Abstract
Introduction
Patients are commonly admitted to the hospital for observation following blunt abdominal trauma (BAT), despite initially negative emergency department (ED) evaluations. With the current use of screening technology, such as computed tomography (CT) of the abdomen and pelvis, ultrasound, and laboratory evaluations, it is unclear which patients require observation. The objective of this study was to determine the prevalence of intra-abdominal injury (IAI) and death in hemodynamically normal and stable BAT patients with initially negative ED evaluations admitted to an ED observation unit and to define a low-risk subgroup of patients and assess whether they may be discharged without abdominal/pelvic CT or observation.
Methods
This was a retrospective cohort study performed at an urban level 1 trauma center and included all BAT patients admitted to an ED observation unit as part of a BAT key clinical pathway. All were observed for at least 8 hours as part of the key clinical pathway, and only minors and pregnant women were excluded. Outcomes included the presence of IAI or death during a 40-month follow-up period. Prior to data collection, low-risk criteria were defined as no intoxication, no hypotension or tachycardia, no abdominal pain or tenderness, no hematuria, and no distracting injury. To be considered low risk, patients needed to meet all low-risk criteria.
Results
Of the 1,169 patients included over the 2-year study period, 29% received a CT of the abdomen and pelvis, 6% were admitted to the hospital from the observation unit for further management, 0.4% (95% confidence interval [CI], 0.1%–1%) were diagnosed with IAI, and 0% (95% CI, 0%–0.3%) died. Patients had a median combined ED and observation length of stay of 9.5 hours. Of the 237 (20%) patients who met low-risk criteria, 7% had a CT of the abdomen and pelvis and 0% (95% CI, 0%–1.5%) were diagnosed with IAI or died.
Conclusion
Most BAT patients who have initially negative ED evaluations are at low risk for IAI but still require some combination of observation and CT. A subgroup of BAT patients may be safely discharged without CT or observation after the initial evaluation.
INTRODUCTION
Blunt abdominal trauma (BAT) is common, and the prevalence of intra-abdominal injury (IAI) following BAT has been reported to be as high as 12% to 15%.1–7 Diagnostic evaluation of patients with BAT varies but may include such modalities as physical examination, focused ultrasonography, computed tomography (CT), diagnostic peritoneal lavage, laparoscopy, laparotomy, laboratory tests, or observation. When patients have sustained BAT and have undergone an otherwise negative diagnostic evaluation in the emergency department (ED), diagnostic algorithms have included the addition of CT of the abdomen and pelvis, admission to the hospital for an extended observation period, or both, to evaluate for occult IAI.8–10 The incidence, however, of IAI in patients who are hemodynamically stable and have initially negative diagnostic evaluations in the ED is quite low, probably occurring in less than 1%.10
Physical examination and focused abdominal ultrasonography comprise the standard initial abdominal evaluation for trauma in most instances. Ultrasound and diagnostic peritoneal lavage have excellent sensitivities for the detection of hemoperitoneum but do not accurately detect IAI in the absence of abdominal free fluid. A significant body of data indicates that physical examination alone is an insensitive predictor of IAI in the setting of blunt trauma.11–15 Similarly, laboratory tests play a limited role in this setting.1,16–18 CT, although excellent for detecting and grading solid organ injuries, is less sensitive for detecting certain injuries, including those to the mesentery, bowel, pancreas, and diaphragm.19,20 The prospect of missing injuries has constituted the rationale for observing patients following BAT.
Historically, experts have recommended a 23-hour observation period following BAT8; however, the optimal observation period remains unknown. More recently, several authors have suggested that patients can be safely discharged without observation if the abdominal/pelvis CT is normal and there is no other reason for admission to the hospital.4,21
There remains significant controversy regarding which trauma patients require abdominal/pelvis CT, which should undergo observation with or without performing abdominal/pelvis CT, and which patients may be safely discharged following the initial evaluation without CT or observation. Multisystem trauma patients with significant injuries to other organ systems are at increased risk for IAI, and these patients typically receive abdominal/pelvis CT in addition to other diagnostic evaluations. Unfortunately, it is unclear how clinicians should evaluate patients whose initial evaluation reveals no injuries. Specifically, it is not clear what constitutes low-risk BAT and what diagnostic approach should be pursued in these patients. No study has defined criteria useful in identifying patients who can be safely discharged from the ED without performing an abdominal/pelvic CT or extended observation.
