Abstract
Purpose
To report a new locking lateral closing wedge osteotomy used in repairing pediatric supracondylar humerus fracture malunions, which allows for coronal and sagittal plane correction of both cubitus varus and extension.
Methods
At our institution, eight children with cubitus varus resulting from prior supracondylar humerus fracture malunions underwent a new technique of lateral closing wedge osteotomy performed by a single surgeon. Preoperative templating created from radiographs of the bilateral upper extremities were compared with clinical exam to determine the angle of triangular bone that must be removed in order to correct the varus and any extension deformity. A lateral approach and subperiosteal dissection exposed the distal humerus. A transverse osteotomy created a proximal and distal fragment, from which two triangles of bone were removed. The fragments were reunited, parallel lateral pins were placed, and live imaging confirmed stable fixation.
Results
The osteotomy was performed in eight patients, with an average age of 6.3 years. The mean interval between the initial injury and corrective osteotomy was 2.4 years. All patients ended up with flexion of 130° or greater with full and symmetrical pronation and supination. The average ulnohumeral angular correction was 25.5°, which was within 2° of the uninvolved elbow in seven patients and to within 5° in one patient. Baumann’s angle averaged 85.3° preoperatively and 73.7° postoperatively, with an average 70.2° in the uninvolved elbow. All of the patients healed with excellent clinical and radiographic alignment and complete function. There were no complications or revisions.
Conclusion
Varus malunion is a well-described complication of pediatric supracondylar humerus fracture repairs, and many different osteotomy techniques have been described. This series demonstrates that an interlocking lateral wedge osteotomy with parallel lateral pin fixation can provide reliable correction of varus and extension deformity, with a minimal complication rate.
Keywords: Supracondylar humerus fractures, Children, Malunion, Osteotomy
Introduction
The treatment of supracondylar humerus fractures in children continues to be a topic of discussion and controversy. It is the most common elbow fracture in children, with the age of presentation peaking at 5–6 years old. The left or nondominant arm is the most frequently affected. Earlier studies indicated a greater incidence in boys. Studies that are more recent indicate that girls are equalizing the incidence over the past 10 years [1].
Complications of a supracondylar fracture and its treatment have included vascular compromise, compartment syndrome, neurological deficit, elbow stiffness, pin track infections, myositis ossificans, nonunion, osteonecrosis, loss of reduction, hyperextension, and cubitus varus [1]. Cubitus varus, along with malunion, remains the most common complication of type 3 supracondylar humerus fractures, which is when complete displacement occurs with no cortical contact according to the Gartland classification [2]. Modern techniques of repairing supracondylar fractures have significantly reduced the incidence of cubitus varus malunion. Tellisi et al. reported a decrease from a 50% cubitus varus rate of 46 fractures in 1995 treated with manipulative reduction alone to a 6.6% cubitus varus rate of 45 fractures in 2000 treated with percutaneous pinning [3]. However, despite modern orthopedic treatment, malunions continue to occur.
Causes of cubitus varus are now believed to be either supracondylar malunion or trochlear osteonecrosis. The consequences of cubitus varus have included an increased risk of lateral condylar fractures, pain, tardy posterolateral rotatory instability, tardy ulnar nerve palsy, internal rotational malalignment, and poor cosmesis [1]. Historically, treatment for cubitus varus has been considered for cosmetic reasons only [4]. Recent reports, however, show that these other consequences of cubitus varus may also be indications for operative reconstruction [4–12].
Lateral condyle fractures following cubitus varus remain a common complication seen by pediatric orthopedists [5]. Furthermore, cubitus varus is thought to shift the mechanical axis medially and lead to external rotational torque. Chronically present, this torque stretches the lateral collateral ligament, leading to posterolateral rotatory instability [6–10]. Additionally, some children may develop posterior shoulder instability with a Bankart lesion [11]. Finally, subluxation of the ulnar nerve and medial head of the triceps over the medial epicondyle can produce pain, snapping, and paresthesias [7, 10, 12].
Research has identified malunion as the most likely culprit for the greater majority of angular deformities. The accuracy of the initial reduction best predicts the incidence of subsequent deformity [13]. The distal humerus malunion typically includes elements of varus, internal rotation, and hyperextension. Numerous osteotomy techniques for treating this malunion have been described with variable success and variable complication rates. Traditional approaches include French, dome, and wedge osteotomies.
