Abstract
Background
The water method has promising features for colonoscopy but the learning curve to master the technique is unknown.
Aims
To describe the learning phase, and pitfalls of the water method and its impact on procedural outcomes by an experienced colonoscopist.
Design
Review of prospectively collected data in a performance improvement project
Setting
endoscopy Unit at a VA medical center
Patients
200 consecutive veterans undergoing colonoscopy
Methods
An experienced colonoscopist examined 4 consecutive groups of 25 patients each using the water method to define the learning curve. Outcomes were compared to a historical cohort (n=100) examined by the same colonoscopist using usual air insufflation.
Main outcome measures
Intent-to-treat (ITT) cecal intubation rate.
Results
ITT cecal intubation rate increased from 76% (first) to 96% (fourth quartile). Cecal intubation time in the first 2 quartiles was significantly longer (8.9±1.0 and 8.2±0.8 min, respectively) than that in the historical cohort (5.8±0.4 min) but decreased and became comparable to control values in the next 2 quartiles (7.2±0.9 and 6.6±0.6 min, respectively). Overall adenoma detection rate as a group (55%), compared favorably to the historical cohort (46%).
Conclusions
The water method is relatively easy to learn for an experienced colonoscopist. Mastery of the method resulted in cecal intubation rate and overall adenoma detection rate meeting quality performance standards.
Key words: water method, learning curve, adenoma detection rate, colonoscopy
Introduction
The water method was developed initially to facilitate completion of unsedated colonoscopy when patients accepted the option of sedation on demand1 and to demonstrate feasibility of cecal intubation using water infusion in lieu of air insufflation in patients sedated with only one half the usual dose of medication2 by a limited number of colonoscopists (n=2). In unsedated patients, the water method succeeded in minimizing discomfort during3 and after3,4 colonoscopy, and in increasing cecal intubation rate and patient willingness to repeat unsedated colonoscopy3,4 by one colonoscopist compelled to develop a less painful approach for scheduled, unsedated colonoscopy to provide access to colonoscopy in a cultural setting where sedated colonoscopy is the norm but institutional nursing shortage (in surmountable direct cost) limited access. The most recent documentation of additional benefit was in the reduction of sedation-imposed recovery time burdens in patients accepting the option of sedation on demand.5 Colonoscopists accustomed to using air insufflation and sedation, however, would find the water method1–7 cumbersome non-conventional not wort the time to learn, and unnecessary in the sedated patients, an opinion held by the lead authorof this study. Nonetheless, the trend towards a higher adenoma detection rate (ADR) repeatedly in small number of unsedated patients3,4 provided the motivation to assess the hypothesis, the investigator even if it is single colonoscopist needs to show proficiency to establish credibility of the observations. The aim of this report is to describe one experienced colonoscopist's learning process of the water method used as the sole insertion technique in sedated patients, and using the intent-to-treat (ITT) cecal intubation rate as the primary outcome.
Methods
Since the water method has beneficial impacts1–10 a performance improvement project evaluating its utility was carried out at the the Carl T. Hayden VA Medical Center in Phoenix, Arizona. Data were collected prospectively to monitor performance. Approval was granted by the local IRB to report the observations. Informed consent waiver was granted since data were de-identified. The early phase of this learning curve study has been reported at the Colorectal Cancer Screening Symposium at the Sacramento VAMC on March 20, 2010 and published in the symposium proceedings.11 The current report provides additional instructive data of the later phase to offer a complete description of the learning curve.
An experienced colonoscopist (FCR) examined 100 consecutive patients (6/2009–8/2009) using the water method based on literature descriptions.1–3 Fentanyl (75 µg) and Midazolam (3 mg) were used as pre-medications. All patients received 4 L polyethylene glycol solution and 20 mg bisacodyl the day before of the procedure. If patients had diabetes, chronic constipation or were using chronic narcotics they were given an extra 2 L polyethylene glycol the day before. Monitoring of blood pressure, pulse, electrocardiogram and pulse oximetry was performed. Colonoscopy began with the patient in the left lateral decubitus position. Additional sedation administered intra-procedure was patient-driven, depending on the level of discomfort reported.