The purposes of this study were to (1) determine the prevalence of IAI and death in hemodynamically normal and stable BAT patients with initially negative ED evaluations admitted to an ED observation unit and (2) define a low-risk subgroup of these patients and to assess whether they may be discharged without abdominal/pelvic CT or observation.
METHODS
This study was approved by the Research Committee and Institution Review Board for our institution and met criteria for exemption from informed consent.
Study Design and Setting
This was a retrospective cohort study performed at Denver Health Medical Center in Denver, Colorado. Denver Health Medical Center is an urban level 1 trauma center for the city and county of Denver as well as a regional trauma referral center for the state of Colorado and the Rocky Mountain region. Its annual major trauma census is approximately 2,500, and its annual ED census is approximately 60,000 adult patients.
Patients who present to the ED after sustaining BAT are evaluated and managed in accordance with Advanced Trauma Life Support guidelines and a previously published institutional BAT key clinical pathway (KCP).13 In the pathway, patients receive an evaluation by the trauma team, which includes radiographs of the cervical spine, chest, pelvis, an abdominal ultrasound, and a limited laboratory evaluation (hematocrit, urinalysis, blood alcohol level, and pregnancy test, where applicable). Patients are examined by members of the trauma team, including emergency medicine and surgical residents, and attending physicians. The decision to obtain an abdominal/pelvic CT is left to the discretion of the trauma team.
Patients enrolled in the BAT KCP who have diagnostic results not requiring admission to the hospital and who remain hemodynamically stable during their initial ED visits are observed. Patients who have minor trauma that does not trigger a trauma team evaluation do not enter the BAT KCP.
According to the BAT KCP, patients are observed for 8 hours in a 6-bed, monitored observation unit adjacent to the ED. All patients who undergo observation for BAT have, as part of their continued evaluation, a repeat abdominal examination and a repeat hematocrit and are discharged if their examination is unchanged or improved, if their hematocrit is stable, if they are ambulatory without altered mental status, and if no other medical conditions are noted that require admission to the hospital.
Study Population
All adult patients (age greater than or equal to 18 years) who underwent observation for BAT in the designated observation unit from January 1, 2000, through December 31, 2001, were included in this study. We searched the patient log of the observation unit electronically and manually to identify all patients observed specifically for BAT.
Patients were included on an intent-to-treat basis, meaning that those not being observed a full 8 hours (usually against medical advice) in accordance to the KCP were still included.
Patients who were younger than 18 years or pregnant were excluded from the study because of the special considerations relevant in the management of these patient subgroups. Patients with unavailable medical records were also excluded from the study sample.
Data Collection
We systematically reviewed all medical records and collected data using a closed-response data collection instrument. The following data were collected for all patients: age, sex, mechanism of injury (eg, fall, assault, motor vehicle collision, etc), vital signs, physical examination findings (eg, abdominal tenderness, evidence of head trauma, lacerations, extremity deformity, etc), bedside abdominal ultrasound results, radiology reports, laboratory results, diagnoses, and final disposition. Additional data included length of observation (defined as the time from ED registration to the time of discharge from the observation unit). Primary outcome measures included IAI and all-cause mortality. We used several parallel and overlapping approaches to identify and classify the outcome variables, including (1) all patient records from repeat or follow-up visits were retrieved and evaluated from the time of initial observation through April 2005 (a minimum 40-month follow-up period), (2) the trauma registries from all level 1 and level 2 trauma centers in the Denver metropolitan area were queried for visits after the original date of service, and (3) the state's Department of Public Health database of death records was queried through April 2005 for deaths after the date of service. We queried each trauma registry for deaths or unscheduled hospital admissions for all patients included or excluded in this study, and the state death registry was queried to identify those patients who had died from the time of their initial ED visit through April 2005.
