Abstract
Introduction
The objective of this study is to identify (1) the current role of simulation in medical student emergency medicine (EM) education; (2) the challenges to initiating and sustaining simulation-based programs; and (3) educational advances to meet these challenges.
Methods
We solicited members of the Clerkship Directors in Emergency Medicine (CDEM) e-mail list to complete a Web-based survey addressing the use of simulation in both EM clerkships and preclinical EM curricula. Survey elements addressed the nature of the undergraduate EM clerkship and utilization of simulation, types of technology, and barriers to increased use in each setting.
Results
CDEM members representing 60 EM programs on the list (80%) responded. Sixty-seven percent of EM clerkships are in the fourth year of medical school only and 45% are required. Fewer than 25% of clerkship core curriculum hours incorporate simulation. The simulation modalities used most frequently were high-fidelity models (79%), task trainers (55%), and low-fidelity models (30%). Respondents identified limited faculty time (88.7%) and clerkship hours (47.2%) as the main barriers to implementing simulation training in EM clerkships. Financial resources, faculty time, and the volume of students were the main barriers to additional simulation in preclinical years.
Conclusion
A focused, stepwise application of simulation to medical student EM curricula can help optimize the ratio of student benefit to faculty time. Limited time in the curriculum can be addressed by replacing existing material with simulation-based modules for those subjects better suited to simulation. Faculty can use hybrid approaches in the preclinical years to combine simulation with classroom settings for either small or large groups to more actively engage learners while minimizing identified barriers.
INTRODUCTION
The increasing role of simulation technology in physician training during residency is well documented in emergency medicine (EM) and other specialties but is not as clearly defined for medical students.1–5 As a teaching tool, simulation engages learners and allows for deliberate practice. Learning modalities such as procedural task trainers, as well as high- and low-fidelity simulation, can help mitigate variations in clinical experiences during medical training. High-fidelity simulation, especially when combined simultaneously with other teaching modalities, allows students to experience learning in an immersive environment. Unlike learning with real patients, simulation allows educators to control the environment and ensure desired learning objectives are met while permitting increased student autonomy without patient safety risks.
Increasingly, undergraduate medical training programs incorporate simulation as a teaching modality. Simulation technology has been used to train students in cardiac and respiratory management,6 trauma management,7 and laparoscopy skills.8 Reports often focus on procedural skills or clinical management, revealing excellent student satisfaction but with little data supporting improved educational outcomes.
Simulation is also useful for teaching basic science concepts in preclinical medical education. Medical students have been taught concepts in shock,9 cardiovascular,10–12 and neuroscience13 physiology. Undergraduate education in EM is also well suited for using simulation technology. In many institutions, EM faculty are heavily involved with teaching basic physician procedures to medical students.14 The recommended EM clerkship curriculum15 consists of many acute and/or critical care topics that can be safely and effectively reproduced for medical students using simulation.
We completed this investigation to determine the current state of simulation use in medical student EM clerkships and by EM faculty in preclinical years, to identify unique challenges associated with the implementation of simulation teaching for undergraduates, and to offer educational advances to meet these challenges.
METHODS
Study Design and Population
A Web-based survey was administered to the Clerkship Directors in Emergency Medicine (CDEM) e-mail list, in preparation for a session at a national meeting for emergency medicine educators. CDEM members are academically affiliated emergency physicians and include EM clerkship directors, assistant clerkship directors, residency program directors and assistant/associate program directors, simulation directors, and other EM faculty interested in undergraduate medical education. Seventy-five institutions are represented on the list. Inclusion criteria included membership on the e-mail list group and voluntary completion of the survey instrument.
Survey Design and Administration
The survey was created by using www.surveymonkey.com and distributed through the e-mail list. Respondents provided demographic information (academic title, institution, in which academic year(s) the EM clerkship is offered, and the number of didactic hours provided). Survey items queried the type of technology used (high fidelity, low fidelity, task trainers, standardized patients), extent of use (as a percentage of available didactic time), and barriers to increased use of simulation. “High fidelity” refers to computer-controlled mannequins with advanced features such as pulses, physical examination findings, and the ability to perform procedures, while “low-fidelity” mannequins lack those capabilities and serve more as physical props or procedural task trainers than as interactive simulated patients. Respondents indicated whether their schools' preclinical curricula included exposure to simulation technology and listed barriers to increasing simulation use. Responses were collected, compiled, and analyzed anonymously.
This study was approved by the local institutional review board.
