Abstract
BACKGROUND
Mail order pharmacies are commonly used to deliver CVD risk factor medications. Previous studies have shown that mail order pharmacy use is associated with greater medication adherence; however, no studies have examined whether mail order pharmacy use is related to improved CVD risk factor outcomes.
OBJECTIVE
To examine the comparative effectiveness of mail order pharmacy vs. local pharmacy use on LDL-C control in new statin users.
DESIGN
Observational cohort study.
PATIENTS
100,298 adult Kaiser Permanente Northern California (KPNC) members who were new users of statins between January 1, 2005 and December 31, 2007.
MEASUREMENTS
The main outcome measure was LDL-C control in the 3–15 month period after statin therapy was initiated.
RESULTS
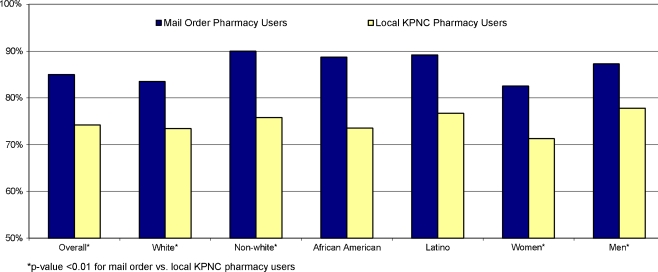
After adjustment for patient, clinical, and census-block characteristics, and for potential unmeasured differences between mail order and local KPNC pharmacy users with instrumental variables analysis, 85.0% of patients who used the mail order pharmacy to deliver their statin at any time achieved target LDL-C levels compared with 74.2% of patients who only used the local KPNC pharmacy to dispense the statin (p < 0.001). Greater adjusted rates of LDL-C control in mail order pharmacy users were seen across all gender and race/ethnicity subgroups.
CONCLUSIONS
Mail order pharmacy use was positively associated with LDL-C control in new statin users. Future research should continue to explore the relationship between mail order pharmacy use and outcomes, and address how to appropriately target mail order services to patients most likely to benefit without compromising patient choice, care, and safety.
KEY WORDS: health services research, hyperlipidemia, pharmaceutical care
INTRODUCTION
Many Americans taking regular medications have the option of using either local pharmacies or mail order pharmacies to fill their prescriptions1. One report suggests that up to 1/3 of medications for chronic conditions are delivered via the mail2, and a 2009 report suggests that mail order pharmacies account for almost 25% of pharmacy sales in the U.S.3 While recent data suggests that the volume of prescriptions delivered via mail has stabilized and may be decreasing3, others propose that the recent expansion of large retail outlets into the mail order pharmacy business means that mail order pharmacies may grow in the future4. The growth of mail order pharmacies to date has largely been driven by economic considerations, as some suggest that mail order pharmacy use may be cost-saving to health plans and to patients5,6. However, studies on whether mail order pharmacy use is actually cost-saving are mixed7,8. Studies also suggest that mail order pharmacy use may associated with greater patient satisfaction with prescription drug benefits and pharmacy services9,10, although preference for mail order pharmacy over community pharmacies may be associated with different patient and benefit-level characteristics11,12.
Despite extensive use of mail order pharmacies in the United States, there is almost no research examining the relationship between patients’ mail order pharmacy use and clinical outcomes. A small number of recent studies have found a positive association between mail order pharmacy use and greater adherence to diabetes and antihypertensive medications13–15. In a prior analysis these authors found that compared to local pharmacy users, diabetes patients who primarily used mail order pharmacies had a 7–8 percentage point higher rate of good adherence to cardiometabolic therapies15. Greater adherence to these medications by mail order pharmacy users may reflect improved access to medications. Mail order does not require travel to the local pharmacy15, which may be of particular benefit to patients with disabilities, time constraints, or limited access to transportation15,16. Previous studies have demonstrated that mail order pharmacy use is associated with greater levels of switching to generic medications17; this increased use of generic medications may reduce cost-related medication non-adherence in patients taking chronic medications. Greater adherence to cardiometabolic medications repeatedly has been shown to be associated with improved outcomes18–20; improved adherence to cardiometabolic therapies for mail order pharmacy users as compared with local pharmacy users may translate into improved intermediate outcomes, including better control of LDL-cholesterol (LDL-C) among statin users21. However, no study to date has directly examined the relationship between mail order pharmacy use and control of intermediate outcomes such as LDL-C. The purpose of this study is to examine the comparative effectiveness of mail order pharmacy vs. local Kaiser Permanente Northern California (KPNC) pharmacy use on achieving LDL-C control in a cohort of new users of statin medications, and to examine whether the effect of mail order pharmacy use varies by patient characteristics such as gender and race/ethnicity.