Low-risk criteria for IAI were based on prior literature and clinical experience for the evaluation of BAT and were defined prior to data collection as the absence of intoxication, absence of hypotension (defined as a systolic blood pressure less than 90 mm Hg) in the prehospital or ED settings, absence of tachycardia in the ED (defined as a heart rate of greater than 100 beats per minute), absence of abdominal pain or tenderness, absence of gross hematuria, and absence of distracting injury. We defined alcohol intoxication as a measured alcohol level greater than or equal to 80 mg/dL or clinical intoxication documented in the medical record. Other intoxication was defined as admitted use or presence of a controlled substance on a urine toxicologic screen. We defined distracting injury as any fracture, any significant soft-tissue or chest injury requiring repeated doses of narcotics during the initial ED evaluation, or a closed head injury significant enough to prompt the ordering of a head CT.
Statistical Analyses
We performed descriptive statistics for all variables. Continuous data are reported as medians with interquartile ranges (IQR), and categorical data are reported as percentages with 95% confidence intervals (CI). We used CIs to compare differences between study groups. No corrections were made for multiple comparisons, and no a priori sample size was calculated.
We entered all data into an electronic spreadsheet (Microsoft Excel, Microsoft Corporation, Redmond, Washington) and transferred into native SAS format using translational software (dfPower DBMS/Copy, DataFlux Corporation, Cary, North Carolina). We performed all statistical analyses with either SAS version 9.1 (SAS Institute Inc, Cary, North Carolina) or Stata Version 10 (Stata Corporation, College Station, Texas).
RESULTS
During the 2-year study period, 7,369 patients were admitted to the observation unit. Of these, 1,277 (17%) were observed specifically for BAT in accordance with the KCP. Of these, 108 (8%) were excluded, resulting in a study sample of 1,169 patients (Figure).
Figure.
Flow diagram illustrating the number and proportion of included and excluded patients, the reasons for exclusion, the proportion of patients who had records for follow up, and the number of primary outcome measures. ED, emergency department; BAT, blunt abdominal trauma.
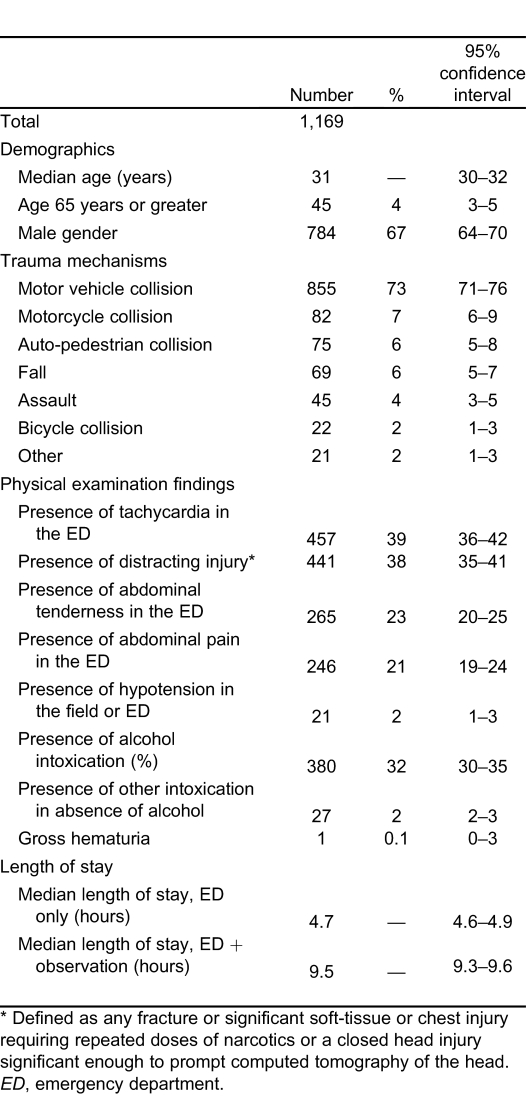
The median age of the study sample was 31 (IQR: 23–42) years, and 715 (66%) were male. The most common mechanisms resulting in BAT were motor vehicle collision (73%), motorcycle collision (7%), auto-pedestrian collision (6%), and fall (6%). The median ED time before transfer to the observation unit was 4.7 (IQR: 3.6–5.9) hours. The median total observation time (ie, ED plus observation length of stay) was 9.5 (IQR: 8.6–11.0) hours. Seventy-nine patients were observed less than the 8 hours specified by the KCP, with a minimum total observation time of 3 hours and 25 minutes. The most common clinical findings were presence of tachycardia (39%), presence of a distracting injury (38%), abdominal tenderness (23%), and abdominal pain (21%; Table 1).
