Abstract
Purpose
Tibial fractures in the skeletally immature patient are usually treated without surgery. Elastic stable intramedullary nailing (ESIN) is commonly used for other diaphyseal fracture locations. Its advantages are minimally invasive surgery with a short hospitalisation duration, primary bone union and early weight bearing. The purpose of this study was to assess the use of ESIN in displaced tibial fractures in children over 6 years old and in cases of polytrauma.
Methods
This study was carried out over a 6-year period. The protocol consisted in ESIN of shaft tibial fractures in children over 6. Frontal and sagittal angulation, shortening and lengthening were measured on days 0, 2, 15, 30 and 45. At 6 months, 1 and 2 years, the femoro-tibial axis and eventual shortening or lengthening were assessed.
Results
The study involved 86 children (average age 11.8 years). As early as day 30, all patients had normal knee mobility and symmetrical foot progress angle. At 2-year follow-up, frontal angulation and leg length discrepancy had decreased and affected 2% of patients. Four patients (5%) suffered from superficial infections. There were no cases of osteomyelitis or refracture.
Conclusions
The fixation of paediatric diaphyseal tibial fractures with ESIN is a rapid, well-codified and effective method for treating long-bone closed fractures in children. Advantages over other fixation techniques include a lower infection rate, a lower refracture rate, ease of management, and an aesthetically pleasing scar.
Keywords: Tibial fracture, Intramedullary nail, Child
Introduction
Tibial fractures in the skeletally immature patient are frequent and can usually be treated without surgery [1–3] by closed reduction and casting during 6 or 8 weeks. Elastic stable intramedullary nailing (ESIN or Métaizeau technique) is a method of diaphyseal fracture osteosynthesis in children and adolescents. It is commonly used in femoral shaft fractures, but much less so for tibial fractures. This technique has many advantages. Namely, it does not require a postoperative cast, there is primary bone union with avoidance of growth plate injury, early weight bearing, and minimally invasive surgery with a short duration of hospitalisation [4–6]. The good results of ESIN in femur and forearm fractures justify the use of this technique to treat tibial shaft fractures [7–9]. The purpose of this study was to assess the use of ESIN with flexible nails to treat displaced tibial fractures in children over 6 years old.
Materials and methods
This study analysed a consecutive series of displaced tibial shaft fractures in children treated in the surgical unit over a 6-year period from January 2000 to March 2006. The protocol consisted in intramedullary nailing of all displaced tibial shaft fractures in children over 6 years old, regardless of the fracture stability. In cases of polytrauma, no lower age limit was considered (Fig. 1). Gustilo grade 2 and 3 open fractures [10] were excluded. The surgical technique was that described by Métaizeau [5, 6].
Fig. 1.

In cases of polytrauma, femur and tibia fracture were treated with intramedullar nails, independently of age: this child was 2 years old
Briefly, the starting point for the nail entry hole is approximately 1.5–2.0 cm distal to the physis. Lateral longitudinal 2-cm incisions are made over the proximal tibial metaphysis. Two 2-mm, 3-mm, or 4-mm nails are selected on the basis of the width of the medullary canal. The nails come with a bevelled blunt tip. The tip of the nail is then bent to 45° to ease its passage along the opposite cortex. The entire length of the nail is contoured to a gentle curve such that the apex will reside at or near the fracture site after reduction. The entry point is confirmed with fluoroscopy in both the anteroposterior and lateral planes. Great care is taken to avoid the tibial tubercle apophysis. The hole is made with the drill in the midpoint of the anterioposterior dimension. Under fluoroscopic guidance, the drill is angled caudally until it is 45° from the long axis of the tibia, with care being taken not to drill out the far cortex or migrate toward the physis. A reduction is performed and the nail is advanced across the fracture site. The nail is embedded in the distal tibial metaphysis without violating the cortex or the physis. The second nail is placed from the other side in a similar fashion. The bent tip of the nails is rotated after passing the fracture site to effect an anatomic reduction. The nail ends are then bent distally and posteriorly and cut 1 cm from the cortical surface so that the nail ends will sit deep to the compartment fascia but be long enough for easy retrieval. The wounds are closed with an absorbable fascial and subcuticular stitch.
