Abstract
Background
ACSCOT has developed and updated field trauma triage protocols for decades, yet the ability to identify major trauma patients remains unclear. We estimate the diagnostic value of the Field Triage Decision Scheme for identifying major trauma patients (Injury Severity Score [ISS] ≥ 16) in a large and diverse multi-site cohort.
Study Design
This was a retrospective cohort study of injured children and adults transported by 94 EMS agencies to 122 hospitals in 7 regions of the Western U.S. from 2006 through 2008. Patients who met any of the field trauma triage criteria (per EMS personnel) were considered triage positive. Hospital outcome measures were probabilistically linked to EMS records through trauma registries, state discharge data and emergency department data. The primary outcome defining a “major trauma patient” was ISS ≥ 16.
Results
122,345 injured patients were evaluated and transported by EMS over the 3-year period, of who 34.5% met at least one triage criterion and 5.8% had ISS ≥ 16. The overall sensitivity and specificity of the criteria for identifying major trauma patients were 85.8% (95% CI 85.0 – 86.6%) and 68.7% (95% CI 68.4 – 68.9%). Triage sensitivity and specificity differed by age: 84.1% and 66.4% (0 – 17 years); 89.5% and 64.3% (18 – 54 years); and 79.9% and 75.4% (≥ 55 years). Evaluating the diagnostic value of triage by hospital destination (transport to Level I/II trauma centers) did not substantially improve these findings.
Conclusions
The sensitivity of the Field Triage Decision Scheme for identifying major trauma patients is lower and specificity higher than previously described, particularly among elders.
INTRODUCTION
The process of triaging injured patients in the out-of-hospital setting is a critically important aspect of concentrating those with serious injuries in high-resource hospitals (i.e., major trauma centers), while conserving limited trauma resources. Such regionalized trauma care has been shown to improve outcomes among seriously injured adults1–8 and children.9–13 Several additional studies also suggest that patients triaged directly to a trauma center may have improved outcomes when compared to those initially transported to a non-trauma hospital.3,14,15 Because the majority of seriously injured patients access acute care through 9-1-1 emergency medical services (EMS), an accurate and effective out-of-hospital mechanism for appropriately matching patients to hospital resources is a vital aspect of trauma systems.
The Field Triage Decision Scheme was developed by the American College of Surgeons Committee on Trauma (ACSCOT) more than 20 years ago16–19 and has been periodically revised and updated. In 2006, the Centers for Disease Control and ACSCOT partnered to bring a broad group of stakeholders together for the most recent revision of the decision scheme.20 These guidelines have been widely promoted and integrated into most EMS and trauma systems throughout the U.S. The guidelines represent a combination of science and expert opinion, built largely from research evaluating individual criteria or portions of the triage algorithm. Several studies show the decision scheme to be highly sensitivity (≥ 95%) for identifying seriously injured patients,21,22 though more recent research suggests the sensitivity may be much lower,23–25 particularly among elder patients.23,25,26 Due to inherent limitations in previous triage research (e.g., study design, patient sampling restrictions, single hospital, single EMS agency, single mechanism of injury, trauma registry patients, variable outcome measures) and the resulting biases, the true diagnostic value of the Field Triage Decision Scheme remains uncertain.
In this project, we sought to estimate the diagnostic value (e.g., sensitivity, specificity) of the Field Triage Decision Scheme for identifying major trauma patients (Injury Severity Score [ISS] ≥16) among a large and diverse population of injured patients evaluated by EMS providers across multiple sites. We conducted secondary analyses to assess the decision scheme by age group and hospital destination.
METHODS
Study Design
This investigation was a multi-site retrospective cohort study. Sixteen Institutional Review Boards at 7 sites approved this protocol and waived the requirement for informed consent.
Study Setting
The study included injured children and adults evaluated and transported by 94 EMS agencies to 122 hospitals (including 15 Level I, 8 Level II, 3 Level III, 4 Level IV, 1 Level V and 91 community/private/federal hospitals) in 7 sites across the Western U.S over a 3-year period (January 1, 2006 through December 31, 2008). The 7 sites included: Portland, OR/Vancouver, WA (4 counties); King County, WA; Sacramento, CA (2 counties); San Francisco, CA; Santa Clara, CA (2 counties); Salt Lake City, UT (4 counties), and Denver County, CO. These sites are part of the Western Emergency Services Translational Research Network (WESTRN), a consortium of geographic regions, EMS agencies and hospitals linked through Clinical and Translational Science Award centers. Each site represents a pre-defined geographic “footprint,” typically consisting of a central metropolitan area and surrounding region, defined by EMS agency service areas. The majority of sites are urban and suburban, though some outlying rural areas are also included. All sites have established trauma systems with designated Level I/II trauma centers and standardized trauma triage protocols to guide selection of transport destinations and trauma care by EMS personnel (Table 1).27
Table 1.
Description of Sites, EMS Systems and Hospitals in the 7 Study Regions
| Hospitals | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Site | EMS service area population* | Geographic area, sq miles | Population density, persons per sq mile | Service area description | EMS agencies† | Type EMS response | Hospitals | Level I | Level II | Level III | Level IV |
| A | 2,082,318 | 3,655 | 570 | Primarily urban/suburban, some rural | 10 | Single tier, dual ALS | 16 | 2 | 1 | 0 | 0 |
| B | 1,916,441 | 2,126 | 901 | Primarily urban/suburban, some rural | 32 | Tiered response, BLS/ALS | 18 | 1 | 0 | 3 | 5‡ |
| C | 610,345 | 153 | 3,989 | Urban/suburban | 1 | Tiered response, BLS/ALS | 11 | 4 | 2 | 0 | 0 |
| D | 744,041 | 46 | 16,175 | Urban | 1 | Tiered response, BLS/ALS | 12 | 1 | 0 | 0 | 0 |
| E | 549,644 | 1,254 | 438 | Primarily urban/suburban, some rural | 2 | Tiered response, BLS/ALS | 28 | 1 | 1 | 0 | 0 |
| F | 2,503,631 | 1,740 | 1,439 | Urban/suburban | 2 | Single tier, dual ALS | 20 | 3 | 1 | 0 | 0 |
| G | 2,112,957 | 3,616 | 584 | Primarily urban/suburban, some rural | 46 | Tiered response, BLS/ALS | 17 | 3 | 3 | 0 | 0 |
| Total | 10,519,377 | 12,590 | 836 | - | 94 | - | 122 | 15 | 8 | 3 | 5 |
2009 population estimates, except site D (2006 estimate).
The number of EMS agencies listed represent those included in the study. In several sites, there are additional first responder, non-transport agencies that participate in the EMS system.
Includes one Level V hospital.
ALS, advanced life support; BLS, basic life support; EMS, emergency medical services.