Table 1.
Mechanisms and physical examination findings of patients with blunt abdominal trauma.
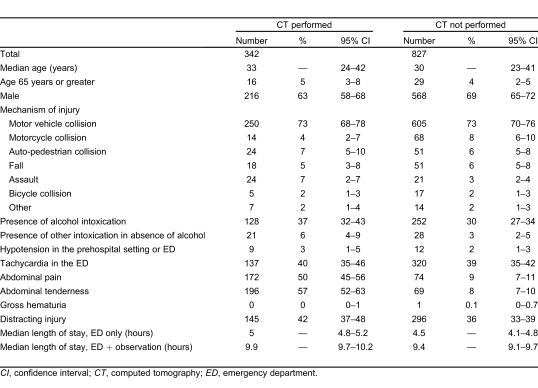
Of the 1,169 patients, 342 (29%) had an abdominal/pelvic CT performed in the ED, leaving 827 patients (71%) who were initially evaluated and managed without an abdominal/pelvic CT. Thirty-five patients (3%) received an abdominal/pelvic CT for a change in condition during their observation, 1 of which was a repeat CT. The distribution of mechanism of injury was not statistically different between those patients who received or did not receive an initial abdominal/pelvic CT (Table 2).
Table 2.
Patient characteristics for those who experienced blunt abdominal trauma by whether abdominal/pelvic CT was performed in the ED.
Patients who had abdominal pain or abdominal tenderness were more likely to undergo abdominal CT as part of their initial evaluation (Table 2).
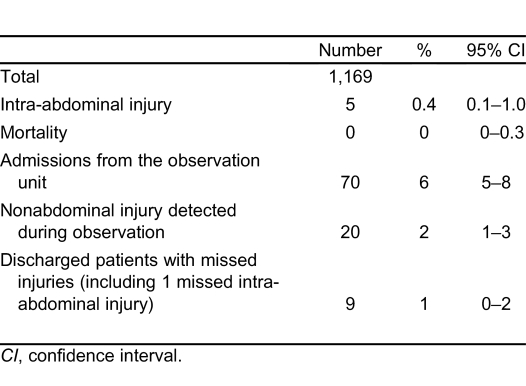
Of the 1,169 patients, 5 (0.4%, 95% CI: 0.1%–1.0%) had an IAI and 0 (0%, 95% CI: 0%–0.3%) died from the resulting trauma (Table 3).
Table 3.
Outcomes of patients observed for blunt abdominal trauma.
Of the 108 excluded patients, 0 (95% CI: 0%–3%) had identifiable IAI or death.
Seventy (6%) patients were admitted to the hospital from the observation unit. Of these, 33 (47%) were admitted for clinical suspicion of occult IAI; 33 (47%) were admitted for other reasons (including nonabdominal injuries, medical diagnoses, or pain control of nonabdominal injuries) and 4 (5%) for IAI diagnosed in the observation unit, 1 of which was later determined to have been an artifact on CT. Of the 33 patients admitted for suspicion of occult IAI, 16 (48%) were admitted for persistently abnormal vital signs, 13 (39%) for persistent abdominal pain or vomiting, and 4 (12%) for abnormal laboratory values (drop in hematocrit or hematuria). Of those admitted for suspicion of IAI, only 1 was later diagnosed with IAI.
Of the 1,099 (94%) patients discharged after observation, only 1 (0%, 95% CI: 0.1%–0.5%) was later diagnosed with IAI. Also, 8 (0.8%, 95% CI: 0.3%–1.5%) of the discharged patients had missed nonabdominal injuries, none of which required operative management, although 2 required readmission.
