Abstract
Cutaneous leishmaniasis (CL) is a rising epidemic in Pakistan. It is a major public health problem in the country especially alongside regions bordering the neighboring Afghanistan and cities that have had the maximum influx of refugees. The purpose of our paper is to highlight the diverse clinical manifestations of the disease seen along with the geographic areas affected, where the hosts are particularly susceptible. This would also be helpful in presenting the broad spectrum of the disease for training of health care workers and help in surveillance of CL in the region. The increased clinical diversity and the spectrum of phenotypic manifestations noted underscore the fact that the diagnosis of CL should be not only considered when dealing with common skin lesions, but also highly suspected by dermatologists and even primary care physicians even when encountering uncommon pathologies. Hence, we would strongly advocate that since most of these patients present to local health care centers and hospitals, primary care practitioners and even lady health workers (LHWs) should be trained in identification of at least the common presentations of CL.
1. Background
Cutaneous leishmaniasis (CL) is a rising epidemic in Pakistan [1]. It is a major public health problem in the country especially alongside regions bordering the neighboring Afghanistan and cities that have had the maximum influx of refugees [2]. Pakistan in particular, as highlighted by Postigo, has been a focus of both anthroponotic cutaneous leishmaniasis caused by Leishmania tropica (L. tropica) and zoonotic CL caused by Leishmania major (L. major) with epidemics occurring in various parts of the country [3]. L. tropica is mostly seen in urban areas whereas L. major is more common in rural areas of the country [4].
The purpose of our paper is to highlight the diverse clinical manifestations of the disease seen along with the geographic areas affected where the hosts are particularly susceptible. This would also be helpful in presenting the broad spectrum of the disease for training of health care workers and help in surveillance of CL in the region [3].
2. Methodology for Our Review
We searched the terms “cutaneous”, “leishmaniasis,” and “Pakistan,” in Pubmed which retrieved a total of 67 articles. These articles were then systematically reviewed with focus on the number of people affected in different areas of the country and the clinical manifestations of the disease documented by the authors. A summary of the studies selected is outlined in Table 1. References citing other studies done in the region were then also studied for the aforementioned objectives.
Table 1.
Summary of studies in Pakistan on clinical manifestations of Cutaneous Leishmaniasis alongside their geographic distribution.†
| Period | City/province | Number of cases | Method of diagnosis | Species of Leishmania | Type of lesions seen | ||
|---|---|---|---|---|---|---|---|
| (1) | Gazozai et al. [8] | 2005–2007 | Quetta, Balochistan | 300 | Histopathological examination; skin smears | Nodules, plaques, ulcers and/or scarring | |
|
| |||||||
| (2) | Firdous et al. [4] | 2005–2007 | Quetta, Balochistan; adjoining areas noted included Sibi, Zhob, Loralai, Pishin, and Kohlu | 207 | Histopathological examination | L. major | 94% of lesions on upper and lower extremities in military personnel. 77 (37%) had a single lesion, 46 (19%) had two lesions, 19 (9%) had three lesions, and 35% had four lesions. The lesions were mostly noduloulcerative plaques with or without crusting |
|
| |||||||
| (3) | Kakarsulemankhel et al. [9] | 1996–2001 | Data from 7 zones of the province of Balochistan | School children: 17–22 years: 1617 cases 11–16 years: 2643 cases 5–10 years: 3210 cases 8,007 patients with active lesions presenting to hospitals/clinics. |
