribution of the whole cohort at baseline. Using data from the baseline and follow-up examinations, participants were classified into four mutually exclusive participation groups (consistently in the medium or high group, consistently in the low group, low at baseline and medium or high group at follow-up only, or medium or high at baseline and low at follow-up).
Exclusions
Participants were excluded if they were not measured in the 15-year follow-up examination (n=1443); missing baseline (n=15) or follow-up (n=63) weight; underweight (BMI <18.5 kg/m2) at baseline (n=145); a weight loser (n=167); or reported being diagnosed with diabetes before 18 years of age (n=6). For analyses of glucose, LDL-cholesterol or triglycerides, we excluded participants with fasting times less than 8 h at baseline (n=67) or follow-up (n=132). Additional participants were excluded for outcome-specific analyses if they were missing baseline or follow-up levels for glucose (n=149), blood pressure (n=10), total cholesterol (n=67), LDL-cholesterol (n=162), HDL-cholesterol (n=67) or triglycerides (n=126). For analyses of glucose, participants who self-reported having diabetes or had fasting glucose levels >126 mg/dl at baseline (n=23) or follow-up (n=169) were excluded. Participants who self-reported taking antihypertensive (n=27) or cholesterol lowering (n=2) medications at baseline were excluded when the outcome of interest was blood pressure or plasma lipids, respectively. We also excluded participants who had extreme values for diastolic blood pressure (n=3), total cholesterol (n=5) and LDL-cholesterol (n=1). The distribution of changes in triglyceride levels was not normal, and we were unable to achieve normality through transformations. We did achieve an approximately normal distribution by excluding participants with changes in triglycerides that were greater than 3 s.d.’s (225 mg/dl) from the mean change (n=54).
Statistical analysis
We found statistical significant interactions (P<0.05) between ethnicity and weight change, but not between gender and weight change; therefore, all of the analyses were run separately for whites and African Americans with the gender groups combined. The objective of this study was to compare changes in risk factors between normal weight and overweight adults independent of their weight change group; therefore, separate multivariable linear regression models were run for weight maintainers and weight gainers. Baseline and follow-up models were adjusted for age and gender. The 15-year change models were adjusted for age, gender, education, baseline risk factor level, smoking status, alcoholic beverage consumption status, physical activity, weight fluctuation, elapsed time between examinations and field center. When examining weight gain, the blood pressure and lipid models were also adjusted for antihypertensive and lipid-lowering medications at follow-up, respectively. Owing to the small number of white and African-American weight maintainers on antihypertensive (5 and 16) and lipid-lowering medications (7 and 4) at follow-up, we did not adjust those models for medication usage. Data were analyzed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
The demographic characteristics of normal weight and overweight maintainers by ethnicity are shown in Table 1. The mean baseline age was similar among whites but slightly higher among normal weight African-American weight maintainers compared to overweight weight maintainers. Among weight maintainers, a larger distribution of overweight white adults was male, whereas the opposite pattern was seen among African Americans. The mean 15-year weight change was higher among white normal weight maintainers (1.9 lbs) compared to white overweight maintainers (0.2 lbs), but was fairly consistent among African Americans (0.8–1.0 lbs) across baseline weight status groups. Normal weight maintainers had less weight fluctuation over 15 years compared to overweight weight maintainers of the same ethnicity. The distribution of education, smoking status, alcoholic beverage consumption status and physical activity levels were similar in the two weight status groups for whites and African Americans.
Table 1.
Characteristics of weight maintainersa who were normal or overweightb at baseline by ethnicity, the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1995–2001
| Whites
|
African Americans
|
|||
|---|---|---|---|---|
| Normal weight (n =266) | Overweight (n =62) | Normal weight (n =107) | Overweight (n =53) | |
| Age at baseline (years, mean (s.d.)) | 25.8 (3.2) | 25.9 (3.0) | 24.5 (3.8) | 26.2 (3.3)* |
| Male (%) | 33.5 | 53.2* | 65.4 | 41.5* |
| Body mass index (BMI) at baseline (kg/m2, mean (s.d.)) | 21.7 (1.7) | 27.7 (3.2)* | 21.9 (1.7) | 31.1 (6.7)* |
| 15-year weight change (lbs, mean (s.d.)) | 1.9 (4.0) | 0.2 (4.1)* | 1.0 (4.3) | 0.8 (4.3) |
| Root mean square error of weight (RMSE, mean (s.d.)) | 4.1 (2.5) | 7.6 (5.4)* | 5.2 (3.5) | 9.9 (5.1)* |
| Education level at follow-up (%) | ||||
| High school education or less | 13.2 | 21.0 | 43.9 | 37.7 |
| Associate degree or some college | 15.4 | 25.8 | 35.6 | 43.4 |
| Bachelors degree | 38.4 | 21.0 | 14.0 | 15.1 |
| Advanced degree | 33.1 | 32.3 | 7.5 | 3.8 |
| Cigarette smoking status at follow-up (%) | ||||
| Non-smoker | 55.6 | 53.2 | 37.4 | 41.5 |
| Former | 25.9 | 21.0 | 14.0 | 18.9 |
| Current | 18.4 | 25.8 | 48.6 | 39.6 |
| Alcoholic beverage consumption at follow-up (%) | ||||
| Non-drinker or rare | 18.8 | 22.6 | 18.7 | 26.4 |
| Former | 15.4 | 17.7 | 17.8 | 13.2 |
| Light to moderate drinker | 47.0 | 38.7 | 35.5 | 39.6 |
| Heavy drinker | 18.8 | 21.0 | 28.0 | 20.8 |
| Physical activity at baseline and follow-up (%) | ||||
| Medium/high tertile at baseline and follow-up | 65.0 | 64.5 | 36.5 | 34.0 |
| Low tertile at baseline and medium/high tertile at follow-up | 9.4 | 9.7 | 15.9 | 20.8 |
| Medium/high tertile at baseline and low tertile at follow-up | 14.3 | 14.5 | 24.3 | 13.2 |
| Low tertilie at baseline and follow-up | 11.3 | 11.3 | 23.4 | 32.1 |
Participants were classified as a weight maintainer if the difference between their weight at follow-up and baseline was within 5 pounds or if their weight at baseline and follow-up was within 5 pounds of their average weight.
