Abstract
Background Depression is a major cause of disability, particularly among women; poverty heightens the risk for depression. Beyond its direct effects, maternal depression can harm children’s health and development. This study aimed to assess the effects of a large-scale anti-poverty programme in Mexico (Oportunidades) on maternal depressive symptoms.
Methods In 2003, 5050 women living in rural communities who had participated in Oportunidades since its inception were assessed and compared with a group of 1293 women from matched communities, whose families had received no exposure to Oportunidades at the time of assessment but were later enrolled. Self-reported depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D). Ordinary least squares regressions were used to evaluate the treatment effect of programme participation on depression while adjusting for covariates and clustering at the community level.
Results Women in the treatment group had lower depressive symptoms than those in the comparison group (unadjusted mean CES-D scores: 16.9 ± 9.8 vs 18.6 ± 10.2). In multivariable analyses, programme participation was associated with lower depression whilst controlling for maternal age, education and household demographic, ethnicity and socio-economic variables [β = −1.7 points, 95% confidence interval (95% CI) −2.46 to −0.96, P < 0.001]. Reductions in perceived stress and increases in perceived control were mediators of programme effects on women.
Conclusions Although Oportunidades did not target maternal mental health directly, we found modest but clinically meaningful effects on depressive symptoms. Our design permits stronger causal inference than observational studies that have linked poverty and depressive symptoms. Our results emphasize that the well-being of individuals is responsive to macro-level economic policies and programmes.
Keywords: Maternal depression, poverty, Mexico
Introduction
Depression is common and is associated with serious impairment and disability worldwide.1,2 The majority of research on depression has been conducted in high-income countries; however, there is accumulating evidence that the prevalence of depression is high among the poor and in poor countries.3–5 Extensive research over the past several decades demonstrates that women are roughly twice as likely to experience depression as men.6 This gender disparity emerges in adolescence and is most prominent during the childbearing years.7,8
Maternal depression is doubly concerning due to its effects not only on the women who suffer from it, but also because of its impact on family functioning and child development. Women are typically the primary caregivers of children; symptoms of depression such as depressed mood, irritability, disrupted sleep, low energy and hopelessness can clearly impair mothers’ capacities to nurture and interact with their children. A growing literature demonstrates that maternal depression is associated with poorer development of children cognitively and physically.9–12
Whereas there has been increasing empirical research regarding the assessment and prevention of maternal depression in high-income countries,13 greater attention to this problem is needed in low- and middle-income countries.5,14 Of the estimated 2.2 billion children in the world, 1.9 billion are growing up in developing countries with 1 billion of those in poverty.15 Multiple studies conducted in low- and middle-income countries demonstrate high rates of depression during pregnancy and during the post-partum period.16 Given the extreme demands involved in raising healthy children in contexts of severe poverty—e.g. seeking to provide adequate nutrition and shelter and prevent disease in resource-poor settings—it has been argued that maternal depression is an even greater concern in the developing world where children are particularly vulnerable to health and safety risks.3,17,18
A large body of psychological research has demonstrated that a major psycho-social risk factor for depression is exposure to stressors that cannot be adequately managed with existing resources. According to the empirically supported transactional model of stress and coping, psychological stress is viewed as mediated by the person’s assessment of the type and controllability of the stressor and the resources available to respond to the stressor.19 For mothers in low- and middle-income countries, the experiencing of economic demands without adequate economic resources would be expected to serve as a source of psychological stress. Reviews of the literature provide evidence for an association between lower socio-economic status (SES) and increased levels of psychological disorders in a range of low- and middle-income countries, with the most consistent pattern found for lower levels of education.5,18,20 Studies of the relationship between SES and maternal mental health have primarily relied on cross-sectional designs; thus, it is difficult to determine the causal direction of effects.
Can decreases in poverty help alleviate maternal depression? Recent experimental and quasi-experimental studies conducted in the USA have found mixed effects of welfare to work and housing voucher programmes on maternal mental health.21 The rapid growth of conditional cash transfer (CCT) poverty reduction programmes for extremely poor families in dozens of low- and middle-income countries since the mid-1990s provides a key context for rigorous investigation of this question. CCT programmes generally involve the government’s provision of income supplements to poor families contingent on their adherence to activities that are expected to promote healthier child development. Evaluation results of CCT programmes from Brazil, Mexico, Argentina and Nicaragua show that CCT programmes raise household consumption; increase school enrolment rates; improve health conditions in children such as anaemia and stunting and are linked with lower behavioural problems for children.22–25 Across countries, mothers typically are the beneficiaries of additional cash transfers from the government, the strategic assumption being that mothers will be more involved in child welfare.26 Thus, although the intended outcomes of these human capital investment programmes are for ‘children’, their mothers are the conduits by which these programmes are implemented.
To what extent does participating in a CCT programme improve the mental health of mothers, even though the mental or physical health of mothers is not targeted by the intervention? Although we could not identify any published, peer-reviewed papers on this question, two working papers by the World Bank reported on the experimental effects of government cash transfer programmes on maternal depression among very poor families in Ecuador and Nicaragua: in Ecuador, there were no effects for women who had received non-conditional (i.e. not contingent on any behaviours on the part of the family) income supplements for 17 months27 and the Nicaraguan study found a ‘borderline’ significant effect on maternal depression after 9 months of conditional cash transfers.28 In Ecuador and Nicaragua, the income supplement was equivalent to 10–15% of the family’s monthly income.