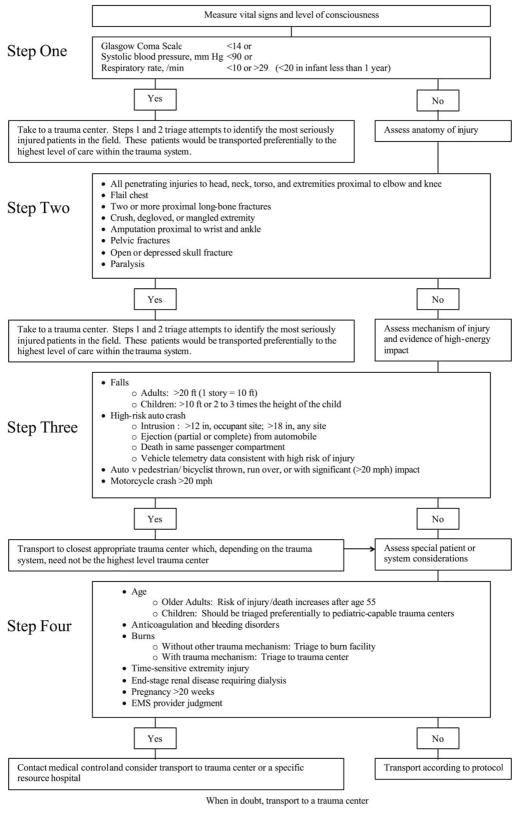
For injured patients evaluated by EMS providers at these sites, there is an initial field triage decision of whether an injured patient meets field trauma triage criteria and warrants transport to a major (i.e., Level I or II) trauma center. The triage processes in all sites use standardized triage protocols27 based on the ACSCOT Field Triage Decision Scheme (Figure 1),19 though there is variability in local figureimplementation and retention of criteria from older versions of the scheme. The presence of one or more trauma triage criteria typically triggers transport to a Level I or II trauma center, but may result in transport to a lower level trauma center (e.g., Level III or IV hospitals) depending on proximity and established protocols in each system.
Figure 1.
The 2006 ACSCOT Field Triage Decision Scheme. (Reprinted with permission from: Resources for the Optimal Care of the Injured Patient. Chicago, IL, American College of Surgeons, 2006.)
Patient Population
The study sample included all patients (children and adults) for whom the 9-1-1 EMS system was activated within the 7 predefined geographic regions, the EMS provider(s) recorded a primary impression of “injury” or “trauma,” the patient was transported to an acute care hospital (trauma centers and non-trauma centers) and a matched hospital record was available. Specifying the sample in this manner allowed for an out-of-hospital injury cohort of patients with both minor and serious injuries, as perceived by EMS providers (i.e., the denominator to whom the Field Triage Decision Scheme is applied). This sampling strategy is distinct from previous triage research and was designed to minimize bias in generating estimates for triage performance. Interhospital transfers without an initial presentation involving EMS were excluded from the sample, though injured patients evaluated and transported by EMS with subsequent transfer to another hospital were included. EMS runs listed as “cancelled,” “no patient found,” “stand by” (i.e., calls without patient contact), and patients that were not transported (e.g., deaths in the field, refusals of transport) were excluded from the sample.
Variables
The primary “exposure” variable of interest was whether the patient met any of the criteria listed in the ACSCOT Field Triage Decision Scheme (Figure 1),19 as determined by EMS providers. Because relying exclusively on recorded trauma triage criteria in EMS records may underestimate the sensitivity of the triage guidelines (due to missing data for triage criteria), we took several steps to ensure comprehensive identification of all patients determined by EMS to meet field triage criteria. The presence of trauma triage criteria was determined as follows: trauma triage criteria specified in the EMS chart; EMS provider documented “trauma system entry” (or similar charting, depending on local terminology); EMS-recorded trauma identification number (used at some sites as a mechanism for tracking injured patients entered into the trauma system); a matched record from the local trauma registry specifying “scene” origin (i.e., EMS-identified trauma patient); or other surrogate EMS charting markers used in local EMS electronic health records to denote triage-positive patients. All other patients were considered triage negative. The presence or absence of triage criteria was considered independent of transport destination (type of hospital to which the patient was initially transported). We recorded all individual triage criteria cited by EMS personnel (up to five per patient), including any of the 24 criteria listed in current Field Triage Decision Scheme19 and any additional criteria cited from previous versions (e.g., rollover motor vehicle crash).16
In addition, we tracked patient demographics (age, gender), out-of-hospital physiology (systolic blood pressure [SBP], Glasgow Coma Scale [GCS] score, respiratory rate), EMS procedures (intubation attempt, intravenous line placement), transport mode (air versus ground), hospital destination (including hospital type), interhospital transfers, injury severity (Injury Severity Score [ISS], Abbreviated Injury Scale [AIS] score), major non-orthopedic surgical procedures (brain, spine, neck, thorax, abdomen, vascular or interventional radiology), orthopedic surgery and in-hospital mortality. Acute care hospitals were categorized as tertiary trauma centers (Level I or II trauma facilities) or non-trauma centers based on their American College of Surgeons accreditation status and state-level designations.
Outcomes
The primary outcome for this study was Injury Severity Score (ISS) ≥ 16, which we use to define a “major trauma patient.” While many definitions of serious injury have been used in previous triage studies, an ISS ≥ 16 is the threshold used by ACSCOT to define under- and over-triage,19 allows comparison to results from multiple previous triage studies, and defines the subset of patients most likely to benefit from trauma center care.1,2,4,7,8,10
Data Sources, Data capture & Processing
EMS and hospital outcome data were collected and transmitted electronically to the WESTRN Data Coordinating Center (Portland, OR). Probabilistic linkage (LinkSolv v8.2, Strategic Matching, Inc., Morrisonville, NY) 28–30 was used to match EMS records to hospital outcomes from local trauma registries, state discharge databases and state emergency department (ED) data. Three sites did not have statewide ED data available. The same probabilistic linkage methodology has been used to link EMS data to hospital records in previous studies30 and has been validated for matching ambulance records to trauma registry data.31 In regions where multiple EMS agencies care for the same patient (and therefore generate multiple EMS records for a single patient), we also used probabilistic linkage to combine EMS records. All hospital data sources had standardized processes to ensure consistent and reliable data collection. Because AIS and ISS are not collected in state discharge or ED databases, we used ICD9 codes and a mapping function (Stata v. 11, StataCorp, College Station, TX) to generate consistent AIS and ISS measures for patients in all sites. ICD9 procedure codes, CPT codes, and abstracted data on surgical procedures (e.g., from trauma registries) were compiled to track surgical interventions.
Data Analysis
We used descriptive statistics to characterize the sample, outcomes and diagnostic metrics for the triage guidelines. We designed the primary analysis to validate the ability of the Field Triage Decision Scheme to identify patients with ISS ≥ 16, regardless of the type of hospital to which they were initially transported. Sensitivity was calculated as the proportion of seriously injured patients identified by field triage criteria and specificity as the proportion of non-seriously injured patients that did not meet triage criteria. Under-triage (the proportion of major trauma patients missed by the triage criteria) was calculated from 1 - sensitivity and over-triage (the proportion of minimally injured patients meeting triage criteria) as 1 – specificity. Additional diagnostic metrics included positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (+LR), negative likelihood ratio (−LR) and area under the curve (AUC). Stratified analyses were conducted by age group for children (0 – 17 years), adults (18 – 54 years), and elders (≥ 55 years) based on previous research demonstrating an age-dependent benefit of trauma center care.1 Because triage can be defined using different perspectives, we recalculated the diagnostic metrics based on transport destination (i.e., to a Level I/II hospital versus non-trauma or lower level trauma hospitals) as the exposure variable, regardless of the presence or absence of triage criteria. All analyses were conducted using SAS (v 9.2, SAS Institute, Cary, NC).