Air method: Air insufflation, shortening maneuvers, abdominal compression and change of patient position were used. Contact with residual feces which would smear the lens and impair the view was avoided. Cecal intubation was defined as passage of the colonoscope tip to a point proximal to the ileocecal valve so that the entire cecal caput, including the medial wall of the cecum between the ileocecal valve and appendix orifice were visible.
Water method: The water method can be summarized as water infusion in lieu of air insufflation, combined with suction removal of residual air to reduce angulations at all flexures to minimize discomfort, and removal of residual feces that obscure luminal view by water exchange.1–3,10,11 The air pump was turned off when the colonoscope was inserted into the rectum. Water (room temperature) was infused by a pedal pump via a tubing connected to the base of the colonoscope. The water was used primarily to find and “open” the lumen so the colonoscope could be safely advanced. In addition, removal of angulations by suction of residual air collapsed the colon around the colonoscope, increasing the chance that the tip would point in the direction of the “future” lumen. The tip of the colonoscope was oriented towards and abutted the “slit-like lumen” ahead. The infused water opened the lumen if the orientation was correct. Incorrect orientation did not lead to opening of the lumen ahead, and water infusion was stopped. The tip of the colonoscope was pulled away from the mucosa and redirected. The colonoscope was advanced by a series of to and fro, back and forth, or repeated insertion and withdrawal motions of the shaft of the colonoscope and torquing in the direction of the expected lumen, and intermittent water infusion. Since air was not used to find the lumen, suspended residual feces or turbid residual fluid obscuring the view had to be suctioned and replaced by clean water until the colonic lumen was visualized again. To minimize suction of the mucosa into the endoscope channel the water infusion was started first followed by application of suction. The volume of water needed to clear the view was kept to a minimum, but not restricted. The turbulence set up by the simultaneous infusion and suction in the collapsed lumen dislodged the residual feces from the surrounding mucosa in close proximity to the tip of the colonoscope. This maneuver made removal of the residual feces “easier” than washing with a single water jet in a dilated air filled colon. Most of the infused water was aspirated into the suction bottle instead of remaining in the colon. Over-distension was obviated. If advancement failed, the assistant provided abdominal compression followed by the patient changing position if necessary. If the advancement was uninterrupted, no abdominal pressure or change in patient position was used. When the cecum was thought to be reached, the air feature was turned on to confirm the location. If the cecum had not been reached, failed intubation was recorded based on intent-to-treat (ITT) but colonoscopy was continued. Cecal intubation was defined as described above.
Both methods during withdrawal: Air insufflation was used to distend the colon for inspection, biopsy and polypectomy. Washing of the stool covered mucosa by irrigation and inspection behind folds were performed systematically as needed. Residual water and liquid stools were removed from the colon as inspection for polyps and their removal was systematically performed. Likewise, residual air in the colon was removed by suction, after leaving each segment.
ADR, intraprocedural sedation requirements, need for external pressure or change in patient's position, overall assessment of the quality of bowel preparation and tolerance, cecal intubation-, withdrawal- and total times were recorded. The data were divided into 4 quartiles to assess the progress achieved with experience and build the learning curve. A historical cohort (100 consecutive colonoscopies performed by FCR using air insufflation) immediately prior to the adoption of the water method was used for comparison.
Data analysis
Data are presented as mean ± SEM (standard error of mean). Continuous data were compared using the Student's t-test and proportional data were compared using the Fisher's exact test. A p value <0.05 was considered statistically significant.
Results
High-definition colonoscopes (CFH 180AL) were used in 85% and 35%, PCF Q180AL in 6% and 38% and CF Q180AL in 9% and 27% of study and control patients, respectively.
Table 1 shows the ITT cecal intubation rate increased from 76% to 96%; the cecal intubation time progressively decreased from 8.9±1.0 to 6.6±0.6 minutes becoming comparable to that of the historical cohort (5.8±0.4 min). The proportion of patients requiring external pressure decreased from 28% to 16%. The proportion of patients requiring change in their position to aid scope advancement dropped from 28% to 0%. Compared to the historical cohort with an ADR of 46%, the first quartile ADR was only 40%, numerically but not statistically lower. The ADR showed an increase from 40% in the first to 56% in the fourth quartile. The overall ADR in the water group (55%) was not statistically different from that of the historical cohort (46%). The reasons for “ITT failure” to reach the cecum using the water method only are depicted in Table 2. There were no complications. There were no significant differences in ADR between patients undergoing screening colonoscopy with (47.2%) and without (63.6%) high-definition scopes in the study group.
