Abstract
Background
The water method facilitates colonoscope insertion in unsedated patients.
Objective
To compare quality indicators in sedated veterans.
Design
Performance improvement.
Setting
VA endoscopy unit.
Patients
368 consecutive screening patients.
Intervention:
Air or water method assignment (high definition colonoscope) was based on the last digit of social security number.
Measurements
Adenoma detection rate (ADR), cecal intubation rate; intubation and withdrawal times; sedation requirements and external pressure used.
Results
ADR was higher with the water method (57.1% vs. 46.1%, p=0.04). After controlling for age, body mass index, smoking, alcohol, withdrawal time and quality of bowel preparation, the odds of detecting an adenoma was 81% higher with the water method (OR 1.81; 95% cI: 1.12–2.90). In the proximal colon ADR was higher with the water method (45.8% vs. 34.6%, p=0.03), including adenomas <10 mm in size (41.8% vs. 31.4%, p=0.04). The water method showed significantly longer cecal intubation time (6.9±0.3 vs. 5.3±0.3 min, p=0.0001); less external pressure used (11.9% vs. 28.3%, p=0.0001); lower need for additional sedation (17.5% vs. 27.2%, p<0.03).
Limitations
Predominance of males, single unblinded endoscopist with high ADR.
Conclusions
The water method is an independent factor associated with significantly higher ADR. Replication by blinded colonoscopist(s) is indicated.
Key words: colonoscopy, adenoma detection, water method, air method
Introduction
The water method developed to minimize colonoscopy discomfort1–7 yielded numerically higher adenoma detection rate (ADR) in unsedated veterans in one observational study3 and one small RCT6 and significantly higher ADR in one retrospective data base review8 in sedated veterans. In predominantly unsedated veterans the impact was more pronounced on the diminutive adenomas in the proximal colon.9 In the current performance improvement project we assessed quality indicators in patients undergoing sedated screening colonoscopy in a head-to-head comparison of the water and air methods. We tested the hypothesis that the water method yields superior quality indicator data.
Methods
Study Design
A performance improvement project evaluating the utility of the water method was carried out by a single unblinded colonoscopist (FCR) at the Carl T. Hayden VAMC in Phoenix, Arizona. Data were collected prospectively to monitor performance. Approval was obtained from the local IRB to report the observations. Informed consent waiver was granted since data were de-identified.
Patients
368 consecutive screening colonoscopy patients (9/2009–8/2010) were scheduled by staff without knowledge of the assignments. A standard bowel preparation of clear liquid diet, bisacodyl 20 mg and four liters of polyethylene glycol (PEG) on the day before procedure was used. Those with diabetes, chronic constipation or on chronic narcotics received an additional two liters of PEG the day prior to the standard preparation.
Assignment
Patients were assigned at the time of endoscopy, using quasi-randomization allocation to treatment10 based on the last digit of the patient's social security number (SSN) - air (odd number) or water (even number). Patients were excluded if any fellow in training was involved in the procedure.
Assessment of Outcomes
All colonoscopies were performed using adult, high-definition equipment (Olympus CFH-180). Pre-medications included fentanyl and midazolam. Blood pressure, pulse, electrocardiogram and pulse oximetry were monitored. Colonoscopy began with the patient in the left lateral decubitus position. Tolerability was assessed by the colonoscopist. Additional sedation administered was patient-driven depending on the level of discomfort reported. Patient age, gender, body mass index (BMI), current smoking and alcohol consumption were recorded.
Interventions
Air method
Air insufflation, shortening maneuvers, abdominal compression and change of patient position were used as needed to facilitate the proximal advancement of the colonoscope.
Water method11,12
The air pump was turned off and water (room temperature) was infused by a pedal pump connected to the base of the colonoscope. Removal of angulations by suction of residual air was implemented. The tip of the colonoscope was oriented towards and abutted the “slit-like lumen” ahead and the infused water opened the lumen if the orientation was correct. The colonoscope was advanced by a series of to and fro, back and forth, or repeated insertion and withdrawal motions of the shaft of the colonoscope with a torque in the direction of the expected lumen, and intermittent water infusion. Suspended residual feces obscuring the view had to be suctioned and replaced by clean water until the colonic lumen was visualized again. The turbulence produced by the simultaneous infusion and suction of water in the collapsed lumen dislodged the residual feces from the surrounding mucosa in close proximity to the tip of the colonoscope. Most of the infused water was aspirated into the suction bottle instead of remaining in the colon. Over-distension was obviated. If advancement failed, the assistant provided abdominal compression followed by the patient changing position if necessary. When the cecum was thought to be reached, the air feature was turned on to confirm the location. If the cecum had not been reached, failed intubation was recorded based on intent-to-treat (ITT) but colonoscopy was continued.
