Abstract
Objective
Homeless people have disproportionately high rates of viral hepatitis. The Gelberg-Andersen Behavioral Model for Vulnerable Populations (predisposing, enabling, and need variables) was expanded to predict prevalence and awareness of hepatitis B (HBV) or hepatitis C (HCV) infection as well as health services utilization (HSU) among homeless adults using structural equation modeling.
Design
A population-based sample of 534 homeless adults in Los Angeles’ “Skid Row” was interviewed and tested for HBV and HCV.
Main outcome measures
HBV/HCV seropositivity, awareness of seropositivity, and HSU in the previous 12 months.
Results
Seropositivity (43%), usually unknown (72% of seropositives), was predicted by injection drug use, alcohol use, older age, and risky sexual behavior. No regular source of care, risky sexual behavior, less case management, and greater age predicted not knowing one’s positive status. Health insurance, younger age, alcohol use, perceived bad health and more medical conditions predicted emergency room (ER) use; ER use was less likely among seropositives. Hospitalizations were predicted by more medical conditions and greater percentage of life homeless and were less frequent among African-Americans and males. Ambulatory visits were predicted by a regular source of care, case management, more education and perceived bad health; they were less likely among seropositives.
Conclusion
The Gelberg-Andersen Behavioral Model provided a useful guide for predicting HBV/HCV positivity as well as HSU in homeless adults. Most hepatitis-positives did not know their status and used health services less often than other homeless adults. More aggressive detection of hepatitis B and C among homeless adults is needed.
Keywords: homeless adults, hepatitis, health services utilization, Gelberg-Andersen Behavioral Model for Vulnerable Populations
The Gelberg-Andersen Behavioral Model for Vulnerable Populations (Gelberg, Andersen, & Leake, 2000) has been used in research with homeless people to explain and predict their health services utilization (HSU) and other health related behaviors (e.g., Austin, Andersen, & Gelberg, 2008; Stein, Andersen, & Gelberg, 2007; Stein, Andersen, Koegel, & Gelberg, 2000). The vulnerable-populations model is a version of the Andersen Behavioral Model (Andersen, 1968) which originally described relationships among predisposing, enabling, and need factors that are associated with HSU and access to medical care in the general population (e.g., Gruber & Kiesel, 2010; Hammond, Matthews, & Corbie-Smith, 2010). Predisposing characteristics exist prior to the perception of illness (e.g., age, education), enabling resources facilitate or impede HSU (e.g., health insurance), and need variables pertain to physical illness. The expanded vulnerable-populations model incorporates traditional Andersen model factors and also includes specific vulnerabilities common among homeless people such as substance abuse, mental illness, and competing needs that are additional barriers to obtaining health care.
U.S. rates of hepatitis B virus (HBV) and hepatitis C virus (HCV) infections are high among homeless people. In national household surveys, estimated rates for persons ever infected with HBV are about 4.7% (Wasley et al., 2010) and with HCV are about 1.6% (Armstrong et al., 2006). In contrast, prevalence rates among homeless people have been reported as high as 17% to 31% for HBV (Gelberg et al., 2001; Lum et al. 2003), and 17% to 53% for HCV (Desai, Rosenheck & Agnello, 2003; Nyamathi et al., 2002; Stein & Nyamathi, 2004). HBV and HCV can be transmitted through exchange of infected blood during injection drug use (IDU), which is prevalent among homeless people (Robertson et al., 2004). HBV and HCV are also common among individuals with incarceration histories due to IDU and unprotected sexual activity within and outside of prison (Weinbaum, Sabin, & Santibanez, 2005).
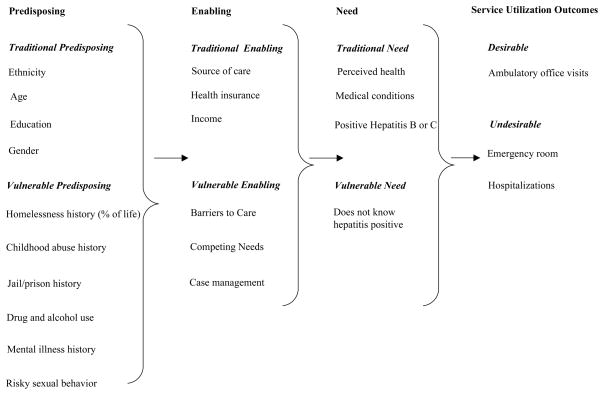
The expanded Gelberg-Andersen behavioral model is the framework we use to predict forms of HSU among homeless adults (an elaboration of previous usage) as well as to predict HBV or HCV seropositivity and lack of knowledge of one’s own positive hepatitis infection status (a new application of the Model). The behavioral model has not been used previously to assess associations between the predisposing and enabling variables and hepatitis. This study has three main objectives: (1) to report the prevalence of hepatitis B and C in a representative sample of homeless adults and to assess whether those who are positive know their status, i.e., we assess a perceived need (knowing they have hepatitis) and an evaluated need (result of testing) and the association between them]; (2) to provide an explanatory model of hepatitis infection as a function of predisposing and enabling variables; and (3) to provide an explanatory model of health services use by homeless adults as a function of the Gelberg-Andersen model domains of predisposing, enabling and need (including hepatitis infection) variables. This analysis will contribute to an understanding of health care disparities within a vulnerable population. See Figure 1 for a schematic representation of the expanded Vulnerable-Populations Model for this study, which includes specific hepatitis-related variables.
Figure 1.
Hypothesized Gelberg-Andersen Behavioral Model for Vulnerable Populations specialized for homeless populations including specific hepatitis-related variables.
Predisposing variables
As depicted in Figure 1, predisposing factors include traditional sociodemographics (gender, education, age, ethnicity) and specialized variables that reflect vulnerability (percentage of one’s adult life spent homeless, a childhood abuse history, jail or prison history, sexual risk behaviors, mental illness history, and substance use, abuse, and dependency) which are associated with HSU in both homeless and general populations (Arangua & Gelberg, 2007; Andersen & Davidson, 2007; Hammond et al., 2010; Stein, Andersen et al., 2000). Demographics are also associated with hepatitis risk. For instance, Stein and Nyamathi (2004) found that older homeless men were more likely to be HCV positive.