Missing values were handled using multiple imputation to minimize bias and preserve study power.32 We have previously demonstrated the validity of multiple imputation for imputing missing out-of-hospital values and trauma data under a variety of conditions.33,34 We used flexible chains regression models for multiple imputation (IVEware, Survey Methodology Program, Survey Research Center, Institute for Social Research, University of Michigan, MI)35 with generation of 10 multiply imputed datasets, each analyzed independently and combined using Rubin’s rules to appropriately account for variance within- and between-datasets.32 Missing data were imputed for: age (< 1%), gender (5%), mechanism of injury (28%), field intubation (1%), field IV (6%), SBP (9%), GCS (14%), heart rate (6%), respiratory rate (8%), triage step (10%), hospital destination (< 1%), ISS (< 1%) and maximum AIS (< 1%).
RESULTS
There were 122,345 injured patients evaluated by 94 EMS agencies and transported to 122 hospitals over the 3-year period, of whom 42,207 (34.5%) met at least one trauma triage criterion. The proportion of patients at each site meeting at least one triage criterion ranged from 18.2 – 50.7%. Of the study sample, 7,100 (5.8%) patients had ISS ≥16. Characteristics of the study sample, separated by the presence or absence of field trauma triage criteria, are demonstrated in Table 2.
Table 2.
Characteristics of Injured Patients Transported by EMS in the 7 Study Regions
| Total sample | Triage positive | Triage negative | ||||
|---|---|---|---|---|---|---|
| n = 122,345 | n = 42,207 34.5 | n = 80,138 65.5 | ||||
| Demographics: | n | % | n | % | n | % |
| Age, mean, y | 46.6 | 42.5 | 48.8 | |||
| < 18 | 14,876 | 12.2 | 5,357 | 12.7 | 9,518 | 11.9 |
| 18 – 54 | 62,435 | 51.0 | 24,474 | 58.0 | 37,961 | 47.4 |
| ≥ 55 | 45,035 | 36.8 | 12,376 | 29.3 | 32,659 | 40.8 |
| Women | 58,178 | 47.6 | 16,034 | 38.0 | 42,143 | 52.6 |
| Out-of-hospital physiology and procedures: | ||||||
| SBP in mmHg, mean | 135.2 | 132.2 | 136.7 | |||
| SBP < 90 mmHg | 3,825 | 3.1 | 2,194 | 5.2 | 1,632 | 2.0 |
| GCS, mean | 14.4 | 13.9 | 14.6 | |||
| GCS ≤ 8 | 3,363 | 2.7 | 2,329 | 5.5 | 1,034 | 1.3 |
| Respiratory rate in breaths/min, mean | 18.7 | 19.0 | 18.5 | |||
| Intubation attempt | 1,531 | 1.3 | 1,387 | 3.3 | 144 | 0.2 |
| Intravenous line placement | 50,065 | 40.9 | 26,172 | 62.0 | 23,893 | 29.8 |
| Mechanism of injury | ||||||
| Gunshot wound | 1,300 | 1.1 | 1,084 | 2.6 | 215 | 0.3 |
| Stabbing | 2,441 | 2.0 | 1,654 | 3.9 | 787 | 1.0 |
| Assault | 7,467 | 6.1 | 2,196 | 5.2 | 5,271 | 6.6 |
| Fall | 44,834 | 36.6 | 11,264 | 26.7 | 33,570 | 41.9 |
| Motor vehicle crash | 41,043 | 33.5 | 16,231 | 38.5 | 24,812 | 31.0 |
| Other | 25,260 | 20.6 | 9,778 | 23.2 | 15,483 | 19.3 |
| Hospital measures | ||||||
| Interhospital transfer | 7,759 | 6.3 | 3,622 | 8.6 | 4,137 | 5.2 |
| Initial transport to Level I/II | 46,839 | 38.3 | 25,288 | 59.9 | 21,551 | 26.9 |
| Final destination Level I/II | 59,795 | 48.9 | 33,201 | 78.7 | 26,593 | 33.2 |
| Outcomes measures | ||||||
| ISS, mean | 4.3 | 7.3 | 2.7 | |||
| ISS >= 16 | 7,100 | 5.8 | 6,091 | 14.4 | 1,009 | 1.3 |
| Maximum AIS, mean | 1.2 | 1.7 | 1.0 | |||
| AIS >=3 | 20,782 | 17.0 | 12,854 | 30.5 | 7,927 | 9.9 |
| Non-orthopaedic surgery | 5,632 | 4.6 | 3,667 | 8.7 | 1,965 | 2.5 |
| Orthopaedic surgery | 19,194 | 15.7 | 7,987 | 18.9 | 11,207 | 14.0 |
| In-hospital mortality | 2,068 | 1.7 | 1,292 | 3.1 | 776 | 1.0 |
EMS, emergency medical services; SBP, systolic blood pressure; GCS, Glasgow Coma Scale; ISS, Injury Severity Score; AIS, Abbreviated Injury Scale score; major non-orthopaedic surgery, brain, spine, neck, thorax, abdomen, interventional radiology or vascular operative procedures during hospitalization.
Field triage diagnostic measures (for individual sites and overall) are demonstrated in Table 3. The overall sensitivity and specificity of the Field Triage Decision Scheme for identifying major trauma patients were 85.8% (95% CI 85.0 – 86.6%) and 68.7% (95% CI 68.4 – 68.9%), respectively. Assessment of the triage diagnostic value by initial transport to a Level I or II trauma center demonstrated a sensitivity of 73.4% (95% CI 72.4 – 74.4%) and a specificity of 63.9% (95% CI 63.6 – 64.2%) (Table 4). For final transport to a Level I or II trauma center (combined primary and secondary triage processes), the sensitivity for identifying major trauma patients was 82.6% (95% CI 81.7 – 83.5%) with specificity 53.2% (95% CI 52.9 – 53.5%) (Table 5). There was inter-site variability in all diagnostic metrics and some intra-site variability based on how triage accuracy was defined (i.e., by triage criteria versus transport destination). Under-triaged patients tended to be older, suffering falls or motor vehicle crashes, and frequently required operative intervention (both non-orthopedic and orthopedic) with elevated mortality (Table 5) compared to the full sample and triage-positive patients (Table 2). Even after combining primary and secondary triage processes, a substantive portion of under-triaged patients were not cared for in major trauma centers (Table 5, Table 6). Triage sensitivity was highest among adults and lowest among elders, with specificity highest among elders (Table 7).
Table 3.