There was no planned complementary immobilisation. The planned hospitalisation duration was 2–5 days. Follow-up was carried out in an outpatient clinic with radiographies at 15, 30, 45 days and 3 months. Long-length X-rays under load were obtained every 6 months from the 6th month to the 2nd year. Partial weight bearing with crutches was allowed on the 15th day for transverse fractures, on the 21st for short oblique fractures and on the 30th day for the other types. Nails were removed by ambulatory surgery in the 4th month. No physiotherapy was prescribed. Sports activities were stopped for 6 months.
Varus, valgus, procurvatum and recurvatum displacements as well as shortening and lengthening were measured on anteroposterior and sagittal radiographies on days 0, 2, 15, 30 and 45. Medial or lateral translations were evaluated on days 0, 2, 15 and 30. At 6 months, 1 and 2 years, the femoro-tibial axis and eventual shortening or lengthening were measured on long-length X-rays obtained under load. Frontal and sagittal displacement are defined by the angulation at the fracture site of the tibial diaphyseal axis. The medial and lateral displacements are defined by the distance in the frontal plane between the cortical of the proximal and the distal fragments. Leg length discrepancy was thereby determined using the opposite uninjured leg length for comparison. Bone union (defined as the presence of callus on all four cortices) was evaluated. The acceptable alignment criteria cited by Heinrich and Mooney [11] were used and are detailed in Table 1.
Table 1.
Acceptable alignment of a paediatric diaphyseal tibial fracture described by Heinrich and Mooney
| Patient age | <8 years | >8 years |
|---|---|---|
| Valgus | 5° | 5° |
| Varus | 10° | 5° |
| Anterior angulation | 10° | 5° |
| Posterior angulation | 5° | 0 |
| Shortening | 10 mm | 5 mm |
| Rotation | 5° | 5° |
Physical examination was used to evaluate the knee and ankle ranges of motion and foot progress angle and to document eventual complications (pain, reflex sympathetic dystrophy, infection or other).
Statistical analysis
Evolution at 6, 12 and 24 months was compared according to the initial fracture characteristics with analysis of variance (ANOVA). The influence of age and fracture type on the frontal and sagittal angulation and on the residual leg length discrepancy was studied. Outcome for patients aged under or over 12 years was compared with that of patients aged over 12 at the time of trauma [12]. Analysis of the fracture type compared transverse and short oblique fractures versus long oblique and spiroid fractures versus multifragmental or comminuted fractures. Qualitative data were compared by chi-square test or Fisher’s exact test for the smallest groups. Statistical analysis was performed with SAS® software. Results were considered to be significant if P < 0.05.
Results
Study population
During the 6-year investigation period, 102 children were included in our study. However, 16 medical records were incomplete as the patients were lost to follow-up, being tourists. The study involved 86 children (67 boys and 19 girls). The average age was 11 years and 8 months (median 12.9; range 2.5–16.5 years). In this cohort, the operative indication was determined immediately in 82 cases, and after a secondary displacement in four cases. The trauma was direct in 17 cases, indirect in 49 and undertermined in 20. Trauma circumstances are detailed in Table 2. Fifty-three children suffered from isolated tibial shaft fracture and 33 from both tibial and fibular shaft fractures. Fractures involved the right tibia in 49 patients and the left in 37.
Table 2.
Circumstances of tibial shaft fractures
| Circumstances | Details | Number | ||
|---|---|---|---|---|
| Sports | 32 skiing | 6 playing soccer | 4 rollerblading | 51 |
| Road traffic accident | 9 biking | 8 walking | 23 | |
| Falls | 8 | |||
| Falls from a window | 2 | |||
| Direct trauma caused by a slab of marble | 1 | |||
| Unknown | 1 | |||
Fracture locations were on the proximal third for four children, the central third for 60 and the distal third for 22. Three were open fractures (Gustilo 1). There was one pathological fracture on fibrous dysplasia. Fracture types are detailed in Table 3. Initial radiographies showed an initial varus angulation in 45 patients (associated with procurvatum in 7 cases and recurvatum in 13 cases) and valgus in 41 (associated with procurvatum in 8 cases and recurvatum in 16 cases).
Table 3.
Fracture type
| Fracture type | Number |
|---|---|
| Transverse | 14 |
| Short oblique | 5 |
| Long oblique | 8 |
| Spiroid | 46 |
| Multifragmental | 12 |
| Comminuted | 1 |
Initial isolated procurvatum was observed in 15 cases and recurvatum in 29. Initially, lengthening was observed in 6 patients (average 2.6 mm, range 2–3 mm) and shortening was observed in 7 (average 4.2 mm, range 1–6 mm). Translation was medial in 9 cases from 1 to 6 mm (average 5.1 mm) and lateral in 14 cases from 2 to 7 mm (average 3.4 mm). Sixteen children had a lesion other than the leg fracture. There was no vascular or nervous complication.