The vulnerable predisposing variables from the expanded Gelberg-Andersen model are relevant to homeless people. Severity of homeless history has been shown to impact numerous health problems (e.g., Stein, Lu, & Gelberg, 2000) including HCV (Stein & Nyamathi, 2004) and maladaptive HSU (Stein et al., 2007). We include childhood abuse. Homeless people often report high rates of childhood abuse, which in turn has negative effects on later health (Wechsberg et al., 2003). Homeless people are also more likely to have prison or jail histories than those in the general population (Greenberg & Rosenheck, 2008; Larimer et al., 2009). Due to the association between incarceration and hepatitis, we expect an incarceration history to predict hepatitis and also impact other variables in the model (e.g., Stein & Nyamathi, 2004). We further expect alcohol and drug use, especially IDU, to have a direct impact on HSU patterns as well as hepatitis prevalence. Risky sexual behaviors are associated with HBV, but the possibility of sexual transmission of HCV is controversial (Nyamathi et al., 2002). We expect risky sexual behaviors to impact hepatitis infection. Homeless adults with mental disorders are more likely to report barriers to needed medical care than other homeless adults (Gelberg & Linn, 1988). Thus, we include a history of mental illness among the vulnerable predisposing variables.
Enabling variables
Traditional enabling variables include health insurance, a regular source of health care, and income, which we expect to predict more use of ambulatory services, the most desirable form of care in terms of patient outcomes and economic considerations. Homeless-specific variables include perceived barriers to obtaining health care, competing needs, and having case management, and they are also expected to impact HSU. Barriers to care and competing needs, such as struggles for shelter and food, lead to delays in seeking care and may precipitate reliance on acute care (Gelberg, Gallagher, Andersen & Koegel, 1997; Kushel, Gupta, Gee, & Haas, 2006). Lewis, Gelberg, and Andersen (2003) found that unmet needs for medical care were associated with barriers such as long office waiting times and not knowing where to go for care. Lewis et al. (2003) found that the odds of unmet needs were lower among individuals with a regular source of care, although health insurance was not related to unmet or competing needs. We further hypothesize that using case management will facilitate better HSU. Sadowski, Kee, VanderWeele and Buchanan (2009) reported that homeless individuals offered housing and case management services had fewer hospitalizations, hospital days and emergency department visits compared with a usual-care group that was not offered housing and case management. Horvitz-Lennon et al. (2009) reported ethnic disparities in case management services. Our model also will identify any ethnicity-related disparities in the use of case management services. Finally, we expect that hepatitis-related variables (specifically, knowledge of infected status) will be more likely among adults with access to a regular source of care and health insurance.
Need variables
Traditional need variables include perceived poor health and specific health conditions (other than hepatitis) in the current study. We also include HBV or HCV infection separately as a need variable. The vulnerable need variable is represented by not knowing one’s seropositivity status, which endangers health by delaying vital medical treatment and monitoring and by increasing transmission risk. The Vulnerable-Populations Model assumes that the direction of relationships between HSU (i.e., appropriately realized access to care) and the predisposing and enabling variables will be the same for evaluated and perceived need (in this case, for both hepatitis infected status and knowledge of that status). For instance, more education and having a regular source of care may lead not only to better utilization but also to less hepatitis and a greater likelihood of knowing one’s infected status (evaluated and perceived need), although we would expect perceived status would be more closely related to evaluated status for persons with higher education and a regular source of care.
Outcome variables
Some forms of HSU are more desirable than others, such as obtaining preventive care in an outpatient setting so that health problems can be dealt with earlier and more effectively (Stein et al., 2007). Less desirable HSU includes reliance on ERs or hospitalizations for problems that could have been addressed more easily and earlier by timely outpatient office visits. The model assesses the relative impact of the traditional and vulnerability-specific variables on these three types of HSU: more desirable outpatient office visits and less desirable ER and hospitalizations. Based on prior findings, we expect the need variables of medical conditions and perceived poor health to drive HSU because homeless people have less opportunities for preventive health visits in the absence of illness. In addition, we expect that the traditional- and vulnerable-model enabling variables will be relevant for HSU as well.
Method
Participants
Participants were recruited for a community-based probability survey of homeless adults (age 18 or older) living in the downtown “Skid Row” area of Los Angeles in 2003–2004. The final sampling frame consisted of 41 sites: 19 shelter programs at 10 locations and 22 meal programs at 9 locations. Homeless participants were identified by having spent the previous night either (1) in a public or private shelter, or (2) on the “streets” (in a public or private place not designed for or ordinarily used as regular sleeping accommodations for humans). Additional eligibility criteria included a minimum level of cognitive competence and English fluency. Only an estimated 5% of the sample were monolingual Spanish speakers. As needed, the 6-item Short Blessed Test was used to assess cognitive competence (Katzman et al., 1983).
The study employed a conventional two-stage representative sampling design to select homeless adults from shelters and meal programs. First, the sampling frame was stratified by site using site-days as sampling units. Second, selection of subjects employed either simple random sampling or systematic random sampling strategies tailored to each site. One site refused to participate, giving a site refusal rate of 1/41 or 2%. Of the 903 persons sampled from remaining sites, 588 were identified as eligible for interview. Of these, 41 refused to be enrolled in the study, 10 were later identified as repeaters, 1 could not be located, 1 had a language barrier, and 1 interview was discarded due to concern about client credibility. The combined screening and interview completion rate was 83%; the final study sample was 534 adults. The racial/ethnic makeup of the sample was 10% Hispanic/Latino, 16% White, 72% African-American, and 2% other ethnicities. Nearly 80% percent of the sample was male; the average age was 46 years.