METHODS
Study Design/Participants
The study population consisted of KPNC members who were new users of statin medications between January 1, 2005 and December 31, 2007. Statin use was obtained from KPNC automated pharmacy records, which capture all prescriptions dispensed to members through a KPNC pharmacy. Patients were considered to be new users if they had no recorded use of a statin in KPNC records for 24 months prior to the initial statin prescription date (i.e. the “index” date). Patients were excluded from the analysis if they were <18 years of age by January 1, 2005, and did not have an active pharmacy benefit during the 2 years prior to the index date. We also excluded patients who did not refill the new statin medication at least once, since nearly all initial fills in the KPNC system are through the “brick and mortar” pharmacy. All subjects were required to have at least one LDL-C test result in the 12 months prior and the 3–15 months post the index date of the new statin prescription. New statin dispensings were captured and included if the statin was prescribed alone or as part of a combination drug with other medications used to treat dyslipidemia (e.g. ezetimibe/simvastatin).
Mail Order and Local Pharmacy Use within the KPNC System
KPNC maintains a mail order pharmacy distribution system in coordination with over 120 local “walk-in” KPNC pharmacies located within outpatient clinics and hospitals. KPNC patients have the option of filling both new and existing prescriptions either by mail or at one of the KPNC local pharmacies. KPNC members do have the option of filling prescriptions via non-KPNC local pharmacies; however, the cost of these fills would not be covered by the patient’s pharmacy benefit. Mail order delivery of medications, with free shipping, can be requested either by phone or through the KP member website. Pharmacists are available via telephone to answer medication-related questions for members using either mail order or local KPNC pharmacies. There is no minimum or proscribed days’ supply of pills required for mail order delivery, which typically dispenses 100-day medication supplies through both mail order and local KPNC pharmacies. Unlike some other mail order pharmacy systems, KPNC patients using the mail order pharmacy must request a prescription and provide up-front payment before the medication is delivered (i.e. no “auto-refills”.) Some patients have a financial incentive to use mail order in the form of a lower co-payment for the same days’ supply obtained by mail versus at a local KPNC pharmacy.
For the purposes of this analysis, patients were defined as local KPNC pharmacy users if they never used the mail order pharmacy to fill the new statin prescription in the 3–15 months post-statin initiation, and as a mail-order pharmacy user if they filled the new statin prescription at least once via the mail order pharmacy system during that timeframe.
Statistical Analysis
A potential concern in using observational studies to assess the effect of mail order pharmacy use on CVD intermediate outcomes is the potential for self-selection, or omitted (unmeasured) variable bias. For example, it is possible that patients who use mail order pharmacy services are intrinsically more motivated to take care of their health than patients who do not use such services; this characteristic cannot be directly measured in electronic databases. We provide two estimates of the comparative effectiveness of mail order pharmacy use vs. local KPNC pharmacy use on LDL-C levels; first, using a difference-in-differences approach22,23, and then using the econometric technique of instrumental variables15,24–27.
A probit model was used to examine the “difference in differences” in pre and post LDL-C control levels between mail order pharmacy and local KPNC pharmacy users, adjusting for patient, clinical, and census-block characteristics22–24. The last LDL-C value in the 12 months immediately prior to new statin dispensing was considered the “pre” value, and the last LDL-C value measured in the 3–15 month period after the first new statin dispensing was considered the “post” value. LDL-C levels in the first three months after dispensing were not examined in order to account for the gradual therapeutic onset of the new statin medication, and to also ensure that post-period LDL-C control was being assessed after mail order pharmacy use was initiated in the mail order group.
