Pyogenic liver abscess is a rare but serious condition resulting in significant morbidity and mortality if left untreated1. The first line treatment for hepatic abscess is the transcutaneous or surgical approach with an 80–100% success rate2–4. However, these modalities are associated with numerous risks including bleeding, biliary peritonitis, fistula formation, and patient discomfort. The caudate lobe is anatomically difficult to access percutaneously. Given its proximity to the stomach, a transgastric approach to drainage is feasible. We report two consecutive patients who underwent EUS-guided transgastric drainage of a caudate lobe abscess.
Methods
Endoscopic ultrasound (EUS) was performed using a therapeutic linear array echoendoscope (Olympus GF-UCT 140; Center Valley, PA). A 19-gauge needle (EchoTip Ultra; Cook Endoscopy, Winston-Salem, NC) was advanced into the abscess. Aspirates were obtained followed by contrast injection. A 0.035″ guidewire (Jagwire; Boston Scientific, Natick, MA.) was coiled inside the cavity. Serial dilation of the hepatico-gastrostomy was performed with a 4mm Hurricane® RX hydrostatic balloon (Boston Scientific, Natick, MA) and an 8–10 mm CRE balloon (Boston Scientific, Natick, MA.). One or two double pigtail biliary endoprosthesis (Wilson-Cook Medical Inc., Winston-Salem, N.C.) were then placed under fluoroscopic guidance into the abscess. This resulted in immediate drainage of pus into the stomach.
Case 1
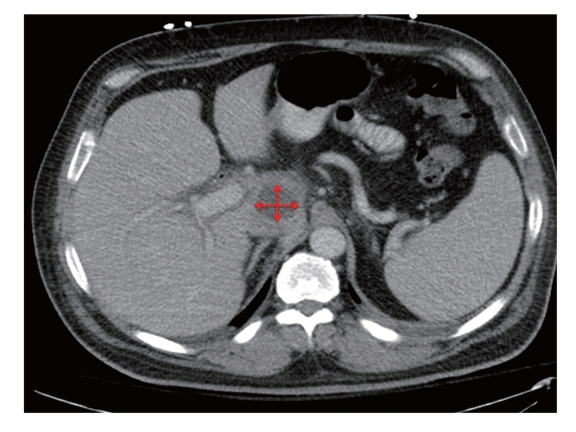
A 63 year old man with a history of metastatic pancreatic cancer presented with fever and lethargy. CT abdomen confirmed a 25 mm × 25 mm caudate lobe liver abscess (Fig. 1). Transcutaneous drainage was attempted; however the patient became hemodynamically unstable during the procedure. The patient developed septic shock with subsequent renal failure requiring hemodialysis and ICU admission. Given the favorable location of the abscess relative to the stomach, EUS-guided transgastric drainage was pursued. Drainage was successful, with placement of two stents (7Fr/5cm, 10Fr/7cm). There were no immediate complications. After a prolonged hospitalization of 1 month he was discharged home well and able to resume treatment for his pancreas cancer. CT scan performed 5 weeks after endoscopy confirmed resolution of the abscess. The stents were removed 46 days post endoscopy.
Figure 1.
CT scan demonstrating caudate lobe abscess.