Bellemore et al. reported supracondylar osteotomies on 16 patients using a modified French method. This technique, originally described in 1959 as a lateral closing wedge through a posterior approach [14], uses an intact periosteal hinge medially and two screws with a wire loop laterally to control the distal fragment. Bellemore et al. found this technique to be safe and satisfactory, with no infections or neurovascular complications [15].
Tachdjian initially mentioned the dome osteotomy in 1972 [16], with Higaki and Ikuta later describing the technique more thoroughly [17]. Kanaujia et al. reported dome osteotomies on 11 children to correct varus deformities. This involved a posterolateral approach, the use of Ikuta’s fixation device, and crossing Kirschner wires for fixation. The correction was satisfactory in all of the cases, and there was no serious complication [18].
Various wedge osteotomies have also been reported. Voss et al. and Wong et al. described lateral closing wedge osteotomies through lateral approaches in 36 and 27 patients, respectively [19, 20]. Voss et al. had good correction of the cubitus varus and no nerve palsies or infections, and Wong et al. stated a concern regarding bony prominences over the lateral condyle postoperatively in 14 of their patients. Hui et al. used a medial approach with a lateral closing wedge in 14 cases, with one case of transient ulnar nerve paresis with residual varus [21]. And Koch and Exner used an anteromedial approach and a medial opening wedge with external fixation in four patients with one residual varus deformity [22].
Other described techniques include step-cut, interlocking wedge, and arc osteotomies. DeRosa and Graziano used a step-cut technique of distal humerus valgus osteotomy using one cortical screw for fixation in 11 patients. They found no radial or ulnar nerve injuries, nonunions, infections, or hypertrophic scars. One patient had residual varus [23]. Miura et al. treated 20 patients with an interlocking wedge osteotomy, with only one poor result [24]. Matsushita and Nagano treated 12 patients with an arc osteotomy, and they observed no complications [25].
Options for osteotomy stabilization have included casting alone, internal fixation, and Kirschner pin fixation in the reports described above. Levine et al. used external fixation in five patients. They reported no loss of correction or motion while observing one transient radial neurapraxia, one superficial pin infection, and one keloid [26].
Many osteotomies address only the varus or extension components of the deformity, leading to residual malalignment and, often, disappointing results [27]. Three-dimensional osteotomies address varus, internal rotation, flexion/extension, and lateral translation [28]. A comparative study of 25 patients randomized between the French and dome osteotomies found improved rotational correction using the dome method, but this technique offered significant complications, including inadequate correction, nerve palsy, loss of motion, and circulatory compromise [29].
Some authors report complication rates of over 20% for corrective osteotomies of the distal humerus. Ippolito et al. performed 24 supracondylar osteotomies with six immediate postoperative complications, including ulnar-nerve palsy, hematoma, and circulatory disturbance. After an average follow-up of 23 years, they found that all but two of the patients lost correction, 14 of the patients were dissatisfied with the appearance of the scar, 12 of the patients had measurable atrophy of the affected arm, and 10 of the patients had loss of motion [30]. Oppenheim et al. performed 45 corrective supracondylar osteotomies in 43 children with a 24% complication rate, including neurapraxia, sepsis, and cosmetically unacceptable scarring [31]. With slightly improved results, Labelle et al. reported 33% unsatisfactory results after 15 supracondylar osteotomies [13]. Newer techniques of percutaneous pin fixation vice casting alone and closer postoperative observation for correction of the deformity have decreased the complication rate to less than 15% [32].
Suffice to say, a clear method that achieves long-term deformity correction and complete patient satisfaction while minimizing complications has yet to be fully developed. Toward that goal, we report a new locking lateral closing wedge osteotomy of the distal humerus using a modification of the osteotomy technique described by Wiltse in 1972. Wiltse originally described resecting a triangular segment of distal tibia to treat malalignment of the lower leg [33]. Modifying this procedure for the distal humerus to treat cubitus varus following supracondylar fractures allows for the correction of both varus and extension. Use of the osteotomy described by Wiltse over a simple closing wedge osteotomy offers key advantages. Firstly, this technique avoids a prominence usually present following a simple closing wedge osteotomy, which allows for better cosmesis. Also, the method presented below allows for rotation at the center of the deformity, rather than at the edge of the closing wedge. This should result in improved rotational correction without neurovascular compromise.