Survey data, clinical and/or histopathological examination employed in different regions | Dry lesions more common in Quetta; wet lesions in other 6 regions of the province. Both active lesions and scarring were noted | |
|
| |||||||
| (4) | Raja et al. [10] | 1998 | Balochistan | 1709 patients; 2% (37) had unusual presentations | Clinical and histopathology | These included acute paronychial, chancriform, annular, palmoplantar, zosteriform, and erysipeloid forms in a total of 37 patients | |
|
| |||||||
| (5) | Kassi et al. [1, 11] | Quetta, Balochistan | 166 | FNAC/Histopathology | Dry ulcerated lesions were noted to be more common on face, arms, and legs | ||
|
| |||||||
| (6) | Shoai et al. [12] | 1997–2001 | Karachi, Sindh (areas of origin of patients were noted from all 4 provinces, mainly from Sindh (40.5%) and Balochistan (28%)) | 175 | Histopathological examination and PCR | Both L. Tropica and L. major | h 60 (82.6%) showed wet type of lesions characterized by exudates, redness, and inflamed margins. The remaining 15 (17.3%) were of dry and nodular type covered by crust |
|
| |||||||
| (7) | Brooker et al. [13] | 2002-2003 | 19 neighboring villages in Balochistan and Khyber Pakhtunkhwa | 7,305 persons | Clinical diagnosis | Overall, 650 persons (2.3%) had anthroponotic CL (ACL) lesions only, 1,236 (4.4%) had ACL scars only, and 38 persons had both ACL lesions and scars | |
|
| |||||||
| (8) | Myint et al. [14] | 2008 | Samples from both Sindh and Balochistan: 48 cases from lowland areas; 21 cases from highland areas | 69 | Gene sequencing | 47 L. Major and 1 L. Tropica in lowland areas. 5 L. Major and 16 L. Tropica in highland areas. |
Again, no correlation between clinical presentation (wet, dry and/or mixed types of cutaneous lesions) and causal leishmania parasites |
|
| |||||||
| (9) | Bhutto et al. [15] | 1996–2001 | Jacobabad, Larkana, and Dadu districts of Sindh province and residents of Balochistan province | 1210 | Clinical; a giemsa-stained smear test and histopathology | Clinically, the disease was classified as dry papular type, 407 cases; dry ulcerative type, 335 cases; wet ulcerative type, 18 cases | |
|
| |||||||
| (10) | Bari et al. [7] | 2009 | Peshawar, Khyber Pakhtunkhwa | 2 | Slit skin smear and FNAC | Cutaneous fissures on lip and dorsum of finger | |
|
| |||||||
| (11) | Rahman et al. [5] | 2006–2008 | Peshawar, Khyber Pakhtunkhwa | 1680 498 patients from different areas of Peshawar; 688 from FATA; 89 from other urban and rural areas of the province |
Skin smear for LD bodies | Typical “oriental sore” noted in 1512 cases; 168 had an atypical presentation. Several chronic nonhealing ulcers were noted. | |
|
| |||||||
| (12) | Ul Bari and Ejaz [6] | 2009 | Peshawar, Khyber Pakhtunkhwa | 1 | Skin smear preparation | Rhinophyma-like plaque on nose | |
|
| |||||||
| (13) | Ul Bari [16] | 2009 | Peshawar, Khyber Pakhtunkhwa | 72 | Smear preparations/histopathological examination | Nasal leishmaniasis. Main morphological patterns included psoriasiform (30), furunculoid (8), nodular (13), lupoid (8), mucocutaneous (4), and rhinophymous (3) | |
|
| |||||||
| (14) | Qureshi et al. [17] | 2007 | Abbottabad, Khyber Pakhtunkhwa | 1 | Histopathology | Typical butterfly-like rash seen in SLE | |
|
| |||||||
| (15) | Saleem et al. [18] | 2004–2006 | Karachi, Sindh | 100 | Clinical and histopathological examination | Nodules, plaques, ulcers, crusted ulcers, lupoid lesions, and plaques with scarring were mainly noted | |
|
| |||||||
| (16) | Bhutto et al. [19] | 2009 | Larkana, Sindh | 108 | Polymerase chain reaction (PCR) | L. Major (105) L. Tropica (3) | |
|
| |||||||
| (17) | Ul Bari and Ber Rahman [20] | 2004–2006 | Punjab and Khyber Pakhtunkhwa | 60 | Slit-skin smear and histopathology | Presentation either (a) wet type (early ulcerative, rural) or (b) dry type (late ulcerative, urban) | |
|
| |||||||