Diagnostic Metrics for the Field Triage Decision Scheme (as Applied by EMS Personnel) for Identifying Major Trauma Patients (Injury Severity Score ≥ 16)
| Site | Total n | Triage + n | ISS ≥ 16 n | Sens % | 95%CI (%) | Spec % | 95%CI (%) | Under-triage % | Over-triage % | PPV % | NPV % | +LR | −LR | AUC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 15,427 | 7,307 | 1,887 | 90.2 | (88.8–91.5) | 58.6 | (57.8–59.4) | 9.8 | 41.4 | 23.3 | 97.7 | 2.18 | 0.17 | 0.74 |
| B | 12,071 | 6,116 | 2,101 | 84.9 | (83.3–86.4) | 56.5 | (55.6–57.5) | 15.1 | 43.5 | 29.1 | 94.7 | 1.95 | 0.27 | 0.71 |
| C | 8,523 | 3,070 | 926 | 84.8 | (82.5–87.1) | 69.9 | (68.9–71.0) | 15.2 | 30.1 | 25.6 | 97.4 | 2.82 | 0.22 | 0.77 |
| D | 3,476 | 1,054 | 100 | 97.0 | (93.6–1.00) | 71.7 | (70.1–73.2) | 3.0 | 28.3 | 9.2 | 99.9 | 3.42 | 0.04 | 0.84 |
| E | 2,300 | 897 | 118 | 76.3 | (68.6–84.0) | 63.0 | (61.0–65.0) | 23.7 | 37.0 | 10.0 | 98.0 | 2.06 | 0.38 | 0.70 |
| F | 47,644 | 17,763 | 588 | 93.2 | (91.2–95.2) | 63.4 | (63.0–63.9) | 6.8 | 36.6 | 3.1 | 99.9 | 2.55 | 0.11 | 0.78 |
| G | 32,904 | 6,000 | 1,380 | 78.7 | (76.5–80.9) | 84.4 | (84.0–84.8) | 21.3 | 15.6 | 18.1 | 98.9 | 5.05 | 0.25 | 0.82 |
| Total | 122,345 | 42,207 | 7,100 | 85.8 | (85.0–86.6) | 68.7 | (68.4–68.9) | 14.2 | 31.3 | 14.4 | 98.7 | 2.74 | 0.21 | 0.77 |
EMS, emergency medical services; ISS, Injury Severity Score; sens, sensitivity; spec, specificity; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve.
Table 4.
Diagnostic Metrics for Identifying Major Trauma Patients (Injury Severity Score ≥ 16), Based on Initial and Final Destination Hospital, Regardless of Triage Criteria, Initial Emergency Medical Services Transport to a Level I/II Trauma Center
| Site | n | n Initial Level I/II | n ISS ≥ 16 | Sens % | 95%CI (%) | Spec % | 95%CI (%) | Under-triage % | Over-triage % | PPV % | NPV % | +LR | −LR | AUC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 15,427 | 9,365 | 1,887 | 93.3 | (92.2–94.5) | 43.9 | (43.0–44.7) | 6.7 | 56.1 | 18.8 | 97.9 | 1.66 | 0.15 | 0.69 |
| B | 12,071 | 3,890 | 2,101 | 67.8 | (65.8–69.8) | 75.3 | (74.4–76.1) | 32.2 | 24.7 | 36.6 | 91.7 | 2.74 | 0.43 | 0.72 |
| C | 8,523 | 6,438 | 926 | 95.9 | (94.6–97.2) | 27.0 | (26.0–28.0) | 4.1 | 73.0 | 13.8 | 98.2 | 1.31 | 0.15 | 0.61 |
| D | 3,476 | 1,850 | 100 | 98.0 | (95.2–100) | 48.1 | (46.4–49.8) | 2.0 | 51.9 | 5.3 | 99.9 | 1.89 | 0.04 | 0.73 |
| E | 2,300 | 1,321 | 118 | 91.5 | (86.5–96.6) | 44.4 | (42.3–46.5) | 8.5 | 55.6 | 8.2 | 99.0 | 1.65 | 0.19 | 0.68 |
| F | 47,644 | 14,979 | 588 | 55.3 | (51.2–59.3) | 68.9 | (68.4–69.3) | 44.7 | 31.1 | 2.2 | 99.2 | 1.77 | 0.65 | 0.62 |
| G | 32,904 | 8,996 | 1,380 | 44.1 | (41.4–46.7) | 73.4 | (72.9–73.9) | 55.9 | 26.6 | 6.8 | 96.8 | 1.66 | 0.76 | .59 |
| Total | 122,345 | 46,839 | 7,100 | 73.4 | (72.4–74.4) | 63.9 | (63.6–64.2) | 26.6 | 36.1 | 11.1 | 97.5 | 2.03 | 0.42 | 0.69 |
EMS, emergency medical services; ISS, Injury Severity Score; sens, sensitivity; spec, specificity; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve.
Table 5.
Diagnostic Metrics for Identifying Major Trauma Patients (Injury Severity Score ≥ 16), Based on Initial and Final Destination Hospital, Regardless of Triage Criteria, Final Destination of Level I/II Trauma Center
| Site | n | Final Level I/II | n ISS ≥ 16 | Sens % | 95%CI (%) | Spec % | 95%CI (%) | Under-triage % | Over-triage % | PPV % | NPV % | +LR | −LR | AUC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | 15,427 | 9,670 | 1,887 | 94.9 | (93.9–95.9) | 41.8 | (41.0–42.6) | 5.1 | 58.2 | 18.5 | 98.3 | 1.63 | 0.12 | 0.68 |
| B | 12,071 | 4,178 | 2,101 | 72.2 | (70.3–74.2) | 73.3 | (72.4–74.2) | 27.8 | 26.7 | 36.3 | 92.6 | 2.71 | 0.38 | 0.73 |
| C | 8,523 | 6,454 | 926 | 96.1 | (94.8–97.3) | 26.8 | (25.8–27.8) | 3.9 | 73.2 | 13.8 | 98.2 | 1.31 | 0.15 | 0.61 |
| D | 3,476 | 1,864 | 100 | 98.0 | (95.2–100) | 47.7 | (46.0–49.4) | 2.0 | 52.3 | 5.3 | 99.9 | 1.87 | 0.04 | 0.73 |
| E | 2,300 | 1,388 | 118 | 100 | (97.5–100) | 41.8 | (39.7–43.9) | 0 | 58.2 | 8.5 | 100.0 | 1.72 | 0 | 0.71 |
| F | 47,644 | 26,296 | 588 | 95.2 | (93.5–97.0) | 45.3 | (44.9–45.8) | 4.8 | 54.7 | 2.1 | 99.9 | 1.74 | 0.11 | 0.70 |
| G | 32,904 | 9,945 | 1,380 | 64.4 | (61.9–67.0) | 71.3 | (70.8–71.8) | 35.6 | 28.7 | 8.9 | 97.9 | 2.24 | .50 | .68 |
| Total | 122,345 | 59,795 | 7,100 | 82.6 | (81.7–83.5) | 53.2 | (52.9–53.5) | 17.4 | 46.8 | 9.8 | 98.0 | 1.76 | 0.33 | 0.68 |
Assessing final destination of Level I/II trauma center allows for combined assessment of primary (field) and secondary (hospital) triage processes, whether major trauma patients were ultimately cared for in a major trauma center. Final destination of a major trauma center includes both initial transports to a Level I/II hospital and subsequent interhospital transfers to a Level I/II hospital after initial EMS transport to a non-Level I/II hospital.