Case 2
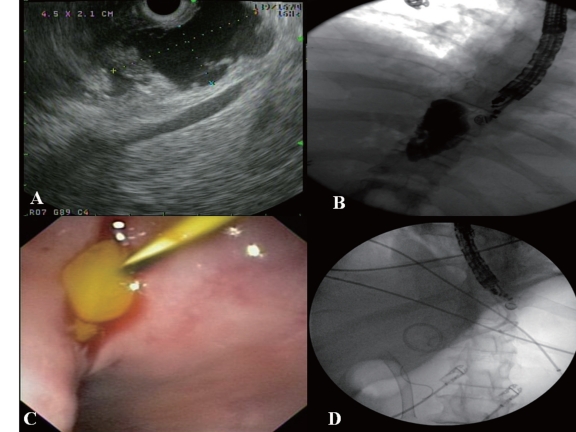
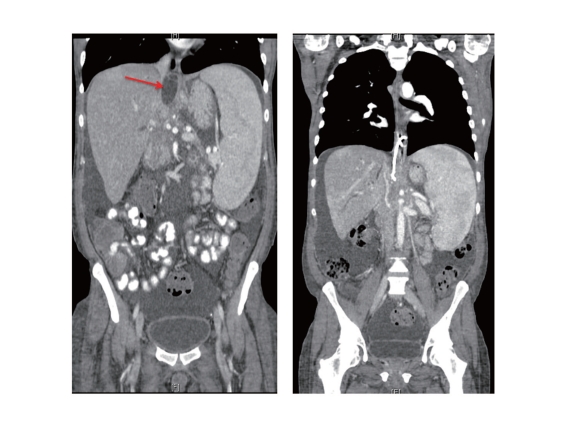
A 42 yr old male with a history of diffuse large B cell lymphoma, status post bone marrow transplant, with a clinical course notable for choledocholithiasis, benign biliary stricture, and portal hypertension presented with right upper quadrant pain and fever. CT scan demonstrated a 45 mm × 21 mm caudate lobe liver abscess. EUS-guided transgastric drainage with placement of a single 7Fr/5cm double pigtail stent was successfully performed (Fig.2). The patient had no immediate complications. He had a prolonged admission due to pancytopenia and complications from portal hypertension. A follow-up CT scan at 6 weeks confirmed resolution of the abscess (Fig.3). The stent was subsequently removed 60 days post endoscopy.
Figure 2.
(A) EUS image of caudate abscess from stomach, (B) Fluoroscopy image of transgastric puncture and contrast within abscess cavity, (C) Endoscopic view with 0.035′ wire inserted into abscess cavity and pus draining, (D) Fluoroscopy image post transgastric double pigtail stent placement.
Figure 3.
CT coronal reconstruction demonstrating pre and post EUS guided drainage of caudate abscess.
Discussion
As the role for therapeutic EUS continues to expand, these two cases further illustrate a new modality for draining caudate, and potentially left liver lobe abscesses in those where the transcutaneous or surgical approach may be contraindicated. There is limited published data with one recent case series and a case report demonstrating its safety and efficacy both via transduodenal and transgastric approach5,6. In this article, we present two cases of a caudate lobe abscess successfully drained by EUS-guided transgastric drainage without complication. The technique used was similar to those previously described. EUS allows for easy identification of intervening vessels and thus may reduce the risk of bleeding. Furthermore by avoiding the transcutaneous route, the risk of discomfort associated with an external drain is obviated, and may allow for improved quality of life. Further experience with therapeutic EUS and the development of improved echoendoscopes will allow for increased application in this field.
Abbreviations
- EUS
endoscopic ultrasound
Footnotes
Previously published online: www.landesbioscience.com/journals/jig
References
- 1.Malik AA, Bari SU, Rouf KA, Wani KA. Pyogenic liver abscess: Changing patterns in approach. World J Gastrointest Surg. 2010;2:395–401. doi: 10.4240/wjgs.v2.i12.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bergamini TM, Larson GM, Malangoni MA, Richardson JD. Liver abscess. Review of a 12-year experience. Am Surg. 1987;53:596–599. [PubMed] [Google Scholar]
- 3.Giorgio A, Tarantino L, Mariniello N, Francica G, Scala E, Amoroso P, et al. Pyogenic liver abscesses: 13 years of experience in percutaneous needle aspiration with US guidance. Radiology. 1995;195:122–124. doi: 10.1148/radiology.195.1.7892451. [DOI] [PubMed] [Google Scholar]
- 4.Liu CH, Gervais DA, Hahn PF, Arellano RS, Uppot RN, Mueller PR. Percutaneous hepatic abscess drainage: do multiple abscesses or multiloculated abscesses preclude drainage or affect outcome? J Vasc Interv Radiol. 2009;20:1059–1065. doi: 10.1016/j.jvir.2009.04.062. [DOI] [PubMed] [Google Scholar]
- 5.Ang TL, Seewald S, Teo EK, Fock KM, Soehendra N. EUS-guided drainage of ruptured liver abscess. Endoscopy. 2009;41:E21–E22. doi: 10.1055/s-0028-1103468. [DOI] [PubMed] [Google Scholar]
- 6.Noh SH, Park do H, Kim YR, Chun Y, Lee HC, Lee SO, et al. EUS-guided drainage of hepatic abscesses not accessible to percutaneous drainage (with videos) Gastrointest Endosc. 2010;71:1314–1319. doi: 10.1016/j.gie.2009.12.045. [DOI] [PubMed] [Google Scholar]