Abstract
Background
Alcohol dependence is more prevalent among those with any one of several anxiety or depressive (“internalizing”) disorders than among those in the general population. However, because internalizing disorders are highly inter-correlated, it is ambiguous whether alcohol dependence is related to internalizing psychopathology components that are: a) unique to a particular internalizing disorder (“specific”); versus b) shared across a number of internalizing disorders (“general”). To clarify this ambiguity, we employed structural equation and logistic models to decompose the specific versus general components of internalizing psychopathology and then related these components separately to alcohol dependence.
Methods
The data were based on face-to-face interviews of U.S. community residents collected in the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; N = 43,093).
Results
Both analytic approaches demonstrated that increases in the general internalizing psychopathology load are accompanied by increases in the prevalence of alcohol dependence. Once the general internalizing psychopathology load is accounted for, knowing whether a particular internalizing disorder is present or absent provides little additional information regarding the prevalence of alcohol dependence.
Conclusions
The components of internalizing psychopathology that are associated with alcohol dependence are shared and cumulative among common anxiety and depressive disorders. These findings have the potential to influence clinical and scientific conceptualizations of the association between alcohol dependence and internalizing psychopathology.
Keywords: Alcohol Dependence, Anxiety Disorders, Depressive Disorders, Comorbidity
Introduction
Epidemiological surveys show a doubling to quadrupling of the odds of being diagnosed with alcohol dependence among those with versus without any one of a number of common anxiety and affective (“internalizing”) disorders (Kessler et al., 1997). Because each internalizing disorder is considered to be an independent construct with a unique biology, psychology, course and optimal treatment (Gorman et al., 2000), it logically follows that each has a unique association with alcohol dependence. Consistent with this logic, the relationship between internalizing disorders and alcohol use disorder has typically been studied across a number of largely independent and minimally interacting research groups that “specialize” in a single internalizing disorder such as: social phobia (Thomas et al., 2008); generalized anxiety disorder (GAD) (Smith and Tran, 2007); post-traumatic stress disorder (PTSD) (Driessen et al., 2008); panic disorder (Kushner et al., 2009); and depression (Nunes and Levin, 2004).
A potentially serious flaw in this research strategy, however, stems from studies showing that most individuals identified with one internalizing disorder also meet diagnostic criteria for additional internalizing disorders; i.e., internalizing disorder are correlated (Andrews et al., 2002; Boyd et al., 1984; Brown et al., 2001; Kushner et al., 2005; Magee et al., 1996). Consider that there are 2n unique combinations that are possible for n binary (i.e., present vs. absent) disorders; e.g., there are 16, 32 and 64 possible combinations of four, five and six internalizing disorders, respectively. While uncorrelated disorders would co-occur by chance according to the disorders’ base-rates, correlated disorders co-occur at rates that significantly exceed chance (Boyd et al., 1984). This creates various configurations of shared and unique variances that are theoretically discernable in correlated disorders. However, it is presently unknown how the shared versus unique variances of correlated internalizing disorders relate to alcohol dependence.
In the present work, we sought to determine the extent to which alcohol dependence is related to components that are shared across various internalizing disorders (“general”) versus those that are unique to a single internalizing disorder (“specific”). To begin to address this issue, we established the factor structure of multiple internalizing disorders in a large nationally representative epidemiological sample. Past studies report that factor analysis of up to seven common internalizing diagnoses reliably identifies just two latent variables that explain a significant proportion of the co-variation among the diagnoses (Goldberg et al., 1987; Krueger, 1999; Krueger and Finger, 2001; McGlinchey and Zimmerman, 2007; Prenoveau et al., 2010; Slade and Watson, 2006; Watson, 2005). Further, the residuals of the factor analyzed disorders quantify the component of each that does not covary with the latent factor(s); i.e., the residuals represent the component of each disorder that is unique relative to the other disorders. Therefore, latent factor scores and their residuals generated from a set of internalizing disorders provide a practical measurement approach that can be entered into structural equation models to test specific hypotheses about the association of general versus specific internalizing psychopathology components with alcohol dependence.
As a means of cross-method validation, we also sought to employ a complementary analytic framework that does not rely on latent variables. A conceptually simple index of internalizing “density” or “load” is the count of the total number of internalizing disorders that are present, without reference to which specific internalizing disorders are present. Logistic regression analyses can then be used to determine the relative contribution of the internalizing psychopathology density/load (the count) versus the presence or absence of particular internalizing disorders in predicting alcohol dependence. We conducted both analytic approaches in parallel using 12-month and lifetime diagnoses to help distinguish between the more state-like implications of the former versus the more trait-like implications of the latter.