The present study further addresses this question regarding the effects on maternal depression of one of the largest and earliest CCT programmes in Latin America, the Oportunidades programme implemented by the Mexican government. Oportunidades (originally Progresa) began in 1997 with an initial roll-out in rural areas with an extension to urban areas. By 2004, 5 million families in all 31 states of Mexico had enrolled in Oportunidades. To provide a context for understanding the poverty levels addressed by the programme, the average hourly wage for rural Mexicans who work in agriculture is 7 pesos (roughly equivalent to US$0.09 or €0.07).29 The income supplementation provided by Oportunidades was ∼25% of household income. Mothers whose families participated in Oportunidades received benefits only when family members complied with required activities, including pre-natal care, nutrition monitoring and supplementation, well infant care and immunization, preventive checkups and participation in educational workshops. Participation was monitored on a regular basis.30 Systematic evaluation of the Oportunidades programme has demonstrated beneficial effects on child health, including physical growth, fewer sick days, cognitive development and behavioural problems.22,24,31 Women participating in the present study had received income supplementation for between 3.5 and 5 years; this time frame allows for more opportunity for potential effects on maternal mental health to be realized than in the prior evaluations conducted in Ecuador and Nicaragua. In addition, the 25% income supplement studied here for the Mexican programme represented a more substantial and potentially more psychologically impactful alleviation of the family’s level of extreme poverty.
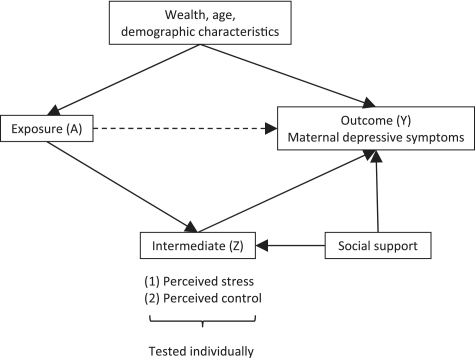
Prior cross-sectional research with women participating in Oportunidades identified perceived stress and perceived control as the strongest predictors of depressive symptoms.32 Although the improvement of maternal mental health was not an explicit focus of Oportunidades, we believe that it is plausible and consistent with the large literature on stress and coping to hypothesize that this programme aimed at relieving poverty and improving child health could exert a non-trivial side effect on maternal depression. Oportunidades may meaningfully reduce economic stress for women, reduce some stress related to the health problems and poor development of their children and increase their perception of control over their lives. Thus, we further expected that reductions in perceived stress and increases in perceived control might mediate the effects of participation in Oportunidades on maternal depression. Our model for the potential mediators of programme effects is displayed in Figure 1. Since inadequate social support could serve as a cause of both higher perceived stress and depression, we also include social support in our mediation model.
Figure 1.
Diagram of mediation relationships
Methods
Design and sampling
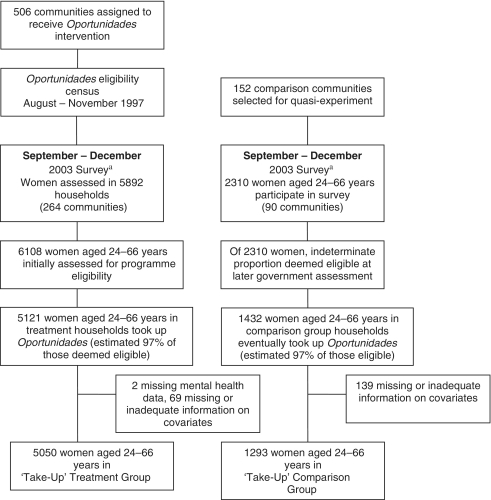
Treatment sample
The treatment sample consisted of 5121 women from 506 poor rural communities whose households had been receiving Oportunidades benefits for 3.5–5 years.33 The programme selected these communities in 1997 based on the proportion of households in communities living in poverty using data from the 1995 National Census. Within the communities assigned to the programme, households were then deemed eligible for participation in Oportunidades according to an index of objective characteristics, such as housing materials, water and sanitation facilities, education and family structure, which were shown to be good proxies for annual income.34 On average, 78% of the households in selected communities were classified as eligible for programme benefits and 97% of these households enrolled in the programme.33 Please see Figure 2 for details regarding the design and sample.
Figure 2.
Flow chart of participants. aCommunities only included in 2003 survey if they included at least ten children <5 years
Eligible households in the treatment group began receiving programme benefits between April 1998 and November 1999, conditional on meeting the Oportunidades programme requirements. Oportunidades beneficiary families received cash transfers every 2 months, equivalent to an increase of ∼25% of household income. The sample of communities was representative of the Oportunidades rural (less than 2500 inhabitants) beneficiary communities and the families were the poorest 20% of the population with daily per capita income of US$ 2 or less in seven Mexican states.
Comparison sample of communities
In 2003, the government added a comparison group of 152 communities as part of the 5-year evaluation of Oportunidades. Substantial care was taken in selection of communities to minimize selection bias.35 The criteria used for the selection of communities into the original treatment groups were fully documented, and all communities were motivated to participate in Oportunidades. Data from the 2000 census were used to select and match new comparison communities that were: (i) from the same state as the original community, in all but one case; (ii) had not yet been incorporated into Oportunidades; and (iii) most closely matched the original using propensity score methods applied to socio-demographic and infrastructure characteristics.36
Comparison sample of women
After selecting the new communities for the comparison group, the government evaluators identified very poor families within those communities to be assessed for possible inclusion in a quasi-experimental control group. This family sampling plan capitalized on the opportunity to assess a large range of economic, health and psycho-social indicators among very poor families who might eventually be deemed eligible for Oportunidades and offered the programme. The evaluators did not know or have control over who would be considered eligible or be offered Oportunidades by the government officials responsible for those activities. Thus, inclusion in the evaluation studied here did not bear on the likelihood of being included in the programme. A total of 2310 women from these very poor families were interviewed in the 2003 assessment in the quasi-experimental comparison communities (total comparison sample). Of these, 1432 were eventually deemed eligible by the Oportunidades programme and took up the programme but only at least a year after their participation in the research described in the present study. Administrative data for the Oportunidades programme indicate an overall take-up rate of 97% for those offered the programme. Thus, we interpret the difference in numbers between the 2310 comparison women who were interviewed and the 1432 in our take-up comparison sample as primarily a gap in eligibility, not a gap in take-up of the conditional cash transfer programme.