Normal weight (BMI: 18.5–24.9 kg/m2) and overweight (BMI: ≥25.0 kg/m2).
Statistically significant difference (P<0.05) between normal weight and overweight participants.
White and African-American weight gainers who were normal weight at baseline were slightly younger and had less weight fluctuation over 15 years compared to overweight participants of the same ethnicity (Table 2). Our definition of weight gain allowed for a larger weight change range compared to our weight maintenance definition; therefore, the mean 15-year weight change varied significantly between those who were normal weight versus overweight at baseline among whites (27.7 versus 37.6 lbs) and African Americans (37.0 versus 45.8 lbs). In addition, there was more weight fluctuation over 15 years in those overweight versus normal weight at baseline. Among weight gainers who were white and normal weight at baseline, they were more likely to be male and were less educated compared to overweight weight gainers, but there was no association with gender or education in African Americans. Compared to normal weight gainers, overweight weight gainers were less likely to be consumers of alcoholic beverages at the 15-year followup visit. The distribution of cigarette smoking and physical activity levels were similar between normal weight and overweight gainers for whites and African Americans.
Table 2.
Characteristics of weight gainersa who were normal or overweightb at baseline by ethnicity, the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1995–2001
| Whites
|
African Americans
|
|||
|---|---|---|---|---|
| Normal weight (n =970) | Overweight (n =446) | Normal weight (n =773) | Overweight (n =599) | |
| Age at baseline (years, mean (s.d.)) | 25.5 (3.4) | 26.0 (3.2)* | 24.0 (3.7) | 25.1 (3.8)* |
| Male (%) | 49.5 | 60.1* | 44.5 | 37.2* |
| Body mass index (BMI) at baseline (kg/m2, mean (s.d.)) | 22.1 (1.7) | 28.6 (3.6)* | 22.2 (1.7) | 30.1 (4.8)* |
| 15-year weight change (lbs, mean (s.d.)) | 27.7 (18.6) | 37.6 (26.0)* | 37.0 (20.7) | 45.8 (28.8)* |
| Root mean square error of weight (RMSE, mean (s.d.)) | 6.1 (3.9) | 9.9 (6.5)* | 7.0 (4.1) | 10.3 (6.4)* |
| Education level at follow-up (%) | ||||
| Less than high school education | 1.1 | 1.6 | 5.3 | 4.3 |
| High school education | 11.6 | 15.3 | 25.2 | 26.5 |
| Associate degree | 7.4 | 10.5 | 15.0 | 17.0 |
| Some college | 16.2 | 22.6 | 25.9 | 29.2 |
| Bachelors degree | 37.6 | 27.8 | 21.5 | 17.9 |
| Advanced degree | 26.1 | 22.2* | 7.2 | 5.0 |
| Cigarette smoking status at follow-up (%) | ||||
| Non-smoker | 54.6 | 54.7 | 56.1 | 57.1 |
| Former | 30.3 | 28.7 | 16.8 | 20.2 |
| Current | 15.0 | 16.6 | 27.0 | 22.7 |
| Alcoholic beverage consumption at follow-up (%) | ||||
| Non-drinker or rare | 20.3 | 25.6 | 35.8 | 42.7 |
| Former | 16.9 | 21.3 | 20.1 | 20.2 |
| Light to moderate drinker | 43.9 | 36.3 | 30.5 | 26.0 |
| Heavy drinker | 18.9 | 16.8* | 13.6 | 11.0* |
| Physical activity at baseline and follow-up (%) | ||||
| Medium/high tertile at baseline and follow-up | 50.6 | 47.1 | 38.4 | 31.7 |
| Low tertile at baseline and medium/high tertile at follow-up | 9.0 | 8.5 | 12.2 | 13.2 |
| Medium/high tertile at baseline and low tertile at follow-up | 24.0 | 24.7 | 22.8 | 21.4 |
| Low tertile at baseline and follow-up | 16.4 | 19.7 | 26.7 | 33.7 |
Participants were classified as a weight gainer if they did not meet the weight maintenance definition and the difference between their follow-up and baseline weight was greater than 5 pounds.
