Abstract
Objective
We assessed the impact of reducing the binge eating frequency and duration thresholds on the diagnostic criteria for bulimia nervosa (BN) and binge eating disorder (BED).
Method
We estimated the lifetime population prevalence of BN and BED in 13,295 female twins from the Swedish Twin study of Adults: Genes and Environment employing a range of frequency and duration thresholds. External validation (risk to co-twin) was used to investigate empirical evidence for an optimal binge eating frequency threshold.
Results
The lifetime prevalence estimates of BN and BED increased linearly as the frequency criterion decreased. As the required duration increased, the prevalence of BED decreased slightly. Discontinuity in co-twin risk was observed in BN between at least four times per month and at least five times per month. This model could not be fit for BED.
Discussion
The proposed changes to the DSM-5 binge eating frequency and duration criteria would allow for better detection of binge eating pathology without resulting in a markedly higher lifetime prevalence of BN or BED.
Debate exists regarding the appropriateness of the frequency and duration specifications for the symptom of binge eating in the Diagnostic and Statistical Manual of Mental Disorders 4th ed., text rev. [DSM-IV-TR].1–6 It is relevant to examine empirically how alterations to these specifications could influence the prevalence of bulimia nervosa (BN) and binge eating disorder (BED) and the nature of populations captured when applying various thresholds. In DSM-IV, for BN, episodes of binge eating must occur at least twice a week for three months whereas, for a provisional diagnosis of BED, binge eating must occur on average at least two days per week for six months. Although the lifetime prevalence of symptoms of binge eating are relatively common,7,8 threshold diagnoses of BN and BED are considerably more rare, in part, due to the additional frequency and duration criteria imposed by the DSM-IV.4,9,10
The binge eating frequency criterion may create a diagnostic inflection point by distinguishing individuals with less severe psychopathology from those with threshold presentations.4 Despite the importance of this criterion, empirical evidence supporting the validity of the current twice per week threshold for BN or two days per week threshold for BED is lacking.4, 11–14 The binge eating frequency criterion was first introduced for BN in the DSM-III-R, raising concern in the Eating Disorders Work Group of the American Psychiatric Association’s Task Force on DSM-IV. At that time, unpublished data suggested that individuals who binge once per week did not differ significantly from those who binge more frequently on concurrent psychopathology or treatment outcome.15 The work group acknowledged the arbitrary nature of the twice a week frequency criterion. However, they expressed concern that few studies had examined the utility of a wide range of thresholds, and, in the absence of definitive empirical evidence, no modifications were made.16
Since the publication of the DSM-IV, additional research has documented limitations inherent with the binge eating frequency criterion for BN2, 4, 17 and BED,18–20 suggesting that the current criterion may be too stringent. For example, individuals who binge eat twice per week are similar to individuals who binge eat less frequently on demographic characteristics, body mass index (BMI), eating disorder symptomatology, and psychiatric distress.20 Further, individuals who binge eat once per week and individuals who meet the frequency criterion respond similarly to a variety of treatments including group psychoeducation,21 behavioral weight loss,22 and bariatric surgery.5
Nonetheless, research investigating the utility of a range of thresholds is lacking.6 Sullivan, Bulik, and Kendler4 addressed this issue by exploring a range of alternative thresholds for binge eating frequency in a population-based sample of 1,897 female twins with a lifetime history of BN (n = 31). Thresholds ranging from one to eight times per month were investigated against external validators in several domains including familial aggregation (risk to co-twin), symptom duration, comorbidity, and the personality measures of neuroticism and extraversion. For most validators, there was no indication of a clear threshold at which there was a qualitative change. The only exception was risk to co-twin, where the data suggested an appropriate threshold of one binge per week. Several other investigations have also advocated for a once per week threshold3, 5, 23 and, in a recent review, Wilson and Sysko6 concluded that changing DSM-5 frequency threshold to once per week is the most empirically supported option. The six month duration criterion for BED is also arbitrary and standardizing the binge eating duration criterion to three months across diagnoses has been recommended for DSM-5.24
One significant advantage to lowering the binge eating frequency and duration criteria is that a larger number of individuals with binge eating pathology would be identified.6 Currently, those with subthreshold binge eating frequency are excluded from receiving a DSM-IV diagnosis of BN or a provisional diagnosis of BED based on the arbitrary twice per week or two days per week cut-off.17 The majority of individuals with eating disorders (20–60%) currently receive a diagnosis of eating disorder not otherwise specified (EDNOS). EDNOS is intended to be a “residual” diagnosis and yet it encompasses the majority of patients who present for treatment.25, 26 Further, a full syndrome DSM-IV diagnosis is often required for reimbursement for third-party payers,27 which prohibits individuals from receiving optimal care. Several options have been proposed to address the high frequency of EDNOS in the DSM-5 including removing the amenorrhea criterion for anorexia nervosa (AN)28 and including BED as a primary diagnosis.28