In order to test the treatment effect for women who were beneficiaries vs non-beneficiaries of the Oportunidades programme, we identified the subsample of treatment (n = 5121) and control (n = 1432) women who all met the eligibility requirements and eventually enrolled (∼97% of those eligible in the treatment group). For clarity, those who were eligible and eventually enrolled are referred to as the ‘take-up’ treatment and comparison samples. Again, the control sample enrolled only after the research was complete. This approach minimized selection biases associated with programme take-up; this is a key strength of this analysis in light of extensive prior research indicating that people who take up and adhere to social and health programmes can differ meaningfully from those who do not.37 Observations lacking necessary data (i.e. age or education) further reduced our sample size to 6343 observations.
Total sample analysis
To address concerns regarding selection bias in terms of programme take-up/eligibility, we also conducted a second analysis with less-restricted samples, using all women from the treatment (n = 6108) and comparison (n = 2310) conditions. As described above, this total sample includes a large proportion of comparison women who participated in the 2003 interview but were not deemed eligible for treatment, were not offered treatment and did not receive treatment. Observations lacking necessary data further reduced the total sample size to 8260 observations.
Data collection and measures
Data for the psycho-social measures were gathered in 2003 via home interviews conducted in Spanish by teams of trained nurses from Mexico’s National Institute of Public Health (INSP); indigenous language translation was provided as needed for a small proportion of interviews. Interviewers believed that they were conducting a health and development assessment and were blind to the aims and hypotheses of the study; none of the questions pertained to participation in Oportunidades. Only mothers/guardians with at least one child aged 0–5 years were interviewed for maternal psycho-social characteristics. The assessment extended beyond the maternal characteristics presented here to development outcomes for the children aged 5 years living in the household reported elsewhere.24,38 Focus groups and cognitive testing ensured that the interpretation of the interview questions matched the original intent in English.
Maternal psycho-social measures
The primary outcome of interest was maternal depressive symptoms and was measured using the Spanish version of the CES-D (Center for Epidemiologic Studies-Depression Scale), a 20-item questionnaire with a range from 0 to 60 (internal consistency, α = 0.83). 39 Items assess the frequency of symptoms during the past week, including depressed mood, loss of interest and/or pleasure in activities, fatigue, sleep and appetite disturbances. The CES-D has been validated for use in diverse Mexican populations.40,41 We examined outcomes with respect to the total score on the 20-item measure as well as subscale scores for depressive symptoms, (lack of) positive affect, somatic symptoms and interpersonal relations. A total score of 16 has frequently been used as the cut-off indicating clinical levels of distress in the USA; research in Mexico suggests that a higher cut-off score (e.g. in 24–30 range) is more culturally appropriate for identifying clinical levels of depressive symptoms.41
The sum of Cohen et al.’s42 Perceived Stress Scale was used to assess the frequency of stressful situations and feelings of stress in the previous month using a 4-point Likert response format and with a range from 0 to 18 (α = 0.63). Sample items include: ‘… how often have you felt that things were going your way?’ This measure was designed for use with community samples and a Spanish-language version has been validated.43 Mothers’ reported sense of control during the previous week was assessed using the sum of Pearlin et al.’s44 7-item personal mastery scale (α = 0.61). Sample items include ‘I have little control over the things that happen in my life.’
Maternal social support (α = 0.62) was assessed with a 5-item Likert scale adapted from the Coronary Artery Risk Development in Young Adults (CARDIA) studies; the range of scores was 5–25.45 Sample items include ‘How often do members of your family and friends criticize you?’
Demographic and other household-level control variables
Demographic, educational and economic variables were obtained via interview with the head of household or spouse and are shown in Table 1 for our take-up samples. Household-level variables pertained to characteristics of the family and household at baseline (1997/1998). Data from baseline were available for women from treatment communities because it had been collected in a baseline questionnaire in 1997. To obtain this information from comparison communities, an additional questionnaire was used in 2003, which asked comparison families retrospectively about easily-recallable household demographic structure and ownership of assets in 1997/1998. Household-level information included whether an indigenous language was spoken or understood by any member of the household, the occupation of the head of household, crowding in the household, ratio of wage earners to dependents, presence of electricity and water in the household, dwelling characteristics, number of small and draught animals owned and household assets. Principal components analysis was used to consolidate the wealth and occupation variables into a wealth index (first component retained from household asset and dwelling indicators) and two occupational indices (first and second components retained from occupation, farming indicators and education of head of household). In cases with missing household information (∼18% of households), values were imputed using the mean for the community. Indicator variables for state were included in all models.
Table 1.