Of the 1,169 patients, 237 (20%, 95% CI: 18%–23%) met our predefined low-risk criteria, and of these, none (0%, 95% CI: 0%–2%) was ultimately diagnosed with IAI or died. Only 7 (3%) of the low-risk patients were admitted to the hospital, 2 for being unable to ambulate due to musculoskeletal pain and the others for reasons thought to be unrelated to trauma. One of the patients unable to ambulate was discovered to have a nonoperative pubic ramus fracture. Low-risk patients also spent less time in the ED when compared with all other patients. The frequencies of the study endpoints and of admissions were significantly lower in the low-risk group (Table 4).
Table 4.
Low-risk patients compared to all other patients by study endpoints and characteristics of their evaluations.
Direct follow-up data were available for 548 (47%) of the patients included in the study. Of these, 244 (45%) had follow up related to the initial injury (admission from observation unit or a repeat visit to a clinic or the ED), and 304 (55%) had follow up unrelated to the initial trauma. In a query of the state database for records of deaths, 27 patients in this study died between the time they were discharged and April 2005. Of these, none (0%) had been excluded from the study and (0%) died as a result of injuries related to their initial ED visits. In addition, we queried the trauma registries from all level 1 and level 2 trauma centers in the surrounding Denver metropolitan area for any study patients who had presented to one of these institutions and were subsequently diagnosed with missed injuries. Only 16 patients were identified as having presented to 1 of these institutions, and only 1 (0%) was admitted due to an injury resulting from the initial traumatic event.
DISCUSSION
There is little consensus in the literature for the management of patients deemed low risk for IAI following BAT. As a result, a number of approaches have emerged that potentially increase utilization of resources. Among these is the liberal use of CT scanning, even in patients with presumed minor mechanism trauma. Another approach has been to observe patients for extended periods of time, sometimes after CT scanning has failed to detect injury.
Our data clarify a number of issues pertaining to patients who sustain BAT. First, we were able to identify a subset of patients who were extremely unlikely to have IAI. We chose our low-risk criteria from the existing body of literature on BAT and included vital sign abnormalities, abdominal pain or tenderness, hematuria, distracting injury, or intoxication. Previously studied risk factors have included hypotension at any time; abdominal tenderness; presence of a seat belt sign; fractures of lower ribs, pelvis, or L-spine; distracting injuries; altered mental status or intoxication; and gross hematuria.11,22–29 In many instances, these low-risk criteria have either been difficult to apply or involved additional imaging to obviate the need for CT. For instance, Sirlin et al26,30 proposed that CT was unnecessary if patients had a negative screening abdominal ultrasound, no hematuria (defined as less than 50 red blood cell per high powered field), or fractures of the lumbar spine, pelvis, or lower 6 ribs. Poletti et al1 proposed that a negative abdominal ultrasound and chest radiograph, coupled with a normal white blood cell count, a hematocrit greater than 35%, a normal aspartate aminotransferase, and a nontender abdomen were evidence to discharge patients without obtaining an abdominal CT. While their criteria would have resulted in a 12% reduction in patients needing CT prior to discharge, they did not account for imaging or treatment of concomitant extra-abdominal injuries.
In our study, only 1 patient meeting low-risk criteria who was subsequently discharged had a significant missed injury (fractured sternum), and he did well. Seven patients (3%) of the 237 who met low-risk criteria were admitted to the hospital. Only 1 patient had a significant injury (a pubic ramus fracture managed nonoperatively), which was detected after the patient was unable to ambulate in the observation unit. An additional patient was unable to ambulate because of soft-tissue contusions and pain. None of the other admitted low-risk patients had a final discharge diagnosis that required specific treatment or was definitively attributed to trauma. Thus, all ambulatory low-risk patients could have been safely discharged without observation (or abdominal/pelvic CT) after completion of their initial ED evaluations.