Depending on patient risk for adverse cardiovascular outcomes, two different thresholds for LDL targets were used28. Target LDL levels were set at LDL-C <100 mg/dL for patients with a “cardioequivalent” condition, including diabetes, stroke, or coronary artery disease. All other patients had an LDL-C target level of <130 mg/dL. The difference-in-differences models included dummy variables for time of LDL-C measurement (pre vs. post) and pharmacy type (mail order vs. local), as well as an interaction term between time of LDL-C measurement and pharmacy type. These analyses controlled for the effects of age, sex, race/ethnicity, presence of a cardioequivalent condition, number of comorbidities, smoking status, use of non-formulary medications, antidepressants, insurance type, whether the index medication was generic or brand name, total days’ supply, medical facility, follow-up time until the “post” LDL-C test, and number of primary care visits in the year prior to start of the statin medication. These variables were chosen because of their potential relationship with medication adherence, LDL-C levels, or both. Number of primary care visits was included in the model to adjust for potential differences in utilization and self-management practices between patients who use mail order pharmacy services vs. those who do not. Further information on these variables and their definitions is available elsewhere15.
In the instrumental variables analysis, whether or not a patient had a financial incentive to order medications via the KPNC mail order pharmacy was used as the instrument under the assumption that having a financial incentive would affect the probability that a patient would use the mail order pharmacy (exposure), but should not directly affect whether a patient achieved LDL-C control (outcome). Analyses confirmed that having a financial incentive to use mail order was, in fact, associated with a greater likelihood of mail order pharmacy use in unadjusted and adjusted analyses (p < 0.0001), but not independently or directly associated with LDL-C levels. We conducted tests for weak or irrelevant instruments and found none of these problems with our instrument29 (see Appendix Table 3 for more details). The endogeneity test for omitted variable bias indicated that mail order use could not be considered exogenous (p =< 0.001), meaning that the instrumental variables approach using bivariate probit analysis may provide a less-biased estimate of the effect of mail order pharmacy use on LDL-C control. Results from the difference-in-differences and IV analyses were very similar, and both are presented below. To facilitate interpretability of the results, adjusted regression results were converted to predicted percentages of patients reaching LDL-C target levels for both mail order pharmacy users and local KPNC pharmacy users overall and by key patient characteristics, holding all other covariates at their mean value.
All analyses were performed using Stata Version 10.1. The study protocol was approved by the KPNC Institutional Review Board.
RESULTS
A total of 100,298 new users of statin medications met study eligibility criteria. Of these, 29,279 (29.2%) used the mail order pharmacy at least once to refill their new statin medication during the study period (Table 1). Mail order pharmacy users were more likely to be white and to live in census tracts with higher socioeconomic status (p < 0.001). Patients live, on average, less than 10 miles from the nearest KPNC local mail-in pharmacy regardless of whether they used mail order pharmacy services to deliver their medications. Mail order pharmacy users and local KPNC pharmacy users had identical LDL-C levels within both the 12-month period (130 mg/dL for both groups) and within the six-month period (147 mg/dL for both groups) prior to their start of a new statin medication. As demonstrated in previous studies13–15, adherence of > = 80% to the index statin medication, measured using the Continuous Medication Gaps (CMG) method30–32, in the 15 months post-statin initiation was higher in the mail order pharmacy group (87.8% vs. 72.9%, p < 0.001).