Interviews were conducted by the RAND Survey Research Group. Eligible adults were interviewed using a face-to-face computer-assisted questionnaire that included mental health and substance abuse modules from a shortened version of the Diagnostic Interview Schedule–IV (DIS-IV) (Robins, Cottler, Bucholz, & Compton, 2000). Blood serum was tested for HCV, HBV, and HIV. Data collection averaged 90 minutes per person for which participants were compensated $30. Participants were given appointments to return one week later for test results and referrals. Participants who returned were paid $10. If necessary, they could call for results but would not receive the incentive. After three months of fieldwork, payment was raised to $25 to increase the return rate. The overall rate of notification of test results was 92%. The study was approved by the Institutional Review Boards of UCLA, the Public Health Institute, and the RAND Corporation.
Measures
Single-item variables, composites, and multiple-indicator latent variables were indicators of the variables representing the domains of the expanded Gelberg-Andersen model.
Predisposing variables
Traditional predisposing variables
One dummy variable represented ethnicity (African-American = 1 vs. 0 = all others). Hispanic ethnicity was not significantly associated with any outcome variable and was not included. A general minority ethnicity variable also was also tested but was not associated with the other model variables. Continuous variables of age (from 20–72 years) and education (3–17 years) were included. Gender was coded 1 = female, 2 = male.
Vulnerable predisposing variables
Percent of adult life homeless was based on the percentage of their lives spent homeless after age 18. Childhood Abuse History was a latent variable indicated by 2 items: 1) whether they had been hit, beaten, burned, or hurt by someone they lived with before they turned 18; and 2) whether they had been made to have sex against their will before they turned 18. Incarceration history was dichotomous (no history = 0, jail or prison = 1). Alcohol use was a latent variable based on 1) How many days they drank 5 or more drinks in the previous 30 days ( “binge” drinking), 2) frequency of binge drinking in the previous 12 months (once or more per month vs. less than once per month), and 3) classification as alcohol dependent using DSM-IV criteria (Robins et al., 2000). Drug use was indicated by the mean of 3 parcels of 9 drug use items (coefficient α = .72) scaled from 0 (never used), 1 (more than 12 months ago), 2 (in the previous 12 months but more than 30 days ago), to 3 (in the previous 30 days). The drugs included marijuana, heroin, street methadone, opiates, sedatives, crack cocaine, cocaine, hallucinogens, and speed. Other measured variables represented injection of illegal drugs (IDU, yes/no), and classification as drug dependent based on DSM-IV diagnostic criteria (Robins et al., 2000). Mental illness history was represented by a dichotomous variable that indicated one or more overnight hospitalizations for mental health problems. Risky sexual behavior was a latent variable indicated by a history of trading: 1) sex for cash, and 2) sex for drugs. Other items such as regular condom use were not significant predictors and were not included.
Enabling variables
Traditional enabling variables
Regular source of care was assessed by: “Is there one place in particular, like a doctor’s office or clinic, where you go when you are sick or need advice about your health?”(yes = 1, no = 0). Health insurance was assessed with a single item: “In the past 12 months, were you covered at any time by health insurance or medical coverage?” (yes = 1, no = 0). Income was based on respondent report of total monies received over the past 30 days (mean = $375; standard deviation = $415.50). This variable was not retained in the model because it had no significant impact on any other model variable.
Vulnerable enabling variables
Barriers to care was a latent variable with 3 indicators that were each the sum of “yes” answers to 9 types of barriers to health care that the participant may have encountered in 3 situations (yes = 1, no = 0): 1) when attempting to receive medical care (coefficient α = .85); 2) when attempting to receive care for mental problems (α = .86); and 3) when attempting to receive treatment for alcohol or drug use (α = .86). Items include: “You didn’t know where to go,” and “It takes too long to travel to the treatment site.” Competing needs was indicated by 4 items scaled from “never” (0) to “always” (4) that assessed how often in the past 30 days it was a problem 1) Getting a place for the night; 2) Getting food to eat; 3) Finding a place to wash up, and 4) Finding a place to go to the bathroom” (α = .76). Case management was indicated by 2 yes/no items: 1) Whether any service programs were working with them to help them get on their feet (including shelters, drop-in centers, or other service programs), and 2) Whether they had a case manager, counselor or advocate who handled things for them.
Need variables
Traditional need variables
Perceived bad health was a latent variable indicated by 4 items from the SF-12 (Ware & Sherbourne, 1992): 1) The degree to which pain interfered with a participant’s normal activities in the previous 4 weeks [1 (not at all) to 5 (extremely)]; 2) a subjective rating of personal general health [excellent (1) to poor (5)]; 3) a mean of responses to 2 items that assessed whether during the past 4 weeks they had accomplished less than they would like as a result of their physical health and whether their physical health limited the kind of work or other regular activities they do; 4) the mean of 2 problems with physical function including a) moderate activities such as moving a table and b) climbing several flights of stairs; [”a lot” (3), “a little” (2), to “not at all” (1)]. Conditions was the sum of 10 possible serious health conditions that they reported ever having (not including hepatitis) such as a heart attack, cancer, or tuberculosis. HBV or H CV seropositivity was a yes/no variable that was based on objective blood screening for history of presence of either virus (43% tested positive [47% of the males, 31% of the females]; 31% tested HBV seropositive, 28% tested HCV seropositive; 16% tested seropositive for both). Blood samples were tested for the hepatitis B core antibody and hepatitis B surface antigen, with confirmation using the neutralization assay. HBV seropositivity was determined if the participant tested positive for either or both tests. Blood samples were tested for HCV antibodies using a second-generation enzyme-linked immunosorbent assay (ELISA). Per Centers for Disease Control recommendations, only ELISA tests with a signal-to-cut-off ratio < 3.8 required confirmation. These tests were confirmed using a supplemental recombinant immunoblot assay (RIBA, 3.0) (Alter, Kuhnert & Finelli, 2003).
Vulnerable need variable
Does not know hepatitis-positive was based on whether participants reported being told that they had been infected with HBV or HCV. Participants who tested positive for HBV or HCV, but who reported no knowledge of their positive status, were given a 1 (31% of entire sample; 72% of positives did not know their status). Otherwise, they received a zero. Those who did not test positive for either HBV or HCV were also given a zero.