Both methods during insertion and withdrawal
Cecal intubation was defined as passage of the colonoscope tip to a point proximal to the ileocecal valve so that the entire cecal caput, including the medial wall of the cecum between the ileocecal valve and appendix orifice were visible. Cleaning of mucosal surface with water and suction of residual water were implemeted. Air insufflation was used to distend the colon for inspection, biopsy and polypectomy.
Primary endpoint
The primary outcome was ADR (proportion of patients with at least one adenoma of any size).
Secondary endpoints
Colon cleanliness was documented using the Clinical Outcomes Research Initiative (CORI) drop box (Table 1) as an overall (non-segmental) assessment at the end of each procedure. Success of cecal intubation (ITT and final), intubation and withdrawal time (stopwatch was started at the time of introduction of the colonoscope into the rectum and stopped at the time of its removal from the patient; intubation time was calculated as the time elapsed from insertion to cecal intubation whereas withdrawal time was calculated as: total procedure time - cecal intubation time), use of external compression, patient position change, additional sedation medication during colonoscopy, and polyp and adenoma detection rates (total, proximal and distal) were recorded. Adverse events were registered.
Table 1.
Colon cleanliness was recorded using the Clinical Outcomes Research Initiative (CORI) drop box
| Excellent | No more than small bits of adherent fecal material |
| Good | Small amounts of feces or fluid not interfering with the examination |
| Fair-adequate | Between good and fair-compromised |
| Fair-compromised | Enough feces or fluid to prevent a completely reliable examination |
| Poor | Large amounts of fecal residue with additional cleansing required |
Statistical analysis
For sample size calculation, an ADR of 46% in the air group based on historical data13 was adopted. An 11% increase in ADR was considered to be clinically significant.3,8 To show a significant difference with 80% power and an alpha of 0.05, 354 subjects or 177 per group were needed. All outcomes were analyzed using ITT. Data are frequency count (%) and mean±SEM (standard error of mean). Student's t-test, Fisher's exact test and logistic regression analysis calculated using SPSS 16.0 software (SPSS, Chicago, Illinois). A p value <0.05 was considered significant.
Results
In the time needed to recruit 177 subjects in the water group, 191 were examined in the air group (see Figure 1: Flow Chart). The mean age was 60.0±0.5 and 59.3±0.5 years, with seven and six women in the water and air group, respectively. The proportion of current smokers was significantly higher in the air group; the proportion of current 3“occasional” alcohol drinkers was similar in the two groups. Seventeen patients underwent colonoscopy without any sedation (8 in the water, and 9 in the air group). Patients in the water group received significantly lower doses of both fentanyl (68.8±1.4 vs. 76.5±1.7 mg; p=0.0006) and midazolam (2.8±0.1 vs. 3.1±0.1 mg; p=0.0007) (Table 2).
Figure 1.
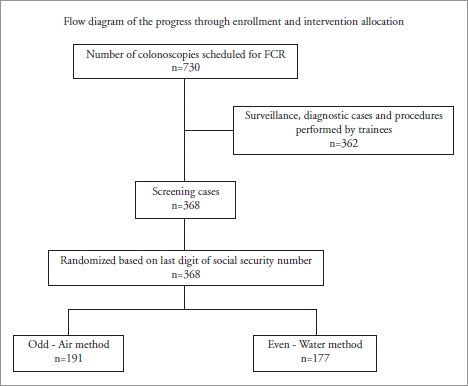
Flow diagram
Table 2.