Mean operation duration was 44 min (range 15–90 min for polytrauma). Titanium nails were used in 83 cases and stainless steel nails in 3 cases. Nail diameters were of 2.5 mm in 4 cases, 3 mm in 19, 3.5 mm in 34 and 4 mm in 29 cases.
Three patients had a postoperative cast: one due to a comminuted tibital fracture, and two due to long postoperative transportation for children returning home to faraway cities. Mean hospitalisation duration was 3.8 days (range 2–11 days). Hospitalisation duration did not exceed 5 days except in the case of the patient with polytrauma.
Fracture outcome
All patients had normal knee mobility from the 30th day to the 24th month and symmetrical foot progress angle. All patients were able to have unrestricted physical activity at the 6-months visit.
No patient had reflex sympathetic dystrophy. Four patients suffered from superficial infections: 3 on the medial surgical wound and 1 on the lateral, and were reoperated on. Nails were shortened on day 15 in 2 cases and removed early in 2 cases, one on day 45 and on day 60 in the other. A walking cast was applied for the latter patient. Partial weight bearing was allowed on day 15 for 25 patients, on day 21 for 28, on day 30 for 29 and on day 45 for 4 children. Among the 86 patients, 59 had an immediate postoperative residual displacement, and 50 on day 2. Comparative results between postoperative and day 2 displacements measured on radiographies are displayed in Table 4. Those between days 15, 30 and 45 are described in Table 5, and the remaining displacements at 6 months, 1 year and 2 years are displayed in Table 6. It is noteworthy that the number of cases of residual displacements in frontal and sagittal planes decreased with time. The remodelling rate was 77% (66 out of 86 patients). Only 2 patients (2.3%) retained a frontal or sagittal angulation at 2 years (Fig. 2). Initial leg length discrepancy did not seem to be greatly modified by growth, as the number of cases (N) with tibial lengthening and shortening after 2 years was similar to that at day 0 (Fig. 3). There was no case of refracture at 2-year follow-up (Fig. 4).
Table 4.
Comparison of displacements between postoperative and day 2 radiographies
| Displacement type | Postoperative radiographies | Day 2 radiographies | ||
|---|---|---|---|---|
| N | Mean displacement (range) | N | Mean displacement (range) | |
| Isolated varus (°) | 5 | 4.5 (1–12) | 6 | 4.8 (2–11) |
| Varus with procurvatum (°) | 3 | 3 | ||
| Varus with recurvatum (°) | 8 | 3 | ||
| Isolated valgus (°) | 6 | 4 (1–10) | 8 | 2.9 (1–8) |
| Valgus with procurvatum (°) | 7 | 9 | ||
| Valgus with recurvatum (°) | 17 | 8 | ||
| Isolated procurvatum (°) | 6 | 4.6 (2–16) | 4 | 3.5 (2–8) |
| Isolated recurvatum (°) | 7 | 5.2 (1–15) | 9 | 4.8 (1–10) |
| Lengthening (mm) | 6 | 2.6 (2–3) | 2 | 2 (2) |
| Shortening (mm) | 7 | 4.2 (1–6) | 7 | 4.2 (1–6) |
| Medial translation (mm) | 9 | 5.1 (1–6) | 6 | 5 (2–6) |
| Lateral translation (mm) | 14 | 3.4 (2–7) | 12 | 3.4 (1–7) |
Table 5.