RESULTS
Sixty-four CDEM members (64% of 100 individuals on the list) responded to the survey, representing 60 institutions (80% of 75 institutions represented on the list). Four programs submitted duplicate responses from 2 different educators at the same institution. When duplicate responses were found, data from the respondent identified as the clerkship director were used to report year of clerkship and whether the EM clerkship is mandatory. For all other questions, all responses were used. These responses were included in the summary results. Most represented programs (97%) have EM experiences in the fourth year of medical school, with 67% in the fourth year only. Only 3% of programs offer exclusively third-year exposure. Almost half (45%) are required clerkships. Most respondents (83%) stated that simulation is available to students at their institution during preclinical years.
Simulation in the Clerkship
For most clerkships (> 60%), fewer than 25% of didactic hours use any type of simulation technology, including high fidelity (79% of respondents), task training (55%), and low fidelity (30%), with some clerkships containing no simulation experiences at all. Other modes noted by respondents include computerized cases and suture or airway laboratories, which could be considered under the heading of task trainers (Figure, part a).
Survey respondents stated that limited faculty time (88.7% of respondents) and clerkship hours (47.2%) are the most common barriers to implementing simulation training for medical students. Lack of financial resources and technical expertise were also cited as anticipated difficulties. Other concerns include faculty training and the cost associated with initiating a new simulation program (Figure, part b).
Simulation in the Preclinical Curriculum
Survey respondents described student exposure in the preclinical years to standardized patients (77.6%), high-fidelity simulators (67.3%), low-fidelity models, and task trainers (Figure, part a). Most respondents (95%) felt that students would benefit from more exposure to simulation before beginning clinical training.
They listed institutional support in terms of financial resources and faculty time, as well as volume of students and difficulties with incorporation into the preclinical curriculum, as the main barriers to providing more simulation exposure to preclinical students (Figure, part c).
DISCUSSION
Simulation in the Clerkship
Our results show that simulation exposure during the EM clerkship is highly variable. No published educational standards exist to define an ideal amount of exposure time, but the EM educators who responded desire more simulation time in medical student education. Future efforts should attempt to identify how much exposure is necessary to elicit the desired educational benefit. Challenges to greater use include faculty time and available clerkship time, similar to previous reports.3 Respondents also identified training, financial resources, and developmental difficulties as challenges. A proposed solution to some of these barriers is to start small, approaching simulation as an additional teaching tool to support existing curricular learning objectives. The limited simulation exposure reported by survey respondents implies that use of this approach may already be common. Choosing 1 or 2 particular topics that may lend themselves to a change may help when a program desires simulation but has not incorporated it into the curriculum owing to uncertainty about how to begin. This avoids a complete curricular overhaul, while still providing experience with simulation to learners and educators.
When simulation sessions replace another teaching method in the curriculum, the barriers of limited clerkship time and faculty time are largely addressed. The EM faculty at Wright State University Boonshoft School of Medicine used this approach to replace most group discussion sessions in their fourth-year medical student core curriculum with simulation. In a randomized controlled trial, they demonstrated high student satisfaction scores and increased examination scores for material taught with simulation compared to group discussion.16 Students at MetroHealth Medical Center/Case Western Reserve University are incorporated into resident simulation sessions during EM residency conference. These hybrid simulation sessions (using multiple modalities) do not add more time to either the resident or student curriculum.17 Simulation has also been used to replace vivisection in medical school, which may reduce long-term cost and time commitment.18
Although the literature addressing improved student performance may be inconclusive,16–20 simulation has been shown to have a positive impact in a number of other trainee groups.21–24 Incorporating high-fidelity simulation into emergency medicine clerkships allows reproduction of physiologic extremes, and students can practice critical care scenarios for critically ill patients without interruption from faculty.25
Many medical student experiences focus on stable patients for whom rapid focused evaluation, quick decision making, and an abbreviated presentation to faculty/consultants are not essential components. For ethical reasons, we do not permit medical students to have complete autonomy in the evaluation and treatment of critical patients. However, immediately after becoming interns, they are at risk of being responsible for the evaluation and treatment of a critically ill or injured patient for a finite period until a more experienced clinician arrives. This is not just limited to EM, but applies at least as much to any intern responding to the bedside of a patient admitted to the hospital for 1 problem, but who develops chest pain, shortness of breath, altered mental status, or some other acute problem while in the hospital.
Although it takes time to create, field test, and deploy a simulation, the same holds true in the development of any new teaching session or lecture. A new simulation session can be used repeatedly with periodic updates, similar to a core lecture. Repeated use and refinements to the teaching session with different groups of students do not require the same time commitment as the initial creation phase. Limiting simulation to just a single topic can minimize required time and provide experience for future efforts. Faculty development opportunities are essential for the success of faculty who are new to simulation, as some of the skills for successful implementation of a case may be unfamiliar, such as debriefing skills, use of evaluation checklists, performance feedback, and observation during live scenarios. Local expert mentors, courses at national meetings, and participation in national simulation organizations are all ways that new faculty can gain experience with these teaching tools.
Financial challenges are universal for any developing simulation program. Interested parties should consider resource-sharing agreements, where the equipment and cost is shared among multiple programs, and starting small by focusing purchases based on selected learning objectives. For example, task trainers for teaching procedural skills are significantly less costly than high-fidelity simulation models, and a simple rhythm generator may suffice in place of an expensive mannequin for rhythm-recognition practice. Simulation educators should decide what capabilities are desired and use their budget in the most efficient manner. Cost, learning objectives, desired fidelity and model capabilities should be closely analyzed before any large purchase.
Simulation in Preclinical Education
Simulation experiences are also highly desired by faculty in preclinical education. Challenges to adoption are similar to those for the clerkship, with some important differences.
Student volume is a major barrier to providing increased preclinical experiences. Large-group simulation is feasible and effective, both for basic science concepts13,26 and clinical correlates of physiology.27 In the former model, a simulator is transported to a class of medical students and a session is presented to the entire group at once. This approach reduces costs by not requiring a dedicated simulation laboratory. The second model involves rotating smaller groups through the simulation laboratory, with other students observing through an audiovisual feed, while a faculty proctor assists participants interacting with a simulated patient. Alternatively, computer-based simulation, instead of high-fidelity mannequins, has been shown to be an effective method to accommodate large numbers of students.28–30
Simulation experiences such as those described earlier, supervised by EM faculty, can also help to increase student exposure to EM before clinical clerkships, with the goal of introducing students to EM as a career choice and to EM faculty with whom they might interact in the future.
LIMITATIONS
Our survey population may not be representative of the entire body of EM educators, as it is a self-selected group of faculty with an expressed interest in undergraduate medical education. Approximately half of EM training programs are represented on the CDEM e-mail list, and not all of the programs represented on the list had faculty who responded to the survey. Data about simulation exposure, barriers, and hours of didactic time were included from all respondents, recognizing that there may be some subjectivity based on role of the respondent in the clerkship. While this may slightly affect the numerical response calculations, inclusion of these educators' viewpoints was considered important.
CONCLUSION
Simulation is an exciting, well-accepted format for incorporating experiential learning into the undergraduate medical curriculum. The experience that EM educators have in caring for patients with undifferentiated critical illnesses makes them well suited to bringing simulation into the medical student curriculum. In many institutions, EM educators are already integral parts of the simulation centers. Simulation can be integrated across all 4 years of medical education, providing links to clinical learning during the preclinical years and more autonomous practice in the clinical years. Identifying opportunities and barriers to implementation are the first steps in using simulation successfully in a preclinical or clerkship teaching program. The discussion provided here can serve as an outline for brainstorming and planning sessions to assist interested faculty in the development of expanded simulation programs for medical students.
FUTURE DIRECTIONS
Future efforts may focus on defining optimal exposure time to simulation for students in both clinical and preclinical years, as there are currently no accepted guidelines for how much simulation training is educationally beneficial. Identifying the preclinical topics that lend themselves most directly to simulation experience is important, as well as determining which types of patient encounters and learning objectives are most appropriate for students in their clinical rotations. This type of information would be extremely valuable to supplement and enhance the recently updated EM clerkship curriculum and objectives.15
Footnotes
Supervising Section Editor: Douglas S. Ander, MD
Volume 12, no. 4 :XXXX 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Figure.
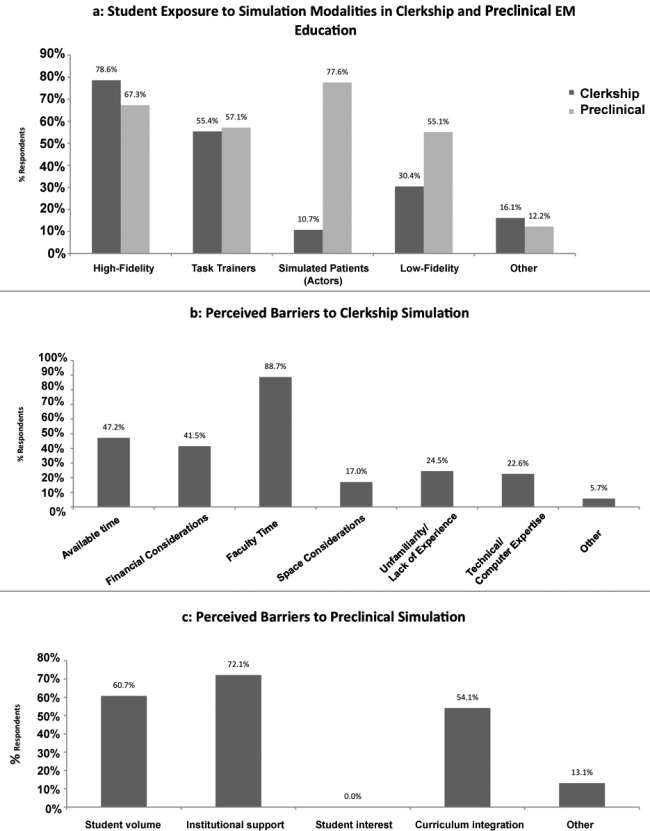
Results of a survey completed by members of the Clerkship Directors of Emergency Medicine. a, Combined answers to the questions “To what simulation modalities are students exposed in the emergency medicine (EM) clerkship?” and “To what simulation modalities are students exposed during preclinical years?” b, Respondents' perceived barriers to further implementation of simulation in the EM clerkship. c, Respondents' perceived barriers to further implementation of simulation in preclinical medical student education.
REFERENCES
- 1.McLaughlin S, Fitch MT, Goyal DG, et al. Simulation in graduate medical education 2008: a review for emergency medicine. Acad Emerg Med. 2008;;15:1117–1129. doi: 10.1111/j.1553-2712.2008.00188.x. [DOI] [PubMed] [Google Scholar]
- 2.McLaughlin SA, Bond W, Promes S, et al. The status of human simulation training in emergency medicine residency programs. SimulHealthc. 2006;;1:18–21. doi: 10.1097/01266021-200600010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Okuda Y, Bond W, Bonfante G, et al. National growth in simulation training within emergency medicine residency programs, 2003–2008. Acad Emerg Med. 2008;;15:1113–1116. doi: 10.1111/j.1553-2712.2008.00195.x. [DOI] [PubMed] [Google Scholar]
- 4.Tubbs RJ, Murphy B, Mainiero MB, et al. High-fidelity medical simulation as an assessment tool for radiology residents' acute contrast reaction management skills. J Am Coll Radiol. 2009;;6:582–587. doi: 10.1016/j.jacr.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Donoghue AJ, Durbin DR, Nadel FM, et al. Effect of high-fidelity simulation on Pediatric Advanced Life Support training in pediatric house staff: a randomized trial. Pediatr Emerg Care. 2009;;25:139–144. doi: 10.1097/PEC.0b013e31819a7f90. [DOI] [PubMed] [Google Scholar]
- 6.Fraser K, Peets A, Walker I, et al. The effect of simulator training on clinical skills acquisition, retention and transfer. Med Educ. 2009;;43:784–789. doi: 10.1111/j.1365-2923.2009.03412.x. [DOI] [PubMed] [Google Scholar]
- 7.Ali J, Adam RU, Sammy I, et al. The simulated Trauma Patient Teaching Module—does it improve student performance? J Trauma. 2007;;62:1416–1420. doi: 10.1097/TA.0b013e3180479813. [DOI] [PubMed] [Google Scholar]
- 8.Kanumuri P, Ganai S, Wohaibi EM, et al. Virtual reality and computer-enhanced training devices equally improve laparoscopic surgical skill in novices. JSLS. 2008;;12:219–226. [PMC free article] [PubMed] [Google Scholar]
- 9.Koniaris LG, Kaufman D, Zimmers TA, et al. Two third-year medical student-level laboratory shock exercises without large animals. Surg Infect (Larchmt) 2004;;5:343–348. doi: 10.1089/sur.2004.5.343. [DOI] [PubMed] [Google Scholar]
- 10.Euliano TY. Small group teaching: clinical correlation with a human patient simulator. Adv Physiol Educ. 2001;;25:36–43. doi: 10.1152/advances.2001.25.1.36. [DOI] [PubMed] [Google Scholar]
- 11.Tan GM, Ti LK, Suresh S, et al. Teaching first-year medical students physiology: does the human patient simulator allow for more effective teaching? Singapore Med J. 2002;;43:238–242. [PubMed] [Google Scholar]
- 12.Gordon JA. A simulator-based medical education service. Acad Emerg Med. 2002;;9:865. doi: 10.1111/j.1553-2712.2002.tb02182.x. [DOI] [PubMed] [Google Scholar]
- 13.Fitch MT. Using high-fidelity emergency simulation with large groups of preclinical medical students in a basic science course. Med Teach. 2007;;29:261–263. doi: 10.1080/01421590701297334. [DOI] [PubMed] [Google Scholar]
- 14.Fitch MT, Manthey DE. A procedures curriculum for medical students. Med Educ. 2009;;43:1100. doi: 10.1111/j.1365-2923.2009.03485.x. [DOI] [PubMed] [Google Scholar]
- 15.Manthey DE, Ander DS, Gordon DC, et al. Emergency medicine clerkship curriculum: an update and revision. Acad Emerg Med. 2010;;17:638–643. doi: 10.1111/j.1553-2712.2010.00750.x. [DOI] [PubMed] [Google Scholar]
- 16.Ten Eyck RP, Tews M, Ballester JM. Improved medical student satisfaction and test performance with a simulation-based emergency medicine curriculum: a randomized controlled trial. Ann Emerg Med. 2009;;54:684–691. doi: 10.1016/j.annemergmed.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 17.Noeller TP, Smith MD, Holmes L, et al. A theme-based hybrid simulation model to train and evaluate emergency medicine residents. Acad Emerg Med. 2008;;15:1199–1206. doi: 10.1111/j.1553-2712.2008.00183.x. [DOI] [PubMed] [Google Scholar]
- 18.Gordon JA, Shaffer DW, Raemer DB, et al. A randomized controlled trial of simulation-based teaching versus traditional instruction in medicine: a pilot study among clinical medical students. Adv Health Sci Educ. 2006;;11:33–39. doi: 10.1007/s10459-004-7346-7. [DOI] [PubMed] [Google Scholar]
- 19.Shukla A, Kline D, Cherian A, et al. A simulation course on lifesaving techniques for third-year medical students. Simul Healthc. 2007;;2:11–15. doi: 10.1097/01.SIH.0b013e31802ccf6c. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz LR, Fernandez R, Kouyoumjian SR, et al. A randomized comparison trial of case-based learning versus human patient simulation in medical student education. Acad Emerg Med. 2007;;14:130–137. doi: 10.1197/j.aem.2006.09.052. [DOI] [PubMed] [Google Scholar]
- 21.Davis DP, Buono C, Ford J, et al. The effectiveness of a novel, algorithm-based difficult airway curriculum for air medical crews using human patient simulators. Prehosp Emerg Care. 2007;;11:72–79. doi: 10.1080/10903120601023370. [DOI] [PubMed] [Google Scholar]
- 22.Hall RE, Plant JR, Bands CJ, et al. Human patient simulation is effective for teaching paramedic students endotracheal intubation. Acad Emerg Med. 2005;;12:850–855. doi: 10.1197/j.aem.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Rosenthal ME, Adachi M, Ribaudo V, et al. Achieving housestaff competence in emergency airway management using scenario based simulation training: comparison of attending vs housestaff trainers. Chest. 2006;;129:1453–1458. doi: 10.1378/chest.129.6.1453. [DOI] [PubMed] [Google Scholar]
- 24.Wayne DB, Didwania A, Feinglass J, et al. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest. 2008;;133:56–61. doi: 10.1378/chest.07-0131. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen HB, Daniel-Underwood L, Van Ginkel C, et al. An educational course including medical simulation for early goal-directed therapy and the severe sepsis resuscitation bundle: an evaluation for medical student training. Resuscitation. 2009;;80:674–679. doi: 10.1016/j.resuscitation.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 26.Heitz C, Brown A, Johnson JE, et al. Large group high-fidelity simulation enhances medical student learning. Med Teach. 2009;;31:e206–e210. doi: 10.1080/01421590802637990. [DOI] [PubMed] [Google Scholar]
- 27.Ten Eyck RT, Markus MM, Janz TJ, et al. Student satisfaction with simulation to support a second-year medical student respiratory module. Simul Healthc. 2009;;4:291. [Google Scholar]
- 28.Smolle J, Prause G, Smolle-Jüttner FM. Emergency treatment of chest trauma—an e-learning simulation model for undergraduate medical students. Eur J Cardiothorac Surg. 2007;;32:644–647. doi: 10.1016/j.ejcts.2007.06.042. [DOI] [PubMed] [Google Scholar]
- 29.Dev P, Heinrichs WL, Youngblood P, et al. Virtual patient model for multi-person virtual medical environments. AMIA Annu Symp Proc. 2007;11:181–185. [PMC free article] [PubMed] [Google Scholar]
- 30.Youngblood P, Harter PM, Srivastava S, et al. Design, development, and evaluation of an online virtual emergency department for training trauma teams. Simul Healthc. 2008;;3:146–153. doi: 10.1097/SIH.0b013e31817bedf7. [DOI] [PubMed] [Google Scholar]