Normal weight (BMI: 18.5–24.9 kg/m2) and overweight (BMI: ≥25.0 kg/m2).
Statistically significant difference (P<0.05) between normal weight and overweight participants.
Weight maintainers
The age- and gender-adjusted mean levels of the risk factors at baseline and follow-up for weight maintainers who were normal or overweight at baseline by ethnicity are shown in Table 3. Among white and African-American weight maintainers, both baseline and follow-up mean risk factor levels were more favorable in normal weight compared to overweight participants, although differences were sometimes small and not statistically significant.
Table 3.
Age- and gender-adjusted baseline and follow-up means for cardiovascular disease risk factors among weight maintainersa who were normal or overweightb at baseline by ethnicity, the Coronary Artery Risk Development in Young Adults (CARDIA) Study, 1995–2001
| Whites
|
African Americans
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Normal weight
|
Overweight
|
Normal weight
|
Overweight
|
|||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Fasting glucose (mg/dl) | ||||||||
| Baseline | 81.1 | 80.2, 82.1 | 84.9* | 82.8, 87.1 | 79.4 | 77.3, 81.5 | 85.3* | 82.1, 88.5 |
| Follow-up | 80.3 | 79.4, 81.2 | 82.8* | 80.8, 84.9 | 78.2 | 76.2, 80.1 | 82.0* | 79.1, 84.9 |
| Systolic blood pressure (mm Hg) | ||||||||
| Baseline | 106.8 | 105.7, 107.9 | 110.2* | 107.9, 112.6 | 110.2 | 108.0, 112.3 | 115.9* | 112.7, 119.0 |
| Follow-up | 104.8 | 103.5, 106.2 | 107.8 | 105.0, 110.6 | 112.2 | 108.7, 115.6 | 122.6* | 117.6, 127.7 |
| Diastolic blood pressure (mm Hg) | ||||||||
| Baseline | 67.1 | 66.0, 68.1 | 68.9 | 66.7, 71.1 | 68.0 | 66.0, 70.1 | 71.5 | 68.5, 74.5 |
| Follow-up | 68.6 | 67.5, 69.7 | 70.3 | 67.9, 72.6 | 75.1 | 72.8, 77.5 | 78.7 | 75.3, 82.2 |
| Total cholesterol (mg/dl) | ||||||||
| Baseline | 173.8 | 170.1, 177.6 | 189.0* | 181.2, 196.9 | 178.2 | 170.9, 185.6 | 194.1* | 183.5, 204.7 |
| Follow-up | 176.0 | 172.1, 179.9 | 185.4* | 177.3, 193.5 | 171.4 | 164.5, 178.3 | 188.2* | 178.2, 198.1 |
| LDL-cholesterol (mg/dl) | ||||||||
| Baseline | 104.4 | 100.9, 107.9 | 119.5* | 112.0, 127.1 | 109.2 | 101.8, 116.6 | 121.4 | 110.9, 131.8 |
| Follow-up | 101.6 | 98.2, 105.0 | 114.7* | 107.4, 122.0 | 96.8 | 89.9, 103.7 | 111.3* | 101.6, 121.0 |
| HDL-cholesterol (mg/dl) | ||||||||
| Baseline | 55.8 | 54.4, 57.3 | 49.5* | 46.5, 52.6 | 59.0 | 56.3, 61.7 | 53.0* | 49.1, 56.9 |
| Follow-up | 59.1 | 57.4, 60.8 | 50.7* | 47.1, 54.2 | 60.6 | 57.6, 63.7 | 55.4 | 51.0, 59.9 |
| Triglycerides (mg/dl) | ||||||||
| Baseline | 65.3 | 60.7, 69.9 | 96.0* | 86.2, 105.8 | 60.5 | 51.6, 69.4 | 86.6* | 74.0, 99.1 |
| Follow-up | 71.5 | 66.5, 76.5 | 104.8* | 94.2, 115.3 | 67.8 | 56.3, 79.2 | 96.8* | 80.6, 113.0 |
BMI =body mass index; CI =confidence interval; LDL =low-density lipoprotein; HDL =high-density lipoprotein.
Participants were classified as a weight maintainer if the difference between their weight at follow-up and baseline was within 5 pounds or if their weight at baseline and follow-up was within 5 pounds of their average weight.
Normal weight (BMI: 18.5–24.9 kg/m2) and overweight (BMI: ≥25.0 kg/m2).
Significant difference (P<0.05) between normal and overweight participants.