Head-to-head comparison of water vs. air method in screening colonoscopy patients
| Air (n=191) | Water (n=177) | p* | |
| Age (years) | 59.3±0.5 | 60.0±0.5 | n.s. |
| Gender (male/female) | 184/7 | 171/6 | n.s. |
| BMI | 29.9±0.4 | 30.1±0.4 | n.s. |
| Current smokers | 68 of 191 (35.6%) | 44 of 174 (25.3%) | 0.03 |
| Proportion of current smokers with adenomas | 33 of 68 (48.5%) | 24 of 44 (54.5%) | 0.56 |
| Current 3occasional alcohol drinkers | 73 of 191 (38.2%) | 78 of 177 (44.1%) | 0.289 |
| Proportion of current 3occasional alcohol drinkers with adenomas | 34 of 73 (46.6%) | 45 of 78 (57.7%) | 0.19 |
| ITT cecal intubation | 100% | 92% | n.s. |
| Final cecal intubation | 100% | 99.4% | n.s. |
| Time to cecum (min) | 5.3±0.3 | 6.9±0.3 | <0.0001 |
| Withdrawal time (min) | 13.7±0.5 | 12.9±0.4 | n.s. |
| Total time (min) | 18.9±0.6 | 19.9±0.5 | n.s. |
| External pressure; n (%) | 54 (28.3%) | 21 (11.9 %) | <0.0001 |
| Change in position | 22 (11.5 %) | 14 (7.9 %) | n.s. |
| Fair-adequate or fair-compromised prep | 41 (21.5%) | 28 (15.8%) | n.s. |
| Good or Excellent prep | 150 (78.5%) | 149 (84.2%) | n.s. |
| Fair-adequate or fair-compromised tolerance | 14 (7.3%) | 12 (6.8%) | n.s. |
| Good or Excellent tolerance | 177 (92.7%) | 165 (93.2%) | n.s. |
| Fentanyl dose (mg) | 76.5±1.7 | 68.8±1.4 | 0.0006 |
| Midazolam dose (mg) | 3.1±0.1 | 2.8±0.1 | 0.0007 |
| Added sedation | 52 (27.2%) | 31 (17.5%) | 0.03 |
Data are mean ± SEM and frequency count (%).
Student's t test or Fisher's exact test.
Primary endpoint
The ADR was significantly higher in the water (57.1%) than the air group (46.1%) (p=0.04). After controlling for age, BMI, current smoking and alcohol consumption, withdrawal time and quality of bowel preparation, the odds of detecting an adenoma was 81% higher in the water than the air group (OR 1.81; 95%CI: 1.12–2.90). Patients with at least one proximal adenoma were significantly more likely to be in the water than the air group (45.8% vs. 34.6%; p=0.03) and this was true for adenomas <10 mm in size (41.8% vs. 31.4%; p=0.04) (Table 3).
Table 3.
Adenoma detection rate (ADR), advanced neoplasia (AN) and anatomical distribution (proximal = proximal to splenic flexure; distal = splenic flexure and below)
| Air Method (n=191) | Water Method (n=177) | p* | |
| Screening | 100% | 100% | |
| Total number polyps | 364 | 375 | |
| Polyps/patient | 1.9±0.2 | 2.1±0.2 | n.s. |
| Total number adenomas | 213 | 211 | |
| Adenomas/patient | 1.1±0.1 | 1.2±0.1 | |
| Number of proximal adenomas | 134 (62.9%) | 142 (67.3%) | n.s. |
| Number of distal adenomas | 79 (37.1%) | 69(32.7 %) | n.s. |
| Patients with AN, n (%) | 39 (20%) | 27 (15.3%) | n.s. |
| Patients with ≥ 3 adenomas (without AN features) | 7 (3.6%) | 10 (5.6%) | n.s. |
| Patients with cancer | 4 (1 Proximal) | 1 (Proximal) | |
| Adenoma detection rate; n (%) | 88 (46.1%) | 101 (57.1%) | 0.04 |
| At least one proximal adenoma; n (%) | 66 (34.6%) | 81 (45.8%) | 0.03 |
| <10 mm | 60 (31.4%) | 74 (41.8%) | 0.04 |
| ≥10 mm | 19 (9.9%) | 15 (8.5%) | n.s. |
| At least 1 distal adenoma; n (%) | 54 (28.3%) | 52 (29.4%) | n.s. |
| <10 mm | 35 (18.3%) | 41 (23.2%) | n.s. |
| ≥10 mm | 31 (16.2%) | 18 (10.2%) | n.s. |
AN, advanced neoplasm. Data are mean ± SEM and frequency count (%).
Student's t test or Fisher's exact test.
Secondary endpoints
Cecal intubation was achieved in 99.4% in the water, and 100% in the air group. ITT cecal intubation was 92% in the water, and 100% in the air group, respectively. Fourteen (8%) patients who were assigned to the water group crossed over to the air group (“failed” cecal intubation using water method only). Although the total procedure and withdrawal times were similar, the water group had a significantly longer cecal intubation time (6.9±0.3 vs. 5.3±0.3 min; p<0.0001) (Table 2).