Materials and methods
Between 1999 and 2003, eight children with cubitus varus resulting from prior supracondylar humerus fracture malunions underwent a new technique of lateral closing wedge osteotomy performed by a single surgeon. Clinical and radiographic measurements were both used to determine the amount of required correction. Clinically, the patients’ elbow flexion, extension, and cubitus varus were measured on the affected arm and compared to the normal arm. Of particular importance was the difference between the two arms’ carrying angles. The differences were used to establish the angles of bone that must be removed in the coronal and sagittal planes (Fig. 1). Most commonly, the previous malunion led to hyperextension of the elbow, which can be corrected for by angling the new osteotomy. If the elbow extends 20° more than the unaffected side, for example, this cut should be aimed distally 20° from the anterior to the posterior in order to correct the sagittal deformity. Template A, corresponding to Arrow A on Fig. 1, would then be created to angle 20°.
Fig. 1.
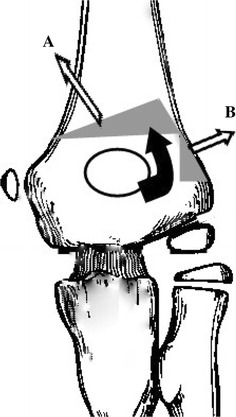
Osteotomy technique. Schematic drawing of osteotomy. The white arrows represent bone that is to be removed, and the solid black arrow represents the direction of rotation of the osteotomy [38]
In addition, preoperative radiographs of the patient’s bilateral upper extremities were analyzed to confirm the angle of triangular bone that must be removed in order to correct the varus and any extension deformity, if necessary (Fig. 2). The clinical and radiographic methods usually predict a very similar amount of required correction, and serve as two independent measurements to verify each other.
Fig. 2.

Preoperative elbow. Preoperative anteroposterior (AP) and lateral radiographs of a supracondylar malunion with templating
The lateral approach was easiest for this operation. A longitudinal incision, measuring approximately 5–6 cm, was made over the lateral distal humerus. The antebrachial cutaneous nerve and its branches were identified and preserved. (This approach should be distal to the radial nerve; however, one may look proximally in the wound to ensure that the radial nerve remains out of harm’s way and not in the field.) Dissection was carried out in the interval between the brachioradialis and triceps muscles. Subperiosteal dissection was performed to expose the distal humerus circumferentially. Posterior dissection distal to the olecranon fossa was avoided to prevent compromising the blood supply to the trochlea. The distal humeral shaft was protected circumferentially with Chandler retractors. With continuous irrigation to prevent the saw blade from overheating, a transverse osteotomy was performed just above the olecranon fossa. This osteotomy should be made parallel to the elbow joint in the coronal plane and perpendicular to the humeral shaft in the sagittal plane. The proximal humerus was then delivered out of the wound to allow for a precise osteotomy with direct visualization. Template A, corresponding to Arrow A on Fig. 1, was placed on the proximal fragment, which defined the triangular wedge of bone to be removed. Care was taken to leave the lateral-most spike of the proximal fragment intact, as this will help lock the distal fragment into place and prevent lateral translation of the distal fragment. This translation would otherwise result in a lateral bump that is cosmetically unappealing. The removal of Template A, as previously explained, obtains the sagittal correction.
A 90° triangle was then removed from the lateral portion of the fragment to create space for the lateral spike of the distal humerus, corresponding to Arrow B of Fig. 1. The humerus was then replaced into the wound, and the proximal and distal fragments are brought together in a lock and key mechanism, corresponding to the black curved arrow of Fig. 1. This insertional method prevents excessive lateral translation of the distal fragment.
Three 0.062-in (2-mm) Kirschner wires, or pins, were then placed across the osteotomy site from lateral to medial (Fig. 3). These pins were left extruding from the skin, with the free ends bent back toward the patient’s arm. A goniometer was used to measure alignment of the carrying angle of the elbow, and elbow flexion and extension were then checked to ensure similarity to the contralateral side. If needed, the pins could have been backed out of the fracture site and the proximal humerus delivered out of the wound for adjustments to the osteotomy with a saw or rongeur. The wound was irrigated, and a small amount of local bone graft from the excised wedge was packed around the osteotomy site. After closure, flexion, extension, and varus/valgus stability were checked under fluoroscopic live imaging to ensure that the osteotomy fixation was stable. A long-arm cast was applied in about 60–70° of flexion, with the arm placed in neutral rotation.