Table 1.
Patient Characteristics by Pharmacy Type
| Entire Sample (n = 100,298) | Local KPNC Pharmacy Use Only (n = 71,019) | Mail Order PharmacyUse (n = 29,279) | |
|---|---|---|---|
| Demographics | |||
| Female (%) | 51.8 | 50.7 | 54* |
| Age (Mean) | 61 | 61 | 63* |
| <40 (%) | 3.9 | 4.4 | 2.6* |
| 40-49 (%) | 14.3 | 15.5 | 11.2* |
| 50-59 (%) | 28.4 | 28.8 | 27.3* |
| 60-69 (%) | 26.3 | 25.0 | 29.4* |
| 70-79 (%) | 19.1 | 18.5 | 20.5* |
| 80+ (%) | 8.1 | 7.7 | 9.0* |
| Race/ethnicity | |||
| White, non-Latino (%) | 51.7 | 45.3 | 67.2* |
| African American, non-Latino (%) | 7.0 | 8.6 | 3.0* |
| Latino (%) | 8.0 | 9.5 | 4.4* |
| Asian (%) | 11.9 | 12.9 | 9.6* |
| Native American (%) | 0.5 | 0.5 | 0.3* |
| Mixed-race (%) | 3.7 | 4.1 | 2.8* |
| Missing race (%) | 17.2 | 19.1 | 12.8* |
| Mean home to local pharmacy distance in miles (SD) | 8 (16) | 8 (16) | 9 (18)* |
| Block Group Census Variables | |||
| Mean Household Income ($) | $63,069 | $61,363 | $67,202* |
| Percent in Poverty (%) | 7.6 | 8.1 | 6.5* |
| Percent with at Least a High School Education (%) | 83.6 | 82.3 | 86.2* |
| Percent with at Least a Bachelor’s Degree (%) | 30.7 | 29.2 | 34.5* |
| Clinical Characteristics | |||
| Mean LDL 12–6 months pre-statin (SD) | 130 mg/dL (36) | 130 mg/dL (36) | 130 mg/dL (35) |
| Mean LDL 6–0 months pre-statin (SD) | 147 mg/dL (39) | 147 mg/dL (39) | 147 mg/dL (38) |
| Mean number of comorbidities1 (SD) | 0.66 (0.88) | 0.66 (0.88) | 0.66 (0.89) |
| Has cardiovascular equivalents2 (%) | 38.3 | 39.7 | 34.6* |
| Using medication for depression (%) | 21.9 | 20.9 | 24.4* |
| Using nonformulary medication (%) | 5.5 | 5.4 | 5.7 |
| New medication is brand-name (%) | 3.5 | 3.3 | 4.1* |
| Mean Number of Primary Care Visits in Year Prior to Index Date | 4.08 (4.52) | 4.15 (4.62) | 3.92 (4.27)* |
| Medication Days Supply of 1st Refill | |||
| 1-30 days (%) | 5.6 | 5.8 | 4.9* |
| 31-60 days (%) | 3.0 | 3.0 | 2.8 |
| 61-90 days (%) | 14.8 | 15.3 | 13.7* |
| >90 days (%) | 76.7 | 75.9 | 78.6* |
| Total Medication Days Supply in the 15-Month Period Following the Index Date (Range = 1,525) | |||
| Mean (SD) | 398 (140) | 374 (145) | 456 (104)* |
| Median | 430 | 400 | 500 |
| Total # of Refills in the 15-Month Period Following the Index Date (Range = 19) | |||
| Mean (SD) | 3 (2) | 3 (2) | 4 (1)* |
| Median | 4 | 3 | 4 |
| Length of Follow-up, Index Date to Post-Period LDL Date (Range = 363) | |||
| Mean (SD) | 319 (98) | 313 (101) | 334 (90)* |
| Median | 339 | 332 | 353 |
| Mean Statin Adherence in the 15 -Month Period Following the Index Date (SD) | 77.2 (24.5) | 72.9 (25.9) | 87.8 (16.4)* |
| Mean Statin Adherence during Follow-up (SD) | 80.6 (23.5) | 76.7 (25.2) | 90.0 (15.0)* |
| Insurance Characteristics | |||
| Part D group coverage (%) | 9.6 | 9.6 | 9.8 |
| Part D individual coverage (%) | 11.2 | 9.4 | 15.4* |
| Non-Medicare coverage (%) | 79.2 | 81.1 | 74.8* |
| Financial incentive for mail-order use (%) | 21.8 | 18.3 | 30.4* |
*Difference between mail order and local pharmacy use is statistically significant (p-value < 0.001)
1Comorbidities counted are atrial fibrillation, osteoarthritis, depression, congestive heart failure, chronic obstructive pulmonary disease (COPD), renal failure/insufficiency, and smoking
2Dichotomous variable that equals one if patient has diabetes mellitus, coronary artery disease (CAD), or stroke; equals zero otherwise
Table 2 shows the results of both the difference-in-differences and instrumental variables multivariate models. In both models, mail order pharmacy use was positively and significantly associated with achieving LDL-C control in the 3–15 month period following the initiation of a new statin.
Table 2.
