Abstract
Empirically-supported treatments for alcohol dependence exist, yet understanding of influences contributing to the intended behavior change is limited. The current study, a secondary analysis of the recent multi-site COMBINE trial (The COMBINE Study Research Group, 2003), tested a mediational model wherein change in client self-efficacy for abstinence was examined as a potential mediator of associations between client-report of the therapeutic bond and one-year outcomes of drinking frequency, drinking consequences, and psychiatric functioning. For analyses, the 1383 COMBINE trial participants were grouped as follows: 1) those receiving study medications (Naltrexone, Acamprosate, Naltrexone + Acamprosate, Placebo) and enrolled in medication management (MM) only (n=607), 2) those receiving study medications/MM and also enrolled in a combination behavioral intervention (CBI) as well (n=619), and 3) those enrolled in CBI only (n=157). Mediation analyses using the product-of-coefficients approach indicated self-efficacy change during treatment significantly mediated associations between the therapeutic bond with the CBI therapist and each of the three one-year outcomes among those exclusively receiving CBI, but failed to do so among those receiving pills/MM (with or without CBI). Effect sizes were small, but indicated that variance in bond-outcome associations was partially mediated by self-efficacy change for trial participants. Findings advance understanding of proximal client change processes during delivery of treatments for alcohol dependence.
Keywords: alcohol treatment, therapeutic bond, self-efficacy
Introduction
Promotion of evidence-based practice in addiction treatment has contributed to a growing list of empirically-supported practices (SAMHSA, 2010), yet progress identifying influences that contribute to the impact of such interventions in facilitating behavior change is less advanced (DiClemente, 2007; Nock, 2007). The need to better understand contributing influences to therapeutic change is amplified by a trend in addiction treatment trials to seek synergy by combining empirically-supported practices. An example is the work of the COMBINE Study Research Group (2003), which tested in a multi-site trial if treatment of alcohol dependence could be optimized via pharmacotherapy (e.g., naltrexone, acamprosate), medication counseling, and/or a combined behavioral intervention (CBI). Primary COMBINE publications (Anton et al., 2006; Donovan et al., 2008) document robust drinking reductions across nine treatment conditions, including a CBI-only group, and further analytic work would improve understanding of influences contributing to changes in alcohol consumption observed among trial participants.
Extant literature suggests 20–25% of untreated alcohol treatment trial enrollees (whether assigned to wait-list, placebo, or no-treatment control) achieve short-term abstinence (Moyer & Finney, 2002), but that percentage nearly doubles for those receiving structured treatment (Monahan & Finney, 1996). Further, these differential success rates appear to hold for the year following treatment conclusion (Weisner et al., 2003). Clearly, one's own drinking experience during early treatment stages is a robust predictor of subsequent abstinence (Charney et al., 2010; Ilgen & Moos, 2005; Moos & Moos, 2006). But what influences are associated with such proximal as well as more distal treatment success? Prior to the late 1990's, attempts to address this question primarily examined client demography/background (McLellan et al., 1994; Ornstein & Cherepon, 1985), with scant attention given to treatment process analyses (Morley et al., 1996). Fortunately, greater focus has been subsequently given to more dynamic, process-oriented treatment constructs as potential predictors of recovery/relapse.
Wampold (2001) notes the interpersonal bond between a provider and client, hereafter referred to as therapeutic bond, as a pervasive predictor of intervention response. Therapeutic bond is a core element of a multi-dimensional alliance construct (Saunders et al., 1989), of which clients' early perception predicts retention and outcome in pharmacological and behavioral treatments for substance dependence (Barber et al., 1999; De Weert-Van Oene et al., 2001; Dundon et al., 2008). This research also suggests an influence of early client-rated alliance on nondrinking outcomes, such as improvement in psychiatric functioning (Barber et al., 1999). In their review, Meier and colleagues (2005) note therapeutic bond as a consistent predictor of client engagement and retention in substance abuse treatment, but underscore the need to better identify client process(es) that mediate this association. Notably, extant literature has failed to find a consistent association between therapeutic bond and some salient client variables, such as motivation (Connors et al., 2000; Ilgen et al., 2006a; Joe et al., 1998). Even so, the treatment community would benefit from a more distilled understanding of mechanistic client processes associated with both therapeutic bond and alcohol treatment outcome.
A process that may help explain how therapeutic bond influences outcomes in treatments for alcohol dependence is the change in client self-efficacy for abstinence that occurs over the course of treatment. Self-efficacy, or the perceived ability to capably respond to a situation (Bandura, 1977), at treatment conclusion was inversely associated with prospective drinking in Project MATCH (1998). This finding has since been replicated in other addiction treatment trials (Hser, 2007; Laudet & Stanick, 2010). Self-efficacy change figures prominently in conceptualizations for many behavioral treatment approaches, including those underlying the COMBINE trial's CBI (Marlatt & Gordon, 1985; Miller & Rollnick, 1991; Nowinski et al., 1992). Thus, COMBINE investigators might expect self-efficacy change as an impact of CBI delivery, though whether it should also be an expected impact of other trial provisions is less clear-cut. The possibility that pharmacotherapy in alcohol treatment may actually undermine change in self-efficacy has been acknowledged (Moncrieff & Drummond, 1997). However, both trial medications are efficacious for initiation of abstinence (Mattson & Litten, 2005), and positive immediate impacts of COMBINE's medication management approach are documented (Ernst et al., 2008). If, as Bandura (1977) suggests, a primary antecedent of self-efficacy change is initial behavioral success, then it may also be the case that an initial positive response to pharmacotherapy could predict changes in self-efficacy.
Converging evidence from the field of cardiac rehabilitation (Burns & Evon, 2007) supports the testing of a model wherein self-efficacy change mediates associations between therapeutic bond and a range of treatment outcomes (i.e., cardiorespiratory fitness, weight loss, return to employment). Extant addiction treatment literature also offers some support for this prospective model. Prior analysis of Project MATCH data documents strong intercorrelation among the noted constructs, and that forming a strong therapeutic bond may provide a compensatory effect for clients with low initial self-efficacy (Ilgen et al., 2006b). These analyses did not formally test statistical mediation, nor did they examine associations between self-efficacy and non-drinking outcomes (e.g., psychiatric functioning). Still, their conduct on a dataset from a large multisite trial comparing alcohol treatment approaches mirrors that of the available COMBINE trial data. Given robust treatment effects on distal drinking and psychiatric functioning reported for aggregate COMBINE trial participants (Anton et al., 2006; Donovan et al., 2008; LoCastro et al., 2009), testing of the described mediation model appears warranted.