Observation following BAT is a common occurrence, especially in academic trauma centers. Despite this, the optimal period for observation remains unclear. While the Eastern Association for the Surgery of Trauma guidelines recommend observation following BAT in patients who are clinically and hemodynamically stable, they do not specify the duration.9 Other authors have suggested that 24 hours is sufficient, while recent studies question the utility of this approach since there are very few injuries detected.4,6,8,10,21,31
Our study found that a minimum of an 8-hour observation period provided sufficient time to identify injuries among hemodynamically stable BAT patients. The median observation time in our study population was 9.5 hours because, in part, a relatively large proportion of the sample was intoxicated and required additional time to sober prior to discharge. Only 1 patient (less than 0.1%) with IAI was discharged. This patient, who did not have CT on the initial ED visit, was eventually found to have a grade III splenic laceration. She did not suffer any significant complications and was managed nonoperatively. A review of this patient's records determined that she did not meet our low-risk criteria by being intoxicated and by having a distracting distal radius fracture. As well, the patient also had a drop in her hematocrit by 11% from the first to the repeat performed 8 hours later.
Missed hollow viscous injury is usually the rationale for performing observation after a negative ED evaluation that includes abdominal CT. Our data do not support this as a universal approach as the 2 patients with hollow viscous injury had manifestations of their injuries. Both had persistent abdominal pain and tenderness either during their observation period or, in 1 case, after an abdominal/pelvic CT that was interpreted as normal. This patient was admitted for persistent abdominal pain, and a jejunal injury was detected on a CT performed 24 hours later.
Lastly, there is debate regarding the minimum diagnostic evaluation for patients with presumed BAT, especially when diagnostic endpoints include discharge from the ED or an observation period. In our study, all patients had a physical examination, focused abdominal ultrasound, hematocrit, and urinalysis prior to being placed in observation. While it is tempting to shortcut this approach and leave out certain components, such as the ultrasound, there is caution raised in the literature concerning this technique, even in patients presumed to have minimal trauma. Blaivas et al32 published a case series of 6 patients who were incidentally found to have hemoperitoneum by ultrasound following apparently minimal trauma. In fact, none of the patients in their series had abnormal vital signs, abdominal pain or tenderness, or altered mental status. While it may not be prudent to perform CT imaging on all patients, regardless of their mechanism of trauma, this does suggest an important role for a bedside test such as ultrasound in the initial evaluation of patients with suspected BAT.
LIMITATIONS
There are several limitations to this study. Because it was conducted at one urban level 1 trauma center, the results may not be generalizable. The study sample included patients from a level 1 trauma center who had already undergone a standardized ED evaluation that did not reveal overt injuries requiring hospitalization. As a result, patients included in our analysis were ultimately at lower risk for abdominal injury, as manifested by the low prevalence of IAI (0.4%). Given this, they were still selected from a larger group of patients that typifies those who present to a level 1 trauma center.
Selection bias may have occurred in the inclusion or exclusion of patients from the BAT KCP, retrospective identification of patients who were selected for observation, or the small proportion of patients who were excluded due to missing medical records. In addition, misclassification bias may have occurred as a result of the retrospective data abstraction portion of this project. We believe these potential biases were minimized by using standardized abstraction methodology, rigorous data cleaning, and the multifaceted approach to the acquisition of the outcome measures.
Data were collected on patients at a time when technology, such as the CT scan, was much less advanced and possibly less sensitive than it is currently. In part, an older data set was collected by design to ensure long-term (greater than 40 months) follow up. It is possible that older technology attributed to the low detection of IAI in our patient population. If this is indeed true, our low-risk criteria would be conservative by today's standards and would be even safer to apply with improved diagnostics.
Direct follow-up data were available for only 47% of the patients included in the study. Significant effort was made to acquire other indirect forms of follow-up data, including queries of all metropolitan trauma registries as well as state death records. It is conceivable, but very unlikely, that patients presented with trauma-related complications to hospitals outside the surrounding metropolitan area or died from their injuries outside of the state.
Finally, although our low-risk criteria performed well when retrospectively applied to this population, additional prospective validation and implementation evaluation will be required prior to recommending its widespread use.
CONCLUSION
This retrospective study demonstrates a low prevalence of IAI following BAT in patients who are hemodynamically stable and have initial negative evaluations in the ED. Ambulatory patients meeting our low-risk criteria may be safely discharged from the ED without an abdominal CT or extended observation. Patients who do not meet our low-risk criteria should receive an abdominal/pelvic CT or be observed if imaging availability is limited.