Fig. 3.
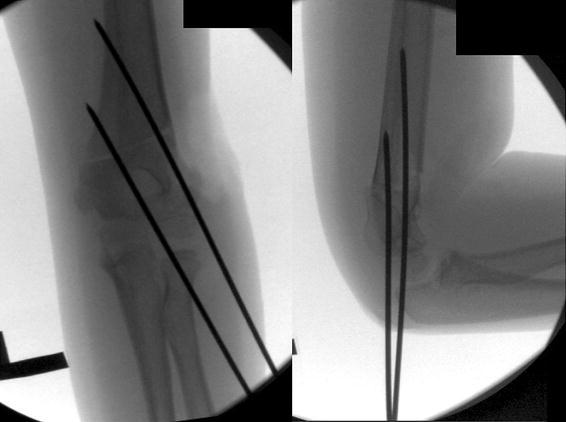
Intraoperative elbow. Intraoperative AP and lateral fluoroscopy with Kirschner wires, demonstrating pin fixation following osteotomy. Though we usually used three Kirschner wires, this patient’s elbow was so stable that only two wires were needed
Postoperatively, the cast and pins were removed approximately 4 weeks later in an outpatient setting after noting callus formation on the radiograph. If this callus had not yet formed, the pins were simply left in for longer. While most children do not require formal physical therapy, we generally teach the parents range of motion exercises to be performed. A follow-up appointment to assess the range of motion is scheduled about 4–6 weeks later, and if motion is not nearly normal at that time, physical therapy to improve elbow motion is commenced.
Results
The osteotomy was performed in eight patients; four males and four females (Table 1). The average age at surgery was 6.3 years (range, 3.2–11.8 years). The mean interval between the initial injury and corrective osteotomy was 2.4 years. The average preoperative flexion–extension motion arc was 125° and the average postoperative motion was 130°. All patients ended up with flexion of 130° or greater, which is commonly accepted as enough flexion for activities of daily living. The three patients with preoperative elbow flexion <100° all improved flexion by 30–40° postoperatively. All patients had full and symmetric pronation and supination preoperatively and postoperatively. One patient, who was lost to follow-up after pin removal, had an anticipated decreased motion in the immediate postoperative period. One other patient was lost to follow-up, for whom postoperative motion was not recorded.
Table 1.
Data for eight patients who underwent the surgical technique for the treatment of supracondylar humerus fracture malunions for this study
| Age (years), gender | Preop. affected elbow ROMa | Postop. affected elbow ROM | UHA preop. (varus) | UHA postop. (valgus) | UHA change | UHA contralateral (valgus) | Difference of UHA postop. from UHA contralateral | |
|---|---|---|---|---|---|---|---|---|
| 1 | 3.3, male | 5–90 | 0–130 | 12 | 10 | 22 | 9 | 1 |
| 2 | 3.3, female | −10–100 | −9–130 | 22 | −2 | 20 | 3 | 5 |
| 3 | 5.8, female | −10–120 | −10–135 | 18 | 10 | 28 | 10 | 0 |
| 4 | 6.1, male | −20–100 | 0–140 | 13 | 4 | 17 | 5 | 1 |
| 5 | 6.3, female | 5–140 | 10–140 | 27 | 10 | 37 | 10 | 0 |
| 6 | 7.0, female | −21–120 | –* | 21 | 14 | 35 | 15 | 1 |
| 7 | 8.0, male | 0–140 | –b | 23 | 6 | 29 | 6 | 0 |
| 8 | 11.8, male | 0–140 | −5–140 | 14 | 2 | 16 | 4 | 2 |
ROM range of motion, UHA ulnohumeral angle
* Data not recorded
aNegative extension indicates hyperextension
bLost to follow-up after pin removal
The ulnohumeral angle and Baumann’s angle were measured pre- and postoperatively. The average ulnohumeral angle was 18.7° of varus preoperatively (range, 12–27°), and an average of 6.8° of valgus postoperatively (range, −2 to 15°). The average angular correction was 25.5° (range, 17–37°). The average contralateral ulnohumeral angle was 7.7° of valgus, so the ulnohumeral angle was restored to within 2° of that of the uninvolved elbow in seven patients and to within 5° in one patient. Baumann’s angle averaged 85.3° (range, 69–90°) preoperatively in the involved elbow and 73.7° postoperatively. Baumann’s angle averaged 70.2° in the uninvolved elbow. A sample preoperative radiograph is shown in Fig. 2, with postoperative follow-up films of the same patient shown in Fig. 4.