LDL-c Control (1 = In control; 0 = Not in Control)
| Probit (Difference-in-Differences Analysis) | Bivariate Probit (IV Analysis) | |||
|---|---|---|---|---|
| Used mail order pharmacy to refill statin | 0.4475*** | (0.0173) | 0.3865*** | (0.0854) |
| Post period | 1.9908*** | (0.0126) | n/a | n/a |
| Length of follow-up | −0.0004*** | (0.0000) | −0.0009*** | (0.0000) |
| Total statin days supply | 0.0024*** | (0.0000) | 0.0033*** | (0.0000) |
| Gender: female | −0.3330*** | (0.0094) | −0.1958*** | (0.0096) |
| Age at statin initiation | 0.0121*** | (0.0004) | 0.0092*** | (0.0004) |
| African American | −0.0578** | (0.0195) | −0.0599** | (0.0193) |
| Asian | 0.1241*** | (0.0153) | 0.1212*** | (0.0160) |
| Latino | 0.1121*** | (0.0177) | 0.0778*** | (0.0180) |
| Native American | 0.1858** | (0.0652) | 0.1166 | (0.0675) |
| Mixed Race | 0.0865*** | (0.0242) | 0.0299 | (0.0247) |
| Race Missing | −0.0520*** | (0.0137) | −0.0438** | (0.0136) |
| Block Group Census | ||||
| Mean household income | 0.0000 | (0.0000) | 0.0000 | (0.0000) |
| Percent in poverty | 0.0022* | (0.0010) | 0.0016 | (0.0010) |
| % with high school education | −0.0009 | (0.0006) | −0.0010 | (0.0007) |
| % with at least a Bachelor’s degree | −0.0006 | (0.0005) | 0.0001 | (0.0005) |
| Number of comorbidities | 0.0625*** | (0.0057) | 0.0098 | (0.0059) |
| Has cardiovascular equivalents | −0.0520 | (0.0096) | −0.2014*** | (0.0097) |
| Using medication for depression | −0.0289* | (0.0116) | −0.0465*** | (0.0118) |
| Using non-formulary medication | −0.4048*** | (0.0222) | −0.4524*** | (0.0212) |
| Index statin is brand-name | 0.3435*** | (0.0271) | 0.2496*** | (0.0277) |
| # of primary care visits in prior year | 0.0120*** | (0.0011) | 0.0076*** | (0.0011) |
| Medicare Part D group coverage | 0.1461*** | (0.0166) | 0.1580*** | (0.0184) |
| Medicare Part D individual coverage | 0.0816*** | (0.0159) | 0.0504* | (0.0206) |
| Constant | −2.5446*** | (0.0714) | −0.8286*** | (0.0753) |
| ρ (disturbance correlation) | n/a | n/a | −0.1568** | (0.0530) |
Notes: (1) table shows estimated coefficients with standard errors in parentheses; (2) models control for patient’s home medical facility (where KP walk-in pharmacy is located); (3) difference-in-differences analysis uses random effects on panel dataset where N = 99,702 and T = 2 (pre and post period)
*p-value < 0.05
**p-value < 0.01
***p-value < 0.001
Figure 1 uses the results of the instrumental variables bivariate probit model to show the adjusted percents of patients considered in control of their LDL-C values based on their latest LDL-C lab value in the 3–15 months after initiation of the new statin medication. After adjustment for patient demographics, clinical characteristics, and census-block characteristics, 85.0% of patients who used the mail order pharmacy to deliver their statin medication at any time in the 3–15 month window achieved target LDL-C levels compared with 74.2% of patients who only used the local KPNC pharmacy to dispense the statin (p < 0.001). The higher adjusted rates of LDL-C control in the mail order pharmacy vs. local KPNC pharmacy users were seen in both men and women, as well as in both white and non-white patients (p < 0.01). African-American and Latino patients who used the mail order pharmacy also had higher adjusted LDL-C control rates compared to those who used the local KPNC pharmacy; however, these differences were not significant.
Figure 1.
Adjusted percents of patients in LDL-C control 3–15 months after first statin fill.
We performed a sensitivity analysis using only the patients with no financial incentive to use mail order. This was to address the issue of whether the financial incentive to use mail order, and the resulting potential out-of-pocket prescription drug cost difference between the mail order pharmacy and local KPNC pharmacy groups, might result in differential LDL-C outcomes. The results showed similar, statistically significant differences between LDL-C outcomes in mail order vs. local KPNC pharmacy users (data not shown).