Comparison of ‘take-up’ sample characteristics by treatment status
| Control | Treatment | P-valueb | |
|---|---|---|---|
| Respondent characteristics | n (%)a | n (%)a | |
| Total respondents | 1293 (100.0) | 5050 (100.0) | |
| Age (years), mean (SD) | 36.9 (9.6) | 37.3 (9.6) | 0.46 |
| Education | 0.54 | ||
| Preschool or less | 233 (18.0) | 1076 (21.3) | |
| Primary | 916 (70.8) | 3388 (67.1) | |
| Secondary or more | 144 (11.1) | 586 (11.6) | |
| Is head of household | 103 (8.0) | 426 (8.4) | 0.72 |
| 1997 household characteristics | |||
| Head of household is indigenous | 278 (21.5) | 1913 (37.9) | 0.052 |
| Head of household occupation | 0.088 | ||
| Field labourer | 655 (54.1) | 2040 (51.2) | |
| Non-agricultural worker | 165 (13.6) | 401 (10.1) | |
| Self-employed | 158 (13.1) | 524 (13.2) | |
| Communal land holder | 64 (5.3) | 539 (13.5) | |
| Other | 168 (13.9) | 478 (12.0) | |
| Number of people/number of rooms in house, mean (SD) | 4.26 (2.0) | 4.32 (2.0) | 0.77 |
| Number of non-workers/number of wage earners, mean (SD) | 1.76 (1.3) | 2.15 (1.3) | 0.0003 |
| Owns draught animals | 281 (21.7) | 1933 (38.3) | 0.0011 |
| Owns animals to sell | 743 (57.5) | 4310 (85.4) | <0.001 |
| Dwelling has dirt floor | 894 (69.1) | 3079 (61.0) | 0.15 |
| Water available on land | 644 (49.8) | 2086 (41.3) | 0.27 |
| Dwelling has electricity | 961 (74.3) | 4016 (79.5) | 0.37 |
| Has fridge | 108 (8.35) | 551 (10.9) | 0.31 |
| Has radio | 623 (48.2) | 3434 (68.0) | <0.001 |
| Has TV | 431 (33.3) | 2629 (52.1) | 0.0012 |
| Wealth indexc, mean (SD) | −0.39 (1.8) | 0.12 (1.9) | 0.036 |
| Occupation index 1d, mean (SD) | −0.41 (1.5) | 0.11 (1.3) | 0.0004 |
| Occupation index 2d, mean (SD) | −0.07 (1.4) | 0.03 (1.3) | 0.50 |
| State | <0.001 | ||
| Guerrero | 104 (8.0) | 607 (12.0) | |
| Hidalgo | 81 (6.3) | 694 (13.7) | |
| Michoacan | 169 (13.1) | 525 (10.4) | |
| Puebla | 171 (13.2) | 744 (14.7) | |
| Queretaro | 60 (4.6) | 211 (4.2) | |
| San Luis Potosi | 255 (19.7) | 1017 (20.1) | |
| Veracruz | 453 (35.0) | 1252 (24.8) |
aData are given as number (percentage) of respondents, except where otherwise indicated.
bP-values are from cluster-adjusted t-test (continuous variables) or chi-squared (dichotomous variables) tests of independence.
cComposed using principal components analysis (PCA) from the following components: baseline (1997) household ownership of a blender, fridge, gas stove, boiler, radio, stereo, TV, video, washer, fan, car and van and dwelling characteristics of having a dirt floor, water available on land, electricity and a bathroom. For the analysis reported here, the first principal component was retained and included in subsequent analyses.
dTwo orthogonal occupation indices were created using PCA from the following components: baseline (1997) head of household’s occupation, education and receipt of social security, household land ownership and number of small and draught animals owned.
Data analysis
We conducted our statistical analyses using STATA 10.1 for Windows (STATA Corporation, College Station, TX, USA). In cases with partially missing item responses in a psycho-social scale for a given individual, values were imputed using the mean of the non-missing responses for that individual. A maximum of 20% of missing items were imputed for any of the scales; ∼4% had some imputation of the depressive symptom scale. We analysed the continuous CES-D measure using multivariable, linear, ordinary least squares regression, regressing a symptom score on our independent variable of interest (Oportunidades participation) and the control variables described in Table 1. Standard errors were adjusted for clustering at the community level. Possible interaction effects for age, gender and ethnicity were each examined as the last step in the regressions. For an additional estimate of the clinical significance of our findings, and as a robustness check of the effect of the programme on depression, Poisson regression with robust standard errors was used with a dichotomous CES-D outcome to obtain relative risk (RR) estimates.46 Logistic regression was not used to estimate the odds ratio because the odds ratio is an over-estimate of the risk in a population with a large proportion of cases (>10%).47
Mediation of the programme treatment effect on depressive symptoms (by perceived stress or perceived control) was calculated using the Sobel test,48 which determines if there is a significant indirect effect of the mediator by testing the hypothesis that there is no significant difference between the total effect (direct plus indirect effects) and the direct effect. The first assumption inherent in our mediation analysis is that there is no unmeasured confounding between exposure to treatment and maternal depressive symptoms; we control for extensive economic, educational and demographic factors related to assignment to treatment and the outcome. Our second assumption is that there is no unmeasured confounding between the mediators (perceived stress and perceived control) and maternal depressive symptoms; we control for maternal social support, which may serve as a confounder potentially related to both mediators and the outcome of maternal depressive symptoms. We assess sensitivity to this no-confounding assumption using sensitivity analysis.49 Our third assumption is that our model specification is correct and there are no significant interactions between the mediator and our exposure on the outcome.50 We found no significant interaction between exposure and either of the mediators and these were thus not included in the final models. Standardized regression coefficients were used to calculate the Sobel test statistic. Confidence intervals for the indirect effect were obtained by using the ‘sggmediation’ command in Stata with bootstrapping 1000 repetitions.
Results
Socio-demographic characteristics of the respondent and the household by treatment status are shown in Table 1. The women in the take-up sample were not statistically different from the treatment group for age, education or status as head of household. There were no statistically significant differences between household indicators of poverty such as crowding, having a dirt floor, water available on land and electricity. The take-up treatment group had a higher dependency ratio than the take-up control group, indicating that more non-working family members were being supported by each wage earner. The treatment group also had more household assets in 1997 (animals, radio, TV) resulting in significant differences in the wealth index (P = 0.036). Comparison of the total treatment and comparison samples, not restricted in terms of eligibility and take-up, demonstrated no significant differences in the wealth index.