| (18) | Rowland et al. [21] | 1997 | Timergara, Dir, Khyber Pakhtunkhwa | 9200 inhabitants | Clinical diagnosis; sample of cases confirmed with microscopy and PCR | Possible L. tropica based on Noyes et al. [22] | 38% of the 9200 inhabitants bore active lesions, and a further 13% had scars from earlier attacks |
|
| |||||||
| (19) | Mujtaba and Khalid [23] | 1995–1997 | Multan, Punjab | 305 | Giemsa-stained smear from the lesion | All the lesions were of the dry type. Most of the lesions (97%) were present on exposed areas of the body | |
|
| |||||||
| (20) | Ayub et al. [24] | 1999–2000 | Multan, Punjab | 173 | Smear for LD bodies | Clinically all the lesions were of dry type, with 67% present on legs | |
|
| |||||||
| (21) | Anwar et al. [25] | 2004 | Khushab district, Punjab | 105 | FNAC of the lesion for first 4 cases; only history and clinical assessment for remaining | Disseminated forms noted in multiple cases; with 1 patient with more than 50 lesions | |
|
| |||||||
| (22) | Bari and Rahman [26] | 2002–2006 | Rawalpindi, Sargodha, and Muzaffarabad | 718 patients with CL; study was on 41 patients with unusual presentations | Clinical and histopathological examination | Common unusual presentations noted were lupoid leishmaniasis in 14 (34.1%), followed by sporotrichoid 5 (12.1%), paronychial 3 (7.3%), lid leishmaniasis 2 (4.9%), psoriasiform 2 (4.9%), mycetoma-like 2 (4.9%), erysipeloid 2 (4.9%), and chancriform 2 (4.9%) | |
|
| |||||||
| (23) | Ul Bari and Raza [27] | 2006–2008 | Muzaffarabad, Azad Jammu and Kashmir | 16 | Histopathological examination | Cutaneous lesions resembling lupus vulgaris or lupus erythematosus, mainly over face. Morphological patterns included erythematous/infiltrated, psoriasiform, ulcerated/crusted, and discoid lupus erythematosus | |
†As noted, the province of Balochistan followed by Khyber Pakhtunkhwa appears to have taken a major toll. Most of the cities and hospitals where the disease has been identified serve as major tertiary care referral centers for the rest of the province. The exact estimates in adjoining cities and rural areas are underestimated and not well known.
3. Clinical Manifestations of Cutaneous Leishmaniasis
CL is usually noted on exposed parts of the body, mainly arms, face, and legs. The clinical manifestations are extremely diverse including unusual sites and atypical morphologies. Typically, the natural course of the lesions seen in CL is outlined by Figure 1. The lesions typically are not painful, but are associated with significant stigma associated with the disease (Figure 2). Women and children are particularly affected. As noted, however, it is increasingly seen in various unusual forms, for example, as fissures on lips, with lupoid features on face and/or psoriasiform plaques on nose [5, 6]. The myriad of manifestations seen is an outcome of the interplay between the parasite infection and host's immune responses [4]. “On one end of the spectrum of CL is the classical oriental sore in which spontaneous cure and immunity to reinfection is the result of an effective parasiticidal mechanism. On the other end of the spectrum is diffuse cutaneous leishmaniasis in which metastatic cutaneous lesions develop and the patient rarely, if at all, spontaneously develops immunity to the parasite” [7].
Figure 1.

Typical sequence of events leading to the formation of the typical oriental or “yearly sore” called “kal dana.” Description adopted from excellent review by Arfan u Bari et al., 2009. Picture of Sandflies obtain through the courtesy of Bruce Alexander, Research Fellow in Molecular and Biochemical Parasitology Group, Liverpool School of Tropical Medicine.
Figure 2.
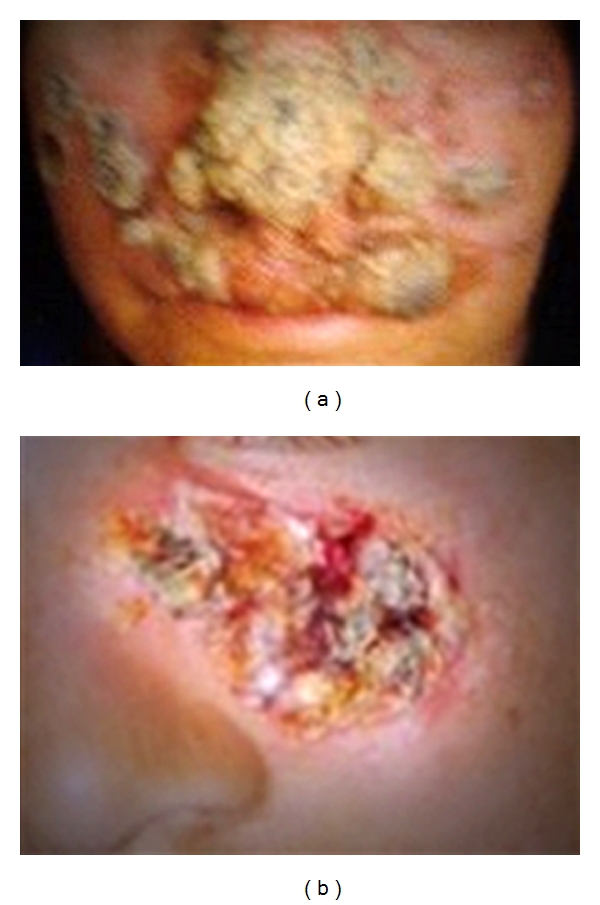
Disfiguring nature of lesions of CL on exposed parts of the body, particularly the face (copyright Kassi et al. [2]). Permission taken under creative commons attribution license.