Compared with the air method, significantly fewer patients in the water method required external pressure (11.9% vs. 28.3%; p<0.0001). The need for change in patient position was lower (but not statistically significant) in the water group (7.9% vs. 11.5%). Colon preparation and patient's tolerance were rated good to excellent similarly in both groups. Additional intraprocedure sedation was required significantly less often with the water (17.5%) than the air method (27.2%) (p=0.03) (Table 2).
The water and air groups had similar number of polyps and polyps/patient (375, 2.1±0.2 vs. 364, 1.9±0.2); adenomas and adenomas/patient (211; 1.2±0.1 vs. 213; 1.1±0.1). The water method group had significantly more patients (79.1%) with at least one polyp, than the air method group (63.8%) (p=0.001).
Supplementary analyses
In patients rated to have a good to excellent bowel preparation the ADR in the water group was significantly higher 58.4% vs. 45.1% (p=0.02).
Five (1.34%) cancers were found, one in the water, and four in the air group. Excluding those with cancer, advanced neoplasia (AN) (defined by size ≥10 mm, villous histology or high grade dysplasia) rates were similar (27 patients (15.3%) vs. 39 patients (20%) in the water and air groups, respectively). In addition, ≥3 adenomas (without AN features) were found in 17 patients: seven in the water, and ten in the air group (Table 3). There was no significant difference in the proportion of subjects with combined advanced neoplasms and cancers (air, 43 of 191, water 28 of 177).
Adverse events
There was one (0.3%) post-polypectomy bleeding requiring endoscopic therapy and hospitalization, and one vasovagal reaction requiring atropine among the 368 patients studied.
Discussion
The already reported beneficial effects of the water method1–7 are further enhanced by the results of this study where the water method group revealed a significantly higher ADR than the conventional colonoscopy. Earlier precursors in the form of water-related techniques as adjuncts to air insufflation have been described14–18 and recently reviewed.18,19 With the patient in the left lateral position, the water infused opens a passage14 and weighs down the left colon straightening the sigmoid segment thus facilitating the advancement of the colonoscope15,16 whereas suction of residual air in the colonic lumen minimizes angulations at the flexures.17 The turbulence set up by the simultaneous suction of dirty water and infusion of clean water in the collapsed colonic lumen facilitates suspension of the residual feces for removal by suction11,12 providing serendipitously salvage bowel cleansing in patients with suboptimal bowel preparation.1–7 This salvage cleansing in part could have accounted for the significantly increased ADR previously observed with the water method.8,9
In the current head-to-head comparative study we found although the cecal intubation time was significantly longer (albeit only 1.6 minutes) in the water group, the method had significantly less frequent assistant involvement to provide external pressure, lower fentanyl and midazolam doses and less intra-procedure added sedation than the air group. These findings may have implications not only from the patient's (safety) but also the assistant's (external pressure application) and nursing staff's (recovery time) perspective.
Even though withdrawal times were equivalent (water, 12.9±0.4 vs. air, 13.7±0.5 min), ADR was significantly higher in the water (57.1%) than the air (46.1%) group. The water group ADR compares favorably to recently reported ADR with high definition white light equipment (48.8%) or high definition chromocolonoscopy (55.5%) in average risk screening patients.20 Compared to the air method, the effect of the water method was more pronounced in the proximal than in the distal colon particularly for those adenomas <10 mm in size (41.8% vs. 31.4%; p=0.04). The number of polyps and adenomas per patient, the number of patients with non-neoplastic lesions being similar in both groups and, finding an ADR of 46.1% in the air group being similar to a prior baseline period,13 argue against an effect of heightened attention to identify polyps and adenomas only in the water group. The ADR (57.1%) with the water method compares more favorably to ADR reported in screening colonoscopy by others.20–22 The explanations for the higher ADR in the water than the air method group remain to be determined.
Although our study did not show any difference in the rate of patients with advanced neoplasia or, three or more adenoma between the two methods, the combined rates (24% and 21% for the air and water methods, respectively) were above those reported in the literature (3.2% to 13%).20–22 The cancer detection rate in our study is similar to those reported in other screening colonoscopy studies.20–22
Our results differ from those of Radaelli et al.27 who reported a significantly lower ADR in the water than the air group (25% vs. 40%) and might be related to fundamental methodolical differences16,28. They permitted the use of air insufflation at the beginning of colonoscopy and whenever difficulty was encountered during colonoscopy; water exchange during insertion was not mentioned. Others have pointed out that one limitation of infusing water into the colonic lumen during insertion is a possible decrease in the ability to detect subtle mucosal disease because of excessive residual water in the colon.16 Although residue could be suctioned while infusing more water to clean the colon, if there is too much residue it is very difficult to see clearly enough to insert the colonoscope properly.28 Whether the salvage cleansing during insertion with the water exchange component of the water method3,6,7,11,12 might have accounted for the improvement remains to be further evaluated.