EMS, emergency medical services; ISS, Injury Severity Score; sens, sensitivity; spec, specificity; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve.
Table 6.
Characteristics of Under-Triaged Patients
| ISS ≥ 16, triage criteria negative | ||
|---|---|---|
| n = 1,009 | ||
| n | % | |
| Demographics | ||
| Age, mean, y | 51.3 | |
| < 18 | 111 | 11.0 |
| 18 – 54 | 425 | 42.1 |
| ≥ 55 | 473 | 46.9 |
| Women | 367 | 36.3 |
| Out-of-hospital physiology and procedures | ||
| SBP,mmHg, mean | 134.7 | |
| SBP < 90 mmHg | 58 | 5.7 |
| GCS, mean | 13.6 | |
| GCS ≤ 8 | 80 | 8.0 |
| Respiratory rate, breaths/min, mean | 18.9 | |
| Intubation attempt | 27 | 2.6 |
| Intravenous line placement | 347 | 34.4 |
| Mechanism of injury | ||
| Gunshot wound | 12 | 1.2 |
| Stabbing | 8 | 0.8 |
| Assault | 73 | 7.2 |
| Fall | 471 | 46.6 |
| Motor vehicle crash | 298 | 29.5 |
| Other | 147 | 14.6 |
| Hospital measures | ||
| Interhospital transfer | 365 | 36.2 |
| Initial transport to Level I/II | 464 | 45.9 |
| Final destination Level I/II | 621 | 61.5 |
| Outcomes measures | ||
| Injury Severity Score, mean | 20.4 | |
| ISS >= 16 | 1,009 | 100 |
| Maximum AIS, mean | 3.8 | |
| AIS >=3 | 1,009 | 100 |
| Major non-orthopedic surgery | 242 | 24.0 |
| Orthopedic surgery | 201 | 19.9 |
| In-hospital mortality | 84 | 8.3 |
SBP, systolic blood pressure; GCS, Glasgow Coma Scale; ISS, Injury Severity Score; AIS, Abbreviated Injury Scale; major non-orthopaedic surgery, brain, spine, neck, thorax, abdomen, interventional radiology or vascular operative procedures during hospitalization.
Table 7.
Diagnostic Metrics for the Field Triage Decision Scheme (as Applied by EMS Personnel) for Identifying Major Trauma Patients (Injury Severity Score ≥16), Stratified by Age Group
| Age group, y | n | n triage + | n ISS ≥ 16 | Sens % | 95%CI (%) | Spec % | 95%CI (%) | Under-triage % | Over-triage % | PPV % | NPV % | +LR | −LR | AUC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 – 17 | 14,874 | 5,355 | 697 | 84.1 | (81.3–86.8) | 66.4 | (65.6–67.1) | 15.9 | 33.6 | 10.9 | 98.8 | 2.50 | 0.24 | 0.75 |
| 18 – 54 | 62,442 | 24,480 | 4,050 | 89.5 | (88.6–90.4) | 64.3 | (63.9–64.7) | 10.5 | 35.7 | 14.8 | 98.9 | 2.51 | 0.16 | 0.77 |
| >= 55 | 45,029 | 12,372 | 2,353 | 79.9 | (78.3–81.5) | 75.4 | (75.0–75.8) | 20.1 | 24.6 | 15.2 | 98.6 | 3.25 | 0.27 | 0.78 |
EMS, emergency medical services; ISS, Injury Severity Score; sens, sensitivity; spec, specificity; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve.
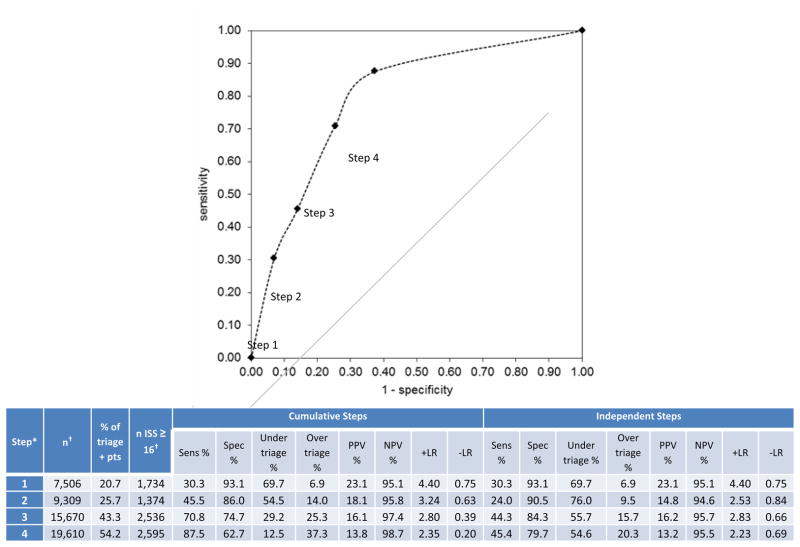
Diagnostic measures for each step of the Field Triage Decision Scheme (cumulative and independent) and the accompanying receiver operating characteristic (ROC) curve are depicted in Figure 2. The physiologic and anatomic criteria (steps 1 and 2) were highly specific, but insensitive for identifying major trauma patients, while mechanism and special considerations criteria (steps 3 and 4) increased sensitivity of the guidelines with modest reductions in specificity.
Figure 2.
Diagnostic metrics and receiver operating characteristic curve for identifying major trauma patients (ISS ≥ 16) using each “step” of the Field Triage Decision Scheme among 6 sites (n = 89,441). *Data were restricted to 6 sites, as the 7th site did not collect adequate information necessary to categorize the triage steps. Diagnostic metrics for the “Cumulative Steps” section includes patients from each of the previous incremental steps in the triage algorithm, while metrics for the “Independent Steps” section assesses each of the triage steps independently. There were 36,230 (40.5%) patients in the 6-site sample that met field triage criteria and 5,720 (6.4%) with ISS ≥ 16. The overall ROC value for the Field Triage Decision Scheme using the 6-site sample is 0.75. *Triage steps include: 1 (physiologic), 2 (anatomic), 3 (mechanism of injury) and 4 (special considerations). †The number of patients in each triage step is based on the total number of patients meeting triage criteria for each independent step. As patients can meet criteria from multiple different triage steps, the column totals for number of triage-positive patients and number of patients with ISS ≥ 16 will be greater than the actual number of patients (ie, the triage steps are not mutually exclusive). EMS, emergency medical services; ISS, Injury Severity Score; sens, sensitivity; spec, specificity; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve.