Table 1.
Learning curve - outcomes by quartiles
| Historical cohort (n=100) | 1st Quartile (n=25) | 2nd Quartile (n=25) | 3rd Quartile (n=25) | 4th Quartile (n=25) | |
| Age | 61 | 59 | 62 | 59 | 60 |
| Screening | 51/100 (51%) | 18/25 (72%) | 12/25 (48%) | 20/25 (80%) | 14/25 (56%) |
| ITT Cecal intubation | 98/100 (98%) | 19/25 (76%) | 21/25 (84%) | 21/25 (84%) | 24/25 (96%) |
| Final Cecal Intubation | 98/100 (98%) | 25/25 (100%) | 25/25 (100%) | 25/25 (100%) | 25/25 (100%) |
| Time to cecum | 5.8±0.4 | 8.9+0.98* | 8.2±0.8* | 7.2±0.9 | 6.6±0.6 |
| Time withdrawal | 12.9±0.5 | 11.9+0.9 | 13.5±0.9 | 15.8±1.4* | 14.2±1.3 |
| Total time | 18.9±0.7 | 20.8+1.1 | 21.7±1.4 | 23.1±1.4* | 20.8±1.5 |
| Fentanyl | 81.4±2.1 | 78.1+2.7 | 77.1±3.3 | 77.0±2.0 | 77.0±2.9 |
| Midazolam | 3.33±0.08 | 3.13+0.08 | 3.08±0.08 | 3.08±0.08 | 2.96±0.08* |
| External pressure | Not recorded | 7/25 (28%) | 4/25 (16%) | 2/25 (8%) | 4/25 (16%) |
| Change in position | 25/98 (25.5%) | 7/25 (28%) | 3/25 (12%) | 1/25 (4%)*,*** | 0/25 (0%)*,*** |
| ADR | 46/100 (46%)** | 10/25 (40%)** | 12/25 (48%) | 19/25 (76%) | 14/25 (56%) |
p<0.05, vs. historical cohort quartile;
p<0.05, vs. Third quartile;
p<0.05, vs. First quartile.
Table 2.
Reasons for “failed” ITT cecal intubation with the water method
| Case # | Reason for ITT “failure” | Location where air was switched on | Time at which air was switched on |
| # 6 | Preparation | Recto-sigmoid | Not recorded |
| # 7 | Prolonged/tortuosity | Not recorded | 10 min |
| # 11 | Misidentification cecum | Hepatic flexure | 12 min |
| # 15 | Prolonged | Hepatic flexure | 12 min |
| # 19 | Misidentification cecum | Hepatic flexure | 8 min |
| # 20 | Misidentification cecum | Transverse colon | 11 min |
| # 38 | Misidentification cecum | Hepatic flexure | 6 min |
| # 44 | Unable to get into ascending colon | Hepatic flexure | 18 min |
| # 48 | Long and tortuous | Splenic flexure | Not recorded |
| # 50 | Could not get into cecum | IC valve | Not recorded |
| # 59 | Misidentification cecum | Hepatic flexure | 4 min |
| # 66 | Misidentification cecum | Hepatic flexure | 7 min |
| # 70 | Misidentification cecum | Transverse colon | 4 min |
| # 76 | Prep/diverticulosis | Left colon | 14 min |
| # 99 | Misidentification cecum | Hepatic flexure | 10 min |
Discussion
Water-related techniques as adjuncts to air insufflation have been described12–16 and recently reviewed17. Water infusion produces local distension to facilitate passage through segments with significant diverticulosis.12 With the patient in the left lateral position, the water infused into the sigmoid colon opens a passage13 and the water weighs down the left colon straightening the sigmoid segment12–14. Suction of residual air in the colonic lumen minimizes angulations at the flexures.18,19 The absence of air insufflation avoids colon elongation which increases difficulty in reaching the cecum in unsedated patients.3 The removal of the residual air in the colonic lumen during insertion also optimizes the rinsing effect of the infused water which touches all of the mucosal surfaces. The turbulence set up by the simultaneous suction of dirty water and infusion of clean water facilitates suspension of the residual feces for removal by suction. These maneuvers also optimize the soaking effect of water on feces adherent to mucosal surfaces. Residual feces suspended in the luminal water are easily removed by suction. These simple maneuvers serendipitously provide colonoscopist-controlled salvage bowel cleansing in patients with suboptimal bowel preparation.3,4