Outcome utilization measures
HSU items included the use of ERs, Hospitals, and Ambulatory office visits. ER use was based on 1 item: “In the past 12 months, how many times, if any, did you go to an emergency room for any health reason?” Hospital visits were assessed by: “In the past 12 months, how many times, if any, were you hospitalized overnight for a physical problem.” This item excluded hospitalizations for mental problems or substance use problems. Ambulatory office visits were based on 1 item: “In the past 12 months, how many visits did you make to a doctor or nurse practitioner for a physical health problem. Do not count times when you only picked up medication or when you saw a doctor when you were hospitalized.”
Analysis
The analyses were performed using the EQS structural equations program (Bentler, 2006). Goodness-of-fit was assessed with the maximum-likelihood χ2 statistic (ML χ2), the Comparative Fit Index (CFI), and the root mean squared error of approximation (RMSEA). The CFI ranges from 0 to 1 and reflects the improvement in fit of a hypothesized model over a model of independence among the measured variables. Values at .95 or greater are desirable, indicating that the hypothesized model reproduces 95% or more of the covariation in the data. The RMSEA is a measure of fit per degrees of freedom; values less than .06 are desirable.
A confirmatory factor analysis (CFA) tested the adequacy of the hypothesized measurement model and provided bivariate associations among the model variables. We allowed a correlation between IDU and hepatitis B or C positivity a priori because we expected that IDU, a measured indicator of the latent variable of Drug Use, would be associated with hepatitis. After minor modification to this model based on plausible suggestions from the LaGrange Multiplier (LM) test (which reports supplementary modifications to the original model that will improve the fit), we tested a saturated predictive path model that positioned all predisposing variables as predicting the enabling variables, all of the predisposing and enabling variables predicting the need variables, and all the predisposing, enabling, and need variables predicting the HSU variables. Relations that were significant among the predisposing variables were also retained in this model as within-domain correlations, and significant correlations among the residuals of the intermediate and outcome variables were also allowed. Nonsignificant paths and correlations were trimmed gradually. Indirect effects were also examined as evidence of possible mediation between the predictor and outcome variables.
Results
Confirmatory Factor Analysis
After minimal model modification, the final CFA model was acceptable: ML χ2 = 766.23, 495 df; CFI = .95, RMSEA = .03. All factor loadings were significant (p < .001) indicating that the model was plausible. Table 1 presents summary statistics including the factor loadings, means, and standard deviations of measured variables. Four correlated error residuals (as suggested by the LM test) were added between some of the drug items and some of the alcohol items (e.g., monthly binge drinking, yearly binge drinking). As expected, IDU was correlated with hepatitis. The table of correlations among the variables in the model is large (23 X 22) and is not presented in the interest of saving space. (The table is available upon request.)
Table 1.
Summary statistics of measured variables in the Gelberg-Andersen Behavioral Model for Vulnerable Populations health care utilization model (N = 534 homeless adults in the Skid Row area of Los Angeles, 2003–2004).
| Variables (range) | Mean or % | SD | Factor Loadinga |
|---|---|---|---|
| Predisposing | |||
| African American | 72% | — | |
| Age (years) | 45.96 | 10.32 | — |
| Education (years) | 11.91 | 2.11 | — |
| Male gender | 79% | — | |
| Mean % of adult life homeless | 9.91 | 12.04 | — |
| Childhood Abuse History | |||
| Physical abuse | 37% | .63 | |
| Sexual abuse | 12% | .43 | |
| Jail/Prison History | 77% | — | |
| Alcohol Use | |||
| Binge (12 month) (yes/no) | 70% | .78 | |
| Days last month:5 drinks or more | 1.97 | 5.60 | .62 |
| Dependency diagnosis DSM-IV | 29% | .66 | |
| Drug Use | |||
| Drug Composite 1 | 0.69 | 0.56 | .72 |
| Drug Composite 2 | 0.21 | 0.43 | .51 |
| Drug Composite 3 | 0.81 | 0.69 | .81 |
| IDU lifetime | 21% | .55 | |
| Dependency diagnosis DSM-IV | 34% | .56 | |
| Mental hospital admission lifetime | 19% | — | |
| Risky Sexual Behavior lifetime | |||
| Sex for cash | 22% | .82 | |
| Sex for drugs | 16% | .65 | |
| Enabling | |||
| Regular source of care | 65% | — | |
| Health insurance | 42% | — | |
| Barriers to Care (0–9) | |||
| Physical health | 0.48 | 1.38 | .47 |
| Mental health | 0.46 | 1.40 | .59 |
| Alcohol or drug treatment | 0.31 | 1.28 | .52 |
| Competing Needs (0–4) | |||
| Place to sleep | 1.36 | 1.42 | .52 |
| Get food | 0.66 | 1.08 | .64 |
| Place to wash up | 0.91 | 1.26 | .84 |
| Place to use bathroom | 1.21 | 1.43 | .69 |
| Case management | |||
| Service program | 38% | .89 | |
| Case manager | 32% | .98 | |
| Need | |||
| Perceived Bad Health (1–5) | |||
| Pain | 2.28 | 1.35 | .77 |
| General health | 3.07 | 1.21 | .56 |
| Role limitations | 0.45 | 0.47 | .71 |
| Functional limitations | 1.60 | 0.70 | .68 |
| Medical Conditions (0–7) | 0.87 | 1.14 | — |
| Hepatitis B or C positive | 43% | — | |
| Does not know hepatitis-positive | 31% | — | |
| Utilization past 12 months | |||
| # Emergency Room visits | 0.92 | 2.44 | — |
| # Hospitalizations | 0.59 | 4.40 | — |
| # Ambulatory Office Visits | 1.45 | 4.68 | — |
All factor loadings significant, p ≤ .001.