Relaxing both the binge eating frequency and duration criteria could theoretically result in significant increases in the prevalence of BN and BED. Based on a family study of overweight individuals with BED, Hudson et al.30 estimated that there would be minimal impact of lowering binge eating frequency (to one day per week) and duration (to one month) on lifetime and point prevalence of BED. However, population based investigations are required to confirm this observation in a less selected sample. Funding for mental health care services is increasingly dictated by considerations of population prevalence.31 The impact of relaxing these criteria on the health care system is unknown. Thus, the primary purpose of the current investigation was to explore the impact of changing the frequency and duration criteria for BN and BED. Our goals were: (1) to examine the lifetime prevalence of BN and BED across frequencies of binge eating ranging from once per month to at least eight times per month in a population-based sample; (2) to examine the lifetime prevalence of BED across different durations including one month, three months, and six months; and (3) to examine risk to co-twin for BN and BED across the range of binge eating frequencies from once per month to at least eight times per month as a means of external validation.
METHOD
Participants
Participants were from the Swedish Twin study of Adults: Genes and Environment (STAGE; http://ki.se/ki/jsp/polopoly.jsp?d=9610&l=en), a large population-based study. STAGE is a subsample of the Swedish Twin Registry (STR; http://ki.se/twinreg) and includes Swedish twins born 1959–1985.32, 33 Twins were between the ages of 20 and 47 years in 2005, at the time of interview. Data were collected on a variety of health related measures, sociodemographic and socioeconomic measures, and habits and behaviors using web-based questionnaires (43.1% responded exclusively using the web-based format) or telephone interviews (16.5% responded using the telephone format exclusively). Over 25,000 twins responded out of 43,000 eligible individuals, a response rate of 59.6%. For the eating disorders section there was adequate agreement between the web-based questionnaire and telephone interviews (Kappa = .76).33 A detailed description of the study design can be found elsewhere.32, 33
Men were excluded in the current study due to low lifetime prevalence of eating disorder symptoms and diagnoses thus precluding meaningful analysis: binge eating = 0.8% (n = 80); BN = 0.1% (n = 7); BED = 0.0% (n = 2). Of note, the prevalence of binge eating, BN, and BED in men was slightly lower in this sample compared with the US national averages (binge eating = 4.0%; BN = 0.5%, BED = 2.0%).34 The observed lower prevalence for men in our sample may reflect cultural differences, including the stigma associated with endorsing items related to experiencing a sense of being ‘out of control’ when eating. The final analysis population included 13,295 women.
After complete description of the study to participants, written informed consent was obtained. STAGE was approved by the Regional Ethics Committee at the Karolinska Institutet and is in accord with the Declaration of Helsinki. The current study was approved by the Biomedical Institutional Review Board at the University of North Carolina at Chapel Hill. All participants provided informed consent.
Definitions: Binge Eating, Bulimia Nervosa, and Binge Eating Disorder
Using an expanded Structured Clinical Interview for DSM-IV-based instrument,35 lifetime histories of binge eating, BN, and BED were assessed. Lifetime binge eating was assessed using the following questions: “Have you ever had binges when you ate what most people would regard as an unusually large amount of food in a short period of time?” with response options yes, no, and don’t know/refuse. Individuals who answered yes to this question were next asked, “When you were having eating binges, did you feel you’re your eating was out of control?” with response options not at all, slightly, moderately, very much, extremely, and don’t know/don’t wish to answer. Individuals were classified as having lifetime binge eating if they answered yes to the first question and slightly, moderately, very much, or extremely to the second question. Specific items and responses used to assign BN and BED diagnoses are listed in Table 1. To assess the effects of lowering the frequency threshold, the binge eating criteria were modified for BN and BED algorithms. Directly following the two binge eating questions listed above, participants were asked, “When you were binging the most, how many binges would you have in a month?” Responses were evaluated separately ranging from at least one time per month to at least eight times per month. It should be noted that participants were not provided with a specific definition of binge eating. In addition, this investigation was limited to assessing BED frequency in episodes per month rather than days per month as required by DSM-IV.