Footnotes
Supervising Section Editor: Eric R. Snoey, MD
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Poletti PA, Mirvis SE, Shanmuganathan K, et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma. 2004;;57:1072–1081. doi: 10.1097/01.ta.0000092680.73274.e1. [DOI] [PubMed] [Google Scholar]
- 2.Poletti PA, Kinkel K, Vermeulen B, et al. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology. 2003;;227:95–103. doi: 10.1148/radiol.2271020139. [DOI] [PubMed] [Google Scholar]
- 3.Stanley AC, Vittemberger F, Napolitano LM, et al. The use of delayed computerized tomography in the evaluation of blunt abdominal trauma: a preliminary report. Am Surg. 1999;;65:369–374. [PubMed] [Google Scholar]
- 4.Livingston DH, Lavery RF, Passannante MR, et al. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: results of a prospective, multi-institutional trial. J Trauma. 1998;;44:273–280. doi: 10.1097/00005373-199802000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Smith DR, Stanley RJ, Rue LW., III Delayed diagnosis of pancreatic transection after blunt abdominal trauma. J Trauma. 1996;;40:1009–1013. doi: 10.1097/00005373-199606000-00026. [DOI] [PubMed] [Google Scholar]
- 6.Lansink KW, Cornejo CJ, Boeije T, et al. Evaluation of the necessity of clinical observation of high-energy trauma patients without significant injury after standardized emergency room stabilization. J Trauma. 2004;;57:1256–1259. doi: 10.1097/01.ta.0000145075.51395.c9. [DOI] [PubMed] [Google Scholar]
- 7.Miller MT, Pasquale MD, Bromberg WJ, et al. Not so FAST. J Trauma. 2003;;54:52–59. doi: 10.1097/00005373-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Cowell VL, Ciraulo D, Gabram S, et al. Trauma 24-hour observation critical path. J Trauma. 1998;;45:147–150. doi: 10.1097/00005373-199807000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Hoff WS, Holevar M, Nagy KK, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: the East practice management guidelines work group. J Trauma. 2002;;53:602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 10.Stephan PJ, McCarley MC, O'Keefe GE, et al. 23-Hour observation solely for identification of missed injuries after trauma: is it justified? J Trauma. 2002;;53:895–900. doi: 10.1097/00005373-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Beck D, Marley R, Salvator A, et al. Prospective study of the clinical predictors of a positive abdominal computed tomography in blunt trauma patients. J Trauma. 2004;;57:296–300. doi: 10.1097/01.ta.0000130612.60661.c3. [DOI] [PubMed] [Google Scholar]
- 12.Mackersie RC, Tiwary AD, Shackford SR, et al. Intra-abdominal injury following blunt trauma: identifying the high-risk patient using objective risk factors. Arch Surg. 1989;;124:809–813. doi: 10.1001/archsurg.1989.01410070063013. [DOI] [PubMed] [Google Scholar]
- 13.Branney SW, Moore EE, Cantrill SV, et al. Ultrasound based key clinical pathway reduces the use of hospital resources for the evaluation of blunt abdominal trauma. J Trauma. 1997;;42:1086–1090. doi: 10.1097/00005373-199706000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Hirshberg A, Wall MJ, Jr, Allen MK, et al. Causes and patterns of missed injuries in trauma. Am J Surg. 1994;;168:299–303. doi: 10.1016/s0002-9610(05)80152-7. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez A, DuPriest RW, Jr, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims: a prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;;48:457–459. [PubMed] [Google Scholar]
- 16.Harris HW, Morabito DJ, Mackersie RC, et al. Leukocytosis and free fluid are important indicators of isolated intestinal injury after blunt trauma. J Trauma. 1999;;46:656–659. doi: 10.1097/00005373-199904000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Dunham CM, Watson LA, Cooper C. Base deficit level indicating major injury is increased with ethanol. J Emerg Med. 2000;;18:165–171. doi: 10.1016/s0736-4679(99)00188-2. [DOI] [PubMed] [Google Scholar]