The current study was designed to examine potential contributing influences of therapeutic bond and self-efficacy change on one-year treatment outcomes, including drinking outcomes and psychiatric functioning. Secondary analyses of COMBINE data were conducted because of several appealing design features of the trial. These include: 1) enrollment of a fairly homogenous, alcohol-dependent, treatment-seeking population, 2) consistent measurement across nine trial conditions, which included client rating of therapeutic bond after an initial treatment session and client self-report of self-efficacy at both outset and conclusion of treatment, and 3) retrospective self-report measures of client drinking during the 16-week treatment interval as well as throughout the following year. All analyses accounted for rates of drinking during early treatment stages, with initial analyses examining relations between therapeutic bond, self-efficacy change, and one-year outcomes in drinking (e.g., frequency, consequences) and psychiatric functioning (e.g., global severity of self-reported symptoms). Therapeutic bond was hypothesized to be positively associated with self-efficacy change during treatment and inversely associated with one-year treatment outcomes. Self-efficacy change was also expected to be inversely associated with one-year treatment outcomes. The formative analysis tested if self-efficacy change mediated relations between therapeutic bond and one-year treatment outcomes.
Methods
This secondary analysis study utilizes data from the COMBINE study [“Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence” (The COMBINE Study Research Group, 2003)], a multi-site randomized trial. A total of 1,383 subjects were randomized into nine conditions across 11 U.S.-based treatment sites, and notably attrition did not differ by treatment condition. Treatment for all conditions was provided for 16 weeks, with participants followed for one year after its conclusion.
Participants
Recruitment in the COMBINE trial occurred through inpatient and outpatient referrals at the study sites and community. A total of 4,965 volunteers were pre-screened by telephone to determine initial meeting of eligibility criteria. Exclusion criteria included: dependence on a drug other than alcohol, nicotine, or cannabis; recent opioid use; presence of a psychiatric disorder requiring medication; presence of a unstable medical condition (e.g., serum liver enzyme levels > 3 times the upper limit of the normal range); use of any study medication in the 30 days prior to baseline; and use of any medication that would raise potential risks of study participation. Additionally, volunteers enrolled in COMBINE study met the following inclusion criteria: 1) a minimum weekly average of 14 (females) or 21 (males) drinks consumed for one month within the 3-month period prior to initiating abstinence, 2) a minimum of two heavy drinking days (defined as at least four drinks for females, five drinks for males) within the 3-month period prior to initiating abstinence, and 3) most recent alcohol consumption within the 3 weeks prior to study enrollment. Those meeting eligibility criteria were then required to report a breath alcohol content level of zero prior to completing consent and baseline assessments.
The sample included 1,383 participants, of which 69% were male. Ethnic distribution was: 76.8% Non-Hispanic White, 11.2% Hispanic American, 7.9% African American, 1.3% American Indian or Alaska Native, 1.3% multi-racial, and 0.3% Asian American or Pacific Islander (1.2% of the sample declined to answer or selected “other”). The median age was 44 years, with 71% reporting 12+ years of education, and 42% currently married. Retention rate did not differ significantly between treatment conditions. Within treatment, 94% completed all drinking data, while one year post treatment 82.3% provided complete drinking data.
Procedures
All trial procedures were approved by institutional review boards at the 11 COMBINE trial sites. Eligible participants provided informed consent, completed baseline assessment, and were randomly allocated to one of nine 16-week treatment conditions. Four conditions included a Medical Management (MM) intervention and prescription of Naltrexone, Acamprosate, Naltrexone + Acamprosate, and Placebo, respectively. A double-blind approach was followed for trial medications, such that clients and research staff were blind to medication assignments for the duration of treatment and throughout the one-year post-treatment assessment period. Four additional conditions paralleled those noted above, though with provision of the CBI added as follows: Naltrexone + CBI, Acamprosate + CBI, Naltrexone + Acamprosate + CBI, Placebo + CBI. The ninth treatment condition, CBI only, was used as a control for potential effects of pill-taking (The COMBINE Study Research Group, 2003).
Trial enrollees who received study medication were offered nine MM visits occurring at weeks 0, 1, 2, 4, 6, 8, 10, 12, and 16. The MM visits approximated a primary care approach. The initial MM visit involved clinician review of client symptoms followed by client receipt of education about alcohol dependence, recommendation of abstinence, instruction for daily medication adherence, and encouragement to attend support groups. The MM clinicians and clients also jointly developed individualized medication adherence plans. Subsequent MM visits involved review of recent medication adherence and drinking behavior, and revision of plans to reduce drinking or achieve abstinence as needed. Notably, elements of any specialty behavioral treatments were excluded from the MM intervention (Ernst et al., 2008).
Trial enrollees assigned to receive the CBI had a maximum of 20 sessions over 16 weeks, with the number of sessions based on therapist's determination of client need. An innovation of the CBI was its integration of motivational interviewing, cognitive-behavioral, and twelve-step facilitation approaches originally developed for Project MATCH (Longabaugh et al., 2005). Initially, an adaptation of motivational enhancement therapy was provided, and followed by a functional analysis assessment to determine appropriate CBI content modules. The nine available modules were: assertiveness training, drink refusal skills training, communication skills training, mood management, craving management, mutual support group facilitation, social/recreational counseling, social support for sobriety, and job finding. The remainder of the CBI included provision of chosen modules, and maintenance sessions to review progress.
Measures
A complete list of all instruments and schedule of assessments is included in a prior trial publication (The COMBINE Study Research Group, 2003). Participant demographics were recorded by research personnel at baseline, and used in the current report for sample description and selected covariates (e.g., gender) in analyses. Alcohol dependence severity, as measured at baseline via the Alcohol Dependence Scale [ADS; (Skinner & Allen, 1982)], was utilized as an additional covariate in analyses. Relevant instruments include those assessing therapeutic bond, self-efficacy, drinking frequency, drinking consequences, and psychiatric functioning.