Method
Sample
The present work was conducted using data from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). The NESARC was designed and supervised by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and conducted by the U.S. Census Bureau Field Representatives from 2001-2002 (Wave 1) (Grant et al., 2004a). NESARC is considered to be a nationally representative sample of the non-institutionalized adult population in the United States, with 43,093 respondents in total. The NESARC sample was first weighted and then adjusted to be representative of the U.S. population for multiple socio-demographic variables, including: region of the country, gender, age, race, and ethnicity. More details on the NESARC’s complex sampling design and methodology, as well as the informed consent process, are available in the Source and Accuracy Statement for Wave 1 of the 2001-2002 NESARC (Grant et al., 2003a).
Diagnostic Assessment
The diagnostic interview used was the NIAAA’s Alcohol Use Disorder Associated Disabilities Interview Schedule – DSM IV Version (AUDADIS-IV) (Grant et al., 2001). The AUDADIS-IV is designed to be administered by lay interviewers. Diagnoses included were: alcohol dependence, major depression (unipolar), dysthymia, panic disorder with and without agoraphobia social phobia, specific phobia, and generalized anxiety disorder. The rationale for including these disorders in the present work is that they comprise the same set of disorders in most studies evaluating the latent internalizing construct (c.f., Krueger and Markon, 2006). All diagnoses were made for the past 12 months and prior to the past 12 months (relative to the interview). By combining these two diagnostic timeframes into a single variable, we created a lifetime timeframe for each diagnosis that, in addition to the 12-month diagnoses, was used in the present work. Note that panic disorder with and without agoraphobia was counted as two separate internalizing disorders to be consistent with past studies (Krueger and Markon, 2006). Finally, good to excellent estimates of reliability were obtained based upon 10% of the sample who were re-interviewed (Grant et al., 2003b).
Analytic Approach
Weighting for complex sampling
In the present paper, we used Mplus Version 5.1 for the latent variable SEM analyses. The STRATIFICATION, CLUSTER and WEIGHT options of the VARIABLE commands were used to model the weighted NESARC data. In addition, the TYPE=COMPLEX option of the ANALYSIS command was used to conjunction with the aforementioned VARIABLE commands to correct the standard errors and chi square test of model fit since the NESARC data features an unequal probability of selection (e.g., an oversampling of both Black and Hispanic households as well as young adults). For all other analyses, we used SAS (v. 9.2). Specifically, PROC SURVEYFREQ was used to calculate Chi-square tests on categorical variables and PROC SURVEYLOGISTIC was used to calculate odds ratios and 95% CIs. All estimates incorporated adjustments (Taylor series linearization) for the complex survey design employed in the NESARC survey.
Latent variable models
We employed robust weighted least squares analysis based on tetrachoric correlations for the exploratory factor analyses (EFAs) with GEOMIN oblique rotation. These factor structures were established using both 12-month and lifetime diagnoses and were established as reliable using random split half replications. Next, we fit structural models relating the latent factors identified in the EFAs to alcohol dependence while treating sex and age as covariates. Finally, we introduced the residual (relative to the latent factor) of each internalizing diagnosis into the model (i.e., a path from the residual to alcohol dependence) using the MODINDICIES option under the OUTPUT command in Mplus. The statistical significance of the addition of each residual path was determined by examining the Chi-square value with one degree of freedom representing the improvement in the fit of the model when the residual path was (vs. was not) included in the model. (Note that one-tailed tests are used since the hypothesis of an improvement in fit is being evaluated.) Finally, note that all SEM results shown are standardized and thus do not depend on how the original latent factors were identified; i.e., whether a single factor loading for each factor was fixed at one or else the factor variances were fixed at one. Nevertheless, we fixed the factor variances to be one in line with standard practice for dichotomous outcome variable factor modeling.
Logistic (manifest variable) models
We also used logistic regression analyses to examine the association of alcohol dependence to each internalizing diagnosis relative to the total count of internalizing disorders for which a given individual met diagnostic criteria. First, the count and diagnosis variables were entered separately to determine their zero-order association (i.e., odds ratio) with alcohol dependence. Next, models were tested in which the count variable was entered simultaneously with each specific diagnostic variable. This approach allowed us to distinguish predictive variance that is unique versus redundant for the count index and each specific internalizing diagnosis. As with latent models, sex and age were entered as covariates when testing all logistic models.