DISCUSSION
This analysis is the first to examine the relationship between mail order pharmacy use and control of LDL cholesterol. This study found that despite equivalent LDL-C values at baseline, new statin users who primarily refilled by mail were more likely to be in control of their LDL-C levels within 3–15 months after medication initiation than patients who used local “brick-and-mortar” KPNC pharmacies. This positive association was consistent across patient gender and race/ethnicity. Consistent with previous studies, this study also found that use of mail order pharmacy was associated with better adherence to cardiometabolic medications13–15. Mail order pharmacy use may streamline the process of refilling medications, and improve access to medications by eliminating the need for travel to the pharmacy15. This improved access may be of particular importance to patients with inadequate transportation, disabilities, or time constraints15,16. Recent research suggests that mail order use may also improve medication adherence by promoting the use of less-expensive generic medications17 and reducing refill complexity33. As demonstrated previously21, this study suggests that this improved adherence may lead to the improved LDL-C outcomes among mail order pharmacy users seen in this analysis. While the findings of the present study should be confirmed in a randomized controlled trial, they provide new evidence indicating that mail order pharmacy use may be associated with improved care and outcomes for patients with risk factors for CVD, and underscore the potential benefit of home delivery of medications directly to patients16.
Mail order pharmacy services, which are provided at the health care delivery system level, rather than the physician or practice level, can be considered a structural or system-level intervention for improving access to chronic illness medications by making medications available to patients without the need to travel to a “brick-and-mortar” pharmacy15. Studies suggest system-level barriers to medication acquisition are usually not addressed when new medications are prescribed to patients34,35. System-level efforts to promote mail order use in patients that may benefit from its use, while preserving patient choice in what type of pharmacy services they prefer to use, have the potential to address medication access and adherence issues for new users of statin medications, and could lead to improved outcomes. This study found a similar positive association between mail order pharmacy use and LDL-C control in men and women, and in both minority and white patients, suggesting that such efforts to encourage mail order pharmacy use would provide benefits to patients regardless of gender and race/ethnicity. Since earlier studies of mail order pharmacy services suggest they are cost-saving to patients3,4 and may be also cost-saving for health care delivery systems3, increasing the proportion of prescriptions refilled by mail has the potential to be a cost-effective intervention for improving CVD risk factor control among diverse groups of patients at high risk for adverse outcomes.
Interventions to encourage the use of, and improve access to, mail order pharmacy use would need to be designed and targeted in a way that does not produce unintended consequences for patients. While the current study adds to the evidence suggesting that patients might benefit from increased mail order pharmacy use, the impact of mail delivery of medications on patient safety has not been studied. While KPNC’s mail order pharmacy system provides telephone access to pharmacists, it is possible that providing medications through the mail reduces important face-to-face interactions with pharmacists and primary care providers; these interactions may help prevent multiple drug interactions and facilitate appropriate preventive care such as laboratory monitoring for patients on certain drug therapies36. Some patients may also be hesitant to use the mail order pharmacy because of unsecured mailboxes or other security reasons. Future research should address the important issue of how to appropriately target mail order pharmacy services without compromising care for patients that can benefit from the interactions that come along with in-person medication acquisition and consultation.
This study has several limitations that should be noted. First, observational studies such as this one cannot entirely control for differences between patients who utilize mail order pharmacy services and those that do not. While we utilized both difference-in-differences and instrumental variable analyses to minimize such biases, and both analyses showed a positive significant association between mail order pharmacy use and LDL-C control, it is possible that we were unable to completely control for these differences.
It is important to note that this study took place in an integrated delivery system where patients access their prescription medications differently than in many other settings. Patient experience with “brick and mortar” pharmacy for filling medications is primarily limited to the KPNC local pharmacy, and unlike in many settings KPNC’s mail order pharmacy and local pharmacies do not differ in the standard amount of pills prescribed15. In addition, KPNC provides relatively easy access to mail order pharmacy services, without requiring physician sign-ups or changes in days’ supply15. It is therefore possible that the use of mail order pharmacy services in KPNC has a different impact on intermediate outcomes than in other settings.
Finally, this study examined only the effects of new statin use on LDL-C outcomes, and did not examine the effects of mail order pharmacy use on outcomes for other CVD risk factors or for outcomes associated with chronic diseases such as asthma or depression. Future work should continue to explore the relationship between mail order pharmacy use and patient outcomes across other quality indicators.
CONCLUSION
Mail order pharmacy use is associated with improved LDL-C control in new statin users. System-level interventions to improve the rates of mail order pharmacy use may be an important strategy for improving processes and outcomes of care for patients with chronic illness, and potentially for addressing disparities in these outcomes among minority patients. This approach should be evaluated in randomized controlled trials testing the effectiveness of different methods of encouraging mail order use among patients on both increasing mail order pharmacy use and improving patient outcomes.