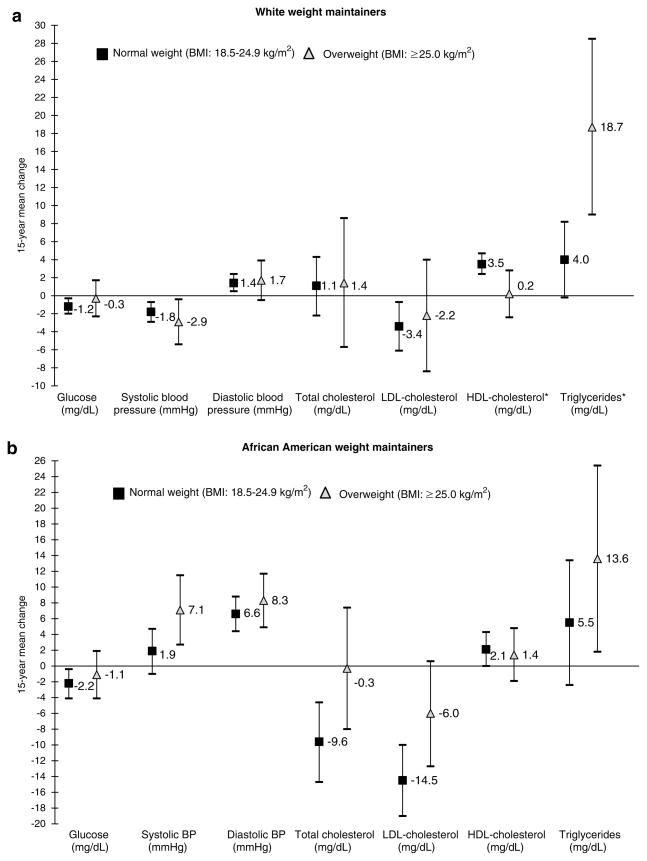
When comparing the fully adjusted 15-year mean change in risk factors among white (Figure 1a) and African-American (Figure 1b) weight gainers, we found that, regardless of baseline weight status, weight maintenance was associated with either improvement or no significant change in glucose, total cholesterol, LDL-cholesterol, HDL-cholesterol, triglycerides (normal weight only), systolic blood pressure (except for overweight African Americans) and diastolic blood pressure (overweight whites only). Among weight maintainers in both ethnic groups, there were no significant differences between normal compared to overweight participants in the direction and magnitude of the 15-year changes in any of the outcomes with two exceptions. Normal weight white maintainers had significantly more favorable changes in HDL-cholesterol (3.3 mg/dl, 95% confidence interval (CI): 0.4, 6.3) and less adverse changes in triglycerides (−14.7 mg/dl, 95% CI: −25.8, −3.7) than overweight white maintainers, respectively. After stratifying the models by gender (data not shown), we did find significantly less adverse change among normal weight maintainers in glucose and LDL-cholesterol (African-American women only), HDL-cholesterol (white men and African-American women) and triglycerides (white women).
Figure 1.
The 15-year mean changes and 95% confidence intervals for cardiovascular disease risk factors among white (a) and African-American (b) weight maintainers who were normal weight or overweight at baseline, the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1995–2001. All models were adjusted for gender, age, education level, baseline risk factor, smoking status, physical activity, alcoholic beverage consumption status, field center, elapsed time between visits and weight fluctuation. *Significant difference (P<0.05) between normal weight maintainers and overweight maintainers.
Weight gainers
The age- and gender-adjusted mean levels of the risk factors at baseline and follow-up for weight gainers who were normal weight or overweight at baseline by ethnicity are shown in Table 4. Among white and African-American weight gainers at baseline, mean risk factor levels were more favorable among young adult who were normal weight at baseline compared to overweight. After 15-years of follow-up, normal weight white and African Americans who gained weight still had significantly lower glucose, systolic and diastolic blood pressure, LDL-cholesterol (whites only), and triglycerides and higher HDL-cholesterol compared to overweight adults who gained weight. There was no statistically significant difference in total cholesterol at follow-up between normal weight and overweight adults who gained weight.
Table 4.
Age- and gender-adjusted baseline and follow-up means for cardiovascular disease risk factors among weight gainersa who were normal or overweightb at baseline by ethnicity, the Coronary Artery Risk Development in Young Adults (CARDIA) Study, 1995–2001
| Whites
|
African Americans
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Normal weight
|
Overweight
|
Normal weight
|
Overweight
|
|||||
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| Fasting glucose (mg/dl) | ||||||||
| Baseline | 81.9 | 81.4, 82.4 | 84.1* | 83.4, 84.9 | 79.4 | 78.8, 79.9 | 82.1* | 81.4, 82.8 |