Therapeutic Bond
The Working Alliance Inventory (Horvath & Greenberg, 1989) includes paired therapist and client Likert ratings (1=Never, 7=Always) and subscales for therapeutic bond, goals, and tasks. To reduce assessment burden, COMBINE investigators titrated assessment of alliance to client-report of the 12-item Bond subscale (Gastfriend et al., 2005) with subscale scores offering a possible range of 12–84. The instrument was administered by nonclinical research personnel after an initial treatment session. Trial participants enrolled in treatment conditions involving both MM and CBI completed separate forms for MM clinicians and CBI therapists (hereafter differentiated as Bond-MM and Bond-CBI, respectively). Wording differences between Bond-MM and Bond-CBI instruments were limited to referral to the MM provider as “clinician” and CBI provider as “therapist.” The correlation between Bond-MM and Bond-CBI among those completing both (n = 619) was r = 0.66 (p < 0.001). Distributions of both measures were similar [Bond-MM Mean (SD) = 73.76 (9.14), range of 31–84; Bond-CBI Mean (SD) = 72.34 (9.66), range of 18–84] with negative skew (p < 0.05), and large ceiling effects. Thirteen percent of MM enrollees and 9% of CBI enrollees reported the highest possible level of therapeutic bond (a score of 84). Internal consistency was acceptable (Cronbach α = 0.85 in both Bond-MM and Bond-CBI). Most trial participants (89.9% of CBI and 93.8% of MM) completed this instrument by the 4th treatment week and timing of completion was unrelated to subscale score (Bond-MM: r = −0.05, p = 0.10; Bond-CBI: r = −0.003, p = 0.94).
Self-efficacy
The Alcohol Abstinence Self-Efficacy scale (DiClemente et al., 1994) determined client confidence to abstain from alcohol in high-risk situations via self-report ratings on a 5-point scale (1=Not at all, 5=Extremely) encompassing subscales of negative affect, positive/social, physical concerns, and withdrawal/urges. This report focuses on assessments of self-efficacy conducted at baseline and at treatment conclusion (week 16). In this sample, confidence subscale scores exhibited excellent internal consistency (average Cronbach α = 0.97).
Drinking Frequency
Drinking frequency was calculated as the percentage of drinking days in the prior month Drinking frequency at baseline and at one-year post-treatment was calculated from Form-90 interviews (Miller & Del Boca, 1994), which gather information over a 90-day interval via a calendar method. Numerous studies have found Form 90 to be a highly reliable instrument (Tonigan et al., 1997). Further, COMBINE drinking reports were biologically verified (Anton et al., 2006). Drinking frequency during treatment was derived via the Timeline Follow-Back (Sobell & Sobell, 1995) using a calendar method whereby standard drinks on each day during treatment were assessed. In the current study, early-treatment percent drinking days (estimated by dividing the total number of drinking days during the second treatment month by 30) were included as a measure of early treatment response.
Drinking Consequences
The Drinker Inventory of Consequences (DrInC; (Miller et al., 1995) assessed consequences experienced as a result of drinking. Clients reported on a 4-point scale (0 = never, 3 = daily) the frequency of 45 drinking consequences. At both assessment points, DrInC scores were categorized as: (1) few or no consequences (DrInC score < 10), (2) medium consequences (DrInC score greater than or equal to 10 and less than 40), and (3) high consequences (DrInC score greater than or equal to 40). This categorization was based on the distribution of DrInC scores, and prior mixture analyses of the instrument (Wu & Witkiewitz, 2008). Internal consistency of DrInC in this sample was adequate (Cronbach α = 0.93). The current report includes analyses of DrInC data collected at baseline and one-year post-treatment.
Psychiatric Functioning
The 53-item Brief Symptom Inventory (BSI; (Derogatis, 1993) assessed self-reported psychiatric symptomatology (e.g., depression, anxiety, somatization, psychoticism) via ratings on a 5-point scale (0 = Not at all, 4 = Extremely). The BSI Global Severity Index provides a broad measure of psychiatric functioning, and internal consistency of this index was excellent in the COMBINE sample (Cronbach α = 0.97). The current report includes analyses of BSI data collected at baseline and one-year post-treatment.
Statistical Analyses
All models, described below, were estimated using Mplus version 5.21 (Muthen & Muthen, 2007). Considering the complex sampling design in the COMBINE study (participants recruited from 11 sites), all parameters were estimated using a weighted maximum likelihood function and all standard errors were computed using a sandwich estimator1 (the MLR estimator in Mplus for maximum likelihood estimation with robust standard errors). This method provides the estimated variance-covariance matrix for the available data and therefore all available data were included in the models. Maximum likelihood is a favored method for estimation when the dataset contains missing information, assuming it is missing at random (Schafer & Graham, 2002). Attrition analyses revealed no significant differences on any study variables between those with missing data and those with complete data.
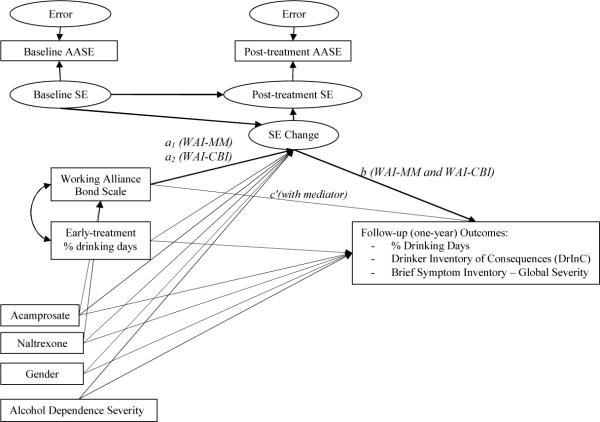
The path model shown in Figure 1 was used to examine direct associations between the predictor, proposed mediator, and outcomes. Three sets of models were estimated to account for the different treatment conditions in the COMBINE study. The first set of models included those individuals (n = 607) in the MM conditions who only completed the Bond-MM (they did not receive CBI). The second set of models included those individuals who received MM and CBI (n = 619), these individuals completed both the Bond-MM and Bond-CBI. Treatment medication conditions within the MM-only and the MM+CBI groups were further evaluated by including medication conditions as dummy-coded covariates in the first two sets of models. The final set of models included those individuals in the CBI-only condition (n = 157). The independent variables were the appropriate version(s) of the Bond scale, and early treatment response, as measured by percent drinking days during the second month of treatment. The proposed mediator was self-efficacy change, which incorporates its assessment at baseline and immediately following treatment. The three outcome domains were drinking frequency, drinking consequences, and psychiatric functioning—all assessed one year after treatment conclusion. Path analyses controlled for baseline levels of each of these outcomes, as well as medication treatment conditions in the set of MM models. Initial model testing with attendance at CBI and MM sessions as an additional covariate were also conducted to determine whether attendance could explain associations between therapeutic bond and self-efficacy change or outcomes. These preliminary models indicated that attendance predicted Bond-CBI and Bond-MM scores (p < 0.05), but was unrelated to both self-efficacy change and one-year treatment outcomes (all p > 0.20). Given these results and the attendance-by-treatment condition confound, we chose not to include attendance as a covariate in the final models presented below.