Fig. 4.

Postoperative elbow. Postoperative AP and lateral radiographs 4 months following surgery
One patient was noted to have slight malrotation preoperatively, but had 90° of both internal and external shoulder rotation with good function. Therefore, the rotation was not changed. No other patients were noted to have significant rotational deformities.
There were no complications, and the patients required no operative revisions. None of the patients had any symptoms of a tardy ulnar nerve palsy. All patients were satisfied with the cosmetic and functional results of the surgery. Indications for the surgery were pain in the affected arm and family and patient unhappiness with the deformity.
Discussion
The treatment of supracondylar humerus fractures in children continues to be controversial. Complications of a supracondylar fracture and its treatment have included vascular compromise, compartment syndrome, neurological deficit, elbow stiffness, pin track infections, myositis ossificans, nonunion, osteonecrosis, loss of reduction, hyperextension, and cubitus varus. Despite modern treatment techniques, cubitus varus remains a complication of type 3 supracondylar humerus fractures. The consequences of cubitus varus and indications for surgery have included an increased risk of lateral condylar fractures, pain, tardy posterolateral rotatory instability, tardy ulnar nerve palsy, internal rotational malalignment, and poor cosmesis.
Malunion is the most likely culprit for the greater majority of angular deformities, not growth disturbance, as there is very little growth in the distal humerus, and the deformity is present at the time of healing. The accuracy of the initial reduction best predicts the incidence of subsequent deformity. The distal humerus malunion typically includes elements of varus, internal rotation, and hyperextension. Numerous osteotomy techniques for treating this malunion have been described with variable success and variable complication rates. These approaches include French, dome, and wedge osteotomies, as well as step-cut, interlocking wedge, and arc osteotomies. Options for osteotomy stabilization have included casting alone, internal fixation, Kirschner pin fixation, and external fixation.
Here, we report a new locking osteotomy of the distal humerus similar to the osteotomy technique described by Wiltse for the distal tibia. This procedure allowed for the correction of both varus and extension with no complications in eight patients.
A somewhat similar technique with a step-cut translation osteotomy was described in 2005 by Kim et al. in 19 cases of cubitus varus. They used a similar wedge osteotomy, and stabilized their construct with a Y-shaped humeral plate. All patients had good alignment and the desired range of motion. One patient had a tardy ulnar nerve palsy, and another patient had considerable scarring [34]. Another case series of 22 children was reported by Yun et al. in 2007 using a similar osteotomy, which had generally excellent results and two complications. One patient had an undisplaced fracture intraoperatively that healed satisfactorily, and another patient had a tardy ulnar nerve palsy [35]. The interlocking Wiltse-type technique provides intrinsic stability that allows secure fixation with pins alone, and leaves the patient with no hardware after the pins are removed.
It has been previously reported that well-placed parallel lateral pins provide secure fixation for acute supracondylar humerus fractures. Skaggs et al. reviewed 345 extension-type supracondylar fractures in children and found that fixation with only lateral pins is safe and effective for both Gartland type 2 and type 3 supracondylar fractures of the humerus in children [36]. In a separate study, Skaggs et al. reviewed 124 consecutive displaced supracondylar humeral fractures in children fixed with only lateral entry pins. Avoiding selection bias, they found that lateral entry pins alone were effective for even the most unstable supracondylar humeral fractures. Fixation was maintained in all cases, and there were no nerve palsies [37].
This series demonstrates that an interlocking lateral wedge osteotomy with lateral pin fixation can provide reliable correction of varus and extension with a low complication rate. This osteotomy has several advantages. It reliably corrects both varus and extension deformities without the presence of a lateral bump. Its stability and security is enhanced by a Wiltse-type locking cut. The lateral approach and lateral pins ensure protection for the ulnar nerve, and the complication rate is low. We recommend this technique for the treatment of supracondylar humerus fracture malunions in children.
Acknowledgments
Conflict of interest
None of the authors received financial support for this study.