Results
Exploratory Factor Analyses (EFAs)
Based on the past work of Krueger and colleagues (Krueger, 1999; Krueger and Markon, 2006), we specified 1-3 factor solutions in the EFAs. Results of the EFAs for both current and lifetime samples produced 1 and 2 factor solutions; however, both analyses failed to compute a 3 factor solution because the model covariance matrices were not “positive definite.” Based on fit statistics and examination of eigenvalues, a two factor solution was chosen for both 12-month and lifetime diagnoses. For both samples, two of the seven eigenvalues were found to be larger than 1 with 55% of the variance being described by the first factor for both samples (eigenvalues = 3.88 and 3.87) with 75% and 76% of the variance in the seven diagnoses being explained by the first two factors in the current and lifetime samples, respectively.
Table 1 shows the two factor solution loadings for the EFAs using 12-month and lifetime diagnoses in the full sample as well as the random halves. Factor loadings larger than 0.40 were used to determine which diagnoses were representative of the factors. In all cases, the factor structures were very stable in finding one factor that included major depression, dysthymia, generalized anxiety disorder and panic disorder and another factor that included agoraphobia, social phobia and simple phobia. Because of the high similarity of the resulting factor structures to those identified by Krueger and Markon (2006), we retained the factor labels used by these researchers (i.e., “Distress” and “Fear” respectively).
Table 1. Exploratory Factor Analyses for Internalizing Diagnoses with Internal Replications.
| 12-Month Diagnoses | ||||||
|---|---|---|---|---|---|---|
| Whole Sample | Random Half (1) | Random Half (2) | ||||
| Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 1 | Factor 2 | |
| Major Depression |
.86 | .02 | .85 | .02 | .90 | .00 |
| Dysthymia | .90 | −.06 | .94 | −.11 | .85 | .00 |
| Panic Disorder |
.44 | .19 | .46 | .13 | .45 | .23 |
| Generalized Anxiety |
.55 | .34 | .61 | .28 | .53 | .38 |
| Agoraphobia | .01 | .84 | .09 | .77 | .00 | .86 |
| Social Phobia |
.01 | .75 | .01 | .78 | .07 | .69 |
| Simple Phobia |
−.16 | .81 | −.12 | .78 | −.16 | .80 |
| Lifetime Diagnoses | ||||||
| Whole Sample | Random Half (1) | Random Half (2) | ||||
| Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 1 | Factor 2 | |
| Major Depression |
.91 | .01 | .89 | .01 | .94 | .00 |
| Dysthymia | .89 | −.06 | .92 | −.10 | .85 | −.01 |
| Panic Disorder |
.45 | .09 | .44 | .07 | .45 | .14 |
| Generalized Anxiety |
.56 | .31 | .60 | .24 | .50 | .38 |
| Agoraphobia | .00 | .90 | .00 | .91 | −.01 | .89 |
| Social Phobia |
.10 | .68 | .05 | .72 | .13 | .65 |
| Simple Phobia |
−.02 | .72 | −.05 | .74 | .00 | .71 |
Structural Equation Models (SEMs)
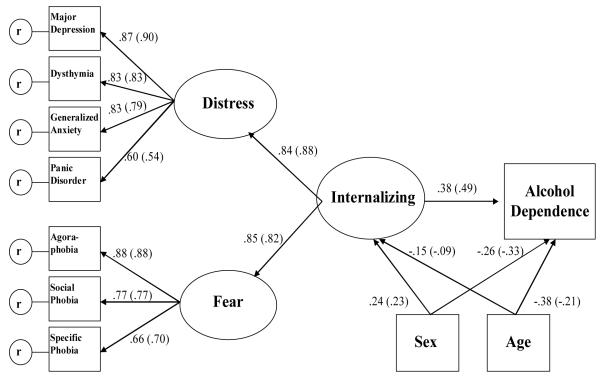
Examination of the standardized parameter estimates from the 2-factor model revealed a high correlation between the Distress and Fear factors (.70 for lifetime diagnoses and .69 for 12-month diagnoses) suggesting that both are subfactors of a higher order internalizing factor. Based on this and highly similar findings by Krueger (1999), we reparameterized the two-factor model by defining Distress and Fear as latent indicators of a higher-order “Internalizing” factor.