| Follow-up | 84.0 | 83.5, 84.6 | 88.2* | 87.3, 89.1 | 83.3 | 82.6, 84.0 | 86.2* | 85.4, 87.0 |
| Systolic blood pressure (mm Hg) | ||||||||
| Baseline | 108.9 | 108.3, 109.5 | 112.6* | 111.7, 113.5 | 109.9 | 109.3, 110.6 | 113.1* | 112.3, 113.9 |
| Follow-up | 109.4 | 108.6, 110.1 | 115.7* | 114.6, 116.9 | 115.7 | 114.6, 116.8 | 119.9* | 118.6, 121.2 |
| Diastolic blood pressure (mm Hg) | ||||||||
| Baseline | 68.1 | 67.6, 68.6 | 70.2* | 69.4, 71.1 | 67.9 | 67.2, 68.5 | 69.8* | 69.0, 70.6 |
| Follow-up | 72.2 | 71.6, 72.8 | 76.5* | 75.6, 77.4 | 75.9 | 75.1, 76.8 | 78.7* | 77.7, 79.7 |
| Total cholesterol (mg/dl) | ||||||||
| Baseline | 173.7 | 171.7, 175.7 | 182.3* | 179.3, 185.3 | 175.5 | 173.2, 177.8 | 181.7* | 179.1, 184.3 |
| Follow-up | 187.8 | 185.6, 190.0 | 191.5 | 188.2, 194.7 | 183.3 | 180.8, 185.8 | 183.5 | 180.7, 186.3 |
| LDL-cholesterol (mg/dl) | ||||||||
| Baseline | 107.2 | 105.2, 109.1 | 115.6* | 112.7, 118.5 | 106.7 | 104.4, 109.0 | 116.4* | 113.8, 119.0 |
| Follow-up | 116.0 | 114.0, 118.0 | 120.5* | 117.5, 123.5 | 113.2 | 110.9, 115.6 | 115.5 | 112.8, 118.2 |
| HDL-cholesterol (mg/dl) | ||||||||
| Baseline | 52.9 | 52.2, 53.6 | 46.6* | 45.5, 47.7 | 57.1 | 56.2, 58.0 | 51.1* | 50.0, 52.1 |
| Follow-up | 49.3 | 48.5, 50.0 | 42.8* | 41.6, 43.9 | 52.0 | 51.1, 52.9 | 47.0* | 46.0, 48.0 |
| Triglycerides (mg/dl) | ||||||||
| Baseline | 69.8 | 66.3, 73.4 | 98.5* | 93.2, 103.8 | 59.9 | 57.5, 62.3 | 70.0* | 67.3, 72.7 |
| Follow-up | 105.2 | 100.8, 109.7 | 133.1* | 126.5, 139.7 | 84.1 | 80.6, 87.7 | 100.6* | 96.6, 104.6 |
BMI =body mass index; CI =confidence interval; LDL =low-density lipoprotein; HDL =high-density lipoprotein.
Participants were classified as a weight gainer if they did not meet the weight maintenance definition and the difference between their follow-up and baseline weight was greater than 5 pounds.
Normal weight (BMI: 18.5–24.9 kg/m2) and overweight (BMI: ≥25.0 kg/m2).
Significant difference (P<0.05) between normal and overweight participants.
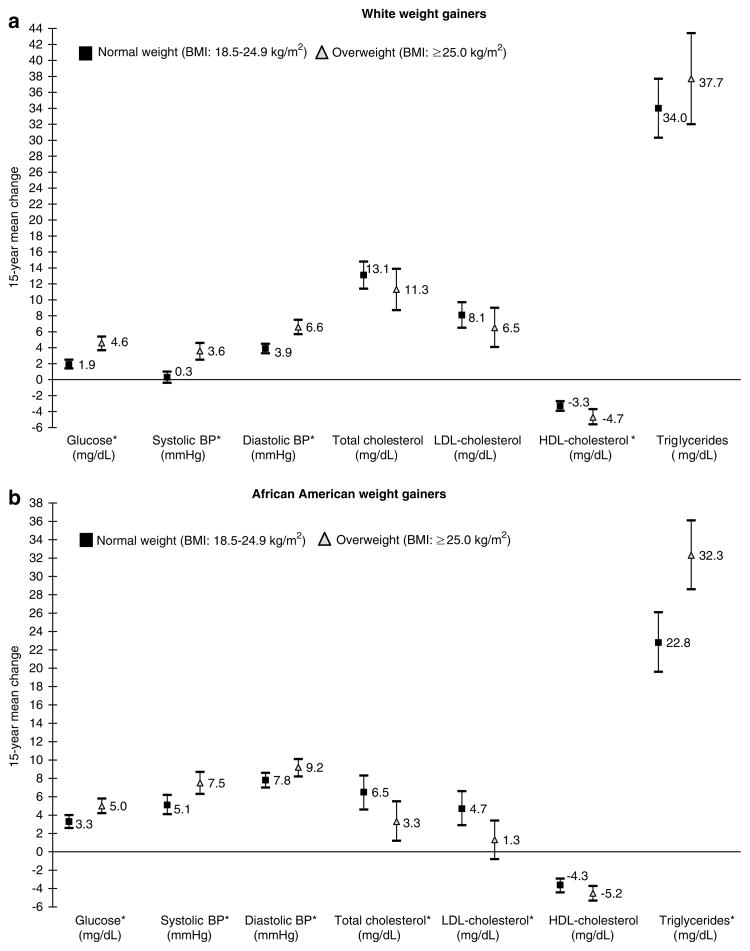
As expected, weight gain over 15 years was associated with unfavorable changes in risk factors. When comparing the differences in the 15-year changes in CVD risk factors, we found, among whites (Figure 2a), significantly larger adverse changes in overweight compared to normal weight participants for glucose (−2.6 mg/dl, 95% CI: −3.7, −1.6), systolic blood pressure (−3.3mm Hg, 95% CI: −4.6, −1.9), diastolic blood pressure (−2.7, 95% CI: −3.8, −1.6) and HDL-cholesterol (1.6, 95% CI: 0.2, 2.5). Changes in total cholesterol, LDL-cholesterol or triglycerides by baseline weight status among whites. However, a different pattern was observed in African Americans (Figure 2a). Overweight adults had significantly more adverse changes in glucose (−1.7 mg/dl, 95% CI: −2.8, −0.6), systolic blood pressure (−2.3mm Hg, 95% CI: −4.0, −0.7), diastolic blood pressure (−1.4mm Hg, 95% CI: −2.7, −0.1) and triglycerides (−9.5 mg/dl, 95% CI: −14.7, −4.3) compared to normal weight gainers. In contrast, total and LDL-cholesterol changes were less adverse in overweight compared to normal weight African Americans, 3.1 mg/dl (95% CI: 0.2, 6.1) and 3.4 mg/dl (0.6, 6.3), respectively. The 15-year changes in HDL-cholesterol were less adverse among normal weight adults compared to overweight adults, although not statistically significant among American Americans.