Analyses for take-up samples
The unadjusted mean depressive symptom score for women in the treatment group was 16.9 points (9.8 SD) and 18.6 points (10.2 SD) in the control group, with higher scores indicating more depressive symptoms (Table 2). Oportunidades participation was significantly associated with lower depressive symptoms (β = −1.7 points, 95% CI −2.46 to −0.96, P < 0.001), whilst controlling for maternal age, education and household demographic, ethnicity and socio-economic variables. This adjusted effect size is ∼10% of the mean for the population. No significant treatment interactions were identified with maternal age, education or household ethnicity. The treatment effect was persistent in three of the four subscales of the CES-D: depressed affect (β = −0.59 points, 95% CI −0.87 to −0.31, P < 0.001), somatic symptoms (β = −0.59 points, 95% CI −0.84 to −0.34, P < 0.001) and interpersonal relations (β = −0.17 points, 95% CI −0.28 to −0.06, P = 0.002). In addition to our primary analyses that investigated the effect of programme participation on depressive symptoms as a continuous variable, we also analysed the extent to which programme participation was associated with the level of clinically significant depressive symptoms among the women in our sample. Using a conservative cut-off score of ≥26 on the CES-D, we found that 19.5% in the treatment group vs 26.8% women in the control group reported clinical levels of depressive symptoms. The treatment group had a 26% reduced risk for depressive symptoms as compared with the control group for this cut-off, whilst controlling for maternal age, education and household demographic, ethnicity and socio-economic variables (RR = 0.74, 95% CI 0.67–0.83, P < 0.001). Using the typical USA cut-off score of 16, 50.5% of women in the treatment group and 57.2% of women in the control group were in the clinically distressed range and there was adjusted 10% reduced risk of depressive symptoms in the treatment group (RR = 0.90, 95% CI 0.84–0.95, P < 0.001).
Table 2.
Treatment effect on depressive symptoms, unadjusted and adjusted for other covariates
| CES-D Scores | Control | Treatment | Adjusteda |
|
|---|---|---|---|---|
| Continuous (range) | mean (SD) | mean (SD) | Effect (β)b | (95% CI)d |
| Full depression scale (0–60) | 18.7 (10.2) | 16.9 (9.8) | −1.71 | (−2.46 to −0.96)*** |
| Depression subscales | ||||
| Depressed affect/mood (0–15) | 4.7 (4.0) | 4.1 (3.7) | −0.59 | (−0.87 to −0.31)*** |
| Lack of positive affect (0–12) | 4.8 (2.9) | 4.7 (3.0) | −0.10 | (−0.32 to 0.12) |
| Somatic symptoms (0–15) | 4.7 (3.2) | 4.0 (3.0) | −0.59 | (−0.84 to −0.34)*** |
| Interpersonal relations (0–6) | 1.4 (1.6) | 1.3 (1.6) | −0.17 | (−0.28 to −0.06)** |
| Dichotomous with cut-off | n (%) | n (%) | RRc | |
| Depression score ≥ 26 | 347 (26.8) | 987 (19.5) | 0.74 | (0.67 to 0.83)*** |
| Depression score ≥ 16 | 740 (57.2) | 2552 (50.5) | 0.90 | (0.84 to 0.95)*** |
aAdjusted for the following covariates: maternal age, education and head of household status and household ethnicity, crowding, dependency ratio, wealth index, head of household occupation indices and state.
bAdjusted average treatment effect sizes are OLS regression coefficients (β) for the continuous scores.
cAdjusted relative risk estimates are Poisson regression coefficients for a dichotomous outcome based on a cut-off score.
dStandard errors for the estimates were adjusted for clustering at the community level.
*P < 0.05; **P < 0.01; ***P < 0.001.
Analyses for full samples
As described earlier, we replicated our analyses with the full treatment and comparison samples, reflecting the total number of women in each group without restrictions as to the women’s programme eligibility or eventual take-up of Oportunidades. The magnitude of our adjusted treatment effect is lower but remains statistically significant and meaningful; our effect is reduced from a risk ratio of 0.74–0.79. (β = −1.36 points, 95% CI −1.99 to −0.74, P < 0.001; adjusted RR = 0.79, 95% CI 0.72–0.87, P < 0.001). Thus, the treatment effect with the total samples indicates a 21% reduced risk for depressive symptoms, compared with 26% for the take-up samples. This reduction in the magnitude of the effect is expectable in this highly conservative analysis because (i) the total treatment sample now includes an indeterminate number of women who were not considered eligible for treatment and did not receive treatment and (ii) the total comparison sample includes a large proportion of women who were not eligible for treatment, were not offered treatment and did not receive treatment.
Stratification by wealth
To test the sensitivity of our analyses in terms of the women’s level of poverty, we conducted two wealth stratification analyses. First, we stratified the sample with respect to meaningful and recallable dwelling/resource characteristics such as having a non-dirt floor, electricity and water available on the property (0–1 vs 2–3 of these assets). The treatment effect was significant for all groups, though we find a stronger treatment effect for the women with higher resourced dwellings (−2.01 vs −1.6 in the take-up sample; −1.65 compared with −1.2 for the total sample). When we stratify by our composite wealth index (median split), we find a stronger effect for wealthier women in the take-up sample (−2.05 for higher wealth; −1.64 for low wealth) and little difference for the total sample (−1.38 for higher wealth, −1.45 for low wealth). Overall, the findings from the stratification analyses indicate that all benefit from the programme, but that the women who are less desperately poor tend to benefit more.