Figure 1.
Mediation model. SE= latent self-efficacy, as indicated by observed Alcohol Abstinence Self-Efficacy Scale (AASE) scores; WAI = Working Alliance Inventory – client report; MM = Medication Management conditions; CBI = Combined Behavioral Intervention conditions; SE Change = latent self-efficacy difference score; Regression paths for mediation models indicated by italics.
Latent difference score models were used to estimate changes in self-efficacy from baseline to the end of treatment. The latent difference score separates true score variance and measurement error in calculating change between observed variables across repeated measures (McArdle & Hamagami, 2001) using a latent variable model, rather than an observed change score as reliability and validity of both observed and residualized change scores have been questioned (Cronbach & Furby, 1970). The latent difference score was estimated by partitioning the observed scores at each time-point into true score and error:
and
| (1) |
where SEbaseline and SEpost-treatment are the observed scores for an individual at baseline and the end of treatment, respectively. The observed scores are defined by the true score at each time point (sebaseline and sebaseline) and measurement error at each time point (ebaseline and epost-treatment). The latent difference score (LDS) is then calculated by taking the difference in true scores:
| (2) |
Therapeutic bond and early-treatment percent drinking days were next incorporated as predictors of the latent self-efficacy difference score given by Equation 2. Gender and alcohol dependence scores were included as covariates given prior research identifying significant interactions between self-efficacy and both gender and alcohol dependence symptoms in the prediction of treatment outcomes (Greenfield et al., 2000; Sitharthan et al., 2003).
Mediation analyses were then conducted to determine whether the latent self-efficacy difference score mediated associations between therapeutic bond and post-treatment outcomes (drinking frequency, drinking consequences, and psychiatric functioning). Mediation analyses were conducted using the product of coefficients method (MacKinnon et al., 2002). This method involves multiplication of regression coefficients for regression of the mediator on the independent variable (a-path) and for regression of the outcome on the mediator (b-path) with the independent variable included in the model (c-path), and with a*b considered the mediated effect. As shown in Figure 1, the mediator was the latent self-efficacy difference score, the independent variables were bond, early-treatment percent drinking days, medication condition (for the MM models), gender and alcohol dependence, and the outcomes were drinking frequency, drinking consequences, and psychiatric functioning. Mediation models were tested separately for each outcome. Effect sizes, in the form of squared-partial correlation coefficients, were estimated for all paths in significant mediation effects (MacKinnon, 2008). The mediation effects were estimated in Mplus using a maximum likelihood estimator to obtain confidence intervals for the indirect effect.
The fit of all models was evaluated by χ2 values, the Root Mean Square Error of Approximation [RMSEA; (Browne & Cudeck, 1993)], and the Comparative Fit Index [CFI; (Bentler, 1990)]. Models with non-significant χ2, RMSEA less than 0.06 and CFI greater than 0.95 were considered a good fit to the observed data (Hu & Bentler, 1999) and models with significant χ2, RMSEA less than 0.08 and CFI greater than 0.90 were considered a reasonable fit.
Results
Descriptive Analyses
Correlations between primary study measures and descriptive statistics, shown in Table 1, indicate that baseline self-efficacy was inversely correlated with outcome measures at baseline. Therapeutic bond, with CBI therapists (below the diagonal) and MM clinicians (above the diagonal), was not associated with baseline self-efficacy, but was significantly correlated with early-treatment percent drinking days, post-treatment self-efficacy and was inversely related to each of the outcome measures at follow-up. Post-treatment self-efficacy was also significantly inversely related to mid-treatment percent drinking days and all follow-up outcome measures.
Table 1.
Correlations between Primary Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | MM Mean (SD) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Baseline Self-Efficacy | 1.00 | −.03 | −.09* | −.22* | .08 | .24* | −.11* | −.08 | −.09 | −.16* | 2.6 (.7) |
| 2. Baseline % Drinking Days | −.05 | 1.00 | −.05 | −.005 | −.14* | −.03 | −.13* | .26* | −.04 | −.06 | 74 (24) |
| 3. Baseline DrInC Score | −.20* | −.10* | 1.00 | .45* | −.03 | −.10* | −.09* | −.15* | .28* | .21* | 49 (21) |
| 4. Baseline BSI Global Index | −.25* | −.06 | .49* | 1.00 | −.10* | −.20* | .02 | −.03 | .26* | .49* | 60 (11) |
| 5. Working Alliance | .07 | −.01 | .01 | −.11* | 1.00 | .21* | −.19* | −.09 | −.18* | −.19* | 74 (9) |
| 6. Post-treatment Self-Efficacy | .15* | −.02 | −.17* | −.20* | .10* | 1.00 | −.43* | −.36* | −.42* | −.44* | 3.4 (.9) |
| 7. Early-treatment % Drinking Days | −.07 | .25* | −.05 | .02 | −.09* | −.38* | 1.00 | .53* | .38* | .27* | 25 (32) |
| 8. Follow-up % Drinking Days | .02 | .25* | −.12* | −.01 | −.15* | −.32* | .51* | 1.00 | .51* | .35* | 38 (37) |
| 9. Follow-up DrInC Score | −.07 | −.05 | .37* | .25* | −.15* | −.46* | .28* | .43* | 1.00 | .67* | 20 (21) |
| 10. Follow-up BSI Global Index | −.08 | −.02 | .31* | .51* | −.18* | −.42* | .18* | .27* | .68* | 1.00 | 51 (13) |
| CBI conditions Mean (SD) | 2.6(.7) | 75(26) | 47(20) | 60(11) | 72(9) | 3.5(.9) | 26(32) | 37(38) | 20(22) | 53(13) |
Notes. Correlations for the CBI Conditions are presented below the diagonal, whereas those for theMM Conditions are above the diagonal; DrInC = Drinker Inventory of Consequences; BSI = Brief Symptom Inventory; Post-treatment assessment refers to that occurring at end of treatment, follow-up assessment corresponds to that occurring one year following treatment;
p<0.05.