References
- 1.Beaty JH, Kasser JR, editors. Rockwood and Wilkins’ fractures in children. 7. Philadelphia: Lippincott Williams & Wilkins; 2010. pp. 488–532. [Google Scholar]
- 2.Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;109:145–154. [PubMed] [Google Scholar]
- 3.Tellisi N, Abusetta G, Day M, et al. Management of Gartland’s type III supracondylar fractures of the humerus in children: the role audit and practice guidelines. Injury. 2004;35:1167–1171. doi: 10.1016/j.injury.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997;5:19–26. doi: 10.5435/00124635-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Davids JR, Maguire MF, Mubarak SJ, et al. Lateral condylar fracture of the humerus following posttraumatic cubitus varus. J Pediatr Orthop. 1994;14:466–470. doi: 10.1097/01241398-199407000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Abe M, Ishizu T, Morikawa J. Posterolateral rotatory instability of the elbow after posttraumatic cubitus varus. J Shoulder Elbow Surg. 1997;6:405–409. doi: 10.1016/S1058-2746(97)90011-2. [DOI] [PubMed] [Google Scholar]
- 7.Abe M, Ishizu T, Shirai H, et al. Tardy ulnar nerve palsy caused by cubitus varus deformity. J Hand Surg Am. 1995;20:5–9. doi: 10.1016/S0363-5023(05)80047-4. [DOI] [PubMed] [Google Scholar]
- 8.Beuerlein MJ, Reid JT, Schemitsch EH, et al. Effect of distal humeral varus deformity on strain in the lateral ulnar collateral ligament and ulnohumeral joint stability. J Bone Joint Surg Am. 2004;86:2235–2242. doi: 10.2106/00004623-200410000-00015. [DOI] [PubMed] [Google Scholar]
- 9.O’Driscoll SW, Spinner RJ, McKee MD, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg Am. 2001;83:1358–1369. doi: 10.2106/00004623-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Spinner RJ, Goldner RD. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J Bone Joint Surg Am. 1998;80:239–247. doi: 10.2106/00004623-199802000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Gurkan I, Bayrakci K, Tasbas B, et al. Posterior instability of the shoulder after supracondylar fractures recovered with cubitus varus deformity. J Pediatr Orthop. 2002;22:198–202. [PubMed] [Google Scholar]
- 12.Spinner RJ, O’Driscoll SW, Davids JR, et al. Cubitus varus associated with dislocation of both the medial portion of the triceps and the ulnar nerve. J Hand Surg Am. 1999;24:718–726. doi: 10.1053/jhsu.1999.0718. [DOI] [PubMed] [Google Scholar]
- 13.Labelle H, Bunnell WP, Duhaime M, et al. Cubitus varus deformity following supracondylar fractures of the humerus in children. J Pediatr Orthop. 1982;2:539–546. doi: 10.1097/01241398-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 14.French PR. Varus deformity of the elbow following supracondylar fractures of the humerus in children. Lancet. 1959;2:439–441. doi: 10.1016/S0140-6736(59)90422-2. [DOI] [PubMed] [Google Scholar]
- 15.Bellemore MC, Barrett IR, Middleton RW, et al. Supracondylar osteotomy of the humerus for correction of cubitus varus. J Bone Joint Surg Br. 1984;66:566–572. doi: 10.1302/0301-620X.66B4.6746695. [DOI] [PubMed] [Google Scholar]
- 16.Tachdjian MO. Pediatric orthopedics. Philadelphia: W.B. Saunders Co.; 1972. pp. 1566–1585. [Google Scholar]
- 17.Higaki T, Ikuta Y. The new operation method of the domed osteotomy for 4 children with varus deformity of the elbow joint. J Jap Ortho. 1982;31:30–35. [Google Scholar]
- 18.Kanaujia RR, Ikuta Y, Muneshige H, et al. Dome osteotomy for cubitus varus in children. Acta Orthop Scand. 1988;59:314–317. doi: 10.3109/17453678809149371. [DOI] [PubMed] [Google Scholar]