Mediation analyses
Our mediation analyses gave moderately strong evidence that perceived stress was a mediator of the treatment effect on depressive symptoms and some evidence that perceived control was also (Table 3). The indirect effect of treatment through perceived stress was −0.53 (95% CI −0.82 to −0.22) and was −0.18 (95% CI −0.39 to 0.00) for perceived control. Perceived stress accounted for 34% of the treatment effect, whilst perceived control accounted for 12%. The direct treatment effect on depression remained fairly large adjusting for either of the mediators. Sensitivity analysis indicated that the mediated effect for perceived stress was moderately robust to unmeasured confounding; the mediated effect for perceived control was not. For example, an unmeasured binary confounder that, amongst those with the same mediator level, had a prevalence of 70% for those with the treatment vs 40% for those without would need to increase CES-D scores by 1.77 points to explain away the mediated effect for perceived stress but would only need to increase CES-D by 0.60 points to explain away the mediated effect for perceived control.
Table 3.
Test of mediation by perceived stress and lack of perceived control, adjusted for other covariates and social support
| Perceived stress |
Lack of mastery/control |
|||
|---|---|---|---|---|
| Effect Sizea | β (95% CI)b | Standard β (95% CI)b | β (95% CI)b | Standard β (95% CI)b |
| Programme effect on depression, without mediator | −1.52*** | −0.062*** | −1.52*** | −0.062*** |
| (−2.18 to −0.86) | (−0.089 to −0.035) | (−2.18 to −0.86) | (−0.089 to −0.035) | |
| Programme effect on depression, adjusted for mediator (direct effect) | −1.00** | −0.040** | −1.34*** | −0.054*** |
| (−1.61 to −0.38) | (−0.065 to −0.016) | (−1.92 to −0.76) | (−0.078 to −0.031) | |
| Programme effect on mediator | −0.64** | −0.044** | −0.25 | −0.023 |
| (−1.05 to −0.24) | (−0.071 to −0.016) | (−0.56 to 0.057) | (−0.052 to 0.0053) | |
| Mediator effect on depression | 0.82*** | 0.49*** | 0.73*** | 0.32*** |
| (0.78–0.85) | (0.47–0.51) | (0.67–0.79) | (0.29–0.34) | |
| Programme effect on depression, through mediator (indirect effectc) | −0.53*** | −0.021*** | −0.18 | −0.0074 |
| (−0.82 to −0.22) | (−0.033 to −0.010) | (−0.39 to 0.0043) | (−0.016 to 0.0007) | |
aEffect sizes are OLS regression coefficients (β) and standardized coefficients (standard β) adjusted for the following covariates: maternal age, education, social support and head of household status and household ethnicity, crowding, dependency ratio, wealth index, head of household occupation indices and state. Standard errors for the effect estimates were adjusted for clustering at the community level.
bStandard errors for the estimates were adjusted for clustering at the community level or bootstrapped (indirect effect only).
cThe product of the coefficient for the programme effect on the mediator and the coefficient for the mediator effect on depression controlling for the programme.
*P < 0.05; **P < 0.01; ***P < 0.001.
Discussions
This quasi-experimental study of a large sample of mothers from rural Mexico found that a decrease in extreme poverty due to participation in Oportunidades—one of the world’s first and most widely-implemented conditional cash transfer programmes—was linked with a 10% decrement in their depressive symptoms from the mean. Framing our results in terms of cut-off scores for clinically significant distress, we found 19.5% of women in the Oportunidades group had scores in the clinical range compared with 26.6% in the control group, a 0.74 times lower probability of clinically significant scores than the control group. Although mothers’ mental health was not targeted by the programme, mothers demonstrated a modest but clinically meaningful effect on their levels of depressive symptoms. The effects for total depressive symptoms and for the subscales that assess depressed mood, somatic symptoms and interpersonal relations were robust after controlling for a wide range of demographic, educational and wealth variables.
We further found that that the Oportunidades treatment effect was mediated by mothers’ levels of perceived stress and possibly perceived control, suggesting that reductions in perceived stress and increases in perceived control may serve as meaningful pathways by which increases in income exerted effects on maternal mental health. The present study extends the literature on CCT programmes, which has found developmental benefits for children’s nutrition, physical growth and school attendance.22,23,38 Previous research on cash transfer programmes in other developing countries had found no or limited evidence for effects on maternal depressive symptoms after 9 and 17 months of programme participation.27,28 Considering these findings, our results suggest that a longer time frame is helpful in detecting these ‘ripple’ effects.
Regarding limitations, it is essential to consider that our quasi-experimental design does not benefit from the same strength of causal inference that could be interpreted from an experimental design despite the rigorous methods used here to minimize selection effects. Our inference is bolstered, however, by important research on Oportunidades using the same analytical methods that confirmed that a quasi-experimental approach showed similar results to a true experiment.51 Our efforts to minimize selection bias for our take-up analysis resulted in a smaller sample size of participants due to the inclusion of only those mothers who actually participated in the programme—immediately in the case of the treatment group and later in the case of the comparison group. This strengthened the internal validity of our design whilst also arguably limiting the generalizeability of our findings insofar as we excluded slightly wealthier women who did not end up meeting programme eligibility criteria. We accordingly took multiple analytical steps to address the sensitivity of our findings. First, we replicated our results using the total treatment and control samples without consideration of programme eligibility and take-up; we found that our treatment effect was reduced in magnitude but remained robust. Second, we conducted an analysis stratified by the poverty indicators for the women’s households; that there were treatment effects for all but those who were less poor demonstrates stronger effects. We speculate that the poorest women may benefit less because their living conditions remain so severely disadvantaged despite the boost from the Oportunidades programme. The very poor women who do have some economic assets may be able to leverage the economic and social investments of the programme more effectively and experience more psychological gains. It should also be noted that we had only adequate internal reliability for our mediator variables; future research may yield more robust effects if measurement error can be reduced. Issues concerning temporality and feedback between the mediators and outcome could potentially be addressed by repeated measures data and alternative analytical techniques.52
Our findings suggest that interventions that invest in the basic human capital needs of children may over time exert distal effects on mothers’ mental health. It is likely, however, that additional intervention components specifically focused on maternal mental health are needed to bring about stronger effects on maternal symptoms of depression. Since the design of Oportunidades did not include a component specifically focused on maternal mental health, we are not able to test the potential additive or synergistic effects of combining cash transfers with components that directly target maternal mental health. In general, the results of this study support a social–ecological perspective on mental health and psychopathology that emphasizes that the well-being of the individual is responsive to macro-level factors such as economic policies and programmes.53 Ideally, policy interventions to improve the development of very poor children and families will generate a reciprocal effect whereby improvements in mental health will further activate mothers in their efforts to support the growth and well-being of themselves and their families.