DISCUSSION
The findings in this multisite cohort study of injured patients triaged by EMS suggest that the sensitivity of the Field Triage Decision Scheme is lower than previously described, supporting several studies showing that a substantive percentage of patients with serious injuries are cared for in non-trauma hospitals.23–25 Further, only a minority of major trauma patients were identified by triage steps 1 and 2 (physiologic and anatomic criteria), with steps 3 and 4 (mechanism of injury and special considerations) serving to identify a larger portion of such patients with a modest decrement in specificity. Calculating diagnostic test measures based on triage criteria versus hospital destination also impacted values for triage accuracy at most sites. While trauma systems remain the model for regionalized healthcare, our results suggest that the ability to fully concentrate all major trauma patients in Level I or II trauma centers is not yet optimized. However, these results also raise questions regarding realistic goals for primary (field) trauma triage, the practical ability to fully concentrate seriously injured patients in high-resource hospitals through EMS and the potential role for secondary (hospital-based) triage.
According to ACSCOT, the target for under-triage in a trauma system is less than 5%.19 Under-triage can be defined either based on the ability of field triage criteria to correctly identify seriously injured patients (regardless of transport destination) or based on transport to a major trauma center (regardless of triage criteria). We calculated estimates using both of these perspectives, with generally similar findings. However, changing the definition did impact the apparent accuracy of trauma triage within individual sites. These findings are in contrast to previous trauma triage research suggesting under-triage rates of ≤ 5% for the ACSCOT criteria identifying patients with ISS ≥ 16,21,22 though variability in the triage criteria used, outcome definitions, patient sampling and study designs hamper direct comparisons with many previous studies. Closer examination of under-triaged patients reveal this group to be older, often suffering falls (and to a lesser extent motor vehicle crashes) with little physiologic derangement and relatively high rates of surgical intervention. The regions represented in this study have established trauma systems with demonstrated redistribution of seriously injured patients and improved survival.2,4,10 Therefore, these estimates approximate primary triage accuracy among well-developed trauma systems. It is possible that less established trauma and EMS systems may have different diagnostic accuracy for field triage.
While the accuracy of triage criteria among different age groups continues to be debated, our findings support results from other studies suggesting that under-triage is substantially worse among elders23,25,26 and to a lesser extent among children.24 Whether triage criteria are less sensitive or are applied more selectively to different age groups remains unclear. There are unique issues among older injured patients, including higher risks associated with operative intervention, increased comorbidity burden, greater potential for medical complications, different physiologic responses to injury, unclear benefit of trauma centers,1 and end-of-life considerations, all of which make this population unique. Whether separate elder-specific triage criteria should be used and the benefit of trauma care among seriously injured elders1 remain ongoing questions. As children were also under-triaged at a higher rate than adults in our study, these findings suggest that field trauma triage processes are most effective at identifying adult major trauma patients (18 to 54 years), but lose sensitivity at the ends of the age spectrum.
The rate of over-triage (defined as the proportion of patients with minor injuries meeting triage criteria or those with minor injuries transported to major trauma centers) was lower in this study compared to previous triage research. However, with the large number of injured patients cared for by EMS, even small rates of over-triage can produce large volumes of patients transported to major trauma centers, so consideration of the absolute numbers is also important. Our findings suggest that the field triage criteria are fairly selective in identifying major trauma patients and fall under the < 50% over-triage target set by ACSCOT.19 Comparing over-triage estimates between triage criteria (lower) and transport destination (higher) suggests that while the triage criteria appear to be used selectively, injured patients not meeting triage criteria are still frequently transported to major trauma centers. Notable exceptions are sites B and F, both of which had lower sensitivity and higher specificity for accuracy assessment by transport destination. Such findings suggest that some sites successfully identify most major trauma patients using field triage criteria, but are more selective in transporting these patients to major trauma centers (or integrate lower level trauma centers for the initial evaluation). We recently explored patient transport patterns and found that among patients not meeting field triage criteria, patient/family preference and to a lesser extent hospital proximity have major influence on transport destination, resulting in a substantive number of triage-negative patients being transported to major trauma centers.36 It is also notable that that mechanism of injury and special considerations criteria increased over-triage, but only modestly, while playing an important role in identifying many major trauma patients missed by the physiologic and anatomic criteria.
One likely reason for the differences between our results and those of previous triage research is the sampling frame. We used a comprehensive multi-site sampling strategy to capture all injured patients evaluated by EMS and therefore approximate the true denominator to who field triage guidelines are applied, rather than relying on more restrictive populations. The current sampling design yielded patients with both minor and serious injuries, transported to trauma and non-trauma hospitals and was therefore reflective of the full injured population evaluated and transported by EMS. Our study included both admitted patients and those discharged from the emergency department; the latter group has been excluded from most previous triage studies, but is still subject to field triage processes. We believe these methodological differences provided less biased estimates for triage accuracy and therefore closer approximation of the true performance of field triage, with greater generalizability of the study results. The improvement in specificity may be explained in part by including the broader denominator of patients to whom the triage guidelines are applied (e.g., patients transported to a hospital and subsequently discharged from the emergency department).
Previous triage research has used a multitude of definitions for “serious injury” including ISS ≥ 16,22,37–41 ISS ≥ 20,42 ISS ≥10 plus LOS,43 ISS plus resource use,22,44,45 and strictly resource-based definitions.46–50 This variability in outcomes has reduced comparability between studies. One mechanism to resolve such discrepancies is to link the target group in trauma triage research to the patient population most likely to benefit from trauma center care (i.e., patients with ISS ≥ 16,2,4,7,8,10 AIS ≥ 41). In concert with this perspective, we used ISS ≥ 16 to evaluate the diagnostic value of field triage in this study. Using an ISS ≥ 16 to define the target population for transport to major trauma centers is also consistent with maximizing the cost-effectiveness of trauma center care.51
Taken together, our findings suggest that there is opportunity for improvement in the field-identification of major trauma patients and matching patient need with hospital capability. However, improving the concentration of seriously injured patients in major trauma centers is likely more complicated than simply revising the triage criteria. There are logistical, financial and philosophical questions built into the optimization of matching need to capacity. A primary logistical question is defining which patients require immediate transport to a major trauma center and the timeliness of trauma center care.52–54 If a window of time exists during which “early” trauma center care still provides an outcome benefit (e.g., < 24 hours), the effective concentration of seriously injured patients in trauma centers may be most efficiently achieved through the combined efforts of primary (field) and secondary (hospital) triage. Our results suggest that the combined primary and secondary triage processes currently fail to fully concentrate major trauma patients in Level I/II trauma centers. These findings point towards a continued opportunity for developing more inclusive trauma systems, improved primary triage processes, formal transfer agreements between hospitals, timely interhospital transport processes, and more objective secondary triage instruments to further optimize the concentration of seriously injured patients in major trauma centers. The cost implications, cost effectiveness and future funding of trauma systems must also be considered. With the cost of care being notably higher in trauma centers51,55 and the cost effectiveness of trauma centers driven by younger patients with more severe injuries (i.e., AIS ≥ 4),51 expanding the field triage criteria to capture ≥ 95% of seriously injured patients runs the risk of substantially increasing the costs of trauma systems (i.e., through over-triage) without improving cost effectiveness. Considering the financial efficiency and costs of a trauma care are necessary aspects of preserving the viability of trauma systems, which continue to face constrained budgets,27 challenges of maintaining on-call panels,56,57 and a declining workforce of trauma surgeons.58
There are limitations in this study that must be considered when interpreting the results. A primary limitation is the retrospective study design. While we applied rigorous strategies for patient sampling, careful attention to identifying patients meeting field triage criteria and matching outcomes to patients regardless of hospital destination, the retrospective nature of the study still limits these findings. In addition, we did not directly measure the frequency of training for EMS personnel on field triage, EMS quality assurance processes and other local EMS factors that likely affect the application and use of field triage criteria. However, the broad inclusion criteria, sampling strategy, and variety of different EMS agencies, hospitals and regions included in this study are a substantial improvement in assessing the diagnostic value of field triage. Prospective efforts to validate the Field Triage Decision Scheme are currently underway.