- 19.Voss FR, Kasser JR, Trepman E, et al. Uniplanar supracondylar humeral osteotomy with preset Kirschner wires for posttraumatic cubitus varus. J Pediatr Orthop. 1994;14:471–478. doi: 10.1097/01241398-199407000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Wong HK, Lee EH, Balasubramaniam P. The lateral condylar prominence. A complication of supracondylar osteotomy for cubitus varus. J Bone Joint Surg Br. 1990;72:859–861. doi: 10.1302/0301-620X.72B5.2211772. [DOI] [PubMed] [Google Scholar]
- 21.Hui JH, Torode IP, Chatterjee A. Medial approach for corrective osteotomy of cubitus varus: a cosmetic incision. J Pediatr Orthop. 2004;24:477–481. doi: 10.1097/01241398-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Koch PP, Exner GU. Supracondylar medial open wedge osteotomy with external fixation for cubitus varus deformity. J Pediatr Orthop B. 2003;12:116–122. doi: 10.1097/01.bpb.0000049571.52224.c8. [DOI] [PubMed] [Google Scholar]
- 23.DeRosa GP, Graziano GP. A new osteotomy for cubitus varus. Clin Orthop Relat Res. 1988;236:160–165. [PubMed] [Google Scholar]
- 24.Miura H, Tsumura H, Kubota H, et al. Interlocking wedge osteotomy for cubitus varus deformity. Fukuoka Igaku Zasshi. 1998;89:119–125. [PubMed] [Google Scholar]
- 25.Matsushita T, Nagano A. Arc osteotomy of the humerus to correct cubitus varus. Clin Orthop Relat Res. 1997;336:111–115. doi: 10.1097/00003086-199703000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Levine MJ, Horn BD, Pizzutillo PD. Treatment of posttraumatic cubitus varus in the pediatric population with humeral osteotomy and external fixation. J Pediatr Orthop. 1996;16:597–601. doi: 10.1097/01241398-199609000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Usui M, Ishii S, Miyano S, et al. Three-dimensional corrective osteotomy for treatment of cubitus varus after supracondylar fracture of the humerus in children. J Shoulder Elbow Surg. 1995;4:17–22. doi: 10.1016/S1058-2746(10)80003-5. [DOI] [PubMed] [Google Scholar]
- 28.Chung MS, Baek GH. Three-dimensional corrective osteotomy for cubitus varus in adults. J Shoulder Elbow Surg. 2003;12:472–475. doi: 10.1016/S1058-2746(03)00090-9. [DOI] [PubMed] [Google Scholar]
- 29.Kumar K, Sharma VK, Sharma R, et al. Correction of cubitus varus by French or dome osteotomy: a comparative study. J Trauma. 2000;49:717–721. doi: 10.1097/00005373-200010000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Ippolito E, Moneta MR, D’Arrigo C. Post-traumatic cubitus varus. Long-term follow-up of corrective supracondylar humeral osteotomy in children. J Bone Joint Surg Am. 1990;72:757–765. [PubMed] [Google Scholar]
- 31.Oppenheim WL, Clader TJ, Smith C, et al. Supracondylar humeral osteotomy for traumatic childhood cubitus varus deformity. Clin Orthop Relat Res. 1984;188:34–39. [PubMed] [Google Scholar]
- 32.Wilkins KE. Supracondylar fractures: what’s new? J Pediatr Orthop B. 1997;6:110–116. doi: 10.1097/01202412-199704000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Wiltse LL. Valgus deformity of the ankle: a sequel to acquired or congenital abnormalities of the fibula. J Bone Joint Surg Am. 1972;54:595–606. [PubMed] [Google Scholar]
- 34.Kim HT, Lee JS, Yoo CI. Management of cubitus varus and valgus. J Bone Joint Surg Am. 2005;87:771–780. doi: 10.2106/JBJS.D.01870. [DOI] [PubMed] [Google Scholar]
- 35.Yun YH, Shin SJ, Moon JG, et al. Reverse V osteotomy of the distal humerus for the correction of cubitus varus. J Bone Joint Surg Br. 2007;89:527–531. doi: 10.1302/0301-620X.89B4.18509. [DOI] [PubMed] [Google Scholar]
- 36.Skaggs DL, Hale JM, Bassett J, et al. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;83:735–740. [PubMed] [Google Scholar]
- 37.Skaggs DL, Cluck MW, Mostofi A, et al. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86:702–707. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Weiss JM, Kay RM, Waters P, et al. Distal humerus osteotomy for supracondylar fracture malunion in children: a study of perioperative complications. Am J Orthop. 2010;39:22–25. [PubMed] [Google Scholar]