Although there is truism in the approach to learning a “new method” with an experienced trainer in attendance, the results of this study support the hypothesis that an onsite “trainer” if the detailed description of the water method is followed with strict adherence to the water infusion in lieu of air insufflation. The progressive increase in ITT cecal intubation ultimately reaching the level expected of high quality performance indicates that the method as the sole modality to aid insertion of the colonoscope can be easily achieved. Importantly, water method ITT failure did not preclude cecal intubation when the colonoscopist reverted back to conventional air insufflation. During the learning process cecal intubation time was significantly longer initially but returned to the endoscopist's usual level attained during air colonoscopy. Mastery of the method was accompanied by progressively less need for the assistant to provide external pressure. A likely implication is that the suction removal of residual air in the colon minimized angulations at the flexures, thereby reducing the predisposition to loop formation. Fewer patients needed to change position and significantly lower doses of midazolam were required (detected during the fourth quartile) compared to the historical cohort. Unexpectedly, the third quartile was associated with significantly longer withdrawal and total procedure times than the historical cohort. This was likely as a result of the significantly greater number of patients with adenomas and thus reflecting the added time required for performing biopsy and polypectomy.
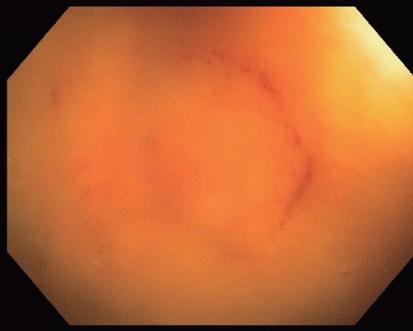
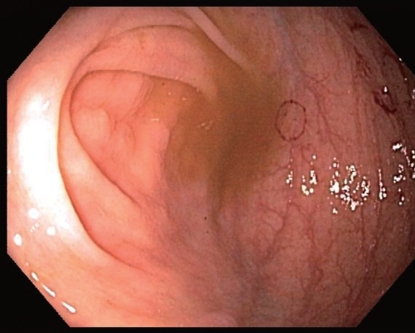
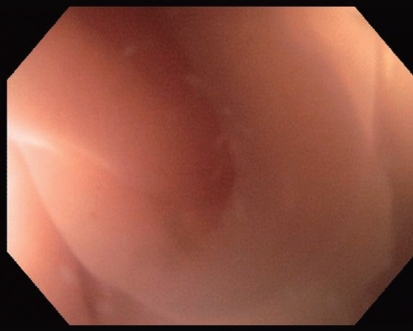
The most common reasons for initially failing to reach the cecum were misidentification of the cecum or premature use of air insufflation which by definition committed the initial outcome to ITT failure of cecal intubation. Visualization of the usual landmarks (appendix orifice, ileocecal valve and the “tripod” folds at the base of the cecum) was initially more difficult in the water filled cecum. The hepatic flexure was the most common site mistaken as the cecum. In retrospect, with a patient in the left lateral position, an air pocket after traversing a considerable length of water filled colon would indicate arrival at the hepatic flexure rather than the cecum. Over time and with experience gained, premature air insufflation was not a problem while monitoring the elapsed insertion time. We learned that the cecal wall was often highlighted by “suction marks” (Fig. 1 and 2) which could be used as another “landmark” signaling cecal intubation. This was used in those cases in which cecal intubation were suspected but the appendix opening was not readily obvious. The distance traveled in centimeters (about 90 cm) was also a good indicator of arrival to the cecum. A good estimation of the expected cecal intubation time at the beginning of the learning process is about 2–3 minutes longer than the expected average time used in air colonoscopy. With practice the appendix openning under water (Fig. 3) can be recognized to confirm cecal intubation.
Figure 1.
Endoscopic picture depicting a cecal suction mark under water
Figure 2.
Endoscopic pictures depicting a characteristic suction mark at the cecum
Figure 3.
Endoscopic picture depicting the appendix orifice under water
Akin to an earlier retrospective report8 and the pool data of two RCT9, the water method was associated with a higher ADR than the historical cohort. The reasons for the highest ADR in the third quartile (76%) are unknown but could be related to the clustering of patients and small sample size. The current study achieved an ADR comparable to those reported for high adenoma detectors.20,24 Our results differ from those of Radaelli et al.25 who reported a significantly lower ADR in the water group than the air group (25% vs. 40%). It is unclear what factors accounted for the difference. These investigators permitted the use of air insufflation at the beginning of colonoscopy and whenever difficulty was encountered during colonoscopy. The methodological difference could have contributed to the difference in ADR. We observed a comparable pattern in that the ADR in the first quartile was only 40%, numerically much lower than that of the historical cohort. It is conceivable that until the colonoscopist has mastered the water exchange technique, suspended feces incompletely removed can impair the view and prevent the detection of all of the lesions. These concerns that excessive residual feces could interfere with colonoscope insertion and detection of mucosal lesions were raised by at least two groups of investigators who evaluated water-related methods.14,26
The main limitations of our study are threefold. First, this is observational and non randomized. Second, only veteran patients were involved making the results not necessarily generalizable to the non veteran population. Third, involved only one experienced endoscopist. In summary, in sedated patients examined by an experienced colonoscopist, the water method has a learning curve that is easily achievable (∼50 cases) even in the absence of an “onsite” trainer. Failure based on ITT did not preclude cecal intubation after the colonoscopist reverted back to the air method. Unfamiliarity with the appearance of the appendix opening under water prolonged initial insertion time which with experience diminished to that of the air method. This study confirms findings in previous reports1–7 that the water method is associated with lower overall sedation requirement, less use of additional intra-procedure sedative medications and less need for external pressure. In conclusion the water method is easy to learn for an experienced colonoscopist. Mastery of the method resulted in cecal intubation rate and overall adenoma detection rate meeting quality performance standards.
Acknowledgement
This study was supported in part by VA Clinical Merit Research Funds and an American College of Gastroenterology Clinical Research Award (FWL).
Abbreviations
- ADR
adenoma detection rate
- IC
ileocecal
- ITT
intent-to-treat
- VA
Veterans Affairs
- CORI
Clinical Outcomes Research Initiative
- SEM
standard error of mean
- n.s.
not significant
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
References
- 1.Leung JW, Mann S, Leung FW. Options for screening colonoscopy without sedation: a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 2.Leung JW, Salera R, Toomsen L, Mann S, Leung FW. Pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci. 2009;54:1997–2001. doi: 10.1007/s10620-008-0576-4. [DOI] [PubMed] [Google Scholar]
- 3.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–550. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 5.Leung JW, Mann SK, Siao-Salera RM, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 6.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 7.Ransibrahmanakul K, Leung JW, Mann SK, Siao-Salera R, Lim BS, Hasyagar C, et al. Comparative effectiveness of water vs. air methods in minimal sedation colonoscopy performed by supervised trainees in the US - randomized controlled trial. Am J Clin Med. 2010;7:113–118. [Google Scholar]
- 8.Leung JW, Do L, Siao-Salera RM, Parikh DA, Mann SK, Leung FW. Retrospective analysis showing the water method increased adenoma detection rate -a hypothesis generating observation. J Interv Gastroenterol. 2011;1:3–7. doi: 10.4161/jig.1.1.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung FW, Leung JW, Siao-Salera RM, Mann SK. The water method significantly enhances proximal diminutive adenoma detection rate in unsedated patients. J Interv Gastroenterol. 2011;1:8–13. doi: 10.4161/jig.1.1.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leung FW. Is there a place for sedationless colonoscopy? J Interv Gastroenterol. 2011;1:19–22. doi: 10.4161/jig.1.1.14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramirez FC, Leung FW. Adopting the water method: lessons, tips and pitfalls learned. Am J Clin Med. 2010;7:121–123. [Google Scholar]
- 12.Falchuk ZM, Griffin PH. A technique to facilitate colonoscopy in areas of severe diverticular disease. New Engl J Med. 1984;310:598. doi: 10.1056/NEJM198403013100919. [DOI] [PubMed] [Google Scholar]
- 13.Baumann UA. Water intubation of the sigmoid colon: water instillation speeds up left-sided colonoscopy. Endoscopy. 1999;31:314–317. doi: 10.1055/s-1999-23. [DOI] [PubMed] [Google Scholar]
- 14.Hamamoto N, Nakanishi Y, Morimoto N, Inoue H, Tatukawa M, Nakata S, et al. A new water instillation method for colonoscopy without sedation as performed by endoscopists-in-training. Gastrointest Endosc. 2002;56:825–828. doi: 10.1067/mge.2002.129608. [DOI] [PubMed] [Google Scholar]
- 15.Church JM. Warm water irrigation for dealing with spasm during colonoscopy: simple, inexpensive, and effective. Gastrointest Endosc. 2002;56:672–674. doi: 10.1067/mge.2002.128916. [DOI] [PubMed] [Google Scholar]
- 16.Brocchi E, Pezzilli R, Tomassetti P, Campana D, Morselli-Labate AM. Corinaldesi R, Warm water or oil-assisted colonoscopy: toward simpler examinations? Am J Gastroenterol. 2008;103:581–587. doi: 10.1111/j.1572-0241.2007.01693.x. [DOI] [PubMed] [Google Scholar]
- 17.Leung FW. Water-related techniques for performance of colonoscopy. Dig Dis Sci. 2008;53:2847–2850. doi: 10.1007/s10620-008-0259-1. [DOI] [PubMed] [Google Scholar]
- 18.Mizukami T, Yokoyama A, Imaeda H, Koichiro Kumai K. Collapse-submergence method: simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Digest Endosc. 2007;19:43–47. [Google Scholar]
- 19.Leung CW, Kaltenbach T, Soetikno R, Wu KK, Leung FW, Friedland S. Colonoscopy insertion technique using water immersion versus standard technique: a randomized trial showing promise for minimal-sedation colonoscopy. Endoscopy. 2010;42:557–563. doi: 10.1055/s-0029-1244231. [DOI] [PubMed] [Google Scholar]
- 20.Kahi CJ, Anderson JC, Waxman I, Kessler WR, Imperiale TF, Li X, et al. High-definition chromocolonoscopy vs. high-definition white light colonoscopy for average-risk colorectal cancer screening. Am J Gastroenterol. 2010;105:1301–1317. doi: 10.1038/ajg.2010.51. [DOI] [PubMed] [Google Scholar]
- 21.Eisele R, Vogelsang E, Kraft K, Baumgarten U, Schick RR. Screening for colorectal lesions with high-resolution video colonoscopes in a German male average-risk population at 40 to 59 years of age. Z Gastroenterol. 2007;45:952–957. doi: 10.1055/s-2007-963477. [DOI] [PubMed] [Google Scholar]
- 22.Rogart JN, Siddiqui UD, Jamidar PA, Aslanian HR. Fellow involvement may increase adenoma detection rates during colonoscopy. Am J Gastroenterol. 2008;103:2841–2846. doi: 10.1111/j.1572-0241.2008.02085.x. [DOI] [PubMed] [Google Scholar]
- 23.Adler A, Pohl H, Papanikolaou IS, Abou-Rebyeh H, Schachschal G, Veltzke-Schlieker W, et al. A prospective randomised study on narrow-band imaging versus conventional colonoscopy for adenoma detection: does narrow-band imaging induce a learning effect? Gut. 2008;57:59–64. doi: 10.1136/gut.2007.123539. [DOI] [PubMed] [Google Scholar]
- 24.Imperiale TF, Glowinski EA, Juliar BE, Azzouz F, Ransohoff DF. Variation in polyp detection rates at screening colonoscopy. Gastrointest Endosc. 2009;69:1288–1295. doi: 10.1016/j.gie.2007.11.043. [DOI] [PubMed] [Google Scholar]
- 25.Radaelli F, Paggi S, Amato A, Terruzzi V. Warm water infusion versus air insufflation for unsedated colonoscopy: a randomized, controlled trial. Gastrointest Endosc. 2010;72:701–709. doi: 10.1016/j.gie.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 26.Friedland S. The water immersion technique for colonoscopy insertion. Gastroenterol Hepatol (N Y) 2010;6:555–556. [PMC free article] [PubMed] [Google Scholar]