TABLE1.
DSM-IV Criteria Used for Bulimia Nervosa and Binge Eating Disorder
| Bulimia Nervosa | |
|---|---|
| 1a. Have you even had eating binges when you ate what most people would regard as an unusually large amount of food in a short period of time? 1b. When you were having eating binges, did you feel your eating was out of control? (response on 5 point Likert Scale) |
1a. Yes AND 1b. (2) Slightly (3) Somewhat (4) Very much OR (5) Extremely |
| 2. Which of these did you use during the same time that you were binge eating? Making yourself vomit? Laxatives? Diuretics? Diet Pills? Exercise more than 2 hours per day? Fast or not eat? Other methods? |
2. A ‘Yes’ response to any of these items meets criteria. |
| 3a. When you were binging the most, how many binges would you have in a month? 3b. For how long did you have binge eating episodes? |
3a. At least 8 times a month AND 3b. At least 3 months |
| 4. Statements regarding weight and shape on a 5 point Likert scale | 4. Weight or shape are important things that affect how I feel about myself. OR Weight or shape are the most important things that affect how I feel about myself. |
| Binge Eating Disorder | |
| 1a. Have you even had eating binges when you ate what most people would regard as an unusually large amount of food in a short period of time? 1b. When you were having eating binges, did you feel your eating was out of control? (response on 5 point Likert Scale) |
1a. Yes AND 1b. (2) Slightly (3) Somewhat (4) Very much OR (5) Extremely |
| 2. During eating binges, did you a) Eat more rapidly than usual? b) Eat large amounts of food when you didn’t feel physically hungry? c) Eat alone because you were embarrassed by how much you were eating? d) Feel disgusted with yourself, depressed, or very guilty after overeating? |
2. A ‘Yes’ response to at least 3 of these items meets criteria. |
| 3. How upset or distressed did binge eating usually make you feel? | 3. (3) Somewhat (4) Very much OR (5) Extremely |
| 4a. When you were binging the most, how many binges would you have in a month? 4b. For how long did you have binge eating episodes? |
4a. At least 8 times a month AND 4b. At least 6 months |
| 5. Which of these methods did you use during the same time you were binge eating? Vomiting, Laxatives, Diuretics, Exercise more than 2 hours per day, Fasting, Other Methods |
5. All inappropriate compensatory behaviors had be scored as ‘No’ |
We also assessed three different duration criteria for BED that reflect proposed changes in DSM-5: 1 month, 3 months, and 6 months, to explore the impact of changing the required duration on lifetime prevalence.
Statistical Analyses
All analyses were performed using SAS/STAT software, Version 9.1 of the SAS System for Windows.36 Frequencies were generated to determine lifetime prevalence estimates for BN and BED across eight binge eating frequencies ranging from once per month to at least eight times per month.
Cox proportional hazard models were used to assess risk of BN to the co-twin for each of the eight frequency criteria. Age at first binge was used as time to onset. Proportional odds assumptions were tested and met. Lifetime prevalence of BED was too low to apply these models.
An increased lifetime relative risk (RR) or hazard ratio of developing a disorder in a relative of an individual with that disorder compared with the risk of developing the disorder in families of comparable individuals without the disorder demonstrates that the trait aggregates in families. In our case, we are examining the risk of BN in co-twins using differing frequency criteria. An RR that equals one implies no risk in the co-twin, whereas an RR greater than one suggests the event is more likely to occur under a particular condition. Using a discontinuity of risk model,37 we expect to see a threshold at which risk to co-twin for BN is maximized across the various frequency criteria. Based on the current DSM-IV frequency criteria, we would expect to see a discontinuity at eight binges per month, suggesting that risk to co-twin is optimized only at this frequency. If no such threshold exists, less frequent binge eating might increase co-twin risk monotonically as frequency increases for BN. This would suggest continuity in risk and no empirical threshold.