Focusing on bivariate relationships with the hepatitis-related variables, testing positive for HBV or HCV was significantly associated with: predisposing variables of African American ethnicity, male gender, greater age, less education, greater percent of life homeless, a childhood abuse history, an incarceration history, drug and alcohol use, IDU, risky sexual behavior, the enabling variable of more competing needs, and the need variables of perceived poor health and medical conditions. Testing positive was significantly associated with fewer office visits. Not knowing one’s positive status was significantly associated with predisposing variables of greater age, less education, risky sexual behavior, and drug use, and the enabling variables of a regular source of care (negatively), more competing needs, and less case management. Regarding HSU, ER use in the past year was significantly associated with not knowing one’s infected status (negatively), female gender, childhood abuse, alcohol use, a mental illness history, a regular source of care, health insurance, perceived bad health, and more medical conditions. Hospitalizations were associated with non-African-American ethnicity, more education, female gender, percent of life homeless, and more medical conditions. Office visits in the previous year were significantly associated with a regular source of care, having a case manager, perceived bad health, and more medical conditions, and negatively with not knowing one’s infection status.
Path analysis
The final trimmed path model had excellent fit statistics: ML χ2 = 921.09, 658 df, CFI = .95, RMSEA = .03. Table 2 presents the significant paths in the predictive model. A correlation suggested by the LM test was added between male gender and less sexual abuse (one indicator of childhood abuse). Not all significant correlations in the CFA remained significant predictors in the path model. Regarding study outcomes, seropositivity was significantly predicted by the predisposing variables of greater age, alcohol use, IDU, and risky sexual behavior. Not knowing one’s hepatitis-infected status was predicted by predisposing variables of greater age and risky sexual behavior and enabling variables of not having a regular source of care, and less case management. ER visits in the prior 12 months were significantly predicted by items in all domains including younger age, alcohol use, health insurance, perceived bad health, and more medical conditions. Less use of ERs was predicted by seropositivity. Hospitalizations in the prior 12 months were predicted by female gender, more medical conditions, and a greater percentage of life homeless; hospitalizations were less likely among African Americans. Office visits in the prior 12 months were predicted by a regular source of care, case management, more education, and perceived bad health. However, visits were less likely among those testing positive for Hepatitis B or C, who averaged less than 1 visit in the prior 12 months compared to nearly 2 visits by the other participants. Other significant predictive relations among the elements of the Vulnerable-Populations Model can be seen in Table 2, including predisposing predictors of enabling variables, and predisposing and enabling predictors of the need variables. Of note, age and gender were important predictors of enabling and need variables.
Table 2.
Significant paths in predictive model (N = 534 homeless adults in the Skid Row area of Los Angeles, 2003–2004).
| Outcome Variables | Significantly Predicted by: | Standardized Regression coefficient |
|---|---|---|
| Enabling variables | ||
| Regular source of care | African-American | .08* |
| Age | .12** | |
| Male | −.12** | |
| Health Insurance | Age | .13** |
| Male | −.11* | |
| Mental illness history | .10* | |
| Barriers to Care | Childhood Abuse History | .23*** |
| Alcohol Use | .33*** | |
| Competing Needs | Percent of Life Homeless | .19*** |
| Drug Use | .18*** | |
| Case Management | Age | − .08* |
| Male | −.13*** | |
| Percent of Life Homeless | −.13*** | |
| Mental illness history | .10* | |
| Need | ||
| Perceived Bad Health | Regular source of care | .08* |
| Barriers to Care | .27*** | |
| Competing Needs | .23*** | |
| Age | .23*** | |
| Education | −.15*** | |
| Male | −.21*** | |
| Medical Conditions | Regular source of care | .19*** |
| Health insurance | .12** | |
| Age | .19*** | |
| Male | −.21*** | |
| Childhood Abuse History | .14*** | |
| Alcohol Use | .17*** | |
| Hepatitis B or C | Alcohol Use | .09* |
| Age | .23*** | |
| Risky Sexual Behavior | .12** | |
| IDU | .29*** | |
| Does not know hepatitis-positive | Regular source of care | −.06* |
| Risky Sexual Behavior | .19*** | |
| Age | .21*** | |
| Case Management | −.04* | |
| Health Care Utilization, past 12 months | ||
| # Emergency Room visits | Alcohol Use | .11* |
| Health Insurance | .15*** | |
| Perceived Bad Health | .20*** | |
| Hepatitis B or C | −.10* | |
| Medical Conditions | .23*** | |
| Age | −.12** | |
| # Hospitalizations | Medical Conditions | .08* |
| African-American | −.09* | |
| Male | −.10* | |
| Percent of Life Homeless | .11** | |
| # Ambulatory Office Visits | Regular Source of Care | .11** |
| Case Management | .11** | |
| Perceived Bad Health | .18*** | |
| Hepatitis B or C | −.09* | |
| Education | .09* |
p ≤ .05,
p ≤ .01,
p ≤ .001
Indirect effects
Indirect effects of predisposing variables on need variables include the following. Bad health was indirectly impacted by a greater percentage of life homeless, more childhood abuse, drug use and alcohol use. There were indirect effects of age and female gender on more medical conditions. Greater age and drug use impacted seropositivity. Not knowing one’s seropositivity was significantly impacted indirectly by male gender. These effects were mediated by the enabling variables that directly predicted the need variables as reported in Table 2. As far as HSU is concerned, some indirect effects of the predisposing and enabling variables are not meaningful or are spurious because the mediators are poor health or more medical conditions which in turn predicted greater use of services. For instance, poor health items were predicted by more problematic variables such as more childhood abuse, competing needs, and barriers to care. If the direct relationship is significant and opposite from the indirect effect, the indirect effect is not reported. Several significant indirect effects on HSU were observed. ER use was indirectly impacted by predisposing variables of greater age, less education, female gender, a greater percentage of life homeless, childhood abuse, alcohol use, and mental illness. It was also impacted by having a regular source of care, health insurance, and more barriers to care. Office visits were indirectly predicted by female gender. There were no significant indirect effects on Hospitalizations.
Discussion
We outlined three objectives in using the expanded Gelberg-Andersen behavioral model. First, we wanted to assess the prevalence of hepatitis B and C in a representative sample of homeless adults and assess whether those who tested positive knew they were infected. Forty-three per cent of the sample tested positive for HBV or HCV or both: 31% were HBV positive, 28% were HCV positive, and 16% were positive for both. Importantly 71% of those testing positive did not know they were positive.