Path Analysis
The first aim of this study was to examine associations between therapeutic bond, early-treatment drinking, post-treatment self-efficacy, and outcomes at follow-up, while controlling for baseline levels of all outcome measures, and associations between outcome measures at baseline and follow-up. As described above, three sets of models were estimated for each outcome: one set of models was estimated for those who completed the bond measure for their MM clinician (MM only), one set of models for those who completed the bond measure for their MM clinician and CBI therapist (MM+CBI), and one set of models for those who completed the bond measure for their CBI therapist (CBI only). All estimated path models provided a reasonable fit to the observed data based on CFIs above 0.92 and RMSEA below 0.08.
Latent Difference Score models
The unconditional latent difference score model of self-efficacy from baseline to post-treatment was identified with the following model constraints: the effect of post-treatment self-efficacy regressed on baseline self-efficacy was constrained to 1.0, the difference score by self-efficacy at post-treatment effect was constrained to 1.0, and the mean and variance of post-treatment self-efficacy was constrained to 0.0. The regression equation for the latent difference score model can be written as:
| (3) |
where the intercept (3.02) is the average self-efficacy score across time, the regression coefficient (B (SE) −0.80 (0.06), p < 0.001) indicates a significant increase in self-efficacy over time (Mean SEbaseline = 2.61 (SD=0.74), Mean SEpost-treatment = 3.54 (SD=0.90)), and there is residual variance in the LDS (eLDS = 0.79). The significant increase in self-efficacy was evident in all sets of models: MM-only (Mean SEchange = 0.85 (SD=1.05)), MM+CBI (Mean SEchange = 0.98 (SD=1.06)), and CBI-only (Mean SEchange = 0.66 (SD=1.10). Post-hoc between group analyses indicated that self-efficacy change was significantly greater in the MM+CBI condition, in comparison to the MM-only and CBI-only conditions (F (2, 1091) = 4.94, p < 0.01).
Second, conditional models with the latent self-efficacy difference score regressed on early-treatment % drinking days, and bond for MM-only, MM+CBI, and CBI-only were estimated. Specific medication conditions, for MM-only and MM+CBI models, were included to control for differences among the corresponding sets of treatment conditions. Finally, alcohol dependence scores and gender were included to control for baseline sample characteristics. Early-treatment drinking was significantly related to the latent self-efficacy difference score in all three models (all p < 0.001), such that significant increases in self-efficacy from baseline to post-treatment was associated with lesser drinking frequency early in treatment. Baseline alcohol dependence scale scores were significantly associated with the latent self-efficacy difference score in the MM-only and MM+CBI models (MM-only: B(SE) = −0.02 (0.005), p < 0.001; MM+CBI: B(SE) = −0.02 (0.007), p = 0.005), but not in the CBI-only model (B (SE) = −0.004 (0.01), p = 0.76). Finally, bond scores were significantly associated with the self-efficacy difference score in the MM only and CBI only models (MM-only: B (SE) = 0.01 (0.004), p = 0.01; CBI-only: B(SE) = 0.03 (0.005), p < 0.05), such that significant increases in self-efficacy from baseline to post-treatment were predicted by higher bond scores. Gender was unrelated to the latent self-efficacy difference in all models (all p < 0.25). All three models explained 48% of the variance in the latent self-efficacy difference score.
Mediation Analyses
The final model, shown as Figure 1, examined whether latent change in self-efficacy mediated relations between bond and one-year outcomes. Significant mediation was determined by estimating 95% confidence intervals of the mediated effect (where 0.00 included in the interval would indicate non-significant mediation). Standardized regression coefficients for all models and all paths are provided in Table 2. The a-paths (first two rows of the table) provide respective estimates of the associations between the Bond-MM/Bond-CBI scores and latent change in self-efficacy from baseline to immediately following treatment. Across all sets of models the association between bond scores and self-efficacy change was strongest for the CBI-only condition (β's range from 0.21–0.23, all p < 0.01). The association between Bond-CBI and self-efficacy change in the CBI+MM conditions was non-significant. Across outcomes, the association between Bond-MM and self-efficacy change did not exceed β = 0.08. The b-path, which was the association between self-efficacy change and outcomes, was large and significant (all p < 0.01) for all sets of models, with regression coefficients ranging from β = −0.11 (self-efficacy predicting drinking frequency in the CBI+MM model) to β = −0.30 (self-efficacy predicting drinking frequency in the CBI-only model).
Table 2.
Standardized Regression Estimates (β) for Path Models predicting Outcomes One Year After Treatment
| Drinking frequency | Drinking consequences | Psychiatric functioning | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Paths | MM only | CBI+MM | CBI only | MM only | CBI+MM | CBI only | MM only | CBI+MM | CBI only |
| a1:WAI-MM→SE change | 0.08* | 0.06 | -- | 0.08* | 0.06* | -- | 0.08** | 0.06 | -- |
| a2:WAI-CBI→SE change | -- | −0.03 | 0.21** | -- | −0.04 | 0.23** | -- | −0.03 | 0.22** |
| b:SE Δ →Outcome | −0.14** | −0.11** | −0.30** | −0.18** | −0.28** | −0.18* | −0.19** | −0.25** | −0.20* |
| c′:WAI-MM→Outcome | 0.002 | −0.01 | -- | −0.12** | −0.09* | -- | −0.11* | −0.05 | -- |
| c′:WAI-CBI→Outcome | -- | −0.07 | −0.03 | -- | −0.05 | 0.04 | -- | −0.06 | 0.02 |
| a1*bWAI-MM indirect | −0.01 | −0.006 | -- | −0.01 | −0.02 | -- | −0.02 | −0.02 | -- |
| a2*bWAI-CBI indirect | -- | 0.003 | −0.06* | -- | 0.01 | −0.04* | -- | 0.01 | −0.04* |
| Gender→Outcome | −0.03 | −0.02 | −0.07 | 0.05 | 0.01 | 0.01 | 0.04 | −0.02 | −0.001 |
| ADS→Outcome | −0.15** | −0.10** | −0.18 | 0.12** | 0.06 | 0.01 | 0.16** | 0.05 | 0.17 |
| Acamp.→Outcome | 0.04 | −0.01 | -- | 0.03 | 0.03 | -- | −0.02 | 0.004 | -- |
| Naltrex.→Outcome | −0.001 | −0.06* | -- | 0.002 | −0.09** | -- | 0.00 | −0.08 | -- |
| Early-PDD→SE change | −0.42** | −0.34** | −0.36** | −0.43** | −0.34** | −0.38** | −0.44** | −0.34** | −0.38** |
| Early-PDD→Outcome | 0.47** | 0.47** | 0.35** | 0.21** | 0.06 | 0.25** | 0.34** | 0.23** | 0.32** |
Note.
p<0.05;
p<0.01.