RESULTS
Frequency Criterion
The lifetime prevalence for binge eating was 5.8% (n = 758) in this population of women. Table 2 presents the lifetime prevalence of BN and BED for each binging frequency for at least three months duration. Not surprisingly, the lifetime prevalence estimates of BN and BED increased linearly as frequency criterion decreased. Lifetime prevalence was highest for the once per month frequency and lowest for at least eight times per month. Specifically, relaxing the binge eating frequency criterion from at least eight times per month to at least four times per month resulted in a lifetime population prevalence increase of 0.3% and a relative increase of 32% for BN (a difference of 50 women). For BED this same change in frequency resulted in a lifetime population prevalence increase of 0.1% and a relative increase of 77% (a difference of 20 women).
TABLE 2.
Lifetime Prevalence (%) of Bulimia Nervosa and Binge Eating Disorder for a Frequency of at Least 1 Time Per Month Through at Least 8 Times Per Month (at Least 3-Months Duration).
| Bulimia Nervosa | Binge Eating Disorder | |||
|---|---|---|---|---|
| Binging Frequency Per Month |
No | Yes | No | Yes |
| ≥ 8 times | 13065 (98.8) | 156 (1.2) | 13099 (99.8) | 26 (0.2) |
| ≥ 7 times | 13061 (98.8) | 158 (1.2) | 13096 (99.8) | 27 (0.2) |
| ≥ 6 times | 13046 (98.7) | 169 (1.3) | 13082 (99.8) | 30 (0.2) |
| ≥ 5 times | 13034 (98.7) | 176 (1.3) | 13071 (99.7) | 34 (0.3) |
| ≥ 4 times | 12989 (98.4) | 206 (1.6) | 13025 (99.7) | 46 (0.4) |
| ≥ 3 times | 12971 (98.3) | 221 (1.7) | 13007 (99.6) | 49 (0.4) |
| ≥ 2 times | 12948 (98.2) | 233 (1.8) | 12989 (98.6) | 55 (0.4) |
| ≥ 1 time | 12934 (98.2) | 241 (1.8) | 12975 (99.5) | 61 (0.5) |
Alternate Duration Criterion
Table 3 presents lifetime prevalence estimates for BED for each binge eating frequency (i.e., at least one time per month through at least eight times per month) for one month, three months, and six months duration. In general, as duration increased from one to three to six months, lifetime prevalence decreased slightly. For example, changing the BED duration criterion from six months to three months (proposed DSM-5 change) results in a 0.03% increase in lifetime prevalence, 0.17% (n = 19) vs. 0.20% (n = 26).
TABLE 3.
Lifetime Prevalence (%) of Binge Eating Disorder for at Least 1 Time Per Month Through at Least 8 Times Per Month for 1-Month, 3-Months, and 6-Months Duration. Total number of participants assessed = 13295.
| Binging Frequency Per Month |
1 Month | 3 Months | 6 Months |
|---|---|---|---|
| ≥ 8 times | 30 (0.23) | 26 (0.20) | 23 (0.17) |
| ≥ 7 times | 32 (0.24) | 27 (0.21) | 23 (0.17) |
| ≥ 6 times | 35 (0.26) | 30 (0.23) | 26 (0.20) |
| ≥ 5 times | 43 (0.32) | 34 (0.26) | 30 (0.23) |