Our second goal was to test a model of HBV and HCV infection and awareness of infection, conceptualized as need variables as a function of predisposing and enabling variables. Infection was related most strongly to predisposing variables associated with hepatitis risk in all populations: alcohol use, IDU, age, and risky sexual behaviors. In addition to the predisposing variables of risky sexual behavior and age, not knowing one’s infection status was negatively predicted by enabling variables of case management and having a regular source of care.
The third goal was to provide an explanatory model of health services use by homeless adults as a function of the Gelberg-Andersen model domains of predisposing, enabling and need variables augmented with the hepatitis-specific variables. As a unique contribution of this study, we found that seropositive people were less likely to report ambulatory office visits or even ER use, which is less desirable but at least exposes an individual to the health care system at some level. People infected with HBV or HBC are in need of screening, evaluation, monitoring, continuing care, and hepatitis-related education. Further, more attention to seropositive people might reduce transmission risk since patients might change their behavior if they learn they are infected. In this population, even an ER visit may be “better than nothing” and present a screening opportunity for seropositivity. In addition, significant associations were noted in the path analysis between not knowing one’s hepatitis infection status and not having a regular source of care or case management. Establishing supportive links between homeless persons and the health care system would help with appropriate management of those that are seropositive and may not know it.
Traditional predisposing variables were generally as important in predicting HSU with homeless adults as they are in general population. However, among these homeless adults, minority ethnicity did not predict negative HSU outcomes. African-Americans were more likely to have a regular source of care and had fewer hospitalizations in the past 12 months than those of other ethnicities in this study. Similar results have been found among homeless women by Stein et al. (2007), Austin et al. (2008) and Gelberg et al. (2009). Stein et al. (2007) hypothesized that the homelessness of the African-American women may have been based more on loss of affordable housing, lack of family supports, and extreme poverty rather than associated with mental illness and substance use that are found more often among white homeless women. This situation may extrapolate to both homeless men and women. Income was not important in this model, perhaps because most homeless are poor; also, their income can vary widely from month to month, making its predictive utility in any one month minimal.
Men, as compared to women, generally reported more substance use and higher rates of hepatitis but fewer enabling resources to get care including less case management and a lower likelihood of having a regular source of care or insurance. Women, as compared to men, reported poorer health, more health conditions, and more hospitalizations. However, despite their greater reported health needs, women did not report more office visits than the men.
As in the general population, age was important for health-related outcomes. Although older homeless adults were more likely to have a regular source of care and insurance, they were less likely to have case management and more likely to report bad health and medical conditions. They were more likely to test positive for hepatitis and less likely to know that they were HBV or HCV positive. Despite greater medical needs and better access to care, older age did not predict more ambulatory office visits, and older adults were less likely to use an ER for their exigent needs. More outreach to older homeless adults appears warranted, including targeting them for hepatitis screening. More education predicted more office visits and better health.
Among vulnerability-specific predisposing variables, there was a significant direct influence of childhood abuse on barriers to care and more medical conditions. Childhood abuse was also significantly associated with other predisposing variables of percent of life homeless, having a jail/prison history, drug and alcohol use, risky sexual behavior, and mental illness. These results reinforce and expand the findings of Wechsberg et al. (2003) who reported that childhood abuse is associated with later stress-filled lives and drug use among homeless people. Abuse also has an impact on health-related outcomes including illnesses and difficulties negotiating the health care system. A more severe homeless history predicted more competing needs, less likelihood of receiving case management, and more hospitalizations. Thus, people who have suffered proportionately more time homeless may be the least effective at connecting with case management and health-related services as they often resorted to hospitalizations, the least discretionary and most expensive form of care. Surprisingly, homelessness history severity did not directly predict hepatitis seropositivity or lack of knowledge of infected status. Stein and Nyamathi (2004) found a significant and positive relationship between severity of homelessness and HCV positivity. Although an incarceration history was not a significant predictor in the path model, it had significant bivariate associations with male gender, more alcohol and drug use, more mental illness, more risky sexual behavior, and more competing needs. Its association with the outcomes was probably attenuated by its associations with other more potent predictors of the outcomes. Historically, incarceration has been a risk factor for hepatitis (e.g., Weinbaum et al., 2005; Stein and Nyamathi, 2004).
A regular source of care predicted poorer health, more medical conditions, more recent office visits, and a greater likelihood of knowing their HBV/HCV-infected status. It is likely that among homeless adults, medical conditions and poorer health may predict having a regular source of care as much as the reverse influence as specified in the model. Clearly, a regular source can provide the continuous and comprehensive care needed to identify and treat health problems. Having health insurance predicted more ER use and more medical conditions. Exigent care for homeless people may be provided more readily when they are insured, and they may be more likely to go to an ER when they have insurance. This finding is similar to one reported by Stein et al. (2007) among a younger sample of women. It was speculated that poor women with illnesses were more likely to qualify for public insurance which may also be the case in this broader sample of men and women with a wider range of ages. Also, participants may have perceived the ER as their regular source of care.
Vulnerable enabling factors of barriers to care and competing needs played only an indirect part in this model because neither directly predicted HSU. These items predicted more Perceived Bad Health. Case management was facilitative. Those who had case management were more likely to know that they were positive for hepatitis and also to make ambulatory office visits. This variable reflects some connectedness to community social services.
In this sample of homeless adults, need was driving HSU. Poor health and medical conditions (other than hepatitis seropositivity) were the strongest predictors of use of emergency services. Alcohol use also predicted more ER use. These chronic conditions would be treated better if homeless adults had greater use of non-emergency services and received preventive screenings, continuity of care, and alcohol treatment in more appropriate settings. Not surprisingly, hospitalizations were predicted by serious medical conditions, and office visits were predicted by perceived bad health. The more desirable ambulatory office visits were facilitated by enabling factors of a regular source of care and case management.