Figure 1 depicts SEM models having a direct path from the higher-order Internalizing factor to alcohol dependence with sex and age as exogenous covariates. 1 Although the Chi-sq tests of model fit were highly significant for both the 12-month and lifetime models (X2 = 210.138 with 24 df and X2 = 333.058 with 23 df, respectively), this test is considered to be overly sensitive when dealing with very large data sets such as the NESARC (Muthén and Muthén, 2007). Other fit statistics were good with CFI = .981, TLI =.978 and RMSEA = 0.013 for the model based on 12-month diagnoses. For the model based on lifetime diagnoses, fit indicators were comparably good with CFI = .982, TLI = .980 and RMSEA = 0.018. The R2 explained for alcohol dependence in both the 12-month and lifetime models was large (.36 and .35, respectively); i.e., approximately 1/3 of alcohol dependence outcomes were explained by the model. The Beta for the direct path from the Internalizing latent variable to alcohol dependence was also significant in both models.
Figure 1.
Structural Equation Model – 12-Month and Lifetime Diagnoses
Note: Values generated for the model using 12 month diagnoses are listed first followed in parentheses by those generated for the model using lifetime diagnoses.
Table 2 shows the standardized Betas and chi-square tests from the modification index output representing the addition of a direct path from the residual of each diagnosis (vis a vis the internalizing factors shown in Figure 1) to alcohol dependence. As can be seen, the magnitudes of the Betas for these paths are all small. In spite of their trivial effect sizes, the fit of the models were significantly improved when adding a path from the residual of 12-month major depression, panic disorder and social phobia to alcohol dependence. For the lifetime diagnoses, the fit of the model was significantly improved by adding a path from the residual of panic disorder and agoraphobia to alcohol dependence. A path from the residual of lifetime generalized anxiety disorder to alcohol dependence marginally improved the model fit (i.e., p = .06). Also note that several Betas were negative. This that the residuals of these disorders, once the internalizing factor is accounted for, are associated with a slight reduction in the likelihood of alcohol dependence. With that said, the variance accounted for by these paths were all trivially small in terms of effect size both absolutely (Cohen, 1988) and in relation to the strong positive association between the internalizing factor and alcohol dependence.
Table 2.
Modification Index Results for Diagnosis Residuals from Factors
| Distress and Fear Factor Residuals |
Path Beta |
Change in Model Fit (Chi Sq) |
Change in Model Fit Significance |
|---|---|---|---|
| Major Depression | |||
| 12-Month | .06 | 6.93 | p<.01. |
| Lifetime | .03 | 0.04 | n.s. |
| Dysthymia | |||
| 12-Month | .00 | 0.0 | n.s. |
| Lifetime | .00 | 0.05 | n.s. |
| Generalized Anxiety | |||
| 12-Month | .00 | 0.0 | n.s. |
| Lifetime | −.03 | 3.82 | p=.06 |
| Panic Disorder | |||
| 12-Month | .09 | 8.04 | p<.01 |
| Lifetime | .09 | 28.48 | p<.001 |
| Agoraphobia | |||
| 12-Month | −.07 | 2.33 | ns |
| Lifetime | −.07 | 7.94 | p<.01 |
| Social Phobia | |||
| 12-Month | −.08 | 6.77 | p<.05 |
| Lifetime | −.02 | 1.24 | n.s. |
| Specific Phobia | |||
| 12-Month | −.03 | 1.21 | n.s. |
| Lifetime | .02 | 0.83 | n.s. |
All chi sq tests had one degree of freedom and were one-tailed.
Logistic Models
The first and third data columns Table 3 show the associations (odds ratio) of each row diagnosis with alcohol dependence and for each level of the count index with alcohol dependence. The ORs for 12-month diagnoses (column 1) with alcohol dependence were all significant and ranged from a low of 2.4 (specific phobia) to a high of 4.6 (agoraphobia). Similarly for the lifetime diagnoses (column 3), all ORs are significant ranging from a low of 2.9 for specific phobia to a high of 4.0 for both agoraphobia and dysthymia. Each level of the count index was also all significant (relative to a count of zero) ranging from a low of 2.9 for a count of one 12-month diagnosis to a high of 5.5 for a count of three 12-month diagnoses and a low of 2.7 for a count of one lifetime diagnosis to a high of 8.8 for a count of four or more lifetime diagnoses. (Note that we collapsed diagnosis counts of four or greater due to the relatively low count and correspondingly increasing confidence intervals in counts greater than 4.)