| ≥ 4 times | 57 (0.43) | 46 (0.35) | 40 (0.30) |
| ≥ 3 times | 60 (0.45) | 49 (0.38) | 42 (0.32) |
| ≥ 2 times | 68 (0.51) | 55 (0.42) | 48 (0.36) |
| ≥ 1 time | 74 (0.56) | 61 (0.47) | 54 (0.41) |
Co-Twin Risk
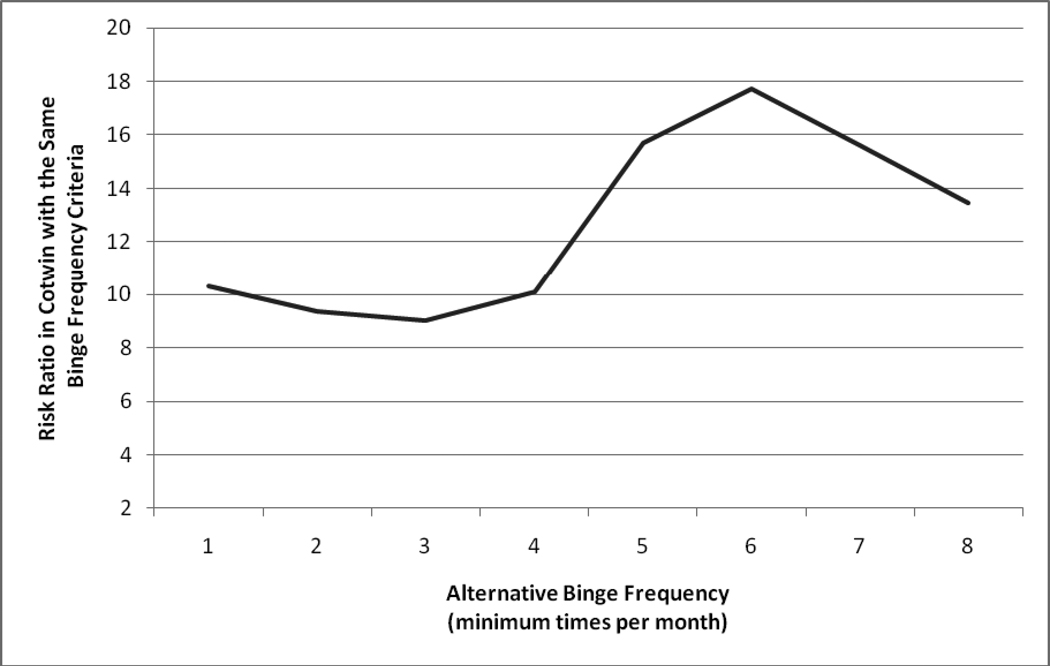
RR estimates to co-twin for BN are presented in Table 4. Figure 1 presents risk to co-twin pictorially. As can be seen in Figure 1, there is a discontinuity in co-twin risk in BN between at least four times per month and at least five times per month. The RR for BN for binge eating frequency of at least four times per month is 10.11 compared to RR = 13.46 for at least eight times per month (see Table 4).
TABLE 4.
Relative Risk Estimates (95% Confidence Limits) in Co-Twin for Bulimia Nervosa for at Least 1 Time Per Month Through at Least 8 Times Per Month for 3-Months Duration.
| Binging Frequency Per Month |
Bulimia Nervosa |
|---|---|
| ≥ 1 time | 10.30 (4.43, 23.95) |
| ≥ 2 times | 9.37 (3.93, 22.35) |
| ≥ 3 times | 9.03 (3.61, 22.58) |
| ≥ 4 times | 10.11 (3.79, 26.99) |
| ≥ 5 times | 15.71 (5.73, 43.06) |
| ≥ 6 times | 17.72 (6.42, 48.91) |
| ≥ 7 times | 15.63 (5.32, 45.90) |
| ≥ 8 times | 13.46 (4.33, 41.89) |
FIGURE 1.
Relative Risk to Co-Twin for Bulimia Nervosa for Binge Eating Frequencies Ranging from 1–8 Binges Per Month for 3-Months Duration.
DISCUSSION
One significant concern regarding the proposed changes to the DSM-5 binge eating frequency and duration criteria is that relaxing these criteria may open the diagnostic “floodgates,” resulting in a dramatic increase in BN and BED prevalence, which could have significant implications for the mental heath care system.31 Assuming that Sweden is representative of the United States (US), our results indicate that relaxing the binge eating frequency and duration criteria as proposed for in DSM-5 is unlikely to have a significant impact on lifetime population prevalence for BN and BED and thus, the impact on the mental health care field should be minimal.
Current results are consistent with those of a prior investigation by Sullivan, Bulik, and Kendler,4 who examined an optimal diagnostic threshold for binge eating frequency for BN and found that, based on risk to co-twin, a once per week threshold was the most empirically supported frequency threshold. The current investigation, which also used risk to co-twin as an external validator, found a similar diagnostic inflection point for BN: a marked increase in the risk ratio to co-twin between at least four and five binges per month (from RR = 6.55 to RR = 10.84). In addition, both the present study and the investigation by Sullivan, Bulik, and Kendler4 found no evidence of discontinuity at the twice per week boundary used in DSM-IV, suggesting that this cut-off does not reflect a natural diagnostic inflection point.