Comparison of displacements between postoperative days 15, 30 and 45 radiographies
| Displacement type | Day 15 radiographies | Day 30 radiographies | Day 45 radiographies | |||
|---|---|---|---|---|---|---|
| N | Mean displacement (range) | N | Mean displacement (range) | N | Mean displacement (range) | |
| Isolated varus (°) | 4 | 3.9 (1–7) | 6 | 3.8 (1–8) | 8 | 4.1 (2–7) |
| Varus with procurvatum (°) | 3 | 2 | 1 | |||
| Varus with recurvatum (°) | 5 | 8 | 7 | |||
| Isolated valgus (°) | 6 | 3.8 (1–15) | 6 | 3.2 (1–10) | 4 | 4 (1–10) |
| Valgus with procurvatum (°) | 9 | 8 | 5 | |||
| Valgus with recurvatum (°) | 6 | 2 | 4 | |||
| Isolated procurvatum (°) | 4 | 4.3 (2–13) | 2 | 3.4 (1–10) | 4 | 3.7 (2–10) |
| Isolated recurvatum (°) | 9 | 4.5 (1–10) | 9 | 4.6 (2–15) | 8 | 5 (2–13) |
| Lengthening (mm) | 3 | 3.7 (3–4) | 2 | 2.5 (2–3) | 2 | 2.5 (2–3) |
| Shortening (mm) | 11 | 3.1 (1–7) | 8 | 5.2 (3–11) | 9 | 4.7 (2–11) |
| Medial translation (mm) | 6 | 4.2 (1–5) | 6 | 4.2 (2–6) | ||
| Lateral translation (mm) | 9 | 2.7 (1–5) | 9 | 2.7 (1–5) | ||
Table 6.
Comparison of displacements between 6-month, 1- and 2-year radiographies
| Displacement | 6-month radiographies | 1-year radiographies | 2-year radiographies | |||
|---|---|---|---|---|---|---|
| N | Mean displacement (range) | N | Mean displacement (range) | N | Mean displacement (range) | |
| Isolated varus (°) | 6 | 5.1 (1–6) | 1 | 1.5 (1–2) | 2 | 1.5 (1–2) |
| Varus with procurvatum (°) | 3 | 1 | ||||
| Varus with recurvatum (°) | 5 | 0 | ||||
| Isolated valgus (°) | 5 | 4.3 (1–9) | 3 | 3.7 (1–5) | 2 | 3 (1–5) |
| Valgus with procurvatum (°) | 2 | 0 | ||||
| Valgus with recurvatum (°) | 6 | 0 | ||||
| Isolated procurvatum (°) | 5 | 3.8 (1–5) | 1 | 1 | ||
| Isolated recurvatum (°) | 13 | 6.2 (3–10) | 0 | |||
| Lengthening (mm) | 13 | 5.2 (1–10) | 5 | 5.6 (2–5) | 5 | 5.4 (2–8) |
| Shortening (mm) | 15 | 6.2 (2–13) | 10 | 4.3 (1–6) | 10 | 4 (1–5) |
| FTA: valgus (°) | 12 | 2.7 (1–5) | 4 | 3.5 (2–5) | 3 | 3 (2–4) |
| FTA: varus (°) | 16 | 3.9 (1–8) | 10 | 4.7 (4–6) | 8 | 4.3 (4–5) |
FTA femoro-tibial axis
Fig. 2.
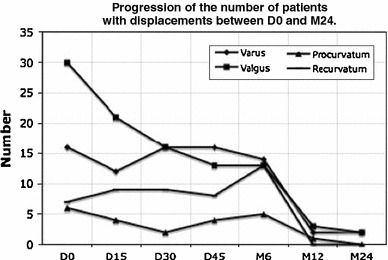
Progression of the number of patients with fracture displacement (varus, valgus, procurvatum and recurvatum angulation) between day 0 and 2 years
Fig. 3.
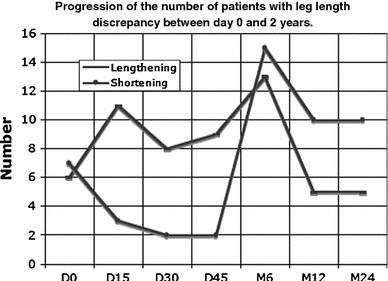
Progression of the number of patients with leg length discrepancy (lengthening or shortening) between day 0 and 2 years
Fig. 4.