4. Causative Agent in Pakistan
The main causative agent noted in our review of the studies was L. major followed by L. tropica. This was also highlighted in a review on molecular epidemiology of leishmaniasis in Asia, where in southern dry areas of the country, L. major was seen more often [28]. However, as noted by Katakura as well as Marco et al., there was no clear association between the skin lesions and the type of leishmaniasis, probably referring to host factors and immunoinflammatory responses being more important in determining the type and severity of lesions noted [28–31]. Likewise, no correlation between the type of CL lesions and the causal leishmania parasites was noted in a gene sequencing study on samples from both provinces of Sindh and Balochistan [14]. However, as outlined in Table 1, in the same study, there was indeed an association between the type of leishmania parasite and the altitude of the region, with L. major (97.9%) being the predominant type of parasite in lowland areas, while L. tropica (76.2%) was more common in highland areas [14]. L. tropica was also the strain most commonly found in a study from Multan and another study with a small sample size from various parts of the country [32, 33]. Clinical presentations appear to vary by endemic regions [31].
5. Distribution of Cutaneous Leishmaniasis in Pakistan
The country Pakistan is divided into 4 provinces: Punjab, Sindh, Khyber Pakhtunkhwa, and Balochistan along with Azad Jammu Kashmir (AJK). As noted from the research studies cited in Table 1, some parts of the country are more affected than others (Figure 3).
Figure 3.
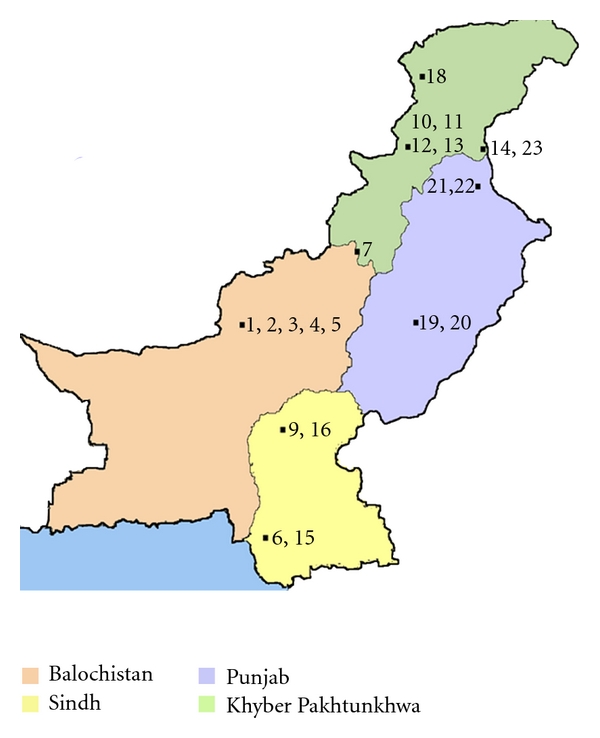
Distribution of CL in the 4 provinces of Pakistan (numbers represent the studies as noted in the references). As noted in the map as well, the province of Balochistan followed by Khyber Pakhtunkhwa appears to have taken a major toll. Most of the cities and hospitals where the disease has been identified serve as major tertiary care referral centers for the rest of the province. The exact estimates in adjoining cities and rural areas are underestimated and not well known.