Table 3.
Association of Alcohol Dependence with Specific Internalizing Disorders Before and After Including Diagnosis Count in the Model
| OR of 12-Month Alcohol Dependence with 12-Month Internalizing Diagnoses |
OR of Lifetime Alcohol Dependence with Lifetime Internalizing Diagnoses |
|||
|---|---|---|---|---|
| DIAGNOSES | Separate Entry into Models1 |
Count and Diagnosis in Model2 |
Separate Entry into Models1 |
Count and Diagnosis in Model2 |
| Depression |
3.8 (3.5-4.2) |
1.6 (1.4-1.9) |
3.7 (3.5-3.9) |
1.2 (1.1-1.3) |
| Dysthymia |
3.6 (3.0-4.2) |
1.1 (ns) (0.9-1.3) |
4.0 (3.8-4.3) |
1.1 (1.0-1.2) |
| Generalized Anxiety |
3.6 (3.1-4.2) |
1.1(ns) (0.9-1.3) |
3.4 (3.2-3.7) |
.84 (.75-.93) |
| Panic Disorder |
4.2 (3.5-5.0) |
1.5 (1.2-1.8) |
3.4 (3.2-3.6) |
1.2 (1.1-1.2) |
| Agoraphobia |
4.6 (3.6-5.8) |
1.4 (1.1-1.8) |
4.0 (3.6-4.4) |
0.97 (ns) (.85-1.1) |
| Social phobia |
2.6 (2.1-3.1) |
.49 (.39-.63) |
3.2 (2.9-3.5) |
0.90 (.80-1.0) |
| Specific Phobia |
2.4 (2.2-2.7) |
1.6 (1.4-1.8) |
2.9 (2.7-3.1) |
.93 (.87-.99) |
| COUNT | ||||
| Any one diagnosis |
2.9 (2.6-3.2) |
Median = 2.9 Range= 2.1-2.9 |
2.7 (2.6-2.9) |
Median = 2.7 Range=2.5-2.8 |
| Any two diagnoses |
3.8 (3.3-4.3) |
Median = 3.7 Range= 3.0-5.0 |
4.9 (4.6-5.3) |
Median = 4.9 Range= 4.3-5.3 |
| Any three diagnoses |
5.5 (4.4-6.9) |
Median = 5.3 Range= 3.8-8.0 |
6.2 (5.6-6.9) |
Median = 6.3 Range= 5.4-6.8 |
| Four or more diagnoses |
5.2 (4.1-6.7) |
Median = 4.4 Range= 3.2-8.0 |
8.8 (8.0-9.7) |
Median = 7.6 Range= 6.4-8.5 |
Each OR in the column was generated by a separate model that included sex and age in the first step and row diagnosis (above the horizontal break) or row count (below the horizontal break) in the second step. 95% CIs are shown in parentheses.
ORs shown in this column were generated by separate models, each including one row diagnosis and the count variable (along with sex and age). The ranges shown for the count variable in this column represent the lowest to the highest OR for the count variable from the seven separate models run along with the median OR for the count variable from the seven runs.
The data most pertinent to testing study hypotheses are shown in columns 2 and 4 of Table 3. These ORs are from models in which individual diagnoses and the count variable are entered simultaneously into the logistic models. As can be seen for the 12-month diagnoses shown in the top half of column 2, the ORs for all diagnoses are substantially reduced once the count variable is in the model, with dysthymia and generalized anxiety disorder no longer statistically significant and the OR for social phobia becoming significantly less than 1; i.e., the presence of social phobia in a model where the count is known significantly predicts the absence of alcohol dependence. As with the SEM models, the few ORs that are less than 1 are small when compared to both standard effect size benchmarks and the magnitude of the ORs for the counts in the same equations. In this regard, the substantial positive (i.e., > 1) zero-order ORs for the 12-month count variables (bottom half of column 2) are nearly unchanged by the addition of any specific diagnosis to the model. A similar pattern is evident for the lifetime diagnoses shown in the top half of column 4.