SE change = self-efficacy latent difference score; WAI = Working Alliance Inventory; MM = Medication Management groups; CBI = Combined Behavioral Intervention groups; ADS = alcohol dependence scale; Acamp. = acamprosate conditions; Naltrex. = naltrexone conditions; Early-PDD = early-treatment % drinking days
The a1*b path provided the test of whether the latent change in self-efficacy significantly mediated the relation between bond and outcomes, with all other covariates (shown in Figure 1) included in the model. Across outcomes, self-efficacy change significantly mediated the association between Bond-CBI and outcomes in the CBI-only condition [(drinking frequency (95% CI: −0.06 - −0.01); drinking consequences (95% CI: −0.20 - −0.02); and BSI-Global severity: 95% CI: −0.12 - −0.01)]. Squared partial correlation coefficients for the associations between therapeutic bond, self-efficacy, and outcomes, controlling for baseline levels, indicated small effects (0.09 for the association between therapeutic bond and self-efficacy change, ranging from 0.003 to 0.04 for the association between therapeutic bond and outcomes, and ranging from 0.11 to 0.17 for the association between self-efficacy change and post-treatment outcomes).
Self-efficacy change did not significantly mediate the associations between Bond-MM or Bond-CBI and outcomes in the MM-only or MM+CBI conditions (all indirect effects: p > 0.10). Squared partial correlation coefficients for the associations between therapeutic bond (MM and CBI), self-efficacy, and outcomes, controlling for baseline levels, indicated small effects (0.005 and 0.009 for respective associations of Bond-MM and Bond-CBI with self-efficacy change, ranging from 0.003 to 0.02 for associations of bond with outcomes and ranging from 0.03 to 0.08 for associations of self-efficacy growth with outcomes).
Discussion
This report describes findings of a secondary analysis project utilizing data from a multi-site trial testing combination therapies for alcohol dependence (The COMBINE Study Research Group, 2003). Initial analyses were consistent with prior alcohol treatment research in that self-efficacy significantly increased during treatment (Finney et al., 1998), and the provider-client bond predicted one-year outcomes in drinking frequency, drinking consequences, and psychiatric functioning, (Barber et al., 1999; Barber et al., 2001). Mediation analyses using the product-of-coefficients approach indicated self-efficacy change during treatment significantly mediated associations between the therapeutic bond with the CBI therapist and one-year outcomes in the CBI-only condition, but did not significantly mediate bond-outcome associations among trial enrollees receiving medication (active or placebo), with or without CBI. Effect sizes were small, but indicate that variance in bond-outcome associations was partially mediated by self-efficacy change, with larger effects among those receiving CBI and no pills (or MM).
Study findings should be interpreted in a larger context of potential influences of alcohol treatment outcomes. A reliable finding in the current analyses was the prediction of one-year drinking outcome by early treatment drinking, which is consistent with a recent study (Charney et al., 2010). Admittedly, this appears a much more robust predictor than either therapeutic bond or self-efficacy change. Even so, bond predicted a range of one-year outcomes and—in models controlling for early treatment drinking—self-efficacy change partially mediated each of these associations among CBI-only trial participants. Thus, self-efficacy change accounted for unique variance in bond-outcome associations above and beyond that due to early treatment drinking, which adds to a rather equivocal extant literature concerning correlates of the therapeutic bond in delivery of behavioral approaches for substance misuse (Meier et al., 2005). Notably, the current mediation model is consistent with findings of recent analyses of Project MATCH (Ilgen et al., 2006b) as well as a behavioral intervention for cardiac rehabilitation (Burns & Evon, 2007).
Though mediation effects were consistent across outcome domains in the CBI-only condition, these were not replicated among those receiving study medications and medication management (MM). That clients' perceived bond with MM clinicians was reliably associated with distal outcomes, whether delivered alone or in conjunction with CBI, is consistent with other recent alcohol treatment literature (Dundon et al., 2008). Notably, greater mean change in self-efficacy was observed among trial participants receiving MM than those receiving CBI exclusively. Thus, it appears some of the influences related to self-efficacy change in these respective pharmacological and behavioral treatment approaches differ. It may be that those receiving trial medications perceived them as effective, and were apt to attribute behavioral successes to these medications rather than other aspects of their treatment provision (Toneatto et al., 1992). Clients who exclusively received CBI were absent a medication attribution, but also participated in a high-contact (up to 20 sessions over 16 weeks) CBI with interventionists trained in approaches that draw heavily on the building of client self-efficacy. Whether these aspects of the CBI help explain the observed mediation is difficult to know in the absence of access to practitioner fidelity data for this trial. This represents a potential avenue for future analyses by COMBINE investigators with access to the noted data.
It is important to differentiate statistical mediation from the specification of a causal mechanism of behavior change (Karno, 2007). The former signifies the meeting of a set of statistical conditions, and does not alone imply causality (Kraemer et al., 2002; MacKinnon et al., 2002). The latter, because it does suggest that the mechanism causes change in behavior, is a more extensive undertaking. Kazdin and Nock (2003, 2007) offer a framework for specifying mechanisms of behavior change that additionally includes tests of specificity, gradient, temporal sequence, experimental manipulation, and replication. The current study identified associations between therapeutic bond and one-year outcomes in treatments for alcohol dependence, and that—for trial participants exclusively receiving CBI—self-efficacy change partially accounted for these bond-outcome associations. This does not imply that a greater level of self-efficacy change causes or is caused by a strong bond, or that either construct causes better eventual treatment outcomes. Nor does it preclude the possibility that other constructs may similarly influence these variables. The current statistical mediation findings may be useful in spurring future research wherein self-efficacy change is put to additional tests in the context of behavioral treatment trials to better address Kazdin and Nock's (2003) aforementioned, remaining criteria.