Balochistan, the largest province by area located in the southwest of Pakistan, appears to have taken a significant toll followed by Khyber Pakhtunkhwa [9]. The geographic distribution, as noted by Firdous et al., is a function of the sandfly vector compounded with activities disturbing their habitat including wars as well as deforestation and agricultural activities [4, 34]. Breeding of animals is also thought to play a contributory role, along with “dark niches and cracks in the ground providing suitable habitat for the sandflies” [24, 28]. Within Balochistan, areas where most patients have been reported from are Quetta, Ormara, and Uthal [35]. Quetta is a metropolitan city and the capital of the province. Reasons for more cases of CL being reported from the capital of the province are that people belonging to different castes live there along with many refugees who were from the adjacent war-torn country of Afghanistan and migrated during the early 1980s and 1990s [1]. The hospitals and clinics serve as major teaching/tertiary care centers not only for the entire province but also for neighboring adjoining areas of Afghanistan.
The increased incidence noted in some parts of the country where major teaching hospitals and where most of the research studies are conducted may be a function of better awareness and more testing of chronic skin lesions for CL. Since a lot of these hospitals and research centers cater and serve as major referral centers for entire provinces in some cases, the true incidence especially in outskirts and rural areas is currently not exactly known and may be an underestimate [11]. For example, even in the survey-based study of thousands of school children, predominant population affected were male children; the severity and the proportion of women affected may not be entirely known given sociocultural factors [9].
6. The Road Ahead
The increased clinical diversity and the spectrum of phenotypic manifestations underscore not only fact that the diagnosis of CL should be not only considered when dealing with common skin lesions, but also highly suspected by dermatologists and even primary care physicians even when encountering uncommon pathologies [26]. Diagnosis in these atypical cases, which are now more frequently being seen, can particularly be challenging. Here, we would strongly advocate that since most of these patients present to local health care centers and hospitals, primary care practitioners and even lady health workers (LHWs) should be trained in identification of at least the common presentations of CL, since the majority of patients especially in rural areas do not have access to dermatologists [36]. Providing training to LHWs in identification of CL can prove helpful not only for women to whom they have access to but also in developing better surveillance systems of catching sporadic epidemics early.
A lot of research is being conducted by the efforts of local universities themselves and some interventions by NGOs and UNHCR. As noted by Brooker and colleagues as well, further work and interventions within the country of Pakistan would have to be supported by the Ministry of Health for improving diagnostic abilities and implementing preventive and treatment programs in more regions of the country before the epidemic continues to rise further [13].
7. Conclusions
CL is usually seen in exposed parts of the body.
The clinical manifestations are extremely diverse including unusual sites and atypical morphologies.
The myriad of manifestations seen is an outcome of the interplay between the parasite infection and host's immune responses.
The increased clinical diversity and the spectrum of phenotypic manifestations underscore not only fact that the diagnosis of CL should be not only considered when dealing with common skin lesions, but also highly suspected by dermatologists and even primary care physicians even when encountering uncommon pathologies.
Hence, we would strongly advocate that since most of these patients present to local health care centers and hospitals, primary care practitioners and even Lady Health Workers (LHWs) should be trained in identification of at least the common presentations of CL, since the majority of patients especially in rural areas do not have access to dermatologists.