Limitations
This study tested the Vulnerable-Populations Model, which posits a particular directionality of influence in HSU (Andersen, 1968; Gelberg et al., 2000). Alternative predictive associations are always possible when data are cross-sectional. Certainly, having a regular source of care does not “cause” more illness, although it can increase diagnoses of existing illnesses. Further, homeless adults with illnesses may be more likely to have medical care available to them. Further, prior utilization could have led to knowledge of seropositivity. However, although most of the sample with hepatitis probably became infected years ago, and only a minority knew their status. Another limitation is that our findings rely on self-reports (except for HBV/HCV status), and self-reported data are subject to recall bias or other errors. However, prior research using chart reviews to compare with self-report indicated that homeless persons were surprisingly accurate in reporting their use of health services (Gelberg & Siecke, 1997). We used percent of adult life homeless which may have underestimated total lifetime homelessness; we did not have access to data on length of homelessness during childhood. However, only 7% of the sample reported experiencing homelessness before the age of 18. Furthermore, although our sample from Skid Row in Los Angeles was carefully and probabilistically derived from many community sources, our findings may not generalize to other homeless adults in other geographical areas. Of Los Angeles County’s estimated homeless population of nearly fifty thousand in 2009 (the largest in the nation), about 5000 are located in downtown Los Angeles (Los Angeles Homeless Services Authority (LAHSA), 2009). In the downtown population, about 46% are sheltered. This corresponds closely with the data from the current study assessed a few years earlier in which 44% were sheltered. In greater Los Angeles County about 33% of homeless people are sheltered. The relatively high sheltered proportion in Metro LA is largely due to the high number of homeless service providers operating emergency and transitional housing in Skid Row (LAHSA, 2009).
Conclusion
Based on our findings, outreach among homeless adults may need to include efforts that provide continuous and comprehensive medical care that addresses multiple and complex health problems. One obvious example of enhancing medical services is related to HBV and HCV detection, which would include screening homeless adults for hepatitis, especially those who are injection drug users. For those testing positive for HBV or HCV, follow-up visits and monitoring may help prevent transmission as well as help the infected adult avoid alcohol and drug use and other risk behaviors for progressive liver disease. For those testing negative, patient education may help prevent exposure by reducing high-risk behaviors, and eligible persons could be encouraged to be vaccinated against HBV (e.g., Nyamathi et al., 2009). Timely treatment might capture various medical problems before they become so serious that hospitalization or over-reliance on burdened emergency rooms is required (U.S. Department of Health and Human Services [USDHHS], 2003). Permanent supportive housing for homeless people combined with in-house medical programs would be helpful as well (Larimer et al., 2009; National Alliance to End Homelessness [NAEH], 2007). Changing housing and health policies to prevent homelessness in the first place among populations at risk would be a pivotal change that would provide a benefit to the health of our society as a whole (NAEH, 2007; USDHHS, 2003).
Acknowledgments
Support for this research was provided by grants P01-DA01070-37 from the National Institute on Drug Abuse (NIDA; J.S.), and RO1-DA14294 from NIDA (L.G., M.R. and R.M.A.) and the Centers for Disease Control (L.G. and M.R.). Dr. Andersen is Wasserman Professor Emeritus, UCLA School of Public Health and received support from UCLA/DREW Project EXPORT, NCMHD, P20MD001148/P20 MD000182 and the UCLA Center for Health Improvement of Minority Elderly/ Resource Centers for Minority/Aging Research, NIH/NIA under Grant P30AG 021684. Lillian Gelberg received support as a Robert Wood Johnson Foundation Generalist Physician Faculty Scholar and as the UCLA George F. Kneller Chair in Family Medicine. Marjorie Robertson received support from the National Alcohol Research Center (P60-AA05595) at the Alcohol Research Group, Public Health Institute. We thank Judith Perlman and Kirsten Becker of the RAND Corporation for their substantial contribution to the design and implementation of this study and to their exceptional fieldwork staff. We thank Katherine Davenny at the National Institute on Drug Abuse, and Miriam Alter and Cindy Weinbaum of the Centers for Disease Control for their support and guidance on this project. We also thank Ellen Silk and Gisele Pham for their administrative support. Correspondence regarding this article should be addressed to Judith A. Stein, Department of Psychology, 1285 Franz Hall, University of California, Los Angeles, CA 90095-1563.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
Contributor Information
Judith A. Stein, Department of Psychology, University of California, Los Angeles
Ronald M. Andersen, Department of Health Services, UCLA School of Public Health
Marjorie Robertson, Alcohol Research Group, Public Health Institute, Emeryville, California.
Lillian Gelberg, Department of Family Medicine, David Geffen School of Medicine at UCLA, and Department of Health Services, School of Public Health, University of California, Los Angeles.