This study is not without limitations. As a secondary analysis of COMBINE trial data, it is bound by methodological caveats of the original trial. As noted by Anton and colleagues (2006), these include limited treatment duration (i.e., 16 weeks) for a chronic illness with high relapse potential, exclusion of persons with substantial comorbid psychiatric difficulty, and assessment burden. Among other concerns is reliance on retrospective self-reports of drinking frequency and consequences, though notably biological verification of COMBINE drinking reports was found (Anton et al., 2006). Relatedly, the impact of therapeutic bond on the reliability of such self-report outcome assessments is unknown. A further concern relates to timing of assessment for some constructs. Concern for participant burden in this multi-site trial led to instrument pruning to those measuring key constructs, administered at salient points for detecting potential change. Consequently, the trajectory of self-efficacy growth during treatment, for instance, is unknown. Given current findings, future research may more closely examine this trajectory during the provision of treatments for alcohol dependence, and explore if self-efficacy growth relates to temporal change in other constructs (e.g., bond).
Noted caveats notwithstanding, the current study extends understanding of influences that contribute to effective treatments for alcohol dependence. Findings are consistent with extant research insofar as: 1) significant self-efficacy change occurred during pharmacological and behavioral treatments (Finney et al., 1998), 2) client perception of the therapeutic bond predicted one-year treatment drinking and psychiatric outcomes (Barber et al., 1999), and 3) self-efficacy change partially mediated these bond-outcome associations among those exclusively receiving a tailored behavior intervention (Burns & Evon, 2007; Ilgen et al., 2006b). While findings are modest and should be interpreted with both caution and the suggested caveats, they add to our understanding of the inner-workings of effective treatment approaches for alcohol dependence. Through further study, we may improve clinical practice with alcohol-dependent clientele.
Acknowledgements
This research was supported by National Institute on Alcohol Abuse and Alcoholism grant R21AA017137. The authors thank members of the COMBINE Study Research Group for their assistance in facilitating access to COMBINE study data.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
References
- Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence. The combine study: A randomized controlled trial. Journal of American Medical Association. 2006;295(17):2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Prentice Hall; New Jersey: 1977. [Google Scholar]
- Barber JP, Luborsky L, Crits-Cristoph P, Thase ME, Weiss RD, Frank A, et al. Therapeutic alliance as a predictor of outcome in the treatment of cocaine dependence. Psychotherapy Research. 1999;9:54–73. [Google Scholar]
- Barber JP, Luborsky L, Gallop R, Crits-Cristoph P, Frank A, Weiss RD, et al. Therapeutic alliance as a predictor of outcome and retention in the national institute on drug abuse collaborative cocaine treatment study. Journal of Consulting and Clinical Psychology. 2001;69:119–124. doi: 10.1037//0022-006x.69.1.119. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indices in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage Publications; Newbury Park: 1993. [Google Scholar]
- Burns JW, Evon D. Common and specific process factors in cardiac rehabilitation: Independent and interactive effects of the working alliance and self-efficacy. Health Psychology. 2007;26(6):684–692. doi: 10.1037/0278-6133.26.6.684. [DOI] [PubMed] [Google Scholar]
- Charney DA, Zikos E, Gill KJ. Early recovery from alcohol dependence: Factors that promote or impede abstinence. Journal of Substance Abuse Treatment. 2010;38:42–50. doi: 10.1016/j.jsat.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Connors GJ, DiClemente CC, Dermen KH, Kadden RM, Carroll KM, Frone MR. Predicting the therapeutic alliance in alcoholism treatment. Journal of Studies on Alcohol. 2000;61:139–149. doi: 10.15288/jsa.2000.61.139. [DOI] [PubMed] [Google Scholar]
- De Weert-Van Oene GH, Schippers GM, De Jong CA, Schrijvers GJ. Retention in substance dependence treatment: The relevance of in-treatment factors. Journal of Substance Abuse Treatment. 2001;20:253–264. doi: 10.1016/s0740-5472(01)00160-x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief symptom inventory: Administration, scoring, and procedures manual. National Computer Systems; Minneapolis, MN: 1993. [Google Scholar]
- DiClemente CC. Mechanisms, determinants, and processes of change in the modification of drinking behavior. Alcoholism: Clinical and Experimental Research. 2007;31(Supplement 10):13s–20s. doi: 10.1111/j.1530-0277.2007.00489.x. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, Hughes SO. The alcohol abstinence self-efficacy scale. Journal of Studies on Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Anton RF, Miller WR, Longabaugh R, Hosking JD, Youngblood M. Combined pharmacotherapies and behavioral interventions for alcohol dependence (the combine study): Examination of posttreatment drinking outcomes. Journal of Studies on Alcohol and Drugs. 2008;69:5–13. doi: 10.15288/jsad.2008.69.5. [DOI] [PubMed] [Google Scholar]
- Dundon WD, Pettinatti HM, Lynch KG, Xie H, Varillo KM, Makadon C, et al. The therapeutic alliance in medical-based interventions impacts outcome in treating alcohol dependence. Drug and Alcohol Dependence. 2008;95:230–236. doi: 10.1016/j.drugalcdep.2008.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst D, Pettinatti HM, Weiss RD, Donovan DM, Longabaugh R. An intervention for treating alcohol dependence: Relating elements of medical management to patient outcomes with implications for primary care. Annals of Family Medicine. 2008;6(5):435–440. doi: 10.1370/afm.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney JW, Noyes C, Coutts A, Moos R. Evaluating substance abuse treatment process models: Changes on proximal outcome variables during 12-step and cognitive behavioral treatment. Journal of Studies on Alcohol. 1998;59:371–380. doi: 10.15288/jsa.1998.59.371. [DOI] [PubMed] [Google Scholar]
- Gastfriend DR, Donovan DM, Lefebvre R, Murray KT. Developing a baseline assessment battery: Balancing patient time burden with essential clinical and research monitoring. Journal of Studies on Alcohol. 2005;Supplement #15:94–103. doi: 10.15288/jsas.2005.s15.94. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Hufford MR, Vagge LM, Muenz LR, Costello ME, Weiss RD. The relationship of self-efficacy and expectancies to relapse among alcohol dependent men and women: A prospective study. Journal of Studies on Alcohol. 2000;61:345–351. doi: 10.15288/jsa.2000.61.345. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Hser Y. Predicting long-term stable recovery from heroin addiction: Findings from a 33-year follow-up study. Journal of Addictive Diseases. 2007;26(1):51–60. doi: 10.1300/J069v26n01_07. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cut-off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Ilgen M, McKellar JD, Moos R, Finney JW. Therapeutic alliance and the relationship between motivation and treatment outcomes in patients with alcohol use disorder. Journal of Substance Abuse Treatment. 2006a;31:157–162. doi: 10.1016/j.jsat.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Ilgen M, Moos R. Deterioration following alcohol-use disorder treatment in project match. Journal of Studies on Alcohol. 2005;66:517–525. doi: 10.15288/jsa.2005.66.517. [DOI] [PubMed] [Google Scholar]