Acknowledgments
The authors are deeply indebted to the Department of Pathology, Bolan Medical College, for their constant support and encouragement. The authors declare that they have no conflict of interests.
References
- 1.Kassi M, Kasi PM. Diagnosis of cutaneous leishmaniasis by fine needle aspiration cytology: a report of 66 cases. Tropical Doctor. 2005;35(1):50–51. doi: 10.1258/0049475053001804. [DOI] [PubMed] [Google Scholar]
- 2.Kassi M, Kassi M, Afghan AK, Rehman R, Kasi PM. Marring leishmaniasis: the stigmatization and the impact of cutaneous leishmaniasis in Pakistan and Afghanistan. PLoS Neglected Tropical Diseases. 2008;2(10, article e259) doi: 10.1371/journal.pntd.0000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Postigo JAR. Leishmaniasis in the World Health Organization Eastern Mediterranean Region. International Journal of Antimicrobial Agents. 2010;36(supplement 1):S62–S65. doi: 10.1016/j.ijantimicag.2010.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Firdous R, Yasinzai M, Ranja K. Efficacy of glucantime in the treatment of old world cutaneous leishmaniasis. International Journal of Dermatology. 2009;48(7):758–762. doi: 10.1111/j.1365-4632.2009.04072.x. [DOI] [PubMed] [Google Scholar]
- 5.Rahman S, Abdullah FH, Khan JA. The frequency of old world cutaneous leishmaniasis in skin ulcers in Peshawar. Journal of Ayub Medical College, Abbottabad. 2009;21(3):72–75. [PubMed] [Google Scholar]
- 6.Ul Bari A, Ejaz A. Rhinophymous leishmaniasis: a new variant. Dermatology Online Journal. 2009;15(3):p. 10. [PubMed] [Google Scholar]
- 7.U Bari A, Ul Bari A, Ejaz A. Fissure leishmaniasis: a new variant of cutaneous leishmaniasis. Dermatology Online Journal. 2009;15(10, article 13) [PubMed] [Google Scholar]
- 8.Gazozai SU, Iqbal J, Bukhari I, Bashir S. Comparison of diagnostic methods in cutaneous leishmaniasis (histopathology compared to skin smears) Pakistan Journal of Pharmaceutical Sciences. 2010;23(4):363–366. [PubMed] [Google Scholar]
- 9.Kakarsulemankhel JK. Cutaneous leishmaniasis in south west Pakistan: a preliminary study. Tarkiye Parazitoloji Degisis. 2004;28:5–11. [Google Scholar]
- 10.Raja KM, Khan AA, Hameed A, Ber Rahman S. Unusual clinical variants of cutaneous leishmaniasis in Pakistan. British Journal of Dermatology. 1998;139(1):111–113. doi: 10.1046/j.1365-2133.1998.02325.x. [DOI] [PubMed] [Google Scholar]
- 11.Kassi M, Tareen I, Qazi A, Kasi PM. Fine-needle aspiration cytology in the diagnosis of cutaneous leishmaniasis. Annals of Saudi Medicine. 2004;24(2):93–97. doi: 10.5144/0256-4947.2004.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shoaib S, Tauheed S, Hafeez A. Cutaneous leishmaniasis: an emerging childhood infection. Journal of Ayub Medical College, Abbottabad. 2007;19(4):40–41. [PubMed] [Google Scholar]
- 13.Brooker S, Mohammed N, Adil K, et al. Leishmaniasis in refugee and local Pakistani populations. Emerging Infectious Diseases. 2004;10(9):1681–1684. doi: 10.3201/eid1009.040179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myint CK, Asato Y, Yamamoto Y-I, et al. Polymorphisms of cytochrome b gene in Leishmania parasites and their relation to types of cutaneous leishmaniasis lesions in Pakistan. Journal of Dermatology. 2008;35(2):76–85. doi: 10.1111/j.1346-8138.2008.00419.x. [DOI] [PubMed] [Google Scholar]
- 15.Bhutto AM, Soomro RA, Nonaka S, Hashiguchi Y. Detection of new endemic areas of cutaneous leishmaniasis in Pakistan: a 6-year study. International Journal of Dermatology. 2003;42(7):543–548. doi: 10.1046/j.1365-4362.2003.01818.x. [DOI] [PubMed] [Google Scholar]
- 16.Ul Bari A. Clinical spectrum of nasal leishmaniasis in Muzaffarabad. Journal of the College of Physicians and Surgeons Pakistan. 2009;19(3):146–149. [PubMed] [Google Scholar]
- 17.Qureshi FA, Suliman MI, Sarwar J. Butterfly rash due to cutaneous leishmaniasis. Journal of the College of Physicians and Surgeons Pakistan. 2007;17(10):624–625. doi: 10.2007/JCPSP.624625. [DOI] [PubMed] [Google Scholar]
- 18.Saleem K, Ayaz B, Shaikh A. Histological grading patterns in patients of cutaneous Leishmaniasis. Journal of the College of Physicians and Surgeons Pakistan. 2007;17(11):650–653. [PubMed] [Google Scholar]