We attempted to track outcomes for all injured patients transported by EMS, including those subsequently transferred to another hospital, though tracking interhospital transfers was challenging. This process involved delineating which hospital a patient was initially transport to, the location of final hospitalization (if a different hospital) and making certain assumptions about what occurred in between these events (i.e., interhospital transfer). While we were able to provide some assessment of the role of secondary triage in concentrating major trauma patients in Level I and II centers, there may have been additional interhospital transfers that we were unable to identify. Also, the data sources did not allow us to assess the timing of transfer. Furthermore, we did not assess the role of Level III and IV trauma centers and the potential for a tiered or staged process for field triage.
Certain analytic methods (probabilistic linkage and multiple imputation) were central to this study. Both of these methodologies have been well-studied and validated, though there remains the possibility that our findings may be different if outcomes were available for every injured patient evaluated by EMS (i.e., not restricted to patients with a matched hospital record). Because we took a more conservative strategy of restricting the primary analysis to EMS records that matched to a hospital record (including sites that did and did not have ED data available), it is possible that this strategy introduced some selection bias. However, inter-site comparisons did not suggest substantive differences by these factors.
CONCLUSIONS
In this multisite cohort investigation, the sensitivity of the Field Triage Decision Scheme for identifying major trauma patients was notably lower than previously described (particularly among injured elders), while the specificity was higher. Assessing the diagnostic value of field triage by initial or final transport to Level I and II trauma centers did not qualitatively change these findings. Efforts to further optimize trauma systems may incorporate refinement of trauma triage criteria and strengthening other aspects of trauma systems (e.g., secondary triage). The challenge going forward will be to develop, evaluate and integrate effective triage strategies for allocating trauma care in an increasingly resource- and cost-constrained healthcare environment without compromising the quality of trauma care or patient outcomes.
Acknowledgments
Funding
This project was supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program; the Oregon Clinical and Translational Research Institute (grant # UL1 RR024140); UC Davis Clinical and Translational Science Center (grant # UL1 RR024146); Stanford Center for Clinical and Translational Education and Research (grant # 1UL1 RR025744); University of Utah Center for Clinical and Translational Science (grant # UL1-RR025764 and C06-RR11234); and UCSF Clinical and Translational Science Institute (grant # UL1 RR024131). All Clinical and Translational Science Awards are from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
We want to acknowledge and thank all the participating EMS agencies, EMS medical directors, trauma registrars, and state offices that supported and helped provide data for this project.
Footnotes
Disclosure Information: Nothing to disclose.
Abstract presented at the American College of Emergency Physicians Research Forum, Las Vegas, NV, September 2010.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Eng J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 2.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 3.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565–581. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Mullins RJ, Veum-Stone J, Hedges JR, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40:536–545. doi: 10.1097/00005373-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Pracht EE, Tepas JJ, Celso BG, et al. Survival advantage associated with treatment of injury at designated trauma centers. Medical Care Research and Review. 2007;64:83–97. doi: 10.1177/1077558706296241. [DOI] [PubMed] [Google Scholar]
- 6.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Mullins RJ, Mann NC. Population-based research assessing the effectiveness of trauma systems. J Trauma. 1999;47:S59–66. doi: 10.1097/00005373-199909001-00013. [DOI] [PubMed] [Google Scholar]
- 8.Jurkovich GJ, Mock C. Systematic review of trauma system effectiveness based on registry comparisons. J Trauma. 1999;47:S46–55. doi: 10.1097/00005373-199909001-00011. [DOI] [PubMed] [Google Scholar]
- 9.Cooper A, Barlow B, DiScala C, et al. Efficacy of pediatric trauma care: results of a population-based study. J Pediatric Surg. 1993;28:299–303. doi: 10.1016/0022-3468(93)90221-6. [DOI] [PubMed] [Google Scholar]
- 10.Hulka F, Mullins RJ, Mann NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Traum. 1997;42:514–519. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Johnson DL, Krishnamurthy S. Send severely head-injured children to a pediatric trauma center. Pediatr Neurosurg. 1996;25:309–314. doi: 10.1159/000121145. [DOI] [PubMed] [Google Scholar]
- 12.Hall JR, Reyes HM, Meller JL, et al. The outcome for children with blunt trauma is best at a pediatric trauma center. J Pediatric Surg. 1996;31:72–77. doi: 10.1016/s0022-3468(96)90322-x. [DOI] [PubMed] [Google Scholar]
- 13.Pracht EE, Tepas JJ, Langland-Orban B, et al. Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatric Surg. 2008;43:212–221. doi: 10.1016/j.jpedsurg.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 14.Nirula R, Maier R, Moore E, et al. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer’s effect on mortality. J Trauma. 2010;69:595–599. doi: 10.1097/TA.0b013e3181ee6e32. [DOI] [PubMed] [Google Scholar]
- 15.Sampalis JS, Denis R, Frechette P, et al. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997;43:288–95. doi: 10.1097/00005373-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehospital Emergency Care. 2006;10:287–294. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 17.Field categorization of trauma patients. Bull Am Coll Surg. 1986;71:17–21. [Google Scholar]
- 18.Hospital and Prehospital Resources for the Optimal Care of the Injured Patient and Appendices A through J. Chicago, IL: American College of Surgeons; 1987. [Google Scholar]
- 19.Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 20.Centers for Disease Control and Prevention. Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage. MMWR. 2009;58:1–35. [PubMed] [Google Scholar]
- 21.Lerner EB. Studies evaluating current field triage: 1966–2005. Prehospital Emergency Care. 2006;10:303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 22.Norcross ED, Ford DW, Cooper ME, et al. Application of American College of Surgeons’ field triage guidelines by pre-hospital personnel. J Am Coll Surg. 1995;181:539–544. [PubMed] [Google Scholar]