Figure 2.
The 15-year mean changes and 95% confidence intervals for cardiovascular disease risk factors among white (a) and African-American (part b) weight gainers who were normal weight or overweight at, the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1995–2001. All models were adjusted for gender, age, education level, baseline risk factor, smoking status, physical activity, alcoholic beverage consumption status, field center, elapsed time between visits and weight fluctuation. Blood pressure and lipid models were adjusted for antihypertensive and lipid-lowering medications, respectively. *Significant difference (P<0.05) between normal weight gainers and overweight gainers.
After stratifying the models by gender (data not shown), we found significant differences among white women and men for glucose, systolic and diastolic blood pressure, HDL-cholesterol (women only) and triglycerides. In addition, 15-year changes in LDL-cholesterol were significantly less adverse among overweight white men compared to normal weight white men. Among African Americans, the significant differences between normal and overweight weight gainers were found only in women for glucose, systolic and diastolic blood pressure, HDL-cholesterol and triglycerides and total and LDL-cholesterol in men.
Discussion
There is currently no standard definition for weight maintenance. Our review of nine studies6,16–23 that examined changes in risk factors for diabetes and CVD by weight change groups (including a weight maintenance group) showed the use of a variety of definitions (a change less than ±2 kg,18,22 −1.0 to +3.0 kg,21 ±4.5 kg,23 ±5 lbs6,17 <10 lbs,20 ±2.4%,16 ±10%,19). We chose to use of a relatively narrow or strict definition for weight maintenance. We defined weight maintenance using the change in weight between baseline and the 15-year follow-up; however, we also took some advantage of the repeated weight measures available in the CARDIA study by using the average weight for each participant in all visits as part of a second criterion for weight maintenance. Approximately 56% of the participants classified as weight maintainers here met both definitions.
To our knowledge, this is first study to examine whether the presumed benefits of weight maintenance for CVD risk were similar regardless of baseline weight status and to address this question in both African-American and white men and women. The results indicate that 15-year changes in glucose, blood pressure and lipid levels were comparable among weight maintainers regardless of whether they were normal weight or overweight at baseline, except for triglycerides among whites. Mean risk factor levels among overweight adults, which were more adverse at baseline compared to normal weight adults, therefore remained more adverse even without further weight gain, consistent with other published studies,2,24–28 but did not worsen disproportionately. A pattern of less adverse changes among those who were normal weight at baseline was suggested in gender stratified analyses, although the observed statistically significant differences between normal weight and overweight maintainers were not for the same risk factors in men and women.
With respect to weight gain, we had hypothesized more adverse changes in risk factors among adults overweight at baseline, as compared to adults’ normal weight at baseline. This was true for glucose, systolic and diastolic blood pressure, HDL-cholesterol (whites only) and triglycerides (African Americans only). However, contrary to our expectations, changes in total cholesterol and LDL-cholesterol were less adverse in those overweight at baseline – opposite to our hypothesized results.
A possible explanation for the unexpected findings (less adverse changes associated with weight gain among adults overweight at baseline) is that the contributions of energy intake versus energy expenditure to weight change may vary by baseline weight status. For example, adults overweight at baseline could have been more likely than adults’ normal weight at baseline to gain weight because of changes in caloric intake rather than caloric expenditure. Sternfeld et al.20 compared changes in physical fitness and lipid profile in the CARDIA study using 7 years of follow-up. Among weight-stable (±10 lbs) adults, total and LDL-cholesterol decreased while HDL-cholesterol increased and triglycerides remained the same, regardless of fitness change category. They found that total cholesterol, LDL-cholesterol and triglycerides increased and HDL-cholesterol decreased among adults who gained weight. They did not examine the role of baseline weight status on these relationships. Davison and Birch29 found that lean and weight-stable (±5%) women consumed fewer calories and were more physically active than women who were overweight at baseline and/or did not maintain their body weight. Dietary composition could also differ by baseline weight status in ways that may impact lipid levels. Lean and weight stable men had diets lower in fat and consumed more fruits and vegetables compared to men who were overweight and/or gained weight.29 In addition, higher body weights tend to be associated with lower fruit and vegetable consumption among adults.30
Observational studies have shown direct associations between weight change during young adulthood and coronary heart disease (CHD) later in life. In the Framingham Heart Study, weight gain was associated with increased risk of CVD in men and women.31 The authors concluded that the ‘increased risk could not be attributed either to the initial weight or the levels of the risk factors that may have resulted from weight gain’. Willett et al. examined the association between weight gain from 18 years of age until 30–55 years of age and subsequent incidence of CHD events (non-fatal myocardial infarction or fatal CHD).28 They found that women who gained weight gain were at greater risk of CHD compared to weight-stable (±4.9 kg) women within each baseline BMI category.28 Similar results were found using data from the Health Professionals Study (weight maintenance defined as ±2.0 kg)32 and a multifactor primary prevention trial in Goteborg, Sweden (weight maintenance defined as ±4%).33 However, none of these studies examined the effect of weight status after stratifying by weight change category.