Discussion
We employed two distinct analytic approaches to evaluate the extent to which alcohol dependence is related to the unique versus shared components of a set of common internalizing disorders. Both approaches indicate that knowing the overall internalizing psychopathology load provides more information about the likelihood of having alcohol dependence than does knowing whether a particular internalizing disorder is or is not present. In this nationally representative sample, having any particular internalizing disorder (in the last 12-months or over one’s lifetime) actually provided little or no predictive information regarding the likelihood of having alcohol dependence once the level of internalizing psychopathology load was factored into the equations. These findings suggest that the strong associations found between individual internalizing disorders and alcohol dependence in multiple epidemiological and clinical datasets (Grant et al., 2004b; Kushner et al., 2000) actually reflects a recycling of essentially the same statistical association across a number of bivariate diagnostic pairings. It would appear, therefore, that the reason each internalizing disorder has been found to correlate with alcohol dependence is because they each provide a rather blunt proxy measure for the broader internalizing psychopathology load. In this regard, general internalizing load appears to be a more fundamental, informative and parsimonious construct in relationship to alcohol dependence than are the myriad internalizing disorders considered separately.
Notably, once the internalizing load variables were in the models, SEM analyses produced some negative beta weights for specific internalizing disorders and the logistic regressions produced some ORs < 1 for specific internalizing disorders. These findings should be interpreted within the context of their small (mostly trivial) effects sizes and only then within the overall predictive equations in which they are embedded. All the internalizing disorders considered in isolation are significantly positively correlated with alcohol dependence risk (e.g., see columns 1 and 3 of Table 3). However, in the models tested, the magnitude of the positive association between internalizing load and alcohol dependence overwhelms the comparatively small association (positive or negative) between the unique components of specific internalizing disorders and alcohol dependence. In other words, the strong positive association of internalizing load with alcohol dependence risk is only very slightly increased or decreased by also knowing whether a specific internalizing disorder is or is not present in the logistic models or by adding components that are unique to a particular internalizing disorder to the SEM models.
A relative strength of the latent variable approach employed includes its potential to model the full range of covariation among the internalizing disorders. This can be contrasted with the manifest (logistic) variable approach in which internalizing load was operationalized by simply counting the number of disorders present. A limitation of the logistic approach is that the relationship of the disorder count to an individual diagnosis is potentially correlated (i.e., the disorder being tested also can contribute to the count). By contrast, the latent internalizing factor and the disorder residuals are independent by definition. With this said, the conceptual and technical simplicity of the count approach can also be taken as strength relative to the conceptual and technical complexities of the latent variable approach (Borsboom et al., 2003). All of the relative strengths and weaknesses of the two approaches notwithstanding, it is reassuring that both produced essentially the same results.
Given that the 12-month and lifetime diagnostic time-frames demonstrated roughly the same pattern and strength of associations between internalizing psychopathology and alcohol dependence, we are inclined to conclude that more trait-like processes are responsible for our findings. For example, these findings are more consistent with the association of alcohol dependence to a general propensity toward experiencing a range of internalizing psychopathology than to a concentration of active internalizing symptoms occurring at a given point in time (Hettema et al., 2006).
Importantly, however, the similarity of analyses using different diagnostic time-frames does not speak directly to the nature of causal or temporal associations between the variables studied. Elsewhere, we have argued that the causal influences between internalizing symptoms and pathological alcohol use are bi-directional (Kushner et al., 1999; Kushner et al., 2000). However, our present study of whether alcohol dependence is related in a unique or general way to a range of internalizing disorders does not imply any necessary causal relationship between internalizing disorders and alcohol dependence. This focus and aim is consistent with our use of the cross-sectional NESARC (Wave 1) dataset. With that said, extensions of the work presented here could include more complex models that specify and test temporal/causal hypotheses. For example, the order of onset could moderate the degree to which general versus unique components of internalizing psychopathology correlate with alcohol dependence.