Funding
The National Institutes of Health Roadmap for Medical Research Initiative [grants P20RR20817 (PI Paul Gertler) and National Institute of Child Health & Human Development R01 HD44146-03 55 (PI Paul Gertler)]; the National Institutes of Health (grant HD060696 to T.J.VW.); and the William T Grant Foundation Scholars Award 6894 (to E.J.O.).
Acknowledgements
The authors express appreciation to the research participants and the other investigators of the Progresa/Oportunidades evaluation, to Thomas Cook for methodological consultation, and to Laura Douglas for research assistance in the preparation of the manuscript. None of the funders had any role in the design and conduct of the study; collection, management, analysis and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Conflict of interest: None declared.
KEY MESSAGES.
A large-scale conditional cash transfer programme in Mexico to alleviate extreme poverty and improve child health in rural families demonstrated modest but clinically meaningful effects on mothers’ depressive symptoms.
The improvement in depressive symptoms was partially mediated by lower perceived stress and possibly higher perceived control.
Macro-level government programmes and policies that focus on economic incentives for human capital investments may show benefits in mental health, above and beyond the targeted health and educational outcomes for children.
References
- 1.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet. 2007;370:851–58. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 2.Kessler R, Aguilar-Gaxiola S, Alono J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) Surveys. Epidemiologia e Psichiatria Sociale. 2009;18:23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black M, Baqui A, Zaman K, et al. Depressive symptoms among rural Bangladeshi mothers: Implications for infant development. J Child Psychol Psychiatry. 2007;48:764–72. doi: 10.1111/j.1469-7610.2007.01752.x. [DOI] [PubMed] [Google Scholar]
- 4.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 5.Wachs T, Black M, Engle P. Maternal depression: A global threat to children's health, development, and behavior and to human rights. Child Dev Perspect. 2009;3:51–59. [Google Scholar]
- 6.Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. Br J Psychiatry. 2000;177:486–92. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the national comorbidity survey: I. Lifetime prevalence, chronicity and recurrence. J Affect Disord. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- 8.Angold A, Costello EJ, Worthman CM. Puberty and depression: the roles of age, pubertal status and pubertal timing. Psychol Med. 1998;28:51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- 9.Engle PL. Maternal mental health: program and policy implications. Am J Clin Nutr. 2009;89(Suppl):963S–66S. doi: 10.3945/ajcn.2008.26692G. [DOI] [PubMed] [Google Scholar]
- 10.Minkovitz C, Strobino D, Scharfstein D, et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115:306–14. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 11.Leiferman J. The effect of maternal depressive symptomatology on maternal behaviors associated with child health. Health Educ Behav. 2002;29:596–607. doi: 10.1177/109019802237027. [DOI] [PubMed] [Google Scholar]
- 12.Radke-Yarrow M. Children of Depressed Mothers: From Early Childhood to Maturity. Cambridge: Cambridge University Press; 1998. [Google Scholar]
- 13.Muñoz R, Cuijpers P, Smit F, Barrera A, Leykin Y. Prevention of major depression. Annu Rev Clin Psychol. 2010;6:181–212. doi: 10.1146/annurev-clinpsy-033109-132040. [DOI] [PubMed] [Google Scholar]
- 14.Rahman A, Harrington R, Bunn J. Can maternal depression increase infant risk of illness and growth impairment in developing countries? Child Care Health Dev. 2002;28:51–56. doi: 10.1046/j.1365-2214.2002.00239.x. [DOI] [PubMed] [Google Scholar]
- 15.The State of the World's Children 2005 - Childhood under threat. published by UNICEF 2004. Available at: http://www.unicef.org/publications/files/SOWC_2005_(English).pdf. [Google Scholar]
- 16.WHO/UNFPA. Maternal Mental Health and Child Health and Development in Low and Middle Income Countries. Report of the WHO–UNFPA Meeting. Geneva, Switzerland: 2008. [Google Scholar]
- 17.Walker SP, Wachs TD, Gardner JM, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007;369:145–57. doi: 10.1016/S0140-6736(07)60076-2. [DOI] [PubMed] [Google Scholar]
- 18.Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: Prospective study from Rawalpindi, Pakistan. J Affect Disord. 2007;100:115–21. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folkman S, Lazarus RS, Gruen R, DeLongis A. Appraisal, coping, health status, and psychological symptoms. J Pers Soc Psychol. 1986;50:571–79. doi: 10.1037//0022-3514.50.3.571. [DOI] [PubMed] [Google Scholar]
- 20.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull WHO. 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 21.Morris P, Huston A, Duncan G, Crosby D, Bos H. Welfare program implementation and parents' depression. The Social Service Review. 2008;82:579–614. doi: 10.1086/597349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gertler PJ. Do conditional cash transfers improve child health? Evidence from PROGRESA's controlled randomized experiment. Am Econ Rev. 2004;94:331–36. doi: 10.1257/0002828041302109. [DOI] [PubMed] [Google Scholar]
- 23.Lomeli EV. Conditional cash transfers as social policy in Latin America: an assessment of their contributions and limitations. Annu Rev Sociol. 2008;34:475–99. [Google Scholar]