Acknowledgements
This study was jointly funded by Program Announcement number 04005 from the Centers for Disease Control and Prevention (Division of Diabetes Translation) and the National Institute of Diabetes and Digestive and Kidney Diseases, Contract no. U58/CCU923527-04-1. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding organizations. Dr. Schmittdiel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis.
Conflicts of Interest Dr. Schmittdiel serves as an unpaid advisor to the American Diabetes Association and Medco joint medication adherence research collaboration. The authors have no other conflicts of interest to report.
Appendix
The results in Table 3 support our use of instrumental variables to estimate our model and in using financial incentive as the instrument for mail order pharmacy use.
Table 3.
Instrumental Variables Tests†
| Endogeneity test | 23.97 |
| p = < 0.001 | |
| Test of excluded instruments (first-stage F-stat) | 1573.27 |
| p = < 0.001 | |
| Weak-instrument-robust inference | 42.46 |
| p = < 0.001 | |
| Overidentification test | Equation exactly identified |
| Underidentification test | 1415.48 |
| p = < 0.001 |
†Tests performed in linear model of LDL-c using ivreg2 command in Stata. See Baum, Schaffer, & Stillman (2007) for details of these tests
References
- 1.Pharmaceutical Strategies Group, 2011. http://www.psgconsults.com/resources/pbm_101.pdf. Accessed June 24, 2011.
- 2.Pharmacy Benefit Managers: Ownership of Mail-Order Pharmacies. Washington, DC: Federal Trade Commission; 2005. [Google Scholar]
- 3.National Association of Chain Drug Stores, Industry “Facts at a Glance.” http://www.nacds.org/wmspage.cfm?parm1=6536. Accessed June 24, 2011.
- 4.Fein AJ. The impact of Walmart’s National Mail Pharmacy. Drug Channels, September 16, 2009. http://www.drugchannels.net/2009/09/impact-of-walmarts-national-mail.html. Accessed June 24, 2011.
- 5.Johnsrud M, Lawsen KA, Shepherd MD. Comparison of mail order with community pharmacy in plan sponsor cost and member cost in two large pharmacy benefit plans. J Manage Care Pharm. 2007;13(2):122–134. doi: 10.18553/jmcp.2007.13.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carroll NV, Brusilovsky I, York B, Oscar R. Comparison of costs of community and mail service pharmacy. J Am Pharm Assoc. 2003;45(3):336–343. doi: 10.1331/1544345054003796. [DOI] [PubMed] [Google Scholar]
- 7.Valluri S, Seoane-Vazquez E, Rodriguez-Monguio R, Szeinbach SL. Drug utilization and cost in a Medicaid population: a simulation study of community vs. mail order pharmacy. BMC Health Serv Res. 2007;7:122–129. doi: 10.1186/1472-6963-7-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clark BE, Siracuse MV, Garis RI. A comparison of mail-service and retail community pharmacy claims in 5 prescription benefit plans. Res Social Adm Pharm. 2009;5(2):133–142. doi: 10.1016/j.sapharm.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Motheral BR, Heinle SM. Predictors of satisfaction of health plan members with prescription drug benefits. Am J Health Syst Pharm. 2004;61(10):1007–1014. doi: 10.1093/ajhp/61.10.1007. [DOI] [PubMed] [Google Scholar]
- 10.Johnson JA, Coons SJ, Hays RD, Sabers D, Jones P, Langley PC. A comparison of satisfaction with mail versus traditional pharmacy services. J Manag Care Pharm. 1997;3:327–337. [Google Scholar]
- 11.Linton A, Garber M, Fagan NK, Peterson M. Factors associated with choice of pharmacy setting among DoD health care beneficiaries aged 65 years or older. JMCP. 2007;13(8):677–86. [DOI] [PMC free article] [PubMed]
- 12.Liberman JN, Wang Y, Hutchins DS, Slezak J, Shrank WH. Revealed preference for community and mail service pharmacy. J Am Pharm Assoc. 2011;51(1):50–7. [DOI] [PubMed]
- 13.Pittman DG, Tao Z, Chen W, Stettin GD. Antihypertensive medication adherence and subsequent health care utilization and cost. Am J Manag Care. 2010;16(8):568–576. [PubMed] [Google Scholar]
- 14.Devine S, Vlahiotis A, Sundar H. A comparison of diabetes medication adherence and healthcare costs in patients using mail order pharmacy and retail pharmacy. J Med Econ. 2010;13(2):203–211. doi: 10.3111/13696991003741801. [DOI] [PubMed] [Google Scholar]