- 23.Vassar MJ, Holcroft JJ, Knudson MM, Kizer KW. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003;197:717–725. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 24.Wang NE, Saynina O, Kuntz-Duriseti K, et al. Variability in pediatric utilization of trauma facilities in California: 1999 to 2005. Ann Emerg Med. 2008;52:607–615. doi: 10.1016/j.annemergmed.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Hsia RY, Wang E, Torres H, et al. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–24. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scheetz LJ. Effectiveness of prehospital trauma triage guidelines for the identification of major trauma in elderly motor vehicle crash victims. J Emerg Nurs. 2003;29:109–115. doi: 10.1067/men.2003.59. [DOI] [PubMed] [Google Scholar]
- 27.Mann NC, MacKenzie E, Teitelbaum SD, et al. Trauma system structure and viability in the current healthcare environment: a state-by-state assessment. J Trauma. 2005;58:136–147. doi: 10.1097/01.ta.0000151181.44658.0a. [DOI] [PubMed] [Google Scholar]
- 28.Clark DE. Practical introduction to record linkage for injury research. Injury Prevention. 2004;10:186–191. doi: 10.1136/ip.2003.004580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jaro MA. Probabilistic linkage of large public health data files. Statistics in Medicine. 1995;14:491–498. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 30.Dean JM, Vernon DD, Cook L, et al. Probabilistic linkage of computerized ambulance and inpatient hospital discharge records: a potential tool for evaluation of emergency medical services. Ann Emerg Med. 2001;37:616–626. doi: 10.1067/mem.2001.115214. [DOI] [PubMed] [Google Scholar]
- 31.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 32.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 33.Newgard CD, Haukoos J. Missing data in clinical research – part 2: Multiple imputation. Acad Emerg Med. 2007;14:669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 34.Newgard CD. The validity of using multiple imputation for missing prehospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–324. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Raghunathan T, Lepkowski, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- 36.Newgard CD, Nelson MJ, Kampp M, et al. Out-of-hospital decision-making and factors influencing the regional distribution of injured patients in a trauma system. J Trauma. 2011;70:1345–1353. doi: 10.1097/TA.0b013e3182191a1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Esposito TJ, Offner PJ, Jurkovich GJ, et al. Do out of hospital trauma center triage criteria identify major trauma victims? Arch Surg. 1995;130:171–176. doi: 10.1001/archsurg.1995.01430020061010. [DOI] [PubMed] [Google Scholar]
- 38.Knopp R, Yanagi A, Kallsen G, et al. Mechanism of injury and anatomic injury as criteria for out of hospital trauma triage. Ann Emerg Med. 1988;17:895–902. doi: 10.1016/s0196-0644(88)80666-8. [DOI] [PubMed] [Google Scholar]
- 39.Cooper ME, Yarbrough DR, Zone-Smith L, et al. Application of field triage guidelines by prehospital personnel: is mechanism of injury a valid guideline for patient triage? Am Surg. 1995;61:363–367. [PubMed] [Google Scholar]
- 40.Long WB, Bachulis BL, Hynes GD. Accuracy and relationship of mechanisms of injury, trauma score, and injury severity score in identifying major trauma. Am J Surg. 1986;151:581–584. doi: 10.1016/0002-9610(86)90553-2. [DOI] [PubMed] [Google Scholar]
- 41.Bond RJ, Kortbeek JB, Preshaw RM. Field trauma triage: combining mechanism of injury with the out-of-hospital index for an improved trauma triage tool. J Trauma. 1997;43:283–287. doi: 10.1097/00005373-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Cottington EM, Young JC, Shufflebarger CM, et al. The utility of physiologic status, injury site, and injury mechanism in identifying patients with major trauma. J Trauma. 1988;28:305–311. doi: 10.1097/00005373-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 43.West JG, Murdock MA, Baldwin LC, et al. A method for evaluating field triage criteria. J Trauma. 1986;26:655–659. [PubMed] [Google Scholar]
- 44.Newgard CD, Hui J, Griffin A, et al. Prospective validation of a clinical decision rule to identify severely injured children at the scene of motor vehicle crashes. Acad Emerg Med. 2005;12:679–687. doi: 10.1197/j.aem.2005.03.526. [DOI] [PubMed] [Google Scholar]
- 45.Simon BJ, Legere P, Emhoff T, et al. Vehicular trauma triage by mechanism: avoidance of the unproductive evaluation. J Trauma. 1994;37:645–649. [PubMed] [Google Scholar]
- 46.Henry MC, Hollander JE, Alicandro JM, et al. Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996;3:992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 47.Baxt WG, Jones G, Fortlage D. The Trauma Triage Rule: a new, resource-based approach to the out-of-hospital identification of major trauma victims. Ann Emerg Med. 1990;19:1401–1406. doi: 10.1016/s0196-0644(05)82608-3. [DOI] [PubMed] [Google Scholar]
- 48.Zechnich AD, Hedges JR, Spackman K, et al. Applying the trauma triage rule to blunt trauma patients. Acad Emerg Med. 1995;2:1043–1052. doi: 10.1111/j.1553-2712.1995.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 49.Phillips JA, Buchman TG. Optimizing out of hospital triage criteria for trauma team alerts. J Trauma. 1993;34:127–132. doi: 10.1097/00005373-199301000-00024. [DOI] [PubMed] [Google Scholar]
- 50.Engum SA, Mitchell MK, Scherer LR, et al. Prehospital triage in the injured pediatric patient. J Pediatr Surg. 2000;35:82–87. doi: 10.1016/s0022-3468(00)80019-6. [DOI] [PubMed] [Google Scholar]
- 51.MacKenzie EJ, Weir S, Rivara FP, et al. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]
- 52.Newgard CD, Schmicker R, Hedges JR, et al. Emergency medical services time intervals and survival in trauma: assessment of the “Golden Hour” in a North American prospective cohort. Ann Emerg Med. 2010;55:235–246. doi: 10.1016/j.annemergmed.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lerner EB, Moscati RM. The golden hour: scientific fact or medical “urban legend”? Acad Emerg Med. 2001;8:758–760. doi: 10.1111/j.1553-2712.2001.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 54.Lerner EB, Billittier AJ, Dorn JM, et al. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med. 2003;10:949–954. doi: 10.1111/j.1553-2712.2003.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 55.Goldfarb MG, Bazzoli GJ, Coffey RM. Trauma systems and the costs of trauma care. HSR. 1996;31:71–95. [PMC free article] [PubMed] [Google Scholar]
- 56.McConnell KJ, Johnson LA, Arab N, et al. The on-call crisis: a statewide assessment of the costs of providing on-call specialist coverage. Ann Emerg Med. 2007;49:727–733. doi: 10.1016/j.annemergmed.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 57.McConnell KJ, Newgard CD, Lee R. Changes in the cost and management of emergency department on-call coverage: evidence from a longitudinal statewide survey. Ann Emerg Med. 2008;52:635–642. doi: 10.1016/j.annemergmed.2008.01.338. [DOI] [PubMed] [Google Scholar]
- 58.Green SM. Trauma surgery: discipline in crisis. Ann Emerg Med. 2009;54:198–207. doi: 10.1016/j.annemergmed.2008.03.023. [DOI] [PubMed] [Google Scholar]