It is also important to note that we did not model some potentially interesting parameters and disorders. We had considered including psychopathological phenomena that were either broader or narrower than those included in our models. In terms of a broader focus, it has been shown that externalizing psychopathology such as anti-social personality disorder and drug abuse are correlated with both alcohol dependence and internalizing psychopathology (Krueger, 1999). In terms of a narrower focus, Markon (2010) studied the common structure of internalizing disorders from the standpoint of symptoms rather than diagnoses and others have argued that temperament and primary personality features such as neuroticism may be a unifying process linking the internalizing disorders to each other (Brown, 2007; Clark, 2005; Krueger and Eaton, 2010; Tang et al., 2009) and to alcohol dependence (Cloninger, 1987; Lahey, 2009). In fixing the scope of psychopathology in the models as we did, we attempted to maximize the relevance of our findings to the broad base of researchers and clinicians that continue to focus specifically on the association of internalizing disorders and alcohol dependence. (Brown et al., 2001; Hobbs et al. 2011; Kessler et al., 1997; Kushner et al., 2000; Nunes and Levin, 2004; Tiet and Mausbach, 2007).
The seven internalizing disorders included match the set of internalizing disorders used in the seminal work on the empirical structure of psychopathology that inspired the present project (i.e., Krueger, 1999). However, the absence of disorders such as PTSD and OCD in earlier studies may reflect their absence in several large epidemiological datasets (including NESARC, wave 1 in which the present work was conducted) more than any theoretical or substantive considerations. With that said, a limited amount of work suggests that PTSD may be distinct from other internalizing disorders in its association with latent internalizing and externalizing factors (Wolf et al., 2010). Thus, we leave it to future research to determine how internalizing disorders not included in the present work would fit into the structural models we tested. Future studies examining such issues would have the potential to extend the findings presented here in important ways.
Because this work did not focus on causal relationships (above), the implications of our findings for treatment are necessarily qualified. With that said, the thinking behind our hypotheses and the results obtained mesh well with the nascent trans-diagnostic treatment movement. It has been well known for several decades that all of the internalizing disorders are likely to be responsive to serotonergic drugs such as SSRI’s (Tang et al., 2009). More recently, innovators in the area of psychological treatments such as cognitive-behavioral therapy have made similar transdiagnostic observations (Ellard et al., 2010). Because its treatments aim at core pathological features shared across a range of internalizing disorders, the trans-diagnostic treatment approach strikes us as the appropriate place to begin the effort to link the present findings to clinical innovations
To conclude, we note that the findings reported here herald a departure from a viewpoint that we first advocated more than twenty years ago (Kushner et al., 1990). We said then: “The authors reviewed relevant…studies and conclude that the relationship between alcohol problems and anxiety appears to be variable among the anxiety disorders.” (p. 685). Since that time, the advent of the massive NESARC database, along with quantitatively intense approaches to modeling disorder covariation (Krueger, 1999; Krueger and Markon, 2006), has allowed us to take a “macroscopic” view (Börner, 2011) of comorbidity that contradicts this earlier conclusion. The empirical data presented here lead us to conclude that the components of internalizing psychopathology that are associated with alcohol dependence are shared and cumulative among common anxiety and depressive disorders.
Acknowledgments
Funding/Support: This work was supported, in part, by grant K02-AA0017886 awarded by the National Institute on Alcohol Abuse and Alcoholism to the first author (MGK).
Footnotes
The reader should note that the directionality of the arrows in the model reflects a standard graphic notation for the regression model tested and does not imply any presumed or expected causal or temporal relationships among variables in the model.
Financial Disclosure: All authors report no competing interests.