Although weight loss has been effective in short-term clinical trials34–36 examining CVD risk factors and diabetes prevention, long-term weight loss has proven to be extremely difficult to maintain.2,3 This study suggests that weight maintenance may prevent or attenuate many of the unfavorable changes often associated with aging, that is, aging accompanied by weight gain. Further, the benefits of weight maintenance on changes in risk factors appear to apply to both normal and overweight adults. This does not mean that risk factor levels are equivalent in the adults’ normal weight and overweight at baseline, but that changes in risk factors can be similar if weight is maintained. Despite similar changes by baseline weight status, overweight adults remain at increased risk for diabetes and CVD based on the seven risk factors we examined.
We are aware that the results from this study could have varied if we used a different definition of weight maintenance. 37 Subsequent analysis using a cut-point of ±3.0% gave similar results. Regardless of whether we used more liberal or conservative definitions for weight maintenance and weight gain, the differences between normal weight and overweight subjects tended to be in the same directions but with some slight variations in magnitudes. In general, the differences in significance that we observed were owing to how the different sample sizes impacted our power to detect significant differences between normal and overweight subjects.
The alarming obesity trends occurring in the US38 are apparent among the CARDIA participants who experienced large mean weight changes over 15 years of follow-up. The average, 15-year weight change exceeded the American Institute for Cancer Research (AICR) recommended weight gain for adults of less than 5 kg (11 lbs).39 Our findings showed stability and even improvement in several CVD risk factors among normal and overweight white and African Americans who maintained their weight over 15 years. Changes associated with weight maintenance were always les adverse than changes associated with weight gain. Therefore, weight maintenance has important public health implications in both normal weight and overweight adults. Weight maintenance may provide an important first step in limiting the health consequences of the obesity epidemic in young adults.
References
- 1.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 2.National Institutes of Health. National Heart Lung and Blood Institute: clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. The Evidence Reports. Obes Res. 1998;6:53S. [PubMed] [Google Scholar]
- 3.Miller MC. How effective are traditional dietary and exercise interventions for weight loss? Med Sci Sports Exerc. 1999;31:1129–1131. doi: 10.1097/00005768-199908000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Williamson DF, Kahn HS, Remington PL, Anda RF. The 10-year incidence of overweight and major weight gain in US adults. Arch Intern Med. 1990;150:655–672. [PubMed] [Google Scholar]
- 5.Rissanen A, Heliovaara M, Aromaa A. Overweight and anthropometric changes in adulthood: a prospective study of 17 000 Finns. Int J Obes Relat Metab Disord. 1988;12:391–401. [PubMed] [Google Scholar]
- 6.St Jeor ST, Brunner RL, Harrington ME, Scott BJ, Daughtery SA, Cutter GR, et al. A classification system to evaluate weight maintainers, gainers, and losers. J Am Diet Assoc. 1997;97:481–488. doi: 10.1016/S0002-8223(97)00126-0. [DOI] [PubMed] [Google Scholar]
- 7.Norman JE, Bild D, Lewis CE, Liu K, Smith West D. The impact of weight change on cardiovascular diesase risk factors in young black and white adults: the CARDIA study. Int J Obes Relat Metab Disord. 2003;27:369–376. doi: 10.1038/sj.ijo.0802243. [DOI] [PubMed] [Google Scholar]
- 8.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 9.Warnick GR. Enzymatic methods for quantification of lipoprotein lipids. Methods Enzymol. 1986;129:101–123. doi: 10.1016/0076-6879(86)29064-3. [DOI] [PubMed] [Google Scholar]
- 10.Warnick GR, Benderson J, Albers JJ. Dextran sulfate-Mg2+ precipitation procedure for quantification of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–1388. [PubMed] [Google Scholar]
- 11.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low density lipoprotien cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 12.Bild DE, Jacobs DR, Liu K, Williams OD, Hilner JE, Perkins LL, et al. Seven-year trends in plasma low-density-lipoprotein-cholesterol in young adults: the CARDIA study. Ann Epidemiol. 1996;6:235–245. doi: 10.1016/1047-2797(96)00005-1. [DOI] [PubMed] [Google Scholar]
- 13.MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke and coronary heart disease, Part 1. Prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 14.Pereira MA, FitzGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, et al. A collection of physical activity questionnaires for health-related research. Med Sci Sports Exerc. 1997;29:S15–S18. [PubMed] [Google Scholar]