Limitations
Results from this study should be considered in light of several limitations. First, the population evaluated included only women from Sweden and results might differ for men or for individuals from different ancestry groups. Second, these data were collected using computer-administered self-report assessments. Although participants might be more forthcoming with sensitive information using computer-administered assessments,44 computer-based assessments can be less precise than interview-based assessments conducted by a clinician. Third, participants were only included in this investigation if they endorsed having previously experienced a loss of control while eating; however, they were not provided with a specific definition of binge eating that stated explicitly that loss of control was required for each binge episode. Although this may have resulted in over reporting of binge eating symptomatology, our estimate for binge eating is lower than that found in a similar investigation using a large population-based Scandinavian sample45 where binge eating was more explicitly defined (5.8% vs. 8.6%). Thus, the estimates in this investigation are unlikely to be inflated due to participants’ misunderstanding the definition of a binge. This investigation also used the number of binge episodes rather than the number of binge days for the frequency criterion for BED. However, days and episodes of binge eating are highly correlated46 and the use of episodes, rather than days for the threashold criterion for both BN and BED, is proposed for DSM-5.47
Conclusion
This investigation offers empirical support for the proposed changes in the frequency and duration criteria for BN and BED in DSM-5 and provides evidence that this relaxing of criteria would allow for better detection of binge eating pathology while not leading to a markedly higher lifetime prevalence of illness nor consequent burdens on the health care system.
Acknowledgements
Dr. Trace was supported by National Institute of Health grant T32MH076694 (PI: Bulik). Drs. Thornton and Root were supported by National Institute of Health grant 1K01AA 18719-01A1 (PI: Root). This study was also supported by grants CA-085739 (PI: Sullivan) and AI-056014 (PI: Sullivan) from the National Institutes of Health. The Swedish Twin Registry is supported by grants from the Swedish Department of Higher Education the Swedish Research Council. We thank all participants for their time and effort.
Footnotes
Disclosures: All authors reported no biomedical financial interests or potential conflicts of interest.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition Text Revision. Washington, DC: American Psychiatric Press; 2000. [Google Scholar]
- 2.le Grange D, Binford RB, Peterson CB, Crow SJ, Crosby RD, Klein MH, et al. DSM-IV threshold versus subthreshold bulimia nervosa. Int J Eat Disord. 2006;39:462–467. doi: 10.1002/eat.20304. [DOI] [PubMed] [Google Scholar]
- 3.Rockert W, Kaplan AS, Olmsted MP. Eating disorder not otherwise specified: the view from a tertiary care treatment center. Int J Eat Disord. 2007;40 Suppl:S99–S103. doi: 10.1002/eat.20482. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan PF, Bulik CM, Kendler KS. The epidemiology and classification of bulimia nervosa. Psychol Med. 1998;28:599–610. doi: 10.1017/s0033291798006576. [DOI] [PubMed] [Google Scholar]
- 5.White MA, Masheb RM, Rothschild BS, Burke-Martindale CH, Grilo CM. The prognostic significance of regular binge eating in extremely obese gastric bypass patients: 12-month postoperative outcomes. J Clin Psychiatry. 2006;67:1928–1935. doi: 10.4088/jcp.v67n1213. [DOI] [PubMed] [Google Scholar]
- 6.Wilson TG, Sysko RS. Frequency of binge eating episodes in bulimia nervosa and binge eating disorder: diagnostic considerations. Int J Eat Disord. 2009;42:603–610. doi: 10.1002/eat.20726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hart KJ, Ollendick TH. Prevalence of bulimia in working and university women. The Am J Psychiatry. 1985;142:851–854. doi: 10.1176/ajp.142.7.851. [DOI] [PubMed] [Google Scholar]