- 24.Ozer EJ, Fernald LCH, Manley J, Gertler P. Effects of a conditional cash transfer program on the behavior problems of young children living in poverty. Pediatrics. 2009;123:e630–37. doi: 10.1542/peds.2008-2882. [DOI] [PubMed] [Google Scholar]
- 25.Rawlings LB, Rubio GM. Evaluating the impact of conditional cash transfer programs. World Bank Res Observer. 2005;20:29–55. [Google Scholar]
- 26.Morley S, Coady D. From Social Assistance to Social Development: Targeted Education Subsidies in Developing Countries. Washington DC: International Food Policy Research Institute; 2003. [Google Scholar]
- 27.Paxson C, Schady N. Does Money Matter? The Effects of Cash Transfers on Child Health and Development in Rural Ecuador. Impact Evaluation Series. Washington DC: The World Bank; 2007. [DOI] [PubMed] [Google Scholar]
- 28.Macours K, Schady N, Vakis R. Cash Transfers, Behavioral Changes, and Cognitive Development in Early Childhood: Evidence from a Randomized Experiment. Impact Evaluation Series. Washington DC: The World Bank Development Research Group; 2008. [Google Scholar]
- 29.Verner D. World Bank Policy Research Working Paper. Washington DC: World Bank; 2005. Activities, Employment, and Wages in Rural and Semi-Urban Mexico. [Google Scholar]
- 30.Fiszbein A, Schady N. Conditional Cash Transfers: Reducing Present and Future Poverty. Washington DC: The World Bank; 2009. [Google Scholar]
- 31.Fernald LCH, Gertler PJ, Neufeld LM. The role of cash in conditional cash transfer programs: An analysis of Mexico's Oportunidades. Lancet. 2008;371:828–37. doi: 10.1016/S0140-6736(08)60382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fleischer NE, Fernald LC, Hubbard AE. Correlates of depression in a large sample of low-income women in Mexico. Epidemiology. 2007;18:678–85. doi: 10.1097/EDE.0b013e3181567fc5. [DOI] [PubMed] [Google Scholar]
- 33.Behrman JR, Todd PE. A Report on the Sample Sizes Used for the Evaluation of the Education, Health and Nutrition Program (PROGRESA) of Mexico. Washington DC: International Food Policy Research Institute; 1999. [Google Scholar]
- 34.Behrman JR, Todd PE. Randomness in the Experimental Samples of PROGRESA (Education, Health and Nutrition Program) Washington DC: International Food Policy Research Institute; 1999. [Google Scholar]
- 35.Todd P. Technical Note on Using Matching Estimators to Evaluate the OPORTUNIDADES Program for Six Year Follow-up Evaluation of OPORTUNIDADES in Rural Areas. Philadelphia: University of Pennsylvania; 2004. [Google Scholar]
- 36.Abadie A, Imbens G. Large sample properties of matching estimators for average treatment effects. Econometrica. 2006;74:235–67. [Google Scholar]
- 37.Peck LC. Subgroup analysis in social experiments: measuring program impacts based on post-treatment choice. Am J Eval. 2003;24:157–87. [Google Scholar]
- 38.Fernald LC, Gertler PJ, Neufeld LM. 10-year effect of Oportunidades, Mexico's conditional cash transfer programme, on child growth, cognition, language, and behaviour: a longitudinal follow-up study. Lancet. 2009;374:1997–2005. doi: 10.1016/S0140-6736(09)61676-7. [DOI] [PubMed] [Google Scholar]
- 39.Radloff L. The CES-D scale: A self report depression scale for research in the general population. Appl Psychol Manag. 1977;1:385–401. [Google Scholar]
- 40.Masten WG, Caldwell-Colbert AT, Alcala SJ, Mijares BE. Confiabilidad y validez de la Escala de Depresion del Centro de Estudios Epidemiologicos [Reliability and validity of the Center for Epidemiological Studies Depression Scale] Hispanic J Behav Sci. 1986;8:77–84. [Google Scholar]
- 41.Salgado de Snyder VN, Maldonado M. Características psicométricas de la Escala de Depresión del Centro de Estudios Epidemiológicos en mujeres mexicanas adultas de áreas rurales [Psychometric characteristics of the Center for Epidemiologic Studies Depression Scale in adult Mexican women from rural areas] Salud Publica Mex. 1994;36:200–09. [PubMed] [Google Scholar]
- 42.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 43.Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS) Span J Psychol. 2006;9:86–93. doi: 10.1017/s1138741600006004. [DOI] [PubMed] [Google Scholar]
- 44.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- 45.Cohen S, Mermelstein R, Kamarck T, Hoberman HM, editors. Measuring the Functional Components of Social Support. Dordrecht: Martinus Nijhoff Publishers; 1985. [Google Scholar]
- 46.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–06. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 47.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–43. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 48.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- 49.VanderWeele T. Bias formulas for sensitivity analysis for direct and indirect effects. Epidemiology. 2010;21:540–51. doi: 10.1097/EDE.0b013e3181df191c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.VanderWeele T, Vansteelandt S. Conceptual issues concerning mediation, interventions and composition. Statistics and Its Interface - Special Issue on Mental Health and Social Behavioral Science. 2009;2:457–68. [Google Scholar]
- 51.Diaz JJ, Handa S. An assessment of propensity score matching as a nonexperimental impact estimator: evidence from Mexico’s PROGRESA program. JHR. 2006;XLI:319–45. [Google Scholar]
- 52.VanderWeele T. Marginal structural models for the estimation of direct and indirect effects. Epidemiology. 2009;20:18–26. doi: 10.1097/EDE.0b013e31818f69ce. [DOI] [PubMed] [Google Scholar]
- 53.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10:282–98. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]