References
- Alter MJ, Kuhnert WL, Finelli L. Guidelines for laboratory testing and result reporting of antibody to hepatitis C virus. MMWR. 2003;52:1–16. [PubMed] [Google Scholar]
- Andersen R. Center for Health Administration Studies Research Series. Chicago: University of Chicago Press; 1968. A behavioral model of families’ use of health services. [Google Scholar]
- Andersen R, Davidson P. Improving access to care in America: individual and contextual indicators. In: Andersen R, Rice T, Kominsk J, editors. Changing the US health care system. 3. San Francisco: Jossey Bass; 2007. pp. 3–31. [Google Scholar]
- Arangua L, Gelberg L. Homeless Persons. In: Andersen R, Rice T, Kominsk J, editors. Changing the US health care system. 3. San Francisco: Jossey Bass; 2007. pp. 491–547. [Google Scholar]
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of Hepatitis C virus infection in the United States, 1999 through 2002. Annals of Internal Medicine. 2006;144:705–14. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Austin EL, Andersen R, Gelberg L. Ethnic differences in the correlates of mental distress among homeless women. Women's Health Issues. 2008;18:26–34. doi: 10.1016/j.whi.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM. EQS structural equations program manual. Encino, CA: Multivariate Software, Inc; 2006. [Google Scholar]
- Desai RA, Rosenheck RA, Agnello V. Prevalence of hepatitis C virus infection in a sample of homeless veterans. Social Psychiatry & Psychiatric Epidemiology. 2003;38(7):396–401. doi: 10.1007/s00127-003-0639-y. [DOI] [PubMed] [Google Scholar]
- Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Services Research. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Andersen R, Longshore D, Leake B, Nyamathi A, Teruya C, et al. Hospitalization among homeless women: Are there ethnic and drug abuse disparities? Journal of Behavioral Health Services Research. 2009;36:212–232. doi: 10.1007/s11414-008-9144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. American Journal of Public Health. 1997;87:217–220. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Linn LS. Social and physical health of homeless adults previously treated for mental health problems. Hospital & Community Psychiatry. 1988;39:510–516. doi: 10.1176/ps.39.5.510. [DOI] [PubMed] [Google Scholar]
- Gelberg L, Robertson MJ, Leake B, Wenzel SL, Bakhtiar L, Hardie EA, et al. Hepatitis B among homeless and other impoverished US military veterans in residential care in Los Angeles. Public Health. 2001;52:1252–1254. doi: 10.1038/sj/ph/1900783. [DOI] [PubMed] [Google Scholar]
- Gelberg L, Siecke N. Accuracy of homeless adults' self-reports. Medical Care. 1997;35:287–290. doi: 10.1097/00005650-199703000-00008. [DOI] [PubMed] [Google Scholar]
- Greenberg GA, Rosenheck RA. Homelessness in the state and federal prison population. Criminal Behaviour and Mental Health. 2008;18:88–103. doi: 10.1002/cbm.685. [DOI] [PubMed] [Google Scholar]
- Gruber S, Kiesel M. Inequality in health care utilization in Germany? Theoretical and empirical evidence for specialist consultation. Journal of Public Health. 2010;18:351–365. [Google Scholar]
- Hammond WP, Matthews D, Corbie-Smith G. Psychosocial factors associated with routine health examination scheduling and receipt among African American men. Journal of the National Medical Association. 2010;102:276–289. doi: 10.1016/s0027-9684(15)30600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvitz-Lennon M, Frank RG, Thompson W, Baik SH, Alegria M, Rosenheck RA, et al. Investigation of racial and ethnic disparities in service utilization among homeless adults with severe mental illnesses. Psychiatric Services. 2009;60:1032–1038. doi: 10.1176/appi.ps.60.8.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short orientation-memory-concentration test of cognitive impairment. American Journal of Psychiatry. 1983;140:734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine. 2006;21:71–77. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer JE, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301:1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- Lewis JH, Andersen RM, Gelberg L. Health care for homeless women: Unmet needs and barriers to care. Journal of General Internal Medicine. 2003;18:921–928. doi: 10.1046/j.1525-1497.2003.20909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Los Angeles Homeless Services Authority (LAHSA) 2009 Greater Los Angeles Homeless Count Report. 2009 www.lahsa.org/docs/HC09/Homeless-Count-2009-Report.pdf.
- Lum PJ, Ochoa KC, Hahn JA, Shafer KP, Evans JL, Moss AR. Hepatitis B virus immunization among young injection drug users in San Francisco, California: the UFO study. American Journal of Public Health. 2003;9:919–923. doi: 10.2105/ajph.93.6.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance to End Homelessness (NAEH) Research Reports on Homelessness. Washington, DC: author; 2007. Homelessness Counts. [Google Scholar]
- Nyamathi A, Dixon E, Robbins W, Wiley D, Leake B, Gelberg L. Risk factors for hepatitis C virus infection among homeless adults. Journal of General Internal Medicine. 2002;17:143–143. doi: 10.1046/j.1525-1497.2002.10415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Liu Y, Marfisee M, Shoptaw S, Gregerson P, Saab S, et al. Effects of a nurse-managed program on Hepatitis A and B vaccine completion among homeless adults. Nursing Research. 2009;58:13–22. doi: 10.1097/NNR.0b013e3181902b93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson MJ, Clark RA, Charlebois ED, Tulsky JP, Long H, Bangsberg DR, et al. HIV seroprevalence among homeless and marginally housed adults in San Francisco. American Journal of Public Health. 2004;94:1207–1217. doi: 10.2105/ajph.94.7.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins L, Cottler L, Bucholz K, Compton W. C-DIS-IV Computerized Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University Dept. of Psychiatry; 2000. [Google Scholar]
- Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. JAMA. 2009;301:1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: A prospective analysis. Journal of Health Care for the Poor and Underserved. 2000;11:212–230. doi: 10.1353/hpu.2010.0675. [DOI] [PubMed] [Google Scholar]
- Stein JA, Andersen R, Gelberg L. Applying the Gelberg-Andersen Behavioral Model for Vulnerable Populations to health services utilization in homeless women. Journal of Health Psychology. 2007;12:791–804. doi: 10.1177/1359105307080612. [DOI] [PubMed] [Google Scholar]
- Stein JA, Lu M, Gelberg L. Severity of homelessness and adverse birth outcomes. Health Psychology. 2000;19:524–534. [PubMed] [Google Scholar]
- Stein JA, Nyamathi A. Correlates of Hepatitis C virus infection in homeless men: A latent variable approach. Drug & Alcohol Dependence. 2004;75:89–95. doi: 10.1016/j.drugalcdep.2004.02.002. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Ending Chronic Homelessness: Strategies for Action. Washington, DC: author; 2003. [Google Scholar]
- Ware J, Sherbourne C. The MOS 36-item Short-Form Health Survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Wasley A, Kruszon-Moran D, Kuhnert W, Simard EP, Finelli L, McQuillan G, Bell B. The prevalence of hepatitis B virus infection in the United States in the era of vaccination. Journal of Infectious Diseases. 2010;202:192–201. doi: 10.1086/653622. [DOI] [PubMed] [Google Scholar]
- Wechsberg WM, Lam WKK, Zule W, Hall G, Middlesteadt R, Edwards J. Violence, homelessness, and HIV risk among crack-using African-American women. Substance Use & Misuse Special Issue: Homelessness and substance use. 2003;38:669–700. doi: 10.1081/ja-120017389. [DOI] [PubMed] [Google Scholar]
- Weinbaum CM, Sabin KM, Santibanez SS. Hepatitis B, hepatitis C, and HIV in correctional populations: a review of epidemiology and prevention. AIDS. 2005;19:S41–S46. doi: 10.1097/01.aids.0000192069.95819.aa. [DOI] [PubMed] [Google Scholar]