- Ilgen M, Tiet Q, Finney JW, Moos R. Self-efficacy, therapeutic alliance, and alcohol use disorder treatment outcomes. Journals of Studies on Alcohol. 2006b;67:465–472. doi: 10.15288/jsa.2006.67.465. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD, Broome KM. Effects of readiness for drug abuse treatment on client retention and assessment of process. Addiction. 1998;93:1177–1190. doi: 10.1080/09652149835008. [DOI] [PubMed] [Google Scholar]
- Karno MP. A case study of mediatiors of treatment effectiveness. Alcoholism: Clinical and Experimental Research. 2007;31(S3):33S–39S. doi: 10.1111/j.1530-0277.2007.00491.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44(8):116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Laudet AB, Stanick V. Predictors of motivation for abstinence at the end of outpatient substance abuse treatment. Journal of Substance Abuse Treatment. 2010;38:317–327. doi: 10.1016/j.jsat.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LoCastro JS, Youngblood M, Cisler RA, Mattson ME, Zweben A, Anton RF, et al. Alcohol treatment effects on secondary nondrinking outcomes and quality of life: The combine study. Journal of Studies on Alcohol and Drugs. 2009;70:186–196. doi: 10.15288/jsad.2009.70.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Zweben A, LoCastro JS, Miller WR. Origins, issues and options in the development of the combined behavioral intervention. Journal of Studies on Alcohol. 2005;Supplement #15:179–187. doi: 10.15288/jsas.2005.s15.179. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Erlbaum; Mahweh, NJ: 2008. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. [Google Scholar]
- Mattson ME, Litten RZ. Combining treatments for alcoholism: Why and how? Journal of Studies on Alcohol. 2005;Supplement #15:8–16. doi: 10.15288/jsas.2005.s15.8. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Metzger D, Grissom G, Woody GE, Luborsky L. Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: Role of treatment services. Journal of Consulting and Clinical Psychology. 1994;62:1141–1158. doi: 10.1037//0022-006x.62.6.1141. [DOI] [PubMed] [Google Scholar]
- Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: A critical review of the literature. Addiction. 2005;100:304–316. doi: 10.1111/j.1360-0443.2004.00935.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the form 90 family of instruments. Journal of Studies on Alcohol. 1994;Supplement 12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. Guilford Press; New York: 1991. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences (drinc): An instrument for assessing adverse consequences of alcohol abuse. U.S. Government Printing Office; Washington, D.C.: 1995. No. NIH Pub. No. 95-3911. [Google Scholar]
- Monahan SC, Finney JW. Explaining abstinence rates following treatment for alcohol abuse: A quantitative synethesis of patient, research design, and treatment effects. Addiction. 1996;91:787–805. doi: 10.1046/j.1360-0443.1996.9167876.x. [DOI] [PubMed] [Google Scholar]
- Moncrieff J, Drummond DC. New drug treatments for alcohol problems: A critical appraisal. Addiction. 1997;92(8):939–947. [PubMed] [Google Scholar]
- Moos R, Moos B. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101(2):212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley JA, Finney JW, Monahan SC, Floyd AS. Alcoholism treatment outcome studies, 1980–1992: Methodological characteristics and quality. Addictive Behaviors. 1996;21:429–443. doi: 10.1016/0306-4603(95)00073-9. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney JW. Outcomes for untreated individuals involved in randomized trials of alcohol treatment. Journal of Substance Abuse Treatment. 2002;23:247–252. doi: 10.1016/s0740-5472(02)00264-7. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus. version 5 Muthen & Muthen; Los Angelos, CA: 2007. [Google Scholar]
- Nock MK. Conceptual and design essentials for evaluating mechanisms of change. Alcoholism: Clinical and Experimental Research. 2007;31:4S–12S. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K. In: Twelve step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. DHHS, editor. Vol. 1. U.S. Government Printing Office; 1992. [Google Scholar]
- Ornstein P, Cherepon JA. Demographic variables as predictors of alcoholism treatment outcome. Journal of Studies on Alcohol. 1985;46:425–432. doi: 10.15288/jsa.1985.46.425. [DOI] [PubMed] [Google Scholar]
- Project MATCH Matching alcoholism treatments to client heterogeneity: Project match three-year drinking outcomes. Alcoholism: Clinical and Experimental Research. 1998;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- SAMHSA . National registry of evidence-based programs and practices. 2010. [Google Scholar]
- Saunders SM, Howard KI, Orlinsky DE. The therapeutic bond scales: Psychometric characteristics and relationship to treatment effectiveness. Psychological Assessment. 1989;1:323–330. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Sitharthan T, Job RFS, Kavanaugh DJ, Sitharthan G, Hough M. Development of a controlled drinking self-efficacy scale and appraising its relation to alcohol dependence. Journal of Clinical Psychology. 2003;59:351–362. doi: 10.1002/jclp.10127. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology. 1982;91:199–209. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- The COMBINE Study Research Group Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: Rationale and methods. Alcoholism: Clinical and Experimental Research. 2003;27:1107–1122. doi: 10.1097/00000374-200307000-00011. [DOI] [PubMed] [Google Scholar]
- Toneatto T, Sellers EM, Sobell LC, Sobell MB. Perception of whether drug or placebo has been administed is a determinant of drinking reduction. In: Naranjo CA, Sellars EMI, editors. Novel pharmacological interventions for alcoholism. Springer-Verlag; New York: 1992. pp. 262–264. [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58(4):358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Wampold BE. The great psychotherapy debate: Models, methods, and findings. Lawrence Erlbaum Associates; Mahwah, NJ: 2001. [Google Scholar]
- Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- Wu J, Witkiewitz KA. Network support for drinking: An application of multiple groups growth mixture modeling to examine client-treatment matching. Journal of Studies on Alcohol and Drugs. 2008;69(1):21–29. doi: 10.15288/jsad.2008.69.21. [DOI] [PMC free article] [PubMed] [Google Scholar]