- 8.Reba-Harrelson L, Von Holle A, Hamer RM, Swann R, Reyes ML, Bulik CM. Patterns and prevalence of disordered eating and weight control behaviors in wmen ages 25–45. Eat Weight Disord. 2009;14:e190–e198. doi: 10.1007/BF03325116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dingemans AE, Bruna MJ, van Furth EF. Binge eating disorder: a review. Int J Obes Relat Metab Disord. 2002;26:299–307. doi: 10.1038/sj.ijo.0801949. [DOI] [PubMed] [Google Scholar]
- 10.Striegel-Moore RH, Franko DL. Epidemiology of binge eating disorder. Int J Eat Disord. 2003;34 Suppl:S19–S29. doi: 10.1002/eat.10202. [DOI] [PubMed] [Google Scholar]
- 11.Garfinkel P, Kennedy S, Kaplan A. Views on classification and diagnosis of eating disorders. Can J Psychiatry. 1996;40:445–456. doi: 10.1177/070674379504000805. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell J, Hoberman H, Peterson C, Mussell M, Pyle R. Research on the psychotherapy of bulimia nervosa: half empty or half full. Int J Eat Disord. 1996;20:219–222. doi: 10.1002/(SICI)1098-108X(199611)20:3<219::AID-EAT1>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 13.Mond J, Hay P, Rodgers B, Owen C, Crosby R, Mitchell J. Use of extreme weight control behaviors with and without binge eating in a community sample: implications for the classification of bulimic-type eating disorders. Int J Eat Disord. 2006;39:294–302. doi: 10.1002/eat.20265. [DOI] [PubMed] [Google Scholar]
- 14.Wilson G. Diagnostic criteria for bulimia nervosa. Int J Eat Disord. 1992;11:315–319. [Google Scholar]
- 15.Wilson G, Walsh B. Eating disorders in the DSM-IV. J of Abnorm Psychol. 1991;100:362–365. doi: 10.1037//0021-843x.100.3.362. [DOI] [PubMed] [Google Scholar]
- 16.Walsh BT. DSM-V from the perspective of the DSM-IV experience. Int J Eat Disord. 2007;40 Suppl:S3–S7. doi: 10.1002/eat.20397. [DOI] [PubMed] [Google Scholar]
- 17.Garfinkel P, Lin E, Goering P, Spegg C, Goldbloom D, Kennedy S, et al. Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry. 1995;152:1052–1058. doi: 10.1176/ajp.152.7.1052. [DOI] [PubMed] [Google Scholar]
- 18.Crow S, Agras W, Halmi K, Mitchell J, Kraemer H. Full syndromal vs subthreshold anorexia nervosa, bulimia nervosa, and binge eating disorder: a multicenter study. Int J Eat Disord. 2002;32:309–318. doi: 10.1002/eat.10088. [DOI] [PubMed] [Google Scholar]
- 19.Striegel-Moore RH, Wilson GT, Wilfley DE, Elder KA, Brownell KD. Binge eating in an obese community sample. Int J Eat Disord. 1998;23:27–37. doi: 10.1002/(sici)1098-108x(199801)23:1<27::aid-eat4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 20.Striegel-Moore RH, Dohm FA, Solomon EE, Fairburn CG, Pike KM, Wilfley DE. Subthreshold binge eating disorder. Int J Eat Disord. 2000;27:270–278. doi: 10.1002/(sici)1098-108x(200004)27:3<270::aid-eat3>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 21.Krug I, Casasnovas C, Granero R, Martinez C, Jimenez-Murcia S, Bulik C, et al. Comparison study of full and subthreshold bulimia nervosa: personality, clinical characteristics, and short-term response to therapy. Psychother Res. 2008;18:37–47. doi: 10.1080/10503300701320652. [DOI] [PubMed] [Google Scholar]
- 22.Delinsky SS, Latner JD, Wilson GT. Binge eating and weight loss in a self-help behavior modification program. Obesity. 2006;14:1244–1249. doi: 10.1038/oby.2006.141. [DOI] [PubMed] [Google Scholar]
- 23.Walsh BT, Sysko R. Broad categories for the diagnosis of eating disorders (BCD-ED): an alternative system for classification. Int J Eat Disord. 2009;42:754–764. doi: 10.1002/eat.20722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilfley DE, Bishop ME, Wilson GT, Agras WS. Classification of eating disorders: toward DSM-V. Int J Eat Disord. 2007;40 Suppl:S123–S129. doi: 10.1002/eat.20436. [DOI] [PubMed] [Google Scholar]
- 25.Andersen AE, Bowers WA, Watson T. A slimming program for eating disorders not otherwise specified. Reconceptualizing a confusing, residual diagnostic category. Psychiatr Clin North Am. 2001;24:271–280. doi: 10.1016/s0193-953x(05)70223-9. [DOI] [PubMed] [Google Scholar]