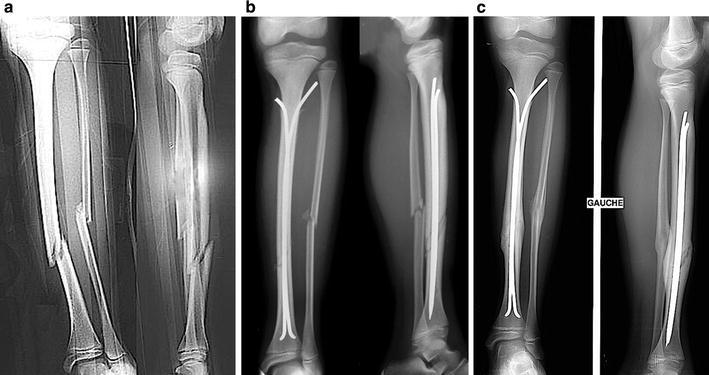
Tibia fracture treated by ESIN, a displaced shaft fracture of fibula and tibia, b ESIN X-rays at day 0 (D0), c X-rays with union
At 12 months postoperative, residual frontal angulation was significantly associated with the transverse and short oblique fractures (5/19; P = 0.004), and particularly so with transverse fractures (5/14). However, none of the initial fracture characteristics had any significant influence on the radiological outcome in frontal plane at 6 and 24 months. Regarding sagittal angulation, no significant results were obtained, probably because of the small number of patients presenting with this displacement. Leg length discrepancy was significantly correlated with age (P = 0.002). Furthermore, leg lengthening was greater in the group of patients under 12 years old (P = 0.005), whereas shortening was not significantly different.
Discussion
Tibial fracture is the second most frequent traumatic paediatric orthopaedic injury requiring hospitalisation, accounting for over 20% of traumatic conditions requiring hospitalisation [2]. Clinical results are good, whichever treatment method is chosen [3, 5, 7, 13–16]. Closed reduction and casting is the mainstay of treatment for diaphyseal tibial fractures [2]. However, this method requires prolonged immobilisation and careful follow-up. Secondary displacement and nonalignment are not exceptional, particularly in cases of isolated tibia facture [17]. In order to avoid these complications, operative treatment can be performed. ESIN is the gold standard for diaphyseal fracture osteosynthesis in children and adolescents [4–6, 13]. In tibial fractures, indications for operative treatment are determined on the basis of a variety of factors including fracture type, location, severity and patient age [4, 5, 7, 13–16, 18, 19]. The good results of ESIN in femur and forearm fractures led us to use this technique to treat tibial shaft fractures [7–9]. In our department, since 2000 every displaced diaphyseal tibial fracture in patents over the age of 6 years was therefore treated by ESIN, apart from Gustilo 2 and 3 open fractures that were treated by external fixation [20]. It is generally recognized that the minimal age for ESIN is 6 years old, apart from polytrauma patients for whom there is no age limit [7]. The mean age of our patients was 11 years and 8 months. We had only one patient under the age of six who sustained polytrauma with a floating knee. Moreover, the fracture types in our study population were similar to those described in the literature [10, 14, 16, 21].
Our study on 86 young patients confirms the efficiency of this technique in the immediate treatment of tibial shaft fractures. The operation duration was short in cases devoid of associated injury (about 15 min, after the learning curve). Most importantly, we evidenced a very low complication rate and the absence of non-union. Radiography analysis shows that 31% (27/86) of initial displacements are reduced postoperatively. A further 10% (9/86) were reduced by D2 as a result of the elasticity of the titanium nails. In cases of persistent frontal angulation, there is a remodelling with a better correction of varus angulation than valgus. It is therefore important to control valgus angulation during surgery. It is noteworthy that only very important initial displacements persisted after 24 months, according to Heinrich and Mooney’s criteria [11]. These findings are in accordance with Gordon’s [21] and Dwyer’s studies [12]. In accordance with O’Brien’s observations [13], our series did not have physeal arrest or proximal tibia growth disturbances. This can be achieved only if the surgical technique is carefully respected, in particular during proximal entry, where special care must be taken not to harm the apophysis of the tibial tubercle in addition to keeping a safe distance from the proximal tibial physis. Great attention must be paid to proper nail balance and rotation to avoid undesirable recurvatum deformity. All of our patients achieved bone union at 6 weeks. This delay is shorter than that described in the literature. In a retrospective review of 60 diaphyseal tibial fractures treated with flexible intramedullary fixation, Gordon [21] achieved 45 bone unions within 18 weeks (average 8 weeks). Furthermore, in their series five patients (11%) had delayed healing, among which 2 required secondary procedures to obtain union (with a mean time to union of 41 weeks). It is noteworthy that patients with delayed healing tended to be older (mean age 14.1 years) versus the study population as a whole (mean age 11.7 years). ESIN provides stable and elastic fixation. Panjabi [22] and Goodship [23] concluded that healed fractures are stronger and more flexible when treated with cyclic compression. Healing by external callus is rapid. This allows early weight bearing with crutches. Moreover, we believe that early weight bearing is a primordial factor in promoting union. This is why we recommend weight bearing on day 15 in transverse fractures, on day 21 in short oblique fractures, on day 30 in long oblique or spiroid fractures and on day 45 in comminuted fractures. The amount of weight bearing is auto-evaluated by the patients themselves according to the pain that it produces. The classical relationship between isolated tibial fracture and non-union [24] was not confirmed in our series. A risk of overgrowth of the fractured tibia exists. In our series, it was greater in children under the age of 12. Premature weight bearing with crutches is also known to prevent overgrowth. This is another reason to fully integrate it in the ESIN technique.