- 15.Jacobs DR, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of short physical activity history: CARDIA and the Minnesota Heart Health Program. J Cardiopulm Rehab. 1989;9:448–459. doi: 10.1097/00008483-198911000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borkan GA, Sparrow D, Wisniewski C, Vokonas PS. Body weight and coronary disease risk: patterns of risk factor change associated with long-term weight change. Am J Epidemiol. 1986;124:410–419. doi: 10.1093/oxfordjournals.aje.a114411. [DOI] [PubMed] [Google Scholar]
- 17.St Jeor ST, Brunner RL, Harrington ME, Scott BJ, Cutter GR, Brownell KD, et al. Who are the weight maintainers? Obes Res. 1995;3 (Suppl 2):249s–259s. doi: 10.1002/j.1550-8528.1995.tb00471.x. [DOI] [PubMed] [Google Scholar]
- 18.Sedgwick AW, Thomas DW, Davies M, Baghurst K. Relationships between weight change and blood lipids in men and women: ‘The Adelaide 1000’. Int J Obes Relat Metab Disord. 1990;14:439–450. [PubMed] [Google Scholar]
- 19.Harris TB, Savage PJ, Tell GS, Haan M, Kumanyika S, Lynch JC. Carrying the burden of cardiovascular risk in old age: associations of weight and weight change with prevalent cardiovascular disease, risk factors, and health status in the Cardiovascular Health Study. Am J Clin Nutr. 1997;66:837–844. doi: 10.1093/ajcn/66.4.837. [DOI] [PubMed] [Google Scholar]
- 20.Sternfeld B, Sidney S, Jacobs DR, Sadler MC, Haskell WL, Schreiner PJ. Seven-year changes in physical fitness, physical activity, and lipid profile in the CARDIA study. Ann Epidemiol. 1999;9:25–33. doi: 10.1016/s1047-2797(98)00030-1. [DOI] [PubMed] [Google Scholar]
- 21.Pihl E, Jurimae T. Relationships between body weight change and cardiovascular disease risk factors in male former athletes. Int J Obes Relat Metab Disord. 2001;25:1057–1062. doi: 10.1038/sj.ijo.0801642. [DOI] [PubMed] [Google Scholar]
- 22.Czernichow S, Mennen L, Bertrais S, Preziosi P, Hercberg S, Oppert J-M. Relationships between changes in weight and changes in cardiovascular risk factors in middle-aged French subjects: effect of dieting. Int J Obes Relat Metab Disord. 2002;26:1138–1143. doi: 10.1038/sj.ijo.0802059. [DOI] [PubMed] [Google Scholar]
- 23.Wing RR, Jeffrey RW, Hellerstedt WL. A prospective study of effects of weight cycling on cardiovascular risk factors. Arch Intern Med. 1995;155:1416–1422. [PubMed] [Google Scholar]
- 24.Berns MAM, De Vries JHM, Katan MB. Increase in body fatness as a major determinant of changes in serum total cholesterol and high density lipoprotein cholesterol in young men over 10-year period. Am J Epidemiol. 1989;130:1109–1122. doi: 10.1093/oxfordjournals.aje.a115438. [DOI] [PubMed] [Google Scholar]
- 25.Stamler R, Stamler J, Riedlinger WF, Algera G, Roberts RH. Weight and blood pressure. JAMA. 1978;240:1607–1610. doi: 10.1001/jama.240.15.1607. [DOI] [PubMed] [Google Scholar]
- 26.Colditz GA, Willett WC, Stampfer MJ, Manson JE, Hennekens CH, Arky RA, et al. Weight as a risk factor for clinical diabetes in women. Am J Epidemiol. 1990;132:501–513. doi: 10.1093/oxfordjournals.aje.a115686. [DOI] [PubMed] [Google Scholar]
- 27.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 28.Willett WC, Manson JE, Stampfer MJ, Colditz GA, Rosner B, Speizer FE, et al. Weight, weight change, and coronary heart disease in women. Risk within the ‘normal’ range. JAMA. 1995;273:461–465. doi: 10.1001/jama.1995.03520300035033. [DOI] [PubMed] [Google Scholar]
- 29.Davison KK, Birch LL. Lean and weight stable: behavioral predictors and psychological correlates. Obes Res. 2004;12:1085–1093. doi: 10.1038/oby.2004.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tohill BC, Seymour J, Serdula M, Kettel-Khan L, Rolls BJ. What epidemiologic studies tell us about the relationship between fruit and vegetable consumption and body weight. Nutr Rev. 2004;62:365–374. doi: 10.1111/j.1753-4887.2004.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 31.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 32.Rimm Eric B. Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men. Am J Epidemiol. 1995;141:1117–1127. doi: 10.1093/oxfordjournals.aje.a117385. [DOI] [PubMed] [Google Scholar]
- 33.Rosengren A, Wedel H, Wilhelmsen L. Body weight and weight gain during adult life in men in relation to coronary heart disease and mortality: a prospective population study. Eur Heart J. 1999;20:269–277. [PubMed] [Google Scholar]
- 34.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134:1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 36.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 37.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes Relat Metab Disord. 2005;30:391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 38.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 39.World Cancer Research Fund Panel. Food, Nutrition and the Prevention of Cancer: A Global Perspective. Research AifC; Washington, DC: 1997. [Google Scholar]