- 26.Grilo CM, Devlin MJ, Cachelin FM, Yanovski SZ. Report of the National Institutes of Health (NIH) Workshop on the Development of Research Priorities in Eating Disorders. Psychopharmacol Bull. 1997;33:321–333. [PubMed] [Google Scholar]
- 27.Kaye WH, Kaplan AS, Zucker ML. Treating eating-disorder patients in a managed care environment. Contemporary American issues and Canadian response. Psychiatr Clin North Am. 1996;19:793–810. doi: 10.1016/s0193-953x(05)70382-8. [DOI] [PubMed] [Google Scholar]
- 28.Attia E, Roberto CA. Should amenorrhea be a diagnostic criterion for anorexia nervosa? Int J Eat Disord. 2009;42:581–589. doi: 10.1002/eat.20720. [DOI] [PubMed] [Google Scholar]
- 29.Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG. The validity and clinical utility of binge eating disorder. Int J Eat Disord. 2009;42:687–705. doi: 10.1002/eat.20719. [DOI] [PubMed] [Google Scholar]
- 30.Hudson JI, Coit CE, Lalonde JK, Pope HG., Jr By how much will the proposed new DSM-5 criteria increase the prevalence of binge eating disorder? Int J Eat Disord. 2010 Dec;10 doi: 10.1002/eat.20890. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Andrews G, Henderson S. Unmet Need in Psychiatry. Cambridge: Cambridge University Press; 2000. [Google Scholar]
- 32.Furberg H, Lichtenstein P, Pedersen NL, Thornton L, Bulik CM, Lerman C, et al. The STAGE cohort: a prospective study of tobacco use among Swedish twins. Nicotine Tob Res. 2008;10:1727–1735. doi: 10.1080/14622200802443551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lichtenstein P, Sullivan PF, Cnattingius S, Gatz M, Johansson S, Carlstrom E, et al. The Swedish Twin Registry in the third millennium: an update. Twin Res Hum Genet. 2006;9:875–882. doi: 10.1375/183242706779462444. [DOI] [PubMed] [Google Scholar]
- 34.Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.First M, Gibbon M, Williams J, Spitzer P, Staff M. SCID Screen Patient Questionnaire (SSPQ) and SCID SCREEN Patient Questionnaire-Extended (SSPQ-X), Computer Program for Windows TM, Software Manual. Washington, D.C.: American Psychiatric Press, Inc.; 1999. [Google Scholar]
- 36.SAS Institute Inc. SAS/STAT® Software: Version 9. Cary, NC: SAS Institute, Inc; 2004. [Google Scholar]
- 37.Kendell RE, Brockington IF. The identification of disease entities and the relationship between schizophrenic and affective psychoses. Br J Psychiatry. 1980;137:324–331. doi: 10.1192/bjp.137.4.324. [DOI] [PubMed] [Google Scholar]
- 38.Ogden C, Carroll M, Curtin L, McDowell M, Tabak C, Flegal K. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 39.Neovius M, Janson A, Rossner S. Prevalence of obesity in Sweden. Obes Rev. 2006;7:1–3. doi: 10.1111/j.1467-789x.2006.00190.x. [DOI] [PubMed] [Google Scholar]
- 40.Bruce B, Agras WS. Binge eating in females: a population-based investigation. Int J Eat Disord. 1992;12:365–373. [Google Scholar]
- 41.de Zwaan M, Nutzinger D, Schoenbeck G. Binge eating in overweight women. Compr Psychiatry. 1992;33:256–261. doi: 10.1016/0010-440x(92)90050-z. [DOI] [PubMed] [Google Scholar]
- 42.de Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metab Disord. 2001;25 Suppl:S51–S55. doi: 10.1038/sj.ijo.0801699. [DOI] [PubMed] [Google Scholar]
- 43.Spitzer RL, Devlin M, Walsh TB, Hasin D, Wing R, Marcus M, et al. Binge eating disorder: a multisite field trail of the diagnostic criteria. Int J Eat Disord. 1992;11:191–203. [Google Scholar]
- 44.Tourangeau R, Smith T, editors. Collecting Sensitive Information with Different Modes of Data Collection. New York: Wiley; 1998. [Google Scholar]
- 45.Reichborn-Kjennerud T, Bulik C, Kendler K, Maes H, Roysamb E, Tambs K, et al. Gender differences in binge-eating: a population-based twin study. Acta psychiatr Scand. 2003;108:196–202. doi: 10.1034/j.1600-0447.2003.00106.x. [DOI] [PubMed] [Google Scholar]
- 46.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. [accessed May 3, 2011];American Psychiatric Association DSM-5 Development [homepage on the Internet]. On Proposed Revision Page. 2010 http://www.dsm5.org/ProposedRevision/Pages/Proposedrevision.aspx?rid=372#.