References
- Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: Data from the Australian national survey of mental health and well-being. Br J Psychiatry. 2002;181:306–314. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- Börner K. Plug-and-play macroscopes. Communications of the ACM. 2011;54(3):60–69. [Google Scholar]
- Borsboom D, Mellenbergh GJ, Heerden JV. The theoretical status of latent variables. Psychol Rev. 2003;110(2):202–219. doi: 10.1037/0033-295X.110.2.203. [DOI] [PubMed] [Google Scholar]
- Boyd JH, Burke JD, Gruenberg E, Holtzer CE, III, Rae DS, George LK, Karno M, Stoltzman R, McEnvoy L, Nestadt G. Exclusion criteria of DSM-III: A study of co-occurrence of hierarchy-free syndromes. Arch Gen Psychiatry. 1984;41:983–989. doi: 10.1001/archpsyc.1984.01790210065008. [DOI] [PubMed] [Google Scholar]
- Brown TA. Temporal and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. J Abn Psychol. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. J Abn Psycholo. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;23:410–416. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M, Kemper U, Koesters G, Chodzinksi C, Schneider U, Broese T, Dette C, Havemann-Reinicke U, TRAUMAB-Study Group Trauma and PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcohol Clin Exp Res. 2008;32(3):481–488. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cog Beh Practice. 2010;17:88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DP, Bridges K, Duncan-Jones P, Grayson D. Dimensions of neuroses seen in primary-care settings. Psychol Med. 1987;17(2):461–470. doi: 10.1017/s0033291700025022. [DOI] [PubMed] [Google Scholar]
- Gorman JM, Kent JM, Sullivan GM, Coplan JD. Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry. 2000;157:493–505. doi: 10.1176/appi.ajp.157.4.493. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDADIS-IV) National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003a;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003b. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend. 2004a;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Arch Gen Psychiatry. 2004b;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. Am J Psychiatry. 2006;163:857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hobbs JD, Kushner MG, Lee SS, Reardon SM, Maurer E. Meta-analysis of supplemental treatment for depressive and anxiety disorders in patients being treated for alcohol dependence. Am J Addict. 2011 doi: 10.1111/j.1521-0391.2011.00140.x. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Eaton NR. Personality traits and the classification of mental disorders: Toward a more complete integration in DSM–5 and an empirical model of psychopathology. Personal Disord. 2010;1(2):97–118. doi: 10.1037/a0018990. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Finger MS. Using item response theory to understand comorbidity among anxiety and unipolar mood disorders. Psychol Assess. 2001;13:140–151. [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clin Psychol Rev. 2000;20:149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL, Brekke M, Sletten SJ. Follow-Up study of anxiety disorder and alcohol dependence in comorbid alcoholism treatment patients. Alcohol Clin Exp Res. 2005;29:1432–1443. doi: 10.1097/01.alc.0000175072.17623.f8. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. Am J Psychiatry. 1990;147:685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. Am J Psychiatry. 1999;156:723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sletten S, Donahue C, Thuras P, Maurer E, Schneider A, Frye B, Van Demark J. Cognitive-behavioral therapy for panic disorder in patients being treated for alcohol dependence: Moderating effects of alcohol outcome expectancies. Addict Behav. 2009;34:554–560. doi: 10.1016/j.addbeh.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB. Public Health significance of neuroticism. Am Psychol. 2009;64(4):241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psycholo Med. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- McGlinchey JB, Zimmerman M. Examining a dimensional representation of depression and anxiety disorders’ comorbidity in psychiatric outpatients with item response modeling. J Abnorm Psychol. 2007;116:464–474. doi: 10.1037/0021-843X.116.3.464. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Statistical Analyses with Latent Variables. User’s Guide. 5th ed. Muthén & Muthén; Los Angeles, CA: 2007. Mplus. [Google Scholar]
- Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: a meta-analysis. JAMA. 2004;291(15):1887–1896. doi: 10.1001/jama.291.15.1887. [DOI] [PubMed] [Google Scholar]
- Prenoveau JM, Zinbarg RE, Craske MG, Mineka S, Griffith JW, Epstein AM. Testing a hierarchical model of anxiety and depression in adolescents: A tri-level model. J Anxiety Disord. 2010;24:334–344. doi: 10.1016/j.janxdis.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychol Med. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Smith JP, Tran GQ. Development and initial validation of the Worry Reduction Alcohol Expectancy Scale. Addict Behav. 2007;32(10):2383–2390. doi: 10.1016/j.addbeh.2007.02.005. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Hollon SD, Amsterdam J, Shelton R, Schalet B. Personality change during depression treatment: A placebo-controlled trial. Arch Gen Psychiatry. 2009;66:1322–1330. doi: 10.1001/archgenpsychiatry.2009.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas SE, Randall PK, Book SW, Randall CL. A complex relationship between co-occurring social anxiety and alcohol use disorders: What effect does treating social anxiety have on drinking? Alcohol Clin Exp Res. 2008;32(1):77–84. doi: 10.1111/j.1530-0277.2007.00546.x. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Mausbach B. Treatments for patients with dual diagnosis: a review. Alcohol Clin Exp Res. 2007;31(4):513–536. doi: 10.1111/j.1530-0277.2007.00336.x. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. J Abnorm Psychol. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Wolf EJ, Miller MW, Krueger RF, Lyons MJ, Tsuang MT, Koenen KC. Posttraumatic stress disorder and the genetic structure of comorbidity. J Abnorm Psychol. 2010;119(2):320–330. doi: 10.1037/a0019035. [DOI] [PMC free article] [PubMed] [Google Scholar]