- 15.Duru OK, Schmittdiel J, Dyer W, Parker M, Uratsu C, Chan J, Karter A. Mail order pharmacy use and adherence to diabetes-related medications. Am J Manag Care. 2010;15(1):33–40. [PMC free article] [PubMed] [Google Scholar]
- 16.Duru OK, Gerzoff RB, Selby JV, et al. Identifying risk factors for racial disparities in diabetes outcomes: the Translating Research into Action for Diabetes (TRIAD) Study. Med Care. 2009;47(6):700–706. doi: 10.1097/MLR.0b013e318192609d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shrank WH, Stedman M, Ettner SL, DeLapp D, Dirstine J, Brookhart MA, Fischer MA, Avorn J, Asch SM. Patient, physician, pharmacy, and pharmacy benefit design factors related to generic medication use. J Gen Intern Med. 2007;22(9):1298–1304. doi: 10.1007/s11606-007-0284-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost. Medical Care. 2005;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 19.Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, Magid DJ. Effect of medication nonadherence on hospitalizations and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 20.Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27(9):2149–2153. doi: 10.2337/diacare.27.9.2149. [DOI] [PubMed] [Google Scholar]
- 21.Lee JK, Grace KA, Taylor AJ. Effect of a Pharmacy Care Program on Medication Adherence and Persistence, Blood Pressure, and Low-Density Lipoprotein Cholesterol. A Randomized Controlled Trial. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 22.Dyer WT, Fairlie RW. Do family caps reduce out of wedlock births? Evidence from Arkansas, Georgia, Indiana, New Jersey and Virginia. Popul Res Policy Rev. 2004;23:441–473. doi: 10.1007/s11113-004-3462-6. [DOI] [Google Scholar]
- 23.Meyer BD. Natural and quasi-experiments in economics. J Bus Econ Stat. 1995;13(2):151–161. doi: 10.2307/1392369. [DOI] [Google Scholar]
- 24.Gameren E. Health insurance and use of alternative medicine in Mexico. Health Policy. 2010;98:50–57. doi: 10.1016/j.healthpol.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Newhouse JP, McClellan M. Econometrics in outcomes research: The use of instrumental variables. Annu Rev Publ Health. 1998;19:17–34. [DOI] [PubMed]
- 26.Greenland S. An Introduction to instrumental variables for epidemiologists. Int J Epidemiol. 2000;29:722–729. doi: 10.1093/ije/29.4.722. [DOI] [PubMed] [Google Scholar]
- 27.McClellan MC, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. 1994;272(11):859–866. doi: 10.1001/jama.272.11.859. [DOI] [PubMed] [Google Scholar]
- 28.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ, National Heart Lung, Blood Institute; American College of Cardiology Foundation. American Heart Association Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 29.Baum CF, Shaffer ME, Stillman S. Enhanced routines for instrumental variables/generalized method of moments estimation and testing. The Stata Journal. 7(4):465–506.
- 30.Steiner JF, Koepsell TD, Fihn SD, Inui TS. A general method of compliance assessment using centralized pharmacy records. Description and validation. Med Care. 26:814–23. [DOI] [PubMed]
- 31.Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;50:105–116. doi: 10.1016/S0895-4356(96)00268-5. [DOI] [PubMed] [Google Scholar]
- 32.Choo PW, Rand CS, Inui TS, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37(9):846–857. doi: 10.1097/00005650-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Choudry NK, Fischer MA, Avorn J, Liberman JN, Schneeweiss S, Pakes J, Brennan TA, Shrank WH. The implications of therapeutic complexity on adherence to cardiovascular medications. Arch Intern Med. 2011;171(9):814–822. doi: 10.1001/archinternmed.2010.495. [DOI] [PubMed] [Google Scholar]
- 34.Richard C, Lussier MT. Nature and frequency of exchanges on medications during primary care encounters. Patient Educ Couns. 2006;64(1–3):207–216. doi: 10.1016/j.pec.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 35.Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. Am J Manag Care. 2006;12(11):657–664. [PubMed] [Google Scholar]
- 36.Raebel ME, Lyons EE, Andrade SE, et al. Laboratory monitoring of drugs at initiation of therapy in ambulatory care. J Gen Intern Med. 2005;20:1120–1126. doi: 10.1111/j.1525-1497.2005.0257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]