- 19.Bhutto AM, Soomro FR, Baloch JH, et al. Cutaneous leishmaniasis caused by Leishmania (L.) major infection in Sindh province, Pakistan. Acta Tropica. 2009;111(3):295–298. doi: 10.1016/j.actatropica.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Ul Bari A, Ber Rahman S. Correlation of clinical, histopathological, and microbiological findings in 60 cases of cutaneous leishmaniasis. Indian Journal of Dermatology, Venereology and Leprology. 2006;72(1):28–32. doi: 10.4103/0378-6323.19714. [DOI] [PubMed] [Google Scholar]
- 21.Rowland M, Munir A, Durrani N, Noyes H, Reyburn H. An outbreak of cutaneous leishmaniasis in an Afghan refugee settlement in north-west Pakistan. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1999;93(2):133–136. doi: 10.1016/s0035-9203(99)90285-7. [DOI] [PubMed] [Google Scholar]
- 22.Noyes HA, Reyburn H, Bailey JW, Smith D. A nested-PCR-based schizodeme method for identifying Leishmania kinetoplast minicircle classes directly from clinical samples and its application to the study of the epidemiology of Leishmania tropica in Pakistan. Journal of Clinical Microbiology. 1998;36(10):2877–2881. doi: 10.1128/jcm.36.10.2877-2881.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mujtaba G, Khalid M. Cutaneous leishmaniasis in Multan, Pakistan. International Journal of Dermatology. 1998;37(11):843–845. doi: 10.1046/j.1365-4362.1998.00469.x. [DOI] [PubMed] [Google Scholar]
- 24.Ayub S, Khalid M, Mujtaba G, Bhutta RA. Profile of patients of cutaneous leishmaniasis from Multan. Journal of the Pakistan Medical Association. 2001;51(8):279–281. [PubMed] [Google Scholar]
- 25.Anwar M, Hussain MA, Ur-Rehman H, Khan I, Sheikh RA. Epidemic of cutaneous leishmaniasis: 109 cases in a population of 500. Eastern Mediterranean Health Journal. 2007;13(5):1212–1215. doi: 10.26719/2007.13.5.1212. [DOI] [PubMed] [Google Scholar]
- 26.Bari AU, Rahman S. Many faces of cutaneous leishmaniasis. Indian Journal of Dermatology, Venereology and Leprology. 2008;74(1):23–27. doi: 10.4103/0378-6323.38402. [DOI] [PubMed] [Google Scholar]
- 27.Ul Bari A, Raza N. Lupoid cutaneous leishmaniasis: a report of 16 cases. Indian Journal of Dermatology, Venereology and Leprology. 2010;76(1):p. 85. doi: 10.4103/0378-6323.58698. [DOI] [PubMed] [Google Scholar]
- 28.Katakura K. Molecular epidemiology of leishmaniasis in Asia (focus on cutaneous infections) Current Opinion in Infectious Diseases. 2009;22(2):126–130. doi: 10.1097/QCO.0b013e3283229ff2. [DOI] [PubMed] [Google Scholar]
- 29.Marco JD, Bhutto AM, Soomro FR, et al. Multilocus enzyme electrophoresis and cytochrome B gene sequencing-based identification of Leishmania isolates from different foci of cutaneous leishmaniasis in Pakistan. American Journal of Tropical Medicine and Hygiene. 2006;75(2):261–266. [PubMed] [Google Scholar]
- 30.Rahman SB, ul Bari A. Comparative cellular immune host response in acute vs healed lesions of cutaneous leishmaniasis. Journal of Ayub Medical College, Abbottabad. 2006;18(3):7–12. [PubMed] [Google Scholar]
- 31.Murray HW, Berman JD, Davies CR, Saravia NG. Advances in leishmaniasis. The Lancet. 2005;366(9496):1561–1577. doi: 10.1016/S0140-6736(05)67629-5. [DOI] [PubMed] [Google Scholar]
- 32.Ayub S, Gramiccia M, Khalid M, Mujtaba G, Bhutta RA. Cutaneous leishmaniasis in Multan: species identification. Journal of the Pakistan Medical Association. 2003;53(10):445–447. [PubMed] [Google Scholar]
- 33.Rab MA, Al Rustamani L, Bhutta RA, Mahmood MT, Evans DA. Cutaneous leishmaniasis: iso-enzyme characterisation of Leishmania tropica . Journal of the Pakistan Medical Association. 1997;47(11):270–273. [PubMed] [Google Scholar]
- 34.Kassi M, Kasi PM, Marri SM, Tareen I, Khawar T. Vector control in cutaneous leishmaniasis of the old world: a review of literature. Dermatology Online Journal. 2008;14(6, article 1) [PubMed] [Google Scholar]
- 35.Shakila A, Bilqees FM, Salim A, Moinuddin M. Geographical distribution of cutaneous leishmaniasis and sand flies in Pakistan. Türkiye Parazitolojii Dergisi. 2006;30(1):1–6. [PubMed] [Google Scholar]
- 36.Khan SJ, Muneeb S. Cutaneous leishmaniasis in Pakistan. Dermatology Online Journal. 2005;11(1):p. 4. [PubMed] [Google Scholar]