- 18.Stassen NA, Lukan JK, Carrillo EH, et al. Examination of the role of abdominal computed tomography in the evaluation of victims of trauma with increased aspartate aminotransferase in the era of focused abdominal sonography for trauma. Surgery. 2002;;132:642–646. doi: 10.1067/msy.2002.127556. [DOI] [PubMed] [Google Scholar]
- 19.Fakhry SM, Watts DD, Luchette FA. Current diagnostic approaches lack sensitivity in the diagnosis of perforated blunt small bowel injury: analysis from 275,557 trauma admissions from the EAST multi-institutional HVI trial. J Trauma. 2003;;54:295–306. doi: 10.1097/01.TA.0000046256.80836.AA. [DOI] [PubMed] [Google Scholar]
- 20.Allen TL, Cummins BF, Bonk RT, et al. Computed tomography without oral contrast solution for blunt diaphragmatic injuries in abdominal trauma. Am J Emerg Med. 2005;;23:253–258. doi: 10.1016/j.ajem.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 21.Heilbrun ME, Chew FS, Tansavatdi KR, et al. The role of negative CT of the abdomen and pelvis in the decision to admit adults from the emergency department after blunt trauma. J Am Coll Radiol. 2005;;2:889–895. doi: 10.1016/j.jacr.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Holmes JF, Harris D, Battistella FD. Performance of abdominal ultrasonography in blunt trauma patients with out-of-hospital or emergency department hypotension. Ann Emerg Med. 2004;;43: 354–361. doi: 10.1016/j.annemergmed.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 23.Richards JR, Derlet RW. Computed tomography and blunt abdominal injury: patient selection based on examination, haematocrit and haematuria. Injury. 1997;;28:181–185. doi: 10.1016/s0020-1383(96)00187-8. [DOI] [PubMed] [Google Scholar]
- 24.Stassen NA, Lukan JK, Carrillo EH, et al. Abdominal seat belt marks in the era of focused abdominal sonography for trauma. Arch Surg. 2002;;137:718–722. doi: 10.1001/archsurg.137.6.718. [DOI] [PubMed] [Google Scholar]
- 25.Schurink GW, Bode PJ, van Luijt PA, et al. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury. 1997;;28:261–265. doi: 10.1016/s0020-1383(97)00007-7. [DOI] [PubMed] [Google Scholar]
- 26.Sirlin CB, Brown MA, Deutsch R, et al. Screening US for blunt abdominal trauma: objective predictors of false-negative findings and missed injuries. Radiology. 2003;;229:766–774. doi: 10.1148/radiol.2293030285. [DOI] [PubMed] [Google Scholar]
- 27.Ferrera PC, Verdile VP, Bartfield JM, et al. Injuries distracting from intraabdominal injuries after blunt trauma. Am J Emerg Med. 1998;;16:145–149. doi: 10.1016/s0735-6757(98)90032-8. [DOI] [PubMed] [Google Scholar]
- 28.Self ML, Blake AM, Whitley M, et al. The benefit of routine thoracic, abdominal, and pelvic computed tomography to evaluate trauma patients with closed head injuries. Am J Surg. 2003;;86:609–613. doi: 10.1016/j.amjsurg.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Knudson MM, McAninch JW, Gomez R, et al. Hematuria as a predictor of abdominal injury after blunt trauma. Am J Surg. 1992;;164:482–485. doi: 10.1016/s0002-9610(05)81185-7. [DOI] [PubMed] [Google Scholar]
- 30.Sirlin CB, Brown MA, Andrade-Barreto OA, et al. Blunt abdominal trauma: clinical value of negative screening US scans. Radiology. 2004;;230:661–668. doi: 10.1148/radiol.2303021707. [DOI] [PubMed] [Google Scholar]
- 31.Salim A, Sangthong B, Martin M, et al. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury. Arch Surg. 2006;;141:468–473. doi: 10.1001/archsurg.141.5.468. [DOI] [PubMed] [Google Scholar]
- 32.Blaivas M, Sierzenski P, Theodoro D. Significant hemoperitoneum in blunt trauma victims with normal vital signs and clinical examination. Am J Emerg Med. 2002;;20:218–221. doi: 10.1053/ajem.2002.32637. [DOI] [PubMed] [Google Scholar]