There were four superficial infections (5%) among our patients, and no case of osteomyelitis. These four patients developed infection as a result of nail migration through the skin, requiring modification or nail removal. Gicquel [14] reported a frequency of 20% of infections among his patients; he also described deep infections for Gustilo 2 open fractures. Furthermore, in Gordon’s series [21], one patient with a Gustilo grade 2 open fracture was diagnosed with osteomyelitis at the fracture site after attaining bone union. We did not have this complication because the Gustilo 2 and 3 open fractures were not treated by this method [20]. In our practice, only Gustilo 1 open fractures can be treated with emergency nailing.
Our study also shows the superiority of the ESIN technique over other fixation techniques, such as locking compression plate and percutaneous plating, in terms of postoperative complications. Indeed our series did not have any refracture (vs. 3% in Sommer’s study with locking compression plate [25]), no deep infection (vs. 1% in Sommer’s study [25]), and a shorter time for bone union (6 weeks vs. 13 weeks in Yusof’s study with percutaneous plating [26]).
Conclusion
Our results indicate that the fixation of paediatric diaphyseal tibial fractures with elastic nails is a rapid, well-codified and effective method for treating long-bone closed fractures in children that can be performed by any paediatric orthopaedic surgeon. Advantages over other fixation techniques include a lower infection rate, lower refracture rate, lack of secondary displacement and a greater ease of management for the patients and their parents owing to early mobility and reduced school absenteeism. All of these could compensate for this technique’s greater direct cost.
Acknowlegments
We would like to thank E. Bérard for his help with the statistical analysis and A. Rubio for the English translation.
Contributor Information
Jacques Griffet, Phone: +33-4-76766122, FAX: +33-4-76765218, Email: jgriffet@chu-grenoble.fr.
Julien Leroux, Phone: +33-6-61114701, Email: julien.leroux@chu-rouen.fr.
Ahmad Abou-Daher, Phone: +33-6-87796500.
Toni el Hayek, Phone: +33-4-92036128, FAX: +33-4-92035951, Email: el-hayek.t@chu-nice.fr.
References
- 1.Chotel F, Bérard J, Parot R (2002) Fractures de jambe. In: Clavert J-M, Karger C, Lascombes P, Ligier J-N, Metaizeau J-P (eds) Fractures de l’enfant. Sauramps Medical, Montpellier, France, pp 247–259
- 2.Galano GJ, Vitale MA, Kessler MW, et al. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop. 2005;25:39–44. doi: 10.1097/00004694-200501000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Mashru RP, Herman MJ, Pizzutillo PD. Tibial shaft fractures in children and adolescents. J Am Acad Orthop Surg. 2005;13:345–352. doi: 10.5435/00124635-200509000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Ligier JN, Métaizeau JP, Prévot J. L’embrochage élastique stable à foyer fermé en traumatologie infantile. Chir Pediatr. 1983;24:383–385. [PubMed] [Google Scholar]
- 5.Métaizeau JP, Ligier JN. Le traitement chirurgical des fractures des os longs chez l’enfant. J Chir (Paris) 1984;121:527–537. [PubMed] [Google Scholar]
- 6.Métaizeau JP. Ostéosynthèse chez l’enfant. Ostéosynthèse Centro-Médullaire Elastique Stable. Montpellier: Sauramps Medical; 1988. [Google Scholar]
- 7.Lascombes P, Haumont T, Journeau P. Use and abuse of flexible intramedullary nailing in children and adolescents. J Pediatr Orthop. 2006;26:827–834. doi: 10.1097/01.bpo.0000235397.64783.d6. [DOI] [PubMed] [Google Scholar]
- 8.Lascombes P. Flexible intramedullary nailing in children. Berlin Heidelberg: Springer; 2010. [Google Scholar]
- 9.Griffet J, el Hayek T, Baby M. Intramedullary nailing in forearm fractures in children. J Pediatr Orthop B. 1999;8:88–89. [PubMed] [Google Scholar]
- 10.Gustilo RB, Merkow RL, Templeman D. The management of open fractures. J Bone Joint Surg Am. 1990;72:299–304. [PubMed] [Google Scholar]
- 11.Heinreich SD, Mooney F., III . Fractures of the shaft of the tibia and fibula. In: Rockwood CA, Wilkins KE, editors. Fractures in children. 6. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 1033–1076. [Google Scholar]
- 12.Dwyer AJ, John B, Krishen M, et al. Remodeling of tibial fractures in children younger than 12 years. Orthopedics. 2007;30:393–396. doi: 10.3928/01477447-20070501-13. [DOI] [PubMed] [Google Scholar]
- 13.O’Brien T, Weisman DS, Ronchetti P, et al. Flexible titanium nailing for the treatment of the unstable pediatric tibial fracture. J Pediatr Orthop. 2004;24:601–609. doi: 10.1097/01241398-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Gicquel P, Giacomelli MC, Basic B, et al. Problems of operative and non-operative treatment and healing in tibial fractures. Injury. 2005;36(Suppl 1):A44–A50. doi: 10.1016/j.injury.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 15.Setter KJ, Palomino KE. Pediatric tibia fractures: current concepts. Curr Opin Pediatr. 2006;18:30–35. doi: 10.1097/01.mop.0000192520.48411.fa. [DOI] [PubMed] [Google Scholar]
- 16.Srivastava AK, Mehlman CT, Wall EJ, et al. Elastic stable intramedullary nailing of tibial shaft fractures in children. J Pediatr Orthop. 2008;28:152–158. doi: 10.1097/BPO.0b013e318165210d. [DOI] [PubMed] [Google Scholar]
- 17.Yang JP, Letts RM. Isolated fractures of the tibia with intact fibula in children: a review of 95 patients. J Pediatr Orthop. 1997;17:347–351. [PubMed] [Google Scholar]
- 18.Vallamshetla VR, De Silva U, Bache CE, et al. Flexible intramedullary nails for unstable fractures of the tibia in children. An eight-year experience. J Bone Joint Surg Br. 2006;88:536–540. doi: 10.1302/0301-620X.88B4.17363. [DOI] [PubMed] [Google Scholar]
- 19.Shannak AO. Tibial fractures in children: follow-up study. J Pediatr Orthop. 1988;8:306–310. doi: 10.1097/01241398-198805000-00010. [DOI] [PubMed] [Google Scholar]
- 20.El Hayek T, Abou Daher A, Meouchy W, et al. External fixator in the treatment of fractures in children. J Pediatr Orthop B. 2004;13:103–109. doi: 10.1097/00009957-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Gordon JE, Gregush RV, Schoenecker PL, et al. Complications after titanium elastic nailing of pediatric tibial fractures. J Pediatr Orthop. 2007;27:442–446. doi: 10.1097/01.bpb.0000271333.66019.5c. [DOI] [PubMed] [Google Scholar]
- 22.Panjabi MM, White AA, Wolf JW. A biomechanical comparison of the effects of constant and cyclic compression on fracture healing in rabbit long bones. Acta Orthop Scand. 1979;50:653–661. doi: 10.3109/17453677908991288. [DOI] [PubMed] [Google Scholar]
- 23.Goodship AE, Kenwright J. The influence of induced microenvironment upon the healing of experimental tibial fractures. J Bone Joint Surg Br. 1985;57:650–655. doi: 10.1302/0301-620X.67B4.4030869. [DOI] [PubMed] [Google Scholar]
- 24.Teitz CC, Carter DR, Frankel VH. Problems associated with tibial fractures with intact fibulae. J Bone Joint Surg Am. 1980;62:770–776. [PubMed] [Google Scholar]
- 25.Sommer C, Gautier E, Müller M, Helfet DL, Wagner M. First clinical results of the locking compression plate (LCP) Injury. 2003;34(Suppl 2):43–54. doi: 10.1016/j.injury.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 26.Yusof NM, Oh CW, Oh JK, Kim JW, Min WK, Park IH, Kim HJ. Percutaneous plating in paediatric tibial fractures. Injury. 2009;40:1286–1291. doi: 10.1016/j.injury.2009.02.020. [DOI] [PubMed] [Google Scholar]