The strengths of this head-to-head comparison include a homogenous population (screening colonoscopy only), the use of high definition equipment in all patients and the absence of ADR variability introduced by multiple endoscopists. The limitations include: the absence of blinding for both endoscopist and nurse injects the potential for bias that could not be avoided; a single endoscopist experience is akin to a case series and the high ADR in the air method group undercut the generalizability of the results; the quasi rather than true randomization design; and the evaluation of predominantly male veterans. Future studies taking these issues into account deserve to be supported.
In conclusion, the data confirm findings that compared to the air method, the water method is associated with significantly higher ADR8 especially in the proximal colon.9 The novelty rests with the enhancement being independent of age, BMI, current smoking and alcohol consumption, withdrawal time and quality of bowel preparation. Applicability in non-veteran settings should be assessed.
Acknowledgements
This study was supported in part by VA Clinical Merit Research Funds and an ACG Clinical Research Award (FWL).
Abbreviations
- ADR
adenoma detection rate
- AN
advanced neoplasia
- BMI
body mass index
- CORI
Clinical Outcomes Research Initiative
- ITT
intent-to-treat
- n.s.
not significant
- VAMC
Veterans Affairs Medical Center
- RCT
randomized controlled trail
- SEM
standard error of mean
- SSN
social security number
Footnotes
Accepted for Oral Presentation at ASGE Topic Forum, May 8, 2011 and selected one of the abstracts to be presented at Best of DDW 2011, May 10, 2011 during Digestive Disease Week.
Previously published online: www.landesbioscience.com/journals/jig/
References
- 1.Leung JW, Salera R, Toomsen L, Mann S, Leung FW. Pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci. 2009;54:1997–2001. doi: 10.1007/s10620-008-0576-4. [DOI] [PubMed] [Google Scholar]
- 2.Leung JW, Mann S, Leung FW. Options for screening colonoscopy without sedation: a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–631. doi: 10.1111/j.1365-2036.2007.03404.x. [DOI] [PubMed] [Google Scholar]
- 3.Leung FW, Aharonian HS, Leung JW, Guth PH, Jackson G. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. 2009;69:546–550. doi: 10.1016/j.gie.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Leung JW, Mann SK, Siao-Salera R, Ransibrahmanakul K, Lim B, Cabrera H, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009;70:505–510. doi: 10.1016/j.gie.2008.12.253. [DOI] [PubMed] [Google Scholar]
- 5.Ransibrahmanakul K, Leung JW, Mann SK, Siao-Salera R, Lim BS, Hasyagar C, et al. Comparative effectiveness of water vs. air methods in minimal sedation colonoscopy performed by supervised trainees in the US-randomized controlled trial. Am J Clin Med. 2010;7:113–118. [Google Scholar]
- 6.Leung FW, Harker JO, Jackson G, Okamoto KE, Behbahani OM, Jamgotchian NJ, et al. A proof-of-principle, prospective, randomized, controlled trial demonstrating improved outcomes in scheduled unsedated colonoscopy by the water method. Gastrointest Endosc. 2010;72:693–700. doi: 10.1016/j.gie.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Leung JW, Mann SK, Siao-Salera RM, Ransibrahmanakul K, Lim BS, Canete W, et al. A randomized, controlled trial to confirm the beneficial effects of the water method on U.S. veterans undergoing colonoscopy with the option of on-demand sedation. Gastrointest Endosc. 2011;73:103–110. doi: 10.1016/j.gie.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 8.Leung JW, Do L, Siao-Salera RM, Parikh DA, Mann SK, Leung FW. Retrospective data showing the water method increased adenoma detection rate - a hypothesis generating observation. J Interv Gastroenterol. 2011;1:3–7. doi: 10.4161/jig.1.1.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung FW, Leung JW, Siao-Salera RM, Mann SK. The water method significantly enhances proximal diminutive adenoma detection rate in unsedated patients. J Interv Gastroenterol. 2011;1:8–13. doi: 10.4161/jig.1.1.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Training manual for handsearchers. Prepared by US Cochrane Center Latest revision December 13, 2002.
- 11.Leung FW. Is there a place for sedationless colonoscopy? J Interv Gastroenterol. 2011;1:19–22. doi: 10.4161/jig.1.1.14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leung FW, Leung JW, Mann SK, Friedland S, Ramirez FC. Innovation Forum - The water method significantly enhances the outcome of colonoscopy in sedated and unsedated patient. Endoscopy. 2011 May 24; doi: 10.1055/s-0030-1256407. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Ramirez FC, Leung FW. The water method for aiding colonoscope insertion: the learning curve of an experienced colonoscopist. J Interv Gastroenterol. 2011 doi: 10.4161/jig.1.3.18507. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Falchuk ZM, Griffin PH. A technique to facilitate colonoscopy in areas of severe diverticular disesase (letter) N Engl J Med. 1984;310:598. doi: 10.1056/NEJM198403013100919. [DOI] [PubMed] [Google Scholar]
- 15.Baumann UA. Water intubation of the sigmoid colon: water instillation speeds up left-sided colonoscopy. Endoscopy. 1999;31:314–317. doi: 10.1055/s-1999-23. [DOI] [PubMed] [Google Scholar]
- 16.Hamamoto N, Nakanishi Y, Morimoto N, Inoue H, Tatukawa M, Nakata S, et al. A new water instillation method for colonoscopy without sedation as performed by endoscopists-in-training. Gastrointest Endosc. 2002;56:825–828. doi: 10.1067/mge.2002.129608. [DOI] [PubMed] [Google Scholar]
- 17.Mizukami T, Yokoyama A, Imaeda H, Kumai K. Collapse-submergence method: simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Digest Endosc. 2007;19:43–48. [Google Scholar]
- 18.Leung FW. Water-related method for performance of colonoscopy. Dig Dis Sci. 2008;53:2847–2850. doi: 10.1007/s10620-008-0259-1. [DOI] [PubMed] [Google Scholar]
- 19.Leung FW. A hypothesis-generating review of the water method for difficult colonoscopy. Scand J Gastroenterol. 2011;46:517–521. doi: 10.3109/00365521.2011.551885. [DOI] [PubMed] [Google Scholar]
- 20.Kahi CJ, Anderson JC, Waxman I, Kessler WR, Imperiale TF, Li X, et al. High-definition chromocolonoscopy vs. high-definition white light colonoscopy for average-risk colorectal cancer screening. Am J Gastroenterol. 2010;105:1301–1307. doi: 10.1038/ajg.2010.51. [DOI] [PubMed] [Google Scholar]
- 21.Rogart JN, Siddiqui UD, Jamidar PA, Aslanian HR. Fellow involvement may increase adenoma detection rates during colonoscopy. Am J Gastroenterol. 2008;103:2841–2846. doi: 10.1111/j.1572-0241.2008.02085.x. [DOI] [PubMed] [Google Scholar]
- 22.Adler A, Pohl H, Papanikolaou IS, Abou-Rebyeh H, Schachschal G, Veltzke-Schlieker W, et al. A prospective randomised study on narrow-band imaging versus conventional colonoscopy for adenoma detection: does narrow-band imaging induce a learning effect? Gut. 2008;57:59–64. doi: 10.1136/gut.2007.123539. [DOI] [PubMed] [Google Scholar]
- 23.Bressler B, Paszat LF, Vinden C, Li C, He J, Rabeneck L. Colonoscopic miss rates for right-sided colon cancer: a population-based analysis. Gastroenterology. 2004;127:4526. doi: 10.1053/j.gastro.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 24.Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150:1–8. doi: 10.7326/0003-4819-150-1-200901060-00306. [DOI] [PubMed] [Google Scholar]
- 25.Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L, Haug U. Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study. J Natl Cancer Inst. 2010;102:89–95. doi: 10.1093/jnci/djp436. [DOI] [PubMed] [Google Scholar]
- 26.Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M. Protection from colorectal cancer after colonoscopy: a population-based, case-control study. Ann Intern Med. 2011;154:22–30. doi: 10.7326/0003-4819-154-1-201101040-00004. [DOI] [PubMed] [Google Scholar]
- 27.Radaelli F, Paggi S, Amato A, Terruzzi V. Warm water infusion versus air insufflation for unsedated colonoscopy: a randomized, controlled trial. Gastrointest Endosc. 2010;72:701–709. doi: 10.1016/j.gie.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 28.Friedland S. The water immersion technique for colonoscopy insertion. Gastroenterol Hepatol (N Y) 2010;6:555–556. [PMC free article] [PubMed